
Analysis Social Determinant of Adherence to Treatment in
Pulmonary Tuberculosis Patients in Medan City
Fazidah A. Siregar
1
, Lita Sri Andayani
1
1
Faculty of Public Health, University of Sumatera Utara, Medan, 20155, North Sumatera, Indonesia
{fazidah, lita.andayani}@ usu.ac.id
Keywords: Social Determinant, Treatment Adherence, Pulmonary Tuberculosis.
Abstract: Tuberculosis a major public health problems in Medan. The incidence of tuberculosis remains high and cure
rate below the target (74.02%). While non-adherence to tuberculosis treatment is still high and impact on high
risk of transmission and thereby increasing number of tuberculosis cases. This study investigated factors
associated with non-adherence to tuberculosis treatment, including social factors. The study was a case control
study with total number of study recruits was 105 at a case: control ratio of 1:2. Data was performed using
simple and multiple logistic regressions. The results showed that history of prior treatment, low education
level, lack of social support, and poor knowledge were determinant factors for non-adherence to tuberculosis
treatment in Medan. Based on these findings, it was recommended to enhance health education regarding
tuberculosis treatment as well as provide social support to tuberculosis patients in the treatment period.
1 INTRODUCTION
Tuberculosis (TB) is global health problem and
leading causes of morbidity and mortality world-
wide. World Health Organization (WHO) reported
10.4 millions people are infected with TB with 1.7
million death worldwide in 2016. Majority of TB
cases (75%) found in developing countries
(WHO, 2017). Indonesia is the second highest for TB
cases in the worldwide among 30 high burden
countries and TB is the fourth leading cause of death
after stroke, coronary disease and diabetes. The
incidence of TB is 395 per 100.000 population in
2015 and tend increased in 2016 (WHO, 2016). North
Sumatera Province is the fifth rank for TB cases in
Indonesia with Medan is endemic area with high
incidence of TB (MHI, 2016). According
to Ministry
of health , number of tuberculosis cases in Medan
increased from 5,814 cases in 2014 to 5,861 cases in
2015 ( MDHO, 2015).
TB control program with the Directly Observed
Treatment Short Course Chemotherapy (DOTS)
strategy had been implemented since 1995. This
strategy consists of five components and one of the
most important component was existence of effective
TB drug with the short time as well as presence of
supervisors taking medication to ensure patient's
adherence to treatment. Unfortunately, non-
adherence to treatment still a problem in TB patient's
treatment in Medan. This could affect on the risk of
TB transmission and thereby increasing the incidence
of new cases and also the Multidrugs Resistant
Tuberculosis (MDR-TB) cases. WHO estimated there
are 490000 people with MDR-TB worldwide in 2016
(WHO, 2017).
Many studies found that factors associated with
non-adherence to tuberculosis treatment are poor
knowledge, low education level, low socioeconomic,
behavior, stigma, lack of social support, adverse drug
reaction, history of prior treatment, lack of access to
health facility, availability of TB drug, health worker
attitude,etc (Tang Y, 2015 ; Xu W, 2009; Bam T,
2006; Kaona F, 2004)
Medan is endemic area for TB cases with high
incidence. Many efforts had been conducted,
however incidence of tuberculosis remains high.
Furthermore, cure rate below the national target and
non-adherence rate in tuberculosis treatment still
high. In designing an effective strategies for control
tuberculosis and prevent MDR-TB, is necessary to
identify factors associated with non-adherence to
treatment to reduce number of new tuberculosis cases
due to treatment failure. Therefore, this study was
undertaken to get information regarding factors
associated with non-adherence to tuberculosis
treatment to assist health professional to develop an
effective TB control strategies.
942
Siregar, F. and Andayani, L.
Analysis Social Determinant of Adherence to Treatment in Pulmonary Tuberculosis Patients in Medan City.
DOI: 10.5220/0010104709420945
In Proceedings of the International Conference of Science, Technology, Engineering, Environmental and Ramification Researches (ICOSTEERR 2018) - Research in Industry 4.0, pages
942-945
ISBN: 978-989-758-449-7
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
2 METHODS
This study was conducted from 2th June, 2018 to 31th
July, 2018 in six health facilities in Medan City that
have non-adherence patients to tuberculosis treatment
including Medan Area Health facility, Medan
Tembung Health facility, Padang Bulan Health
facility, Helvetia Health facility, Petisah Health
facility and Teladan Health facility.
