
Correlation between Salivary and Serum CRP Levels
in Urticaria Patients
Martina Rahmi, Taufiq Hidayat and Herwinda Brahmanti
Department of Dermatology and Venereology, Faculty of Medicine, Universitas Brawijaya,Saiful Anwar General Hospital,
Malang, East java, Indonesia
Keywords: Urticaria, Crp, Serum, Saliva, Correlation.
Abstract: Urticaria are commonand has a detrimental effect on that adversely impacts the quality of life. Urticaria occurs
due to mast cell activation and subsequently followed by inflammatory response. C- reactive protein (CRP),
the prototypical acute-phase reactant has been used widely on-specific clinical indicator to assess systemic
inflammatory status. Development of salivary CRP assays that is non-invasive, stress- and pain-free may
constitute an alternative strategy. To the best knowledge of author, there have been no studies done on the
correlation of saliva and serum CRP in urticaria patients. The objective of this study was to find the correlation
between salivary and serum CRP levels in patients with urticaria. The study design was cross-sectional
observational analytic and 21 urticaria patients were recruited. Saliva and serum CRP levels were measured
within 48 hours of lesion onset using immunoturbidimetry and ELISA method. Statistical analysis of the
Pearson correlation coefficient was used Saliva CRP concentrations ranged from 3,00x10
-6
mg/L to 1,77x10
-
3
mg/l, mean values were 3,77x10
-4
mg/l (± 4,72x10
-4
). Serum CRP concentration ranged from 0,40
mg/lto17,40 mg/l, mean values 3,28 mg/l (±3,85). We found a verystrongassociation CRP measured in saliva
with serum CRP(r= .814, p <.05). Salivary CRP measurement may thus facilitate alternative method of CRP
serum to know inflammatory state in patients with urticaria.
1 INTRODUCTION
Urticariais a distressing disorder that adversely
impacts the quality of life; yet it spathogenesis is not
well delineated and, accordingly, thetreatment is
often palliative and therapeutic outcome is
suboptimal (Jain., 2014). Mast cell activation
accompanied by inflammatory response is associated
with urticaria, which may be manifested by increased
serum concentration of C- reactive protein (CRP)
(Kasperska et al, 2011).
It has been demonstrated that
circulating CRP concentration is increased in acute
and chronic urticaria, and furthermore CRP
concentrations correlate with the disease severity.
Therefore, characterization of CRP in urticaria may
be essential to gain better insight into the activity of
the disease and to assess the degree of inflammation
(Kasperska, 2012).
The presence of CRP molecules in saliva and
recent technical advances provides an opportunity for
development of non-invasive assessments of disease
which would enable research in large population
representative samples and in young people (Oullet,
2011). However, salivary CRP reference ranges and
their correlation with serum levels are not established.
In addition, although a correlation between serum and
salivary CRP concentration has been observed this
relationship has not been investigated in urticaria
subjects. The goal of the study reported here was to
investigate the relationship between salivary and
blood serum levels of this molecules in patients with
urticaria.
2 METHODS
2.1 Subjects and Sample Collection
Study participants were21urticaria patients (76.2%
women) aged between 19 and 55 years (mean (SD) =
34.7 (11.8)). None reported comorbid disease
(cardiovascular, Diabetes mellitus, autoimmune or
liver), vasculitis or pressure urticaria, pregnancy and
overweight. Moreover, no participant reported on
corticosteroid or systemic immunomodulator.
14
Rahmi, M., Hidayat, T. and Brahmanti, H.
Correlation between Salivary and Serum CRP Levels in Urticaria Patients.
DOI: 10.5220/0008149700140017
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 14-17
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

Participants were recruited from
Dermatovenereology outpatient department of Saiful
Anwar General Hospital. Participants gave informed
consent. The study protocol was approved by Saiful
Anwar General Hospital Research Ethics
Commmitte. The subjects were asked to fast for at
least 30 minutes prior to giving their blood and saliva
samples. Unstimulated whole saliva was obtained
using the passive drool method (approximately 5 ml)
and the saliva samples were immediately placed on
ice following collection and stored at -20 °C. Blood
samples were collected by venipuncture into
vacutainer tubes and were immediately centrifuged to
separate blood components and measured.
