
Feasibility of Labor Induction Success Prediction based on Uterine
Myoelectric Activity Spectral Analysis
C. Benalcazar Parra
1
, A.I. Tendero
1
, Y.Ye-Lin
1
, J. Alberola-Rubio
2
, A. Perales Marin
2
,
J. Garcia-Casado
1
and G. Prats-Boluda
1
1
Centro de Investigación e Innovación en Bioingeniería, Universidad Politécnica de Valencia, Valencia, Spain
2
Obstetric service, Hospital Universitario y Politécnico La Fe de Valencia, Valencia, Spain
Keywords: Labor Induction, Electrohysterogram, EHG, EHG-Bursts, Spectral Analysis, Deciles, Vaginal Delivery,
Cesarean Section, Active Phase of Labor.
Abstract: Labor induction using prostaglandins (PG) is a common practice to promote uterine contractions and to
facilitate cervical ripening. However, not all cases of labor inductions result in vaginal deliveries and it has
been associated with an increased risk of cesarean delivery. This last situation is associated to a greater
healthcare economic impact and to an increment in the maternal and fetal mortality and morbidity.
Obstetricians face different scenarios daily during a labor induction and it would be advantageous to be able
to infer the result of the labor induction for a better labor management. Uterine electrohysterogram (EHG)
has been proven to play an outstanding role in monitoring uterine dynamics and in characterizing the uterine
myoelectrical activity. Therefore, the aim of this study was to characterize and to compare the response of
uterine myoelectrical activity to labor induction drugs for different labor induction outcomes by obtaining and
analyzing the evolution of spectral parameters from EHG records picked up during the first 4 hours after labor
induction onset. Specifically, deciles from the EHG-bursts’ power spectral density (PSD) were worked out.
Our results showed that deciles D8 and D9 are able to discriminate between women who achieved active
phase of labor and those who did not. For women who achieved active phase of labor, D5 makes it possible
to separate women who delivered vaginally and those who underwent a cesarean section; finally D2-D6
enabled us to distinguish vaginal deliveries within 24 hours after induction onset from the other outcomes.
Thus, deciles computed from EHG PSD are potentially useful to discriminate the different outcomes of a
labor induction, suggesting the feasibility of induction success prediction based on EHG recording.
1 INTRODUCTION
Labor induction is an ordinary practice in obstetrics
whose objective is to induce a vaginal delivery. The
induction of labor is used in situations where maternal
and fetal risk of continuing pregnancy exceeds those
of termination of pregnancy. Approximately 23% of
all cases of birth in United states in 2012 were
performed with a previous induction (Hamilton et al.,
2012). It is a long process which can last many hours,
approximately 17-20 hours (Filho, Albuquerque and
Cecatti, 2010), and sometimes the waiting can be
extended to 36 hours. Pharmacologic methods for
cervical ripening and labor induction, such as
prostaglandins, have been used for decades (Gilstrop
and Sciscione, 2015) with the purpose of ripen the
cervix and stimulate uterine contractions. However,
this long and uncomfortable process does not ensure
a vaginal delivery and almost 20% of women that
have been induced end up labor with a cesarean
section (Seyb et al., 1999). This last implies the use
of more resources and longer hospital stays, both
associated to a greater healthcare cost when compared
with a spontaneous labor (Garcia-Simon et al., 2016).
Success of a labor induction has been defined as
vaginal delivery within 24 or 48 hours from labor
induction onset (Pandis et al., 2001; Indraccolo,
Scutiero and Greco, 2016) or vaginal delivery at any
time after labor induction onset (Ware and Raynor,
2000). From a pharmacological point of view, a labor
induction is considered successful if drug action
provokes women to achieve active phase of labor
(Baños et al., 2015; Benalcazar-Parra et al., 2017).
The most common method to predict labor induction
success is based on cervix assessment by the Bishop
score (Bishop, 1964). However, this measure is not
reliable and depends on the examiner subjectivity. In
fact, low accuracy of this predictor have been
70
Parra, C., Tendero, A., Ye-Lin, Y., Alberola-Rubio, J., Marin, A., Garcia-Casado, J. and Prats-Boluda, G.
Feasibility of Labor Induction Success Prediction based on Uterine Myoelectric Activity Spectral Analysis .
DOI: 10.5220/0006649400700077
In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) - Volume 4: BIOSIGNALS, pages 70-77
ISBN: 978-989-758-279-0
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

reported (AUC=0.39) (Bastani et al., 2011). Other
studies have considered other obstetrics variables
such as cervical length, maternal age, height, weight,
parity, and birth weight (Crane et al., 2004; Bastani et
al., 2011; Pitarello et al., 2013; Catherine Tolcher et
al., 2015; Prado et al., 2016) and showing an AUC
maximum of 0.69 for cervical length.
