
Impact of Online Health Information on
Patient-physician Relationship and Adherence;
Extending Health-belief Model for Online Contexts
Tahir Hameed
SolBridge International School of Business, Daejeon, Republic of Korea
Keywords: Online Health Information, Patient-physician Relationship, Health-belief Model, Adherence, Health
Behavior.
Abstract: Physicians have information advantage over patients in terms of professional knowledge and expertise,
implying patients have to fully depend on them for diagnosis, prescription and treatment. However, in the
wake of abundant online health information (OHI) on the internet and through mobile apps, these days patients
appear to be better-informed when approaching their physicians. As per health-belief model, patients would
be motivated better to adhere to physicians’ prescribed treatments if they feel threatened by their symptoms
and/or when they are convinced about the benefits of the treatment. This research proposes improved health-
belief model incorporating use of OHI. It identifies different types of OHI shaping up patients’ perceptions
prior to interactions with physicians. It suggests that patient-physician meetings (relationship) and consequent
adherence behavior of the patients are inter-related and deeply affected by the initial perceptions of the
patients based on consumed OHI. The proposed model is being tested using anonymous survey data collected
immediately after patient-physician meetings in clinics/hospitals and subsequent adherence data from the
same patients. Key contribution of this paper is combining individual’s information behavior with health
behavior which provides much better understanding for management of emergent healthcare delivery models
in the digital economy.
1 INTRODUCTION
Nature of the patient-physician relationship plays an
important role in patient outcomes and well-being
(Kaplan et al., 1989). Traditionally, physicians have
held an advantage over patients in terms of
professional knowledge and expertise which implied
patients were fully dependent on physicians for
diagnosis, treatment options and prescriptions.
However, in the wake of abundant online health
information (OHI) on the internet and mobile apps,
these days patients appear to be better-informed when
approaching their physicians (Wald et al., 2007).
While several physicians look at the “informed
patient” in a positive way, a large number of
physicians also consider OHI a source of problems
and in-efficiencies in their diagnosis and treatment
procedures (McMullan, 2006, Rosenstein, 2015).
Informed patients tend to ask more questions during
consultation meetings, would like to discuss
alternative treatment options, are not convinced easily
on prescriptions and might choose not to engage in
further communications (Chung, 2013, Dedding et
al., 2011). Consequent patient-physician relationship,
formed on the basis of authority (from professional
expertise) and mutual trust could deteriorate,
ultimately leading to negative changes in the patient’s
health behavior.
There is a large emerging body of e-health
research, but in case of patient-physician interactions
and relationship, it is focused more on the physician’s
behavior and attitude or the meeting itself (Assis-
Hassid et al., 2016, Rosenstein, 2015); systematic
studies on linking patient-physician relation to
outcomes are largely missing (Clayman et al., 2016).
On the other hand, patient’s ensuing health behavior
and its antecedents have not been discussed to the best
of our knowledge.
Therefore, this version of our larger research,
constructs a theoretical model to study patient’s
health behavior, especially adherence, in the wake of
OHI consumption and changing nature of patient-
physician’s meetings. The second section of the paper
Hameed, T.
Impact of Online Health Information on Patient-physician Relationship and Adherence; Extending Health-belief Model for Online Contexts.
DOI: 10.5220/0006720905910597
In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) - Volume 5: HEALTHINF, pages 591-597
ISBN: 978-989-758-281-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
591

covers literature review, while third section discusses
the research model at some length. Fourth and the
concluding section discusses the progress and future
directions of this research.
2 LITERATURE REVIEW AND
THEORETICAL
BACKGROUND
2.1 Online Health Information Search
Online health information (OHI) search has emerged
as one of the most prolific uses of the internet.
According to (Fox, 2011, Fox and Duggan, 2015),
OHI search is taking a new social life of its own in the
internet.
OHI seekers typically search information about
symptoms, diagnosis, diseases, treatment options and
their effectiveness, while many of them also share
their own experiences about the above with others
(Hameed and Swar, 2015, Frost and Massagli, 2008,
Ba and Wang, 2013). On top of making sense of the
medical information, OHI seekers, especially if they
are diagnosed patients or their caretakers, also seek
information about hospitals, clinics, doctors and
interactions and outcomes of other patients with them
(McMullan, 2006). In general, almost everyone at
some point seek OHI about general well-being,
exercise, and diet and disease prevention.