2.2 C-reactive Protein Measurement
The concentration of CRP in saliva was determined
using ELISA method. C-reactive protein (CRP) levels
in serum were determined using turbidimetry method
using semiautomated analyzer.
2.3 Statistical Analyses
The association between salivary with serum CRP
was investigated using parametric (Pearson r) and
nonparametric (Spearman r). Difference in variations
in salivary and serum CRP mean levels of various
variables were analyzed with One-way Anova and T-
test.
3 RESULTS
3.1 Descriptive Data
In the study, total numbers of patients were 21
urticaria patients. Salivary CRP concentrations
ranged from 3.0 pg/ml to 1769.67 pg/ml (mean (SD)
= 377.44 (471.7)). From the total sample (n = 21),
none of these participants had salivary CRP values
that exceeded from the mean reported in healthy
adults (6131.40 pg/ml) (Salimetrics, 2011). Higher
values were observed for serum CRP (range = .4–
17.48 mg/dl; mean (SD) = 3.28 (3.85)).) The CRP
levels differed little from some variables (Table 1).
The levels of CRP serum were higher in women. Both
salivary and serum CRP levels were significantly
higher in the presence of lesion in time of
measurement.
Table 1: Salivary and Serum CRP levels between Variables.
Subjects Characteristic
SalivaryCRP mean
(mg/l) ± SD
p-value*
Serum CRP
mean (mg/l) ±
SD
p-value*
Age (years)
18 - 30
31 - 45
46 - 55
1,77x10
-4
± 1,67x10
-4
4,76x10
-4
± 5,83x10
-4
6,31x10
-4
± 6,20x10
-4
0,216
2,26 ± 1,93
3,18 ± 2,71
5,80 ± 7,74
0,323
Sex
Men
Women
7,10x10
-4
± 5,00x10
-4
2,74x10
-4
± 4,26x10
-4
0,070
7,28 ± 6,11
2,03 ± 1,66
0,004*
Family History
Yes
No
3,60x10
-4
± 4,90x10
-4
3,96x10
-4
± 4,77x10
-4
0,866
2,44 ± 1,79
4,21 ± 5,24
0,303
Antihistamin use
Yes
No
4,88x10
-4
± 5,92x10
-4
2,31x10
-4
± 1,76x10
-4
0,226
3,90 ± 4,83
2,46 ± 1,87
0,408
BMI
Underweight
Normoweight
2,40x10
-4
± 3,20x10
-4
3,92x10
-4
± 4,89x10
-4
0,675
1,05 ± 0,21
3,52 ± 3,98
0,402
Lesion
Presence
Absence
6,94x10
-4
± 7,63x10
-4
2,51x10
-4
± 2,23x10
-4
0,049*
5,92 ± 6,23
2,23 ± 1,76
0,044*
Correlation between Salivary and Serum CRP Levels in Urticaria Patients
15
Onset Last Lesion
<19 hours
>19 hours
3,32x10
-4
± 4,23x10
-4
6,51x10
-4
± 7,58x10
-4
0,290
2,66 ± 2,24