On the other hand, monitoring uterine contraction
is fundamental to assess maternal and fetal wellbeing
during the process, as well as, to estimate the labor
induction success. Intrauterine pressure is the most
accurate technique for monitoring uterine contractions.
However, it is an invasive technique and its application
requires membrane rupture (Vinken et al., 2009). The
most widely used method for non-invasively
monitoring uterine activity is to place a
tocodinamometer (TOCO) on women abdomen to
record changes of pressure in the abdominal contour
during uterine contractions. But they are uncomfor-
table, often inaccurate and depend on a subjective
interpretation by the examiner (Vinken et al., 2009).
Alternatively, electrohysterography (EHG) has
been proved to be a potentially useful technique for
non-invasively monitoring of uterine dynamics
obtaining better performance than TOCO (Alberola-
Rubio et al., 2013; Euliano et al., 2013; Benalcazar-
Parra et al., 2017). It consists of recording the
electrical activity of the uterus on the abdominal
surface using electrodes. At present, great efforts
have been made to differentiate between effective
contractions and non-effective contractions and
between term and preterm EHG records (Fele-Zorz et
al., 2008; Fergus et al., 2013). A shift of the energy
content toward higher frequencies as labor
approaches has been identified by literature (Marque
et al., 1986). Several spectral parameters have been
extracted from the power spectral density of the EHG
such as the deciles (D1-D9), which correspond to
frequencies below which it is contained 10-90% of
the total energy respectively (Alamedine et al., 2014),
and it has been reported its ability to distinguish
between pregnancy and labor contractions.
However, few efforts have been made to
characterize the uterine myoelectrical response to
labor induction drugs and to predict labor induction
outcome based on EHG recording (Tibor Toth, 2005;
Aviram et al., 2014; Benalcazar-Parra et al., 2017).
Therefore, the aim of this work was to determine the
feasibility of predicting different labor induction
outcomes, during the first 4 hours after labor
induction onset, by analyzing changes in the EHG
spectral characteristics as response of induction
drugs. Specifically, it was analyzed the time evolution
of deciles of the EHG-burst’s PSD.
2 MATERIAL AND METHODS
2.1 Signal Acquisition
The study adheres to the Declaration of Helsinki and
was approved by the ethics committee of the Hospital
Universitario y Politécnico La Fe (Valencia, Spain).
All subjects were informed of the nature of the study
and signed an informed consent form. Recording
sessions were carried out in healthy women with
singleton pregnancies and without risk who were
determined to undergo labor induction by medical
prescription. Specifically, 72 pregnant women with a
gestational age between 40 and 41 weeks were
enrolled in the study. The induction was carried out
by administration of two different types of drugs:
vaginal insertion of 25 μg misoprostol (Misofar, Bial,
Coronado, Portugal) with repeated doses every 4
hours up to a maximum of 3 doses (N=35) and 10 mg
of dinoprostone (Propess, Ferring, Germany) by
vaginal insertion (N=37). The following obstetrical
data was collected: maternal age, body mass index
(BMI), Bishop score and the labor induction outcome.
Patients were divided in 4 groups according to the
outcome of the delivery: G1: vaginal delivery within
24 hours after induction onset (N=26), G2: vaginal
delivery> 24 hours (N=26) after induction onset, G3:
cesarean section after achieving active phase of labor
(N=11), G4: cesarean section without achieving
active phase of labor (N=9).
Three different labor outcome scenarios were
studied:
• Scenario 1 (S1): Women achieving
active phase of labor (Successful group
S1GS= G1+G2+G3; N=63) vs women
non achieving active phase of labor,
(Failed group, S1GF=G4; N=9)
• Scenario 2 (S2): From women who
achieved active phase of labor, those
achieving vaginal delivery (Successful
group, S2GS=G1+G2; N=52) vs
cesarean section (Failed group
S2GF=G3; N=11)
• Scenario 3 (S3): Women achieving
vaginal delivery within 24 hours
(Successful group S3GS=G1; N=26) vs
other outcomes, (Failed group
(S3GF=G2+G3+G4; N=46)
TOCO and EHG were simultaneously acquired in
each recording session. The electrode arrangement
for the acquisition of EHG is shown in Figure 1: 2
electrodes were placed supraumbilically at each side
of the abdominal medial line with 8 cm of inter-
electrode distance corresponding to EHG monopolar
Feasibility of Labor Induction Success Prediction based on Uterine Myoelectric Activity Spectral Analysis
71

records (M1, M2), 1 reference electrode in the right
hip and 1 ground electrode in the left hip. The
recording time comprises 30 minutes corresponding
to recording of basal activity and 4 hour recording
from drug administration (induction onset). Details of
the recording protocol can be found in an previous
study (Benalcazar-Parra et al., 2017).
Figure 1: Surface electrodes arrangement for monopolar
EHG recordings (M1, M2).