2.2 Patient-physician Relationship
Charles et al. (1999) defined “patient-physician
relationship” (PPR) as a medical encounter which
involves shared decision-making and needs
consideration on the part of the physician for
considering different patient positions. However, in
contrast to “patient-physician communications”, PPR
could be generally considered multiple encounters
involving diagnosis, interpretation of medical
records, prescriptions and treatments/interventions.
The quality of PPR has direct relationship with
patient’s outcomes including patient’s willingness to
adhere to the prescribed treatment. (Kaplan et al.,
1989) were among early scholars who pointed out
“physician-patient relationship may be an important
influence on patients' health outcomes and must be
taken into account in light of current changes in the
health care delivery system that may place this
relationship at risk”.
PPR’s two main components include emotional
and informational aspects. Successful healtchare and
intervention requires strong patient-physician
communication. Emotional components include
genuineness, trust, respect, empathy, warmth and
acceptance (Ong et al., 1995). Informational
components include exchanging and sharing medical
information, educating patients and providing quality
medical management. Most patients' complaints and
displeasure arise from breakdown of the relationship
and communication with the physicians.
As noted previously about OHI, these days
patients may treat internet as a substitute or
supplement to traditional sources of health
information (Kitchens et al., 2014). Some people go
to the extent of self-diagnosing their symptoms
online. Hesse et al. (2005) noted that “most
physicians are already experiencing the effects of
patients showing up to their offices armed with
printouts from the World Wide Web and requesting
certain procedures, tests, or medications”.
Several physicians consider “informed patient” as
a participant in their health decisions, however a large
number of physicians also consider OHI a source of
problems and in-efficiencies in their diagnosis and
treatment decisions (McMullan, 2006, Rosenstein,
2015). Therefore, some physicians engage in
disruptive behavior during interactions with their
patients with negative implications for patient’s well-
being and healthcare delivery (Rosenstein, 2015,
Rosenstein and O’daniel, 2005).
Patients might find it hard to challenge their
physician or may not be able to insist for alternatives
due to physician’s knowledge, however it is easy for
them to disengage and ignore physician’s advice on
the spot or after the meetings. In fact, Quill and Brody
(1996) proposed that keeping a balance between
physician’s power and patients autonomy in choosing
the best treatment options would be better for the
well-being of the patients ultimately.
2.3 Health Behavior
Health behavior generally refers to one’s behavioral
actions with an awareness of their health outcomes
(positive or negative). Medical professionals and
policy makers are deeply interested in promoting
preventive health behaviors that could save the
burden on and costs of provision of healthcare
services (unhealthy practise such as smoking, etc.) by
reducing unnecessary negative health outcomes.
Adherence is one of the most common health
behavior which refers to one’s tendency to follow the
prescribed routine treatment or intervention gradually
reducing the illness symptoms or not worsening them
any further. Regular visitations of hospitals and
HEALTHINF 2018 - 11th International Conference on Health Informatics
592
preventive screening for highly likely infections or
diseases are also counted as positive health behavior.
Bering receptive and engaging positively with the
physician would also be counted as a positive health
behavior on the part of patients.
Change in health behaviors and corresponding
interventions have been studied from numerous
perspectives including social-psychological and
socio-cognitive (e.g. theory of planned behavior and
health-belief models), social-ecological and staged
perspectives (such as precede-proceed model),
among others (Glanz et al., 2008). This paper is
particularly interested in the former two approaches
which are discussed and incorporated to build a
theoretical research model in the next section.
3 RESEARCH MODEL AND
HYPOTHESES SETTING
In this section, health behavior of online informed
patients is conceptualized specifically through the
theoretical lenses of health-belief model and theory of
planned behavior.
3.1 Health Belief Model
As noted in the health behavior section, health-belief
model is one of the primary theoretical frameworks
for explaining preventive health behavior of people.
Godfrey Hochbaum, Stephen Kegels and Irwin
Rosenstock originated research on Health Belief
Model (HBM) to predict preventive health behavior
in a systematic way. They attempted to identify
factors behind pre-emptive decisions to obtain a chest
x-ray for early detection of tuberculosis as early as
1950s. HBM generally rests on social-psychological
theories trying to correlate belief patterns (perceptual
worlds) of patients with their health behaviors
(Rosenstock, 1990, Rosenstock, 1974).