2.1 Sample
This study was designed as unmatched case control
study. Cases were patients who compliance to
tuberculosis treatments and control were patients who
not compliance to tuberculosis treatments that
registered as TB patients in six health facilities.
2.2 Sample Size
Sample consist of 35 tuberculosis patients who non-
adherence to treatment and 70 tuberculosis patients
who adherence to tuberculosis treatment. Therefore,
the total number of study recruits was 105 at a case:
control ratio of 1:2.
2.3 Study Instruments
The socio-demographic data as well as knowledge,
social support were collected by interview and
recorded using questionnaires administered by the
researchers that were developed based on
questionnaires published research ((Tang Y, 2015 ;
Xu W, 2009; Bam T, 2006; Kaona F, 2004). The
socio-demographic factors included age, sex,
ethnicity, education level, and income. Income
evaluation was performed using the minimum wage
standard of Medan city. Knowledge was assessed via
thirty three questions regarding cause, symptoms,
prevention, drugs and treatment. These questions
could be answered with yes (scoring 1 point) and no
or do not know (scoring 0 points). Knowledge was
classified as good when 70% or more of the answers
were correct and low when less than 70% of the
answers were correct. For social support was assessed
via five questions regarding family support in taking
medicine, nutritional, financial support and sputum
smear examination. Then, the results were classified
using a similar range as for the classification of
knowledge.
2.4 Stastical Analysis
Data analysis was performed using the Statistical
Package for Social Science (SPSS) Release 22.0
program. To determine risk factor associated with
non-adherence to tuberculosis treatment by using
Simple and multiple logistic regressions.
3 RESULTS AND DISCUSSION
3.1 Results
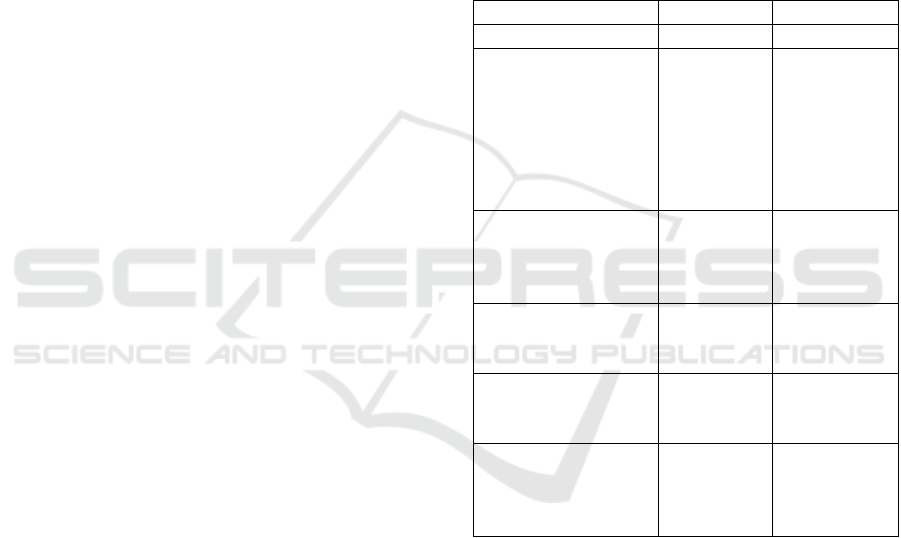
Table 1: Socio-demoghraphic characteristic of respondents.
Characteristic No %
Age 42.7 15.95
Ethnicity
Javanese
Batakish
Mandailing
Malaya
Minangnese
Others
34
30
16
6
14
5
32.4
28.6
15.2
5.7
13.3
4.8
Marital status
Single
Married
Widow
65
32
8
61.9
30.5
7.6
Education
High
Low
64
41
61
39
Income
≥ 2.5 million
< 2.5 million
38
67
36.2
63.8
History of TB
treatment
New cases
Retreated cases
84
21
80.0
20.0
A total of 105 samples were included in this study and
consisted of 35 TB patients non- adherence to
treatment and 70 TB patients with adherence to
treatment. The mean (SD) of sample was 42.17
(15.95) years. The Majority were Javanese (32.4%)
and married (61.9%). They had new treatment
(80%),had high education (61.0%) and came from
huseholds with a monthly income less than minimum
wages (63.8%) (Tabel 1). Based on the social risk
factors, majority of respondent have poor knowledge
(59%) and have social support (79.0%) (Tabel 2).