2.2 EHG Signal Analysis
Since the EHG signal mainly distributes its energy in
the range of 0.1 - 4 Hz, a digital band pass filter was
performed to eliminate unwanted components. Then
EHG signal was down-sampled to a sample frequency
of 20 Hz to decrease the computational cost. After
signal pre-processing, the bipolar register was
obtained digitally as follows:
Bip = M2 - M1
(1)
Subsequently, from bipolar signal, EHG-bursts
associated to uterine contractions were manually
segmented using the same criteria as in a previous
study (Benalcazar-Parra et al., 2017). Next, in order
to characterize the EHG bursts, the deciles of the
power spectral density were obtained in the range of
(0.2-1Hz) since it has been reported that the main
uterine activity is distributed in this frequency range
(Marque et al., 1986; Garfield and Maner, 2007).
First, the Welch periodogram method was used to
calculate the power spectral density of each EHG-
burst with a window size of 60 seconds and 50%
overlap. Subsequently deciles were computed as
follows:
(2)
Where P is the power vector from the PSD and [D
j-1
,
Dj] is the frequency range associated to the decile D
j
with j=1…9.
To analyse the evolution of the EHG-bursts’
spectral parameters in response to labor induction
drugs, firstly the median values of the deciles
associated to the EHG-bursts present in consecutive
intervals of 30 minutes were worked out for each
patient. Then, for each decile and 30-minuteinterval,
the mean and standard deviation were calculated for
all patients of a group. Finally, a statistical analysis
was performed by the Mann–Whitney test (=0.05)
to determine if there were statistical differences
between the groups of each obstetrical scenario.
3 RESULTS
Table 1 summarizes the obstetrical variables and the
labor induction outcome of the population under
study. For a total of 72 patients, 87.5% achieved
active phase of labor. However, only 72.2% reached
vaginal delivery and 27.8% ended up with a cesarean
section. This last include all cesarean sections:
women who succeed to achieve active phase of labor,
but due to other medical issues (loss of maternal-fetal
wellbeing or pelvic-fetal disproportion) underwent
cesarean section and those who did not reach active
phase of labor.
Table 1: Patients’ obstetrical and clinical variables. Mean
(std).
Obstetric variables
Mean ± std
Maternal age (years)
31.7 ± 4.6
BMI (kg/m
2
)
28.9 ± 4.1
Bishop
1.4 ± 0.7
Active phase of labor
63/72 (87.5%)
Vaginal delivery
52/72 (72.2%)
>24h
26/52 (50%)
<=24h
26/52 (50%)
Cesareans
20/72 (27.8%)
Figure 2 shows a representative EHG recording
from an induced woman who reached active phase of
labor and vaginal delivery within 24 hours after
induction onset. Comparing the characteristics of the
EHG-bursts recorded before drug administration
(basal period) and those presented at the last
recording hour, EHG-bursts after 4 hours from
induction onset were of higher amplitude, shorter
duration than those at basal period. Moreover the PSD
analysis revealed a shift of the energy content toward
BIOSIGNALS 2018 - 11th International Conference on Bio-inspired Systems and Signal Processing
72
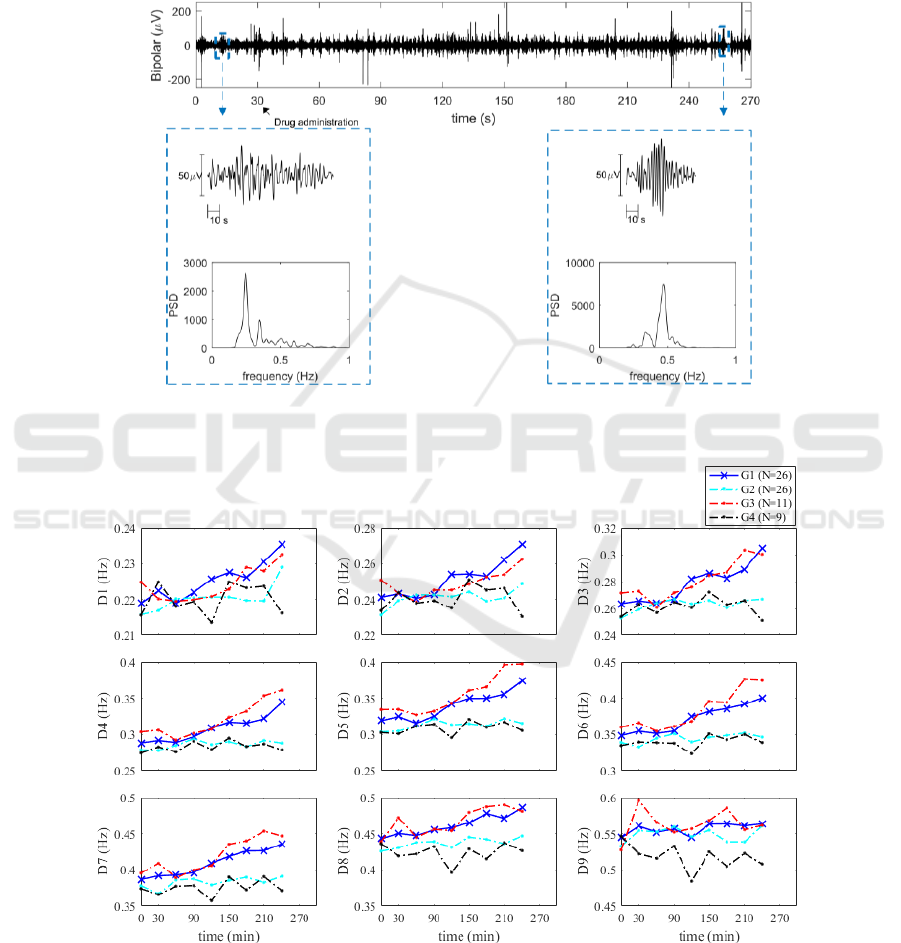
higher frequencies as labor induction progresses.