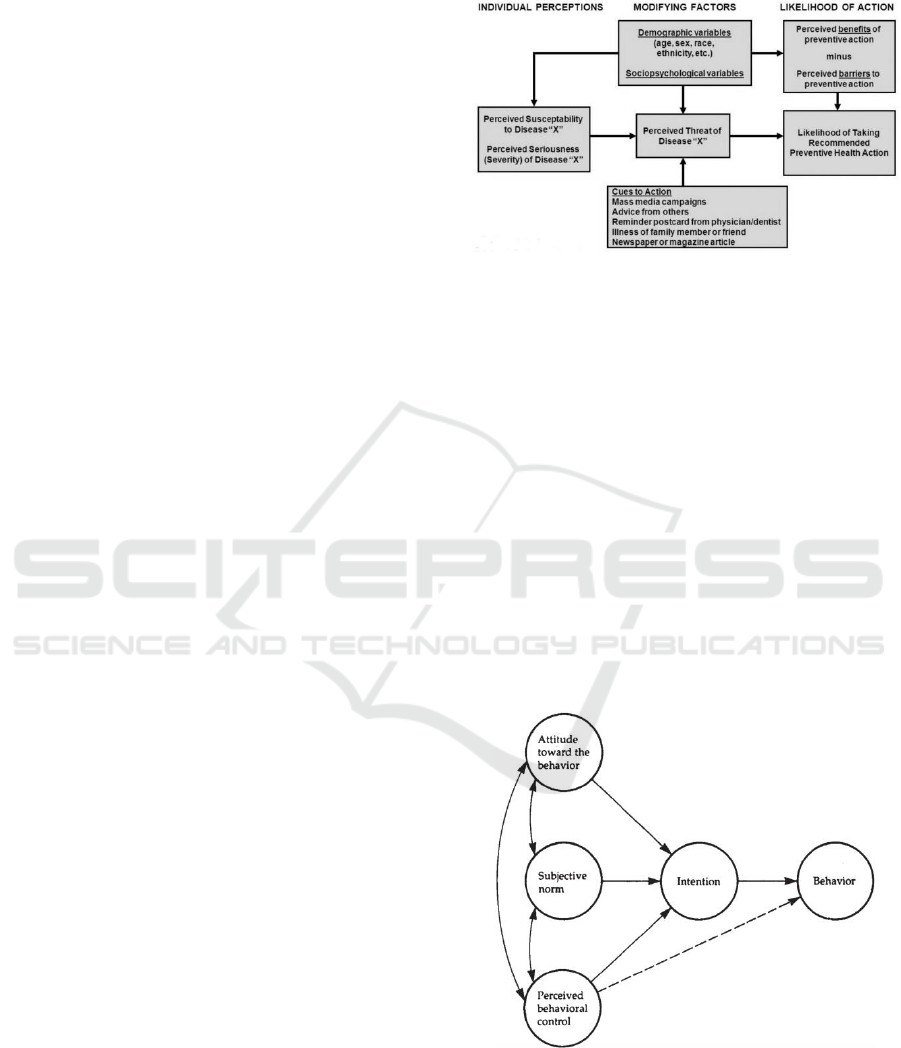
There are three categories of a person’s
motivation to undertake a positive or negative health
behavior: individual perceptions, modifying
behaviors, and likelihood of action (Rosenstock,
1990, Janz and Becker, 1984). Individual perceptions
about the current level of illness, disease or well-
being shape the individual’s perceived susceptibility
and perceived severity. A higher susceptibility and
severity of a disease could be life threatening,
therefore motivating a person highly to save himself
by changing his or her behavior radically. Modifying
factors include demographic variables, perceived
threat, and cues to action. The likelihood of action is
related with factors driving probability of appropriate
health behavior (Janz and Becker, 1984) (Figure 1).
Figure 1: Health Belief Model (Adapted from Becker and
Janz, 1985).
Social Learning Theory adds to HBM by
demonstrating there could be multiple sources of
acquiring new expectations or learning through
imitating others or even improving self-efficacy.
3.2 Theory of Planned Behavior
Theory of Planned Behavior (TPB) (Ajzen, 1985) and
the Theory of Reasoned Action (TRA) (Fishbein and
Ajzen, 1975) help in predicting behavioral intention
and subsequent behavioural actions of actors. TPB
proposes individual behavior is driven by three
factors, namely individual’s attitude, subjective
norms, and the individual’s perception of the ease or
control consequent to the situations arising from that
behavior (Figure 2).