Analysis Social Determinant of Adherence to Treatment in Pulmonary Tuberculosis Patients in Medan City
943
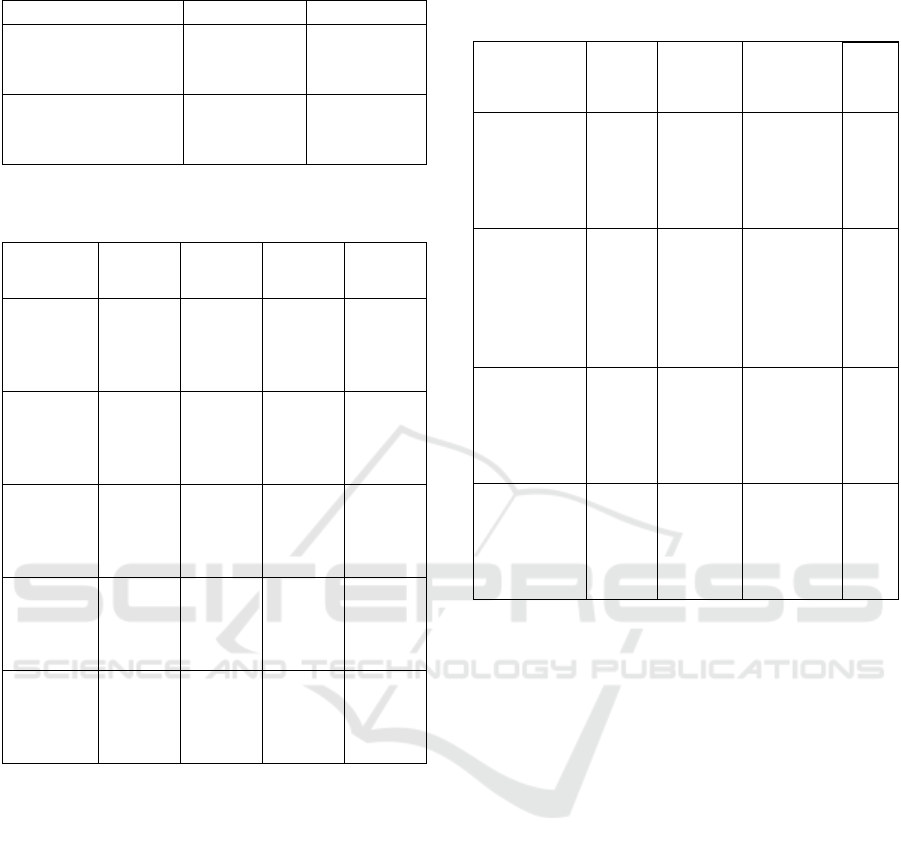
Table 2: The social risk factor of respondents.
Characteristic No %
Knowledge
Good
Poor
43
62
41
59
Social support
Good
Poor
83
22
79
21
Table 3. Factors associated with non-adherence to treatment
in TB patients in Medan Using Simple Logistic Regression.
Variable Cases
n(%)
Control
n(%)
Crude
OR
(95%CI)
p value
Education
High
Low
16 (45,7)
19 (54,3)
48 (68,6)
22 (31,4)
2,591
(1,124;5,
970)
0,04
Income
>=2,5
million
< 2,5
million
12 (34,3)
23 (65,7)
26 (37,1)
44 (62,9)
1,133
(0,484;2,
649)
0,943
History of
Treatment
New
Retreated
17 (48.6)
18 (51.4)
67 (95.7)
3 (4.3)
23,647
(6,235;89,
69)
0,0001
Knowledge
Good
Poor
4 (11,4)
31 (88,6)
39 (55,7)
31 (44,3)
9,750
3,109;30,5
81)
0,0001
Social
support
Good
Bad
21 (60)
14 (40)
62 (88,6)
8 (11,4)
5,167
(1,901;1
4,04)
0,002
The results of our simple logistic regression
revealed the significant variables with p- values less
than 0.25 such as education, history of prior
treatment, social support and knowledge (Table 3).
These significant variables were included in our
multiple logistic regression and with the forward
method revealed four significant variables with p-
values less than 0.5 (Table 4). Therefore, history of
prior treatment, low education , poor knowledge and
social support were risk factors non-adherence to
treatment in TB patients.
Table 4: Factors associated with non-adherence to
treatment in TB patients in Medan Using Multiple Logistic
Regression.