Figure 3 shows the temporal evolution of the
deciles’ mean values for the groups G1, G2, G3 and
G4. Increasing tendencies can be noticed in all deciles
for G1 and G3 groups except for D9. This reveals that
there is a clear shift toward higher frequencies for the
group of women that are closer to vaginal delivery
and for women delivering by a cesarean section but
achieving active phase of labor (G1 and G3
respectively). While for the group that is further away
from vaginal delivery (G2) and the group of women
that failed in reaching active phase of labor (G4),
there is not a clear tendency in any decile, remaining
almost constant throughout the recording session.
Figure 2: EHG recordings from a woman that reached active labor period and vaginal delivery within 24 hours from labor
induction onset.
Figure 3: Deciles’ temporal evolution for the groups: G1: vaginal delivery within 24 hours after induction onset, G2 vaginal
delivery> 24 hours after induction onset, G3: cesarean section after achieving active phase of labor, G4: cesarean section
without achieving active phase of labor.
Feasibility of Labor Induction Success Prediction based on Uterine Myoelectric Activity Spectral Analysis
73
In order to study the different situations derived
from labor induction, and to analyze the capacity of
the deciles derived from EHG bursts’ PSD to
discriminate between success and failure groups in
each scenario, statistical Mann-Whitney test was
performed for each scenario (Tables 2-4).
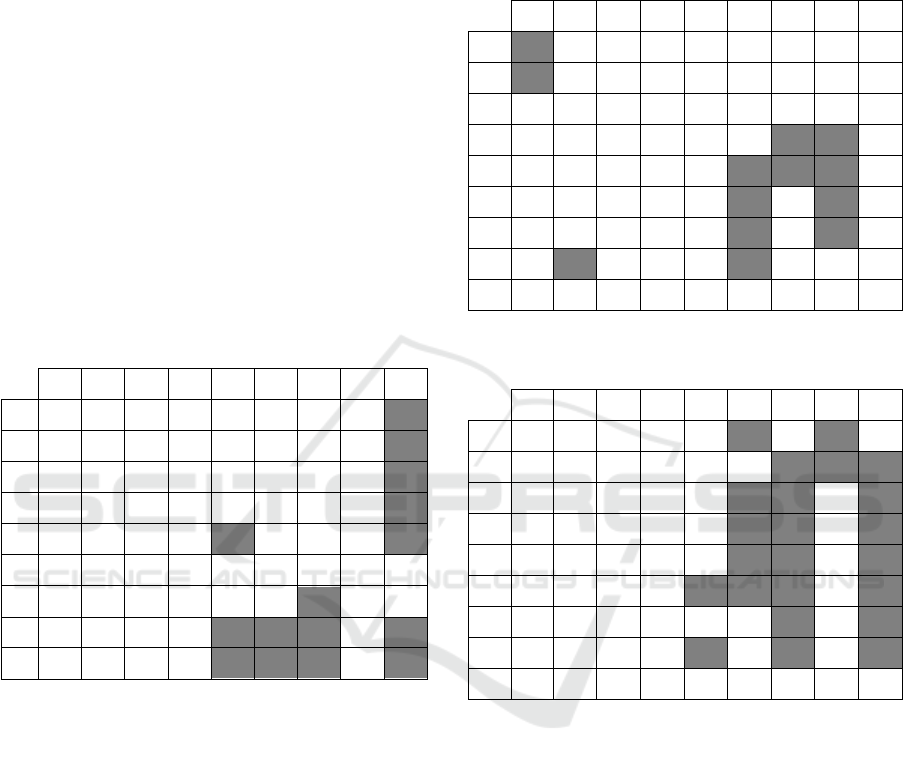
Table 2 shows the statistical significance for each
30-minute analysis interval when comparing the EHG
parameters of women that succeed in achieving active
phase of labor (S1GS) to those that failed (S1GF). It
can be noticed that all deciles show statistically
significant difference at least in one 30-minute
interval (generally the last) except for D6.