Figure 2: Theory of Planned Behavior (Adapted from
Ajzen, 1985).
Attitude generally refers to the positive or
negative about a behavior which could be assessed
through one’s beliefs about consequences of the
Impact of Online Health Information on Patient-physician Relationship and Adherence; Extending Health-belief Model for Online Contexts
593

behavior and their desirability. Subjective norm is the
perception of individual about how divergent or
convergent the behavior would be in the opinion of
people surrounding the individual. Lastly, behavioral
control refers to the perceived difficulty in
performing a behavior.
Therefore, in the healthcare domain, it is not
difficult to discern that patient’s health behavior
(action), for example actual behavior of not
communicating or engaging effectively with the
physician should logically be preceded by an
intention to engage.
However, in this case, it would be critical to note
how attitudes, norms and perceived control are
altered by online health information and modified
health-beliefs. Yun and Park (2010) demonstrated
that consumers’ health consciousness, perceived
health risk and Internet health information use
efficacy influenced consumers’ beliefs, attitude and
intention of use of disease information on the Internet.
In another study, (Mills and Todorova, 2016)
presented the opposite view; they looked at the
propensity of susceptibility and severity of one’s
illness in shaping up their OHI search behavior.
However, this paper is taking a position that once
OHI is obtained information-seekers perceptions of
susceptibility and severity might be affected.
3.3 Extended Health-belief Model
Incorporating Online Health
Information Behavior
An original model (Figure 3) has been developed
amalgamating the theoretical concepts discussed
above i.e. health-belief model and the theory of
planned behavior. Discussion on the model follows.
3.3.1 Hypotheses 1-6: Online Health
Information Search and Health Belief
Formation
OHI sought could be generally categorized into three
categories, namely disease-related information,
physician or clinic related information (including
patient reviews and feedback) and finally the
community related information (experiences and
discussions on effectiveness of treatments, drugs and
interventions) (McMullan, 2006, Frost and Massagli,
2008).
Each type of information relates to different parts
of patient’s belief systems (or patterns). Disease-
related OHI affects perceived severity and severity of
symptoms and diagnostics results, therefore adding to
perceived threat to the life of a person. Therefore,
hypotheses 1-2 and hypotheses 5-6 establish
associations between disease-related OHI and
perceived threat as follows.
H1: Negative disease–related online health
information for one’s symptoms is positively
associated with higher levels of perceived severity
H2: Negative disease–related online health
information for one’s symptoms is positively
associated with higher levels of perceived
susceptibility
H5: Higher levels of perceived severity are
positively associated with perceived threats (to
life/well-being)
H6: Higher levels of perceived susceptibility are
positively associated with perceived threats (to
life/well-being)
Practitioner, hospital or clinic related information
typically drives ones perceptions about the potential
benefits or outcomes (recuperating from the disease).
The following hypothesis is therefore established.
H3: Positive reviews in the practitioner or clinic-
related online health information associate positively
with higher degree of perceived benefits
Finally, information-sharing in online health
communities contributes to self-confidence and self-
regulation of OHI seekers by knowing about the
experiences of others and comparing them with one’s
own (Ba and Wang, 2013, Frost and Massagli, 2008).
That leads us to propose the following hypothesis.