7,03 ± 8,98
0,066
Angioedema
Yes
No
3,54x10
-4
± 5,61x10
-4
3,95x10
-4
± 4,18x10
-4
0,850
2,58 ± 2,14
3,81 ± 4,78
0,482
Urticaria Type
Acute
Chronic
3,50x10
-4
± 4,42x10
-4
4,14x10
-4
± 5,33x10
-4
0,768
3,81 ± 4,85
2,58 ± 1,91
0,482
*Bold text indicates a statistically significant difference with a p-value less than 0.05
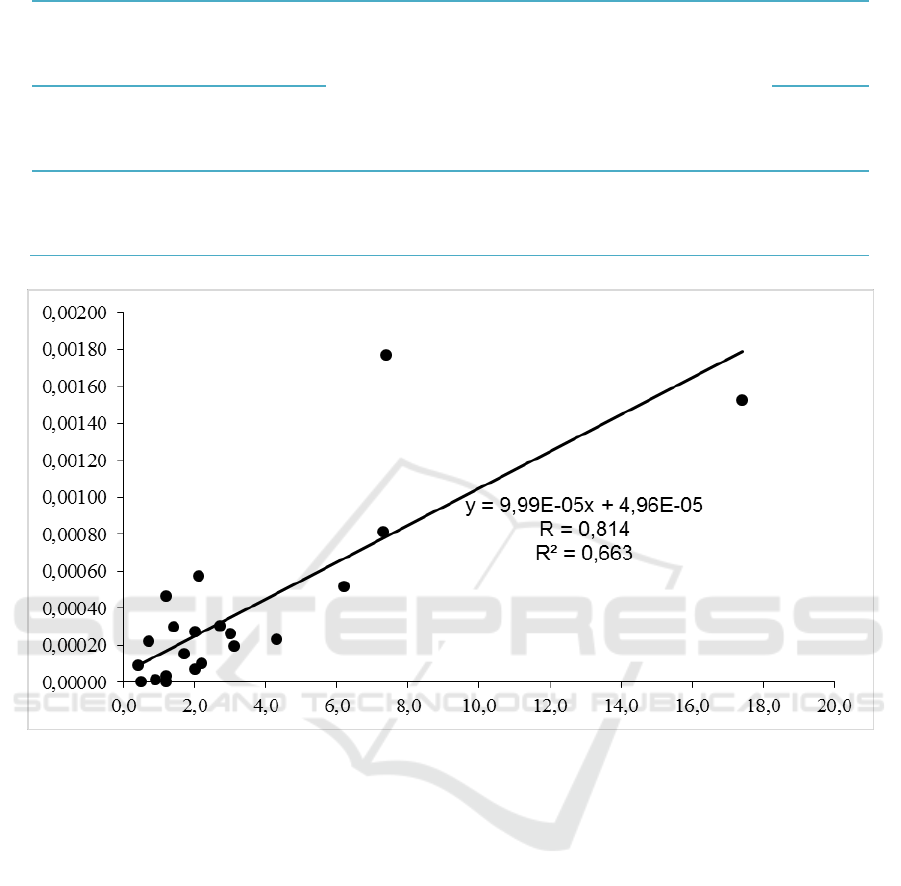
Figure 1: Correlation between salivary CRP and serum CRP in urticariapatients.x = serum CRP, y= salivary CRP, R=
Correlation Coefficient, R
2
= Coefficient of Determination.
3.2 Associations between Salivary with
Serum CRP Levels
As shown in Fig. 1, the correlation between salivary
and serum CRP was r = .81 (very strong). The saliva-
to-serum ratio was low (1:8700). The following
equation can be used to predict serum CRP from
saliva: y = 999.04x + 49.66 where y = salivary CRP
and x = serum CRP.
4 DISCUSSION
We observed a very strong association between CRP
measured in saliva and serum. Our study provides
supporting evidence suggesting that non-invasive
assessment of CRP in saliva allows the valid
prediction of serum CRP. Consistent with that result,
strong saliva and serum CRP correlations were
reported in animal studies, such as in healthy (r = .87)
and diseased dogs (r = .84) and in pigs (r = .73) (Parra
et al, 2005; Gutiérrez et al, 2009).
Our study was also
consistent with previous validation study that found
moderate to strong association in healthy subjects. Our
finding was however inconsistent with the absence of
association found between serum and salivary CRP in
medical students (Dillon et al, 2010).
The salivary CRP measure could be improved in
future studies by exploring three issues in this study.
First, there was significant difference in serum CRP
levels between men and women, probably due to one
men participant had a great extent of serum CRP
values than mean level (530%) with unclear
explanation. There was also significant difference in
salivary and serum CRP according to the presence of
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
16

lesion in time of measurement. Our finding suggests
that salivary CRP determination requires all the
patients show active urticaria at the time of
assessment.