Outstanding results to discriminate between S1GS
and S1GF are found for D8 and D9, both showing
sustained statistical difference after 120 minutes from
drug administration to the last analysis interval
(except for 210’)
Table 2: Statistical differences in scenario 1 (S1GS vs
S1GF). Shaded cells represent p-values <0.05.
0'
30'
60'
90'
120'
150'
180'
210'
240'
D1
0.55
0.29
0.97
0.88
0.05
0.61
0.99
0.94
0.01
D2
0.58
0.51
0.70
0.97
0.11
0.65
0.94
0.77
0.01
D3
0.44
0.77
0.54
0.86
0.24
0.77
0.52
0.66
0.01
D4
0.23
0.78
0.34
0.74
0.14
0.52
0.28
0.31
0.04
D5
0.24
0.25
0.96
0.45
0.04
0.43
0.16
0.30
0.03
D6
0.40
0.80
0.77
0.21
0.06
0.34
0.16
0.32
0.14
D7
0.69
0.41
0.67
0.31
0.07
0.28
0.04
0.51
0.07
D8
0.84
0.20
0.29
0.38
0.01
0.04
0.01
0.25
0.05
D9
0.91
0.12
0.07
0.23
0.01
0.04
0.03
0.20
0.03
Table 3 displays the statistical significance for
each 30-minute analysis interval when comparing the
EHG parameters, from women who achieved active
phase of labor, those of women achieving vaginal
delivery vs those of women that underwent cesarean
section. For this scenario, deciles D3 and D9 are the
only ones that do not show statistical difference in any
analysis interval. The best decile to discriminate
between S2GS and S2GF was D5, showing statistical
differences in intervals 150’-210’.
Table 4 shows the statistical difference of the
EHG parameters of women that achieve vaginal
delivery within 24 hours after labor onset compared
to the rest of labor outcomes. All deciles show
statistical difference at least one analysis interval
except for D9. Deciles D2-D6 and D8 seem to be
potential predictors of the vaginal delivery within 24
hours, since they show statistical differences in at
least 3 analysis intervals, being the best result
obtained for D6.
Table 3: Statistical differences in scenario 2 (S2GS vs
S2GF). Shaded cells represent p-values <0.05.
0'
30'
60'
90'
120'
150'
180'
210'
240'
D1
0.02
0.75
0.85
0.99
0.80
0.99
0.18
0.30
0.95
D2
0.01
0.87
0.72
0.49
0.99
0.86
0.30
0.40
0.95
D3
0.06
0.39
0.62
0.36
0.57
0.41
0.06
0.07
0.97
D4
0.05
0.15
0.73
0.47
0.39
0.18
0.03
0.02
0.59
D5
0.07
0.23
0.54
0.47
0.22
0.03
0.05
0.01
0.55
D6
0.22
0.22
0.75
0.57
0.27
0.05
0.11
0.02
0.39
D7
0.39
0.05
0.95
0.54
0.32
0.02
0.13
0.02
0.55
D8
0.76
0.01
0.88
0.35
0.33
0.05
0.14
0.06
0.87
D9
0.49
0.09
0.93
0.95
0.50
0.53
0.11
0.88
0.82
Table 4: Statistical differences in scenario 3 (S3GS vs
S3GF). Shaded cells represent p-values <0.05.
0'
30'
60'
90'
120'
150'
180'
210'
240'
D1
0.86
0.40
0.55
0.80
0.06
0.03
0.16
0.04
0.07
D2
0.43
1.00
0.83
0.64
0.09
0.25
0.05
0.04
0.01
D3
0.23
0.90
0.76
0.77
0.10
0.03
0.03
0.15
0.01
D4
0.41
0.33
0.43
0.81
0.07
0.04
0.04
0.26
0.00
D5
0.15
0.10
0.98
0.71
0.07
0.04
0.02
0.32
0.01
D6
0.49
0.15
0.77
0.65
0.03
0.05
0.03
0.12
0.02
D7
0.77
0.15
0.80
0.55
0.06
0.13
0.03
0.08
0.03
D8
0.26
0.33
0.48
0.41
0.03
0.26
0.02
0.08
0.02
D9
0.39
0.98
0.75
0.67
0.59
0.34
0.20
0.14
0.14
4 DISCUSSION
In clinical practice, a large percentage of all deliveries
are performed through induction of labor, being one
of the most frequent procedures in obstetrics. In fact,
the number of labor inductions has increased
significantly in recent years (Hamilton et al., 2012).