H4: High number of positive experiences (of
recuperation and adherence) in the community-
related online health information from the people
experiencing similar symptoms promotes higher
levels of self-efficacy
3.3.2 Hypotheses 7-9: Health Belief
Formation and Intention to Engage
with the Physician
Firmed health beliefs of patients regarding threats
would normally reflect their attitude towards
upcoming physician interactions. Patients with higher
levels of perceived life threats would like to get
clearer answers, firm assurances, and would be
willing to try interventions with bigger risks (even
asking for medically incorrect treatments) (Iverson et
al., 2008). Therefore, they would form an intention to
dig deeper, share their acquired OHI in low tone, and
be willing to understand and listen to the physician
more keenly. As a result, a positive relationship
should arise between the patient and the physician
leading to the following hypothesis:
HEALTHINF 2018 - 11th International Conference on Health Informatics
594
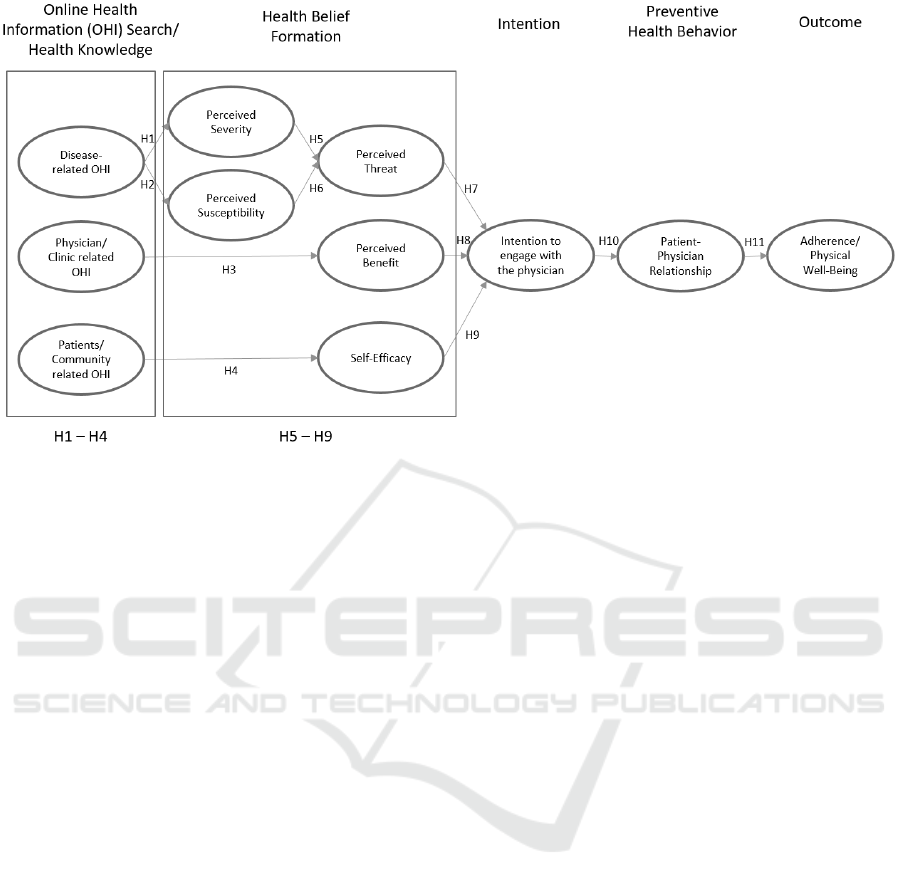
Figure 3: Extended Health-Belief Model incorporating online health information behavior (Source: Author).
H7: A high level of perceived health threats is
positively associated with intentions to positively
engage with the physician and vice versa
On the other hand, a higher level of perceived
benefits, based on the reputation of the physician or
hospital, should also wield similar psychological
effects on the patients’ intentions to engage with the
physician. Such effects come from our tendency to
accept the authority attached with knowledge and
expertise. However, if the reviews are negative,
patients’ might generate the intention to engage
firmly or aggressively with the physician about the
consumed OHI which could generate friction, in
some cases even leading to physician’s disruptive
behavior (Rosenstein, 2015).
H8: A high level of perceived health benefits is
positively associated with intentions to positively
engage with the physician and vice versa
Finally, if one could find positive stories about
others with similar symptoms (threats) recuperating
or fighting back the diseases successfully should
increase one’s confidence. On communities like
patientslikeme.com where extensive comparative
data is available in the form of user feedback on
effectiveness of drugs, treatments and home
remedies, one could adapt own opinions about
previously prescribed drugs or treatments with some
degree of confidence. The following hypothesis
covers these scenarios.
H9: Higher level of self-efficacy leads to
intentions of engaging positively with the physician
3.3.3 Hypothesis 10: Intention to Engage
with the Physician and
Patient-physician Relationship
Since intentions are antecedents of behavior (actions)
in theory of planned behavior, firmed intentions to
engage positively or negatively with the physicians
are highly likely to generate the intended behavior
(Ong et al., 1995). The corresponding hypothesis
follows.