Second, given the low saliva-to-serum CRP ratio,
it is possible that high-sensitivity ELISA may not be
sensitive enough to precisely quantify CRP in saliva,
particularly at low concentrations. Other analytical
methods have been used to determine CRP from
saliva, including time-resolved immunofluorometric
assays surface plasmon resonance immunosensor,
magnetic immunosensor, and lab-on-a-chip devices.
While these analytic strategies may be most remain
under development and thus are not readily accessible
to researchers, it should be explored further whether
the collection of larger saliva volume or parotid saliva
may optimize the measurement of CRP in the saliva.
4
Third, replication in larger samples is needed due to
large Standard of Deviation (SD) in the result of our
study.
This study provides supporting evidence for the
validation of salivary CRP as an alternative marker
for inflammation using a broadly available
technology adapted to saliva specimens. Saliva
sampling is non-invasive, stress-free, can be easily
performed in the participants’ natural settings and can
be repeated over time. Moreover, saliva collection has
considerable economical and logistic advantages over
venipuncture because it does not require immediate
manipulations, access to specialized laboratory
equipment’s and qualified personnel (Oullet et al,
2011).
Furthermore, future studies should extent the
present findings and correlate measurement of
salivary CRP with urticaria clinical severity as well
as therapy evaluation.
5 CONCLUSIONS
This study demonstrates a very strong positive
correlation between salivary and serum CRP in
urticaria patients.
ACKNOWLEDGEMENT
We are grateful to the participants and to laboratory
technician for technical assistance. Our thanks to the
Laboratory of Physiology Sciences, Faculty of
Medicine Universitas Brawijaya and Saiful Anwar
General Hospital Central Laboratory, Malang, East
java, Indonesia.
REFERENCES
Jain, S., 2014. Pathogenesis of chronic urticaria: An
overview. Dermatology Research and Practice.
doi:10.1155/2014/674709
Kasperska-Zajac, A., Sztylc, J., Machura, E., Jop, G., 2011.
Plasma IL-6 concentration correlates with clinical
disease activity and serum C-reactive protein
concentration in chronic urticaria patients. Clinical and
Experimental Allergy 41, 1386–1391.
doi:10.1111/j.1365-2222.2011.03789.x
Kasperska-Zajac, a, 2012. Acute-phase response in chronic
urticaria. Journal of the European Academy of
Dermatology and Venereology: JEADV 26, 665–72.
doi:10.1111/j.1468-3083.2011.04366.x
Ouellet-Morin, I., Danese, A., Williams, B., Arseneault, L.,
2011. Validation of a high-sensitivity assay for C-
reactive protein in human saliva. Brain, Behavior, and
Immunity 25, 640–646. doi:10.1016/j.bbi.2010.12.020
Salimetrics, SalivaBio. Saliva collection and handling
advice. 2011. Availableat www. salimetrics. com.
Parra, M.D., Tecles, F., Martínez-Subiela, S., Cerón, J.J.,
2005. C-reactive protein measurement in canine saliva.
Journal of Veterinary Diagnostic Investigation 17,
139–144. doi:10.1177/104063870501700207
Gutiérrez, A.M., Martínez-Subiela, S., Eckersall, P.D.,
Cerón, J.J., 2009. C-reactive protein quantification in
porcine saliva: A minimally invasive test for pig health
monitoring. Veterinary Journal 181, 261–265.
doi:10.1016/j.tvjl.2008.03.021
Dillon, M.C., Opris, D.C., Kopanczyk, R., Lickliter, J.,
Cornwell, H.N., Bridges, E.G., Nazar, A.M., Bridges,
K.G., 2010. Detection of homocysteine and C-reactive
protein in the saliva of healthy adults: Comparison with
blood levels. Biomarker Insights 2010, 57–61.
doi:10.4137/BMI.S5305
Correlation between Salivary and Serum CRP Levels in Urticaria Patients
17