However, not all inductions end in vaginal delivery,
associated with an increase in the rate of cesarean
sections. The latter may simply be due to the fact that
the uterus is not well prepared for delivery by
presenting an immature cervix or a myometrium
unable to achieve effective synchronous contractions
or any other condition that make vaginal delivery be
inviable (Cunningham et al., 2010). It would be a key
aspect to know, as soon as possible, the outcome of a
BIOSIGNALS 2018 - 11th International Conference on Bio-inspired Systems and Signal Processing
74

labor induction so that clinicians may be able to better
plan deliveries, preventing maternal and fetal stress
which can appear in this long process.
Spectral parameters from EHG have been
extracted and used wideley in intention to predict
preterm labor (Buhimschi et al, 1997; Leman et al,
1999; Alamedine et al, 2013; Fergus et al., 2013;
Alamedine et al., 2014). Nonetheless, the
applicability of EHG during induction of labor or its
ability to predict the outcome to be obtained from
induction has not been thoroughly explored.
In this study, it was analyzed the response of
uterine muscle electrical activity to labor induction
drugs. The results of this work indicate that patients
from G1 and G3 experimented an evident shift of
their energy content toward higher frequencies
throughout the recording session (increasing
tendencies are seen in all deciles). This is consistent
with the literature which points out that agents for the
stimulation of uterine activity, act favoring the
increase of cell junctions (gap junction) and the ratio
of cells’ excitability (Garfield and Maner, 2007)
which is related with the presence of more intense
contractions and with higher frequency components.
Moreover, this increment is consistent with another
study in which was found that decil D8 experienced
an increment in its values from pregnancy to labor
(Alamedine et al., 2014).
In contrast, the group that did not reach active
phase of labor (G4) did not exhibit clear trends in any
decile, that is, no spectral displacement was observed
during the first four hours after labor induction onset.
Nevertheless, the same phenomenon was observed
for women that delivered in more than 24 hours after
induction onset. This result may suggest that more
recording time will be needed to observe the shift of
the EHG-Bursts spectral content towards higher
frequencies for women with a relatively slow
response to labor induction drugs.
Our work confirms the utility of decile parameters
to characterize the electrophysiological response of
the uterus to labor induction drugs, and points to the
possibility of predicting the different outcome of the
labor induction by analyzing the EHG-Bursts during
the first 4 hours after induction onset. D8 and D9
show statistical difference between women achieving
active phase of labor to those that failed after 120
minutes from labor induction onset to end of the
recording session except for the time interval 210’.
Then for women who achieved active phase of labor,
D5 could be useful, to discriminate between vaginal
deliveries and cesarean section in the time intervals
150’-210’. Finally, D2-D6 showed statistical
difference between vaginal deliveries within 24 hours
and the rest of women under study, being D6 the one
with best results and showing statistically significant
difference in the time intervals 120’-240’ (except for
210’). Moreover, the time required to observe
statistical significant differences in EHG spectral
parameters between women achieving active phase of
labor to those that failed (S1) is consistent with
pharmacokinetics studies: literature reported that the
time to reach sustained uterine dynamics was 106 and
127 minutes after misoprostol and dinoprostone
vaginal administration respectively (Yount and
Lassiter, 2013).
Although it has been shown that EHG spectral
parameters contain relevant information for
predicting labor induction outcomes, this study is not
exempt of limitations. First, a larger database is
needed to corroborate these results. Second, the
prediction of labor induction success remains a
challenge from the scientific-technical point of view.
Vaginal delivery> 24 h presents a similar trend to the
non-PAP group during the first 4 hours of recording,
which makes it necessary to extend the recording time
in order to be able to predict more accurately whether
a woman is going to reach active phase of labor or
not. On the other hand, the EHG record only contains
information of the myoelectric uterine activity, and
there are multiple causes, such as loss of maternal-
fetal wellbeing or pelvic-fetal disproportion, that
could lead to cesarean delivery that are not necessary
reflected in the EHG recording. In this sense, the use
of EHG recording together with other obstetric
parameters (bishop score, cervical length, maternal
age, birth weight, etc) could improve prediction
accuracy of induction success. In addition, the
application of advanced pattern identification
techniques such as neural networks and/or support
vector machines could be another key point for
developing new tools for predicting labor induction
success that could help obstetric clinicians in labor
management. .