H10: Intentions to engage positively with the
physician is positively associated with the level of
satisfaction (and trust) of the patient-physician
relationship
3.3.4 Hypothesis 11: Patient-physician
Relationship and Adherence
Finally, it is well-established in the literature that
satisfactory and trustworthy (positive) patient-
physician relationships encourage patients to adhere
to the prescribed treatments and interventions
(Kaplan et al., 1989, Ong et al., 1995). The following
hypothesis is therefore quite discernable.
H11: Satisfactory patient-physician relation-ships
are positively associated with adherence levels by the
patients (hence recuperation) and vice versa
Impact of Online Health Information on Patient-physician Relationship and Adherence; Extending Health-belief Model for Online Contexts
595

4 PROGRESS, CONCLUSIONS
AND FUTURE WORK
The paper has proposed an original conceptual model
connecting the online health information behavior
and health behavior of the patients and online users in
an increasingly online world. Therefore, it aims to
provide much-needed understanding and implications
for changing roles of patient and physician
engagement in the emergent healthcare delivery
model contexts.
A survey has been developed including several
measurement items from published sources (already
tested for construct validity) for each construct shown
in the research model. It is targeted to be circulated to
partner hospitals in South Korea and other countries
with an expected completion rate of around three
hundred surveys. The survey will be administered by
qualified physicians or their staff members. The
adherence data would be collected from the same
patients by the same doctors (or their staff). A due
approval has been acquired from the author’s
institutional ethics board for conducting research
involving human subjects.
Once the data collection would be completed
(approximately 3-6 months), both the measurement
model and the structural model would be tested using
PLS-SEM (partial least squares- structural equation
modelling) approach. Further analysis would lead to
acceptance or negation of the hypotheses and their
underlying explanations.
Future research could consider to test other health
behavioural outcomes than adherence such as those
covered by RAND 36-item survey (Hays et al., 1993).
Additionally moderating or mediating roles of
physicians’ attitudes, physician’s competencies,
cultural differences and gender differences would
greatly enhance the understanding of this model.
Social exchange perspective appears to be an
interesting alternate perspective which could shed
further light on the nature of patient-physical
relationship in this context.
REFERENCES
Ajzen, I. 1985. From intentions to actions: A theory of
planned behavior, Berlin, Heidelberg, Springer. doi:
10.1007/978-3-642-69746-3_2.
Assis-Hassid, S., Heart, T., Reychav, I. & Pliskin, J. S.
2016. Modelling Factors Affecting Patient-Doctor-
Computer Communication in Primary Care.
International Journal of Reliable and Quality E-
Healthcare (IJRQEH), 5, 1-17. doi: 10.4018/IJRQEH.
2016010101.
Ba, S. & Wang, L. 2013. Digital health communities: The
effect of their motivation mechanisms. Decision
Support Systems, 55, 941-947. doi: doi.org/10.1016/
j.dss.2013.01.003.
Charles, C., Gafni, A. & Whelan, T. 1999. Decision-making
in the physician–patient encounter: revisiting the shared
treatment decision-making model. Social science &
medicine, 49, 651-661. doi: 10.1016/S0277-9536(99)
00145-8.
Chung, J. E. 2013. Patient–provider discussion of online
health information: results from the 2007 Health
Information National Trends Survey (HINTS). Journal
of health communication, 18, 627-648. doi:
10.1080/10810730.2012.743628.
Clayman, M. L., Bylund, C. L., Chewning, B. & Makoul,
G. 2016. The impact of patient participation in health
decisions within medical encounters: a systematic
review. Medical Decision Making, 36, 427-452. doi:
10.1177/0272989X15613530.
Dedding, C., van Doorn, R., Winkler, L. & Reis, R. 2011.
How will e-health affect patient participation in the
clinic? A review of e-health studies and the current
evidence for changes in the relationship between
medical professionals and patients. Social science &
medicine, 72, 49-53. doi: 10.1016/j.socscimed.2010.
10.017.
Fishbein, M. & Ajzen, I. 1975. Belief, Attitude, Intention
and Behavior: An Introduction to Theory and Research,
Reading, MA, Addison-Wesley.
Fox, S. 2011. The social life of health information 2011,
Pew Internet & American Life Project Washington,
DC.
Fox, S. & Duggan, M. 2015. Pew Internet and American
Life Project [Online]. Pew Research Center
Washington, DC. Available: http://www.pewinternet.
org/2015].