5 CONCLUSION
To conclude, EHG can provide relevant information
about the uterine myoelectrical state through labor
induction. A clear shift of the EHG-Bursts energy
content toward higher frequencies was identified in
the temporal evolution of G1 (vaginal delivery within
24 hours after induction onset) and G3 (cesarean
section after achieving active phase of labor) groups
for all deciles. In contrast, non-remarkable changes in
the spectral characteristics of the EHG were seen for
G2 (vaginal delivery> 24 hours after induction onset)
Feasibility of Labor Induction Success Prediction based on Uterine Myoelectric Activity Spectral Analysis
75

and G4 (cesarean section without achieving active
phase of labor) during the first four hours after labor
onset. Moreover, deciles of the EHG-Bursts’ PSD are
potentially useful to discriminate between the
different outcomes of the labor induction, suggesting
the feasibility of EHG recording for predicting labor
induction success.
ACKNOWLEDGEMENTS
This work was supported in part by the the Ministry
of Economy and Competitiveness and the European
Regional Development Fund (DPI2015-68397-R).
REFERENCES
Alamedine, D. et al. (2014) ‘Selection algorithm for
parameters to characterize uterine EHG signals for the
detection of preterm labor’, Signal, Image and Video
Processing, 8(6), pp. 1169–1178. doi: 10.1007/s11760-
014-0655-2.
Alamedine, D., Khalil, M. and Marque, C. (2013)
‘Comparison of Different EHG Feature Selection
Methods for the Detection of Preterm Labor’,
Computational and Mathematical Methods in
Medicine, 2013, pp. 1–9. doi: 10.1155/2013/485684.
Alberola-Rubio, J. et al. (2013) ‘Comparison of non-
invasive electrohysterographic recording techniques for
monitoring uterine dynamics’, Medical Engineering
and Physics, 35, pp. 1736–1743. doi:
10.1016/j.medengphy.2013.07.008.
Aviram, A. et al. (2014) ‘Effect of Prostaglandin E2 on
Myometrial Electrical Activity in Women Undergoing
Induction of Labor’, J Perinatol, 31, pp. 413–418. doi:
10.1055/s-0033-1352486.
Baños, N. et al. (2015) ‘Definition of Failed Induction of
Labor and Its Predictive Factors: Two Unsolved Issues
of an Everyday Clinical Situation’, Fetal Diagn Ther,
38, pp. 161–169. doi: 10.1159/000433429.
Bastani, P. et al. (2011) ‘Transvaginal ultrasonography
compared with Bishop score for predicting cesarean
section after induction of labor’, International Journal
of Women’s Health, 3, pp. 277–280. doi:
10.2147/IJWH.S20387.
Benalcazar-Parra, C. et al. (2017) ‘Characterization of
Uterine Response to Misoprostol based on
Electrohysterogram’, in Proceedings of the 10th
International Joint Conference on Biomedical
Engineering Systems and Technologies. SCITEPRESS
- Science and Technology Publications, pp. 64–69. doi:
10.5220/0006146700640069.
Bishop, E. H. (1964) ‘Pelvic Scoring For Elective
Induction’, Obstetrics and gynecology, 24, pp. 266–8.
Available at:
http://www.ncbi.nlm.nih.gov/pubmed/14199536
(Accessed: 6 June 2017).
Buhimschi, C., Boyle, M. B. and Garfield, R. E. (1997)
‘Electrical activity of the human uterus during
pregnancy as recorded from the abdominal surface’,
Obstetrics & Gynecology, 90(1), pp. 102–111. doi:
10.1016/S0029-7844(97)83837-9.
Catherine Tolcher, M. et al. (2015) ‘Predicting Cesarean
Delivery After Induction of Labor Among Nulliparous
Women at Term’, Obstet Gynecol, 126(5), pp. 1059–
1068. doi: 10.1097/AOG.0000000000001083.
Crane, J. M. G. et al. (2004) ‘Predictors of successful labor
induction with oral or vaginal misoprostol’, The
Journal of Maternal-Fetal & Neonatal
MedicineOnline) Journal, 15(5), pp. 319–323. doi:
10.1080/14767050410001702195.
Cunningham, F. G. et al. (2010) Williams Obstetrics. 23rd
edn. McGraw-Hill Professional.
Euliano, T. Y. et al. (2013) ‘Monitoring uterine activity
during labor: A comparison of 3 methods’, American
Journal of Obstetrics and Gynecology, 208(1), p. 66.e1-
66.e6. doi: 10.1016/j.ajog.2012.10.873.
Fele-Zorz, G. et al. (2008) ‘A comparison of various linear
and non-linear signal processing techniques to separate
uterine EMG records of term and pre-term delivery
groups’, Med Biol Eng Comput, 46, pp. 911–922. doi:
10.1007/s11517-008-0350-y.
Fergus, P. et al. (2013) ‘Prediction of Preterm Deliveries
from EHG Signals Using Machine Learning’, PLoS
ONE, 8(10). doi: 10.1371/journal.pone.0077154.
Filho, O. B. M., Albuquerque, R. M. and Cecatti, J. G.