Frost, J. H. & Massagli, M. P. 2008. Social uses of personal
health information within PatientsLikeMe, an online
patient community: what can happen when patients
have access to one another’s data. Journal of medical
Internet research, 10. doi: 10.2196/jmir.1053.
Glanz, K., Rimer, B. K. & Viswanath, K. 2008. Health
behavior and health education: theory, research, and
practice, John Wiley & Sons.
Hameed, T. & Swar, B. 2015. Social value and information
quality in online health information search.
Australasian Conference on Information Systems 2015
Adelaide. Australasian Conference on Information
Systems arXiv preprint arXiv:1606.03507
Hays, R. D., Sherbourne, C. D. & Mazel, R. M. 1993. The
rand 36‐item health survey 1.0. Health economics, 2,
217-227.
Hesse, B. W., Nelson, D. E., Kreps, G. L., Croyle, R. T.,
Arora, N. K., Rimer, B. K. & Viswanath, K. 2005. Trust
and sources of health information: the impact of the
Internet and its implications for health care providers:
findings from the first Health Information National
HEALTHINF 2018 - 11th International Conference on Health Informatics
596

Trends Survey. Archives of internal medicine, 165,
2618-2624. doi: 10.1001/archinte.165.22.2618.
Iverson, S. A., Howard, K. B. & Penney, B. K. 2008. Impact
of internet use on health-related behaviors and the
patient-physician relationship: a survey-based study
and review. Journal of the American Osteopathic
Association, 108, 699.
Janz, N. K. & Becker, M. H. 1984. The health belief model:
A decade later. Health Education & Behavior, 11, 1-47.
doi: 10.1177/109019818401100101.
Kaplan, S. H., Greenfield, S. & Ware Jr, J. E. 1989.
Assessing the effects of physician-patient interactions
on the outcomes of chronic disease. Medical care,
S110-S127.
Kitchens, B., Harle, C. A. & Li, S. 2014. Quality of health-
related online search results. Decision Support Systems,
57, 454-462. doi: 10.1016/j.dss.2012.10.050.
McMullan, M. 2006. Patients using the Internet to obtain
health information: how this affects the patient–health
professional relationship. Patient education and
counseling, 63, 24-28. doi: 10.1016/j.pec.2005.10.006.
Mills, A. & Todorova, N. 2016. An integrated perspective
on factors influencing online health-information
seeking behaviours. Australasian Conference on
Information Systems, 5-7 Dec 2016. Wollongong.
Ong, L. M., De Haes, J. C., Hoos, A. M. & Lammes, F. B.
1995. Doctor-patient communication: a review of the
literature. Social science & medicine, 40, 903-918. doi:
10.1016/0277-9536(94)00155-M
Quill, T. E. & Brody, H. 1996. Physician recommendations
and patient autonomy: finding a balance between
physician power and patient choice. Annals of internal
medicine, 125, 763-769. doi: 10.7326/0003-4819-125-
9-199611010-00010
Rosenstein, A. H. 2015. Physician disruptive behaviors:
Five year progress report. World journal of clinical
cases, 3, 930. doi: 10.12998/wjcc.v3.i11.930.
Rosenstein, A. H. & O’daniel, M. 2005. Disruptive
Behavior & Clinical Outcomes: Perceptions of Nurses
& Physicians. Nursing Management, 36, 18-28.
Rosenstock, I. M. 1974. Historical origins of the health
belief model. Health education monographs, 2, 328-
335. doi: 10.1177/109019817400200403
Rosenstock, I. M. 1990. The health belief model:
Explaining health behavior through expectancies. In:
Glanz, K., Rimer, B. K. & Viswanath, K. (Eds.) Health
behavior and health education: Theory, research, and
practice. San Francisco: Jossey-Bass.
Wald, H. S., Dube, C. E. & Anthony, D. C. 2007.
Untangling the Web—The impact of Internet use on
health care and the physician–patient relationship.
Patient education and counseling, 68, 218-224. doi:
10.1016/j.pec.2007.05.016.
Yun, E. K. & Park, H. 2010. Consumers’ disease
information–seeking behaviour on the Internet in
Korea. Journal of clinical nursing, 19, 2860-2868.
doi:10.1111/j.1365-2702.2009.03187.x.
Impact of Online Health Information on Patient-physician Relationship and Adherence; Extending Health-belief Model for Online Contexts
597