(2010) ‘A randomized controlled trial comparing
vaginal misoprostol versus Foley catheter plus oxytocin
for labor induction’, Acta Obstetricia et Gynecologica
Scandinavica. Blackwell Publishing Ltd, 89(8), pp.
1045–1052. doi: 10.3109/00016349.2010.499447.
Garcia-Simon, R. et al. (2016) ‘Economic implications of
labor induction’, International Journal of Gynecology
& Obstetrics, 133(1), pp. 112–115. doi:
10.1016/j.ijgo.2015.08.022.
Garfield, R. E. and Maner, W. L. (2007) ‘Physiology and
electrical activity of uterine contractions’, Seminars in
Cell & Developmental Biology, 18, pp. 289–295. doi:
10.1016/j.semcdb.2007.05.004.
Gilstrop, M. and Sciscione, A. (2015) ‘Induction of labor—
Pharmacology methods’, Seminars in Perinatology, 39,
pp. 463–465. doi: 10.1053/j.semperi.2015.07.009.
Hamilton, B. et al. (2012) Births: Final data for 2012.
Hyattsville. Available at: www.cdc.gov/
nchs/data/nvsr/nvsr62/nvsr62 09.pdf.
Indraccolo, U., Scutiero, G. and Greco, P. (2016)
‘Sonographic Cervical Shortening after Labor
Induction is a Predictor of Vaginal Delivery’, Revista
Brasileira de Ginecologia e Obstetrícia. Federação
Brasileira das Sociedades de Ginecologia e Obstetrícia,
38(12), pp. 585–588. doi: 10.1055/s-0036-1597629.
Leman, H., Marque, C. and Gondry, J. (1999) ‘Use of the
electrohysterogram signal for characterization of
contractions during pregnancy’, IEEE Transactions on
BIOSIGNALS 2018 - 11th International Conference on Bio-inspired Systems and Signal Processing
76

Biomedical Engineering, 46(10), pp. 1222–1229. doi:
10.1109/10.790499.
Marque, C. et al. (1986) ‘Uterine EHG Processing for
Obstetrical Monitorng’, IEEE Transactions on
Biomedical Engineering, BME-33(12), pp. 1182–1187.
doi: 10.1109/TBME.1986.325698.
Pandis, G. K. et al. (2001) ‘Preinduction sonographic
measurement of cervical length in the prediction of
successful induction of labor’, Ultrasound in Obstetrics
and Gynecology. Blackwell Science Ltd., 18(6), pp.
623–628. doi: 10.1046/j.0960-7692.2001.00580.x.
Pitarello, P. da R. P. et al. (2013) ‘Prediction of successful
labor induction using transvaginal sonographic cervical
measurements’, Journal of Clinical Ultrasound. Wiley
Subscription Services, Inc., A Wiley Company, 41(2),
pp. 76–83. doi: 10.1002/jcu.21929.
Prado, C. A. de C. et al. (2016) ‘Predicting success of labor
induction in singleton term pregnancies by combining
maternal and ultrasound variables.’, The journal of
maternal-fetal & neonatal medicine : the official
journal of the European Association of Perinatal
Medicine, the Federation of Asia and Oceania
Perinatal Societies, the International Society of
Perinatal Obstetricians, pp. 1–35. doi:
10.3109/14767058.2015.1135124.
Seyb, S. T. et al. (1999) ‘Risk of cesarean delivery with
elective induction of labor at term in nulliparous
women.’, Obstetrics and gynecology, 94(4), pp. 600–7.
Available at:
http://www.ncbi.nlm.nih.gov/pubmed/10511367
(Accessed: 15 September 2016).
Tibor Toth (2005) ‘Transcutaneous Electromyography of
Uterus in Prediction of Labor Outcome Induced by
Oxytocine and Prostaglandine Shapes’, Gynaecologia
et perinatologia: journal for gynaecology,
perinatology, reproductive medicine and ultrasonic
diagnostics, 14(2), pp. 75–76.
Vinken, M. P. G. C. et al. (2009) ‘Accuracy of frequency-
related parameters of the electrohysterogram for
predicting preterm delivery: a review of the literature.’,
Obstetrical & gynecological survey, 64(8), pp. 529–41.
doi: 10.1097/OGX.0b013e3181a8c6b1.
Ware, V. and Raynor, B. D. (2000) ‘Transvaginal
ultrasonographic cervical measurement as a predictor
of successful labor induction’, American Journal of
Obstetrics and Gynecology, 182(5), pp. 1030–1032.
doi: 10.1067/mob.2000.105399.
Yount, S. M. and Lassiter, N. (2013) ‘The Pharmacology of
Prostaglandins for Induction of Labor’, Journal of
Midwifery and Women’s Health, 58(2), pp. 133–144.
doi: 10.1111/jmwh.12022.
Feasibility of Labor Induction Success Prediction based on Uterine Myoelectric Activity Spectral Analysis
77