Variable Cases
n(%)
Control
n(%)
Adjusted
OR
(95%CI)
p
val
ue
Education
High
Low
16
(45,7)
19
(54,3)
48
(68,6)
22
(31,4)
8.978
(1.739;
46.348)
0,00
9
History of
prior
Treatment
New
Retreated
17
(48.6)
18 (
51.4)
67
(95.7)
3 (4.3)
107.390
(12.698;9
08.193)
0,00
0
Knowledg
e
Good
Poor
4
(11,4)
31
(88,6)
39
(55,7)
31
(44,3)
8.184
(1.496;44
,761)
0,01
5
Social
support
Good
Bad
21
(60)
14
(40)
62
(88,6)
8 (11,4)
8.540
(1.559
;46.786)
0.01
3
3.2 Discussion
The current study revealed that non-adherence was
still high in Medan City. Some previous studies
revealed that low treatment adherence among TB
patients (Zhou C, 2012 ; Hu D, 2008). A study in
Jiangsu Province in China found that 12.2% of
patients missed at least 10% of their prescribed doses
of anti-TB medication ( Xu W, 2009). The similar
findings by Kaona study in Zambia and
Erawatyningsih study in Subdistrict of Woga in West
Nusa Tenggara found that lack of knowledge leading
to non-adherence to treatment ( Kaona F, 2004 ;
Erawatyningsih, 2009). Lack of knowledge regarding
tuberculosis prevention measures could affect
someone on the risk of tuberculosis infection. This
situation could be a problem in TB control strategy
and thus need more attention.
Low education could influence the ability of
person in receiving information, thus it could affect
the level of understanding about pulmonary TB
disease, prevention and treatment. In the present
study, low education was associated with non-
adherence and had a risk of 8.9 times to non-
adherence compared to high education. This is
consistent to a study in Subdistrict of Woga in West
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
944

Nusa tenggara found that low education was
associated with non-adherence to treatment
(Erawatyningsih, 2009). Likewise, Xu W study In
Jiangsu Province in China found that illiteracy was
associated and have risk of 2.42 to non-adherence of
treatment ( Xu W, 2009).
The role of family support on treatment successes
had been studied. Family support increases patients
compliance with taking medicine. In this study lack
of social support was associated with non-adherence
and have a risk of 8.540 times to non-adherence. This
is consistent to Than Ying study in Shenzen, China
found that social support was associated with non-
adherence ( Tang Y, 2015).
4 CONCLUSIONS
This study found that non-adherence to treatment
among pulmonary TB patients is still problem in TB
control program in Medan and are influenced by
many factors such as low education, poor knowledge,
history of treatment as well as lack of social support.
Poor knowledge about anti-TB treatment could
impact on non-adherence to TB treatment, so is
crucial to improve knowledge of patients about
pulmonary TB treatment. Moreover, social support
by family and health workers is necessary.
ACKNOWLEDGEMENTS
We are grateful to Rector University of Sumatera
Utara that supported this study. Thanks also for head
of district health office and head of health facility for
their assistance and for all people who were involved
in this study.
REFERENCES
Erawatyningsih, E., & Purwanta, S. H. 2009. Factors
affecting incompliance with medication among lung
tuberculosis patients. Berita kedokteran masyarakat,
25, 117-124.
Hu D, Liu X, Chen J, Wang Y, Wang T, Zeng W, Smith H,
Garner P. Direct observation and adherence to
tuberculosis treatment in Chongqing, China: a
descriptive study.Health Policy Plan. 2008;23:43–55.
Ministry of Health of Indonesia. 2016. Indonesian Health
Profile. Jakarta 2016.
Medan District Health Office (2015). Tuberculosis case
report in Medan.
Kaona, F. A., Tuba, M., Siziya, S., & Sikaona, L. (2004).
An assessment of factors contributing to treatment
adherence and knowledge of TB transmission among
patients on TB treatment. BMC Public health, 4(1), 68.
Tang, Y., Zhao, M., Wang, Y., Gong, Y., Yin, X., Zhao, A.,
... & Wu, C. (2015). Non-adherence to anti-tuberculosis
treatment among internal migrants with pulmonary
tuberculosis in Shenzhen, China: a cross-sectional
study. BMC public health, 15(1), 474.
World Health Organization (WHO). Global Tuberculosis
Report 2017.
http://www.who.int/tb/publications/global_report/en/.
World Health Organization (WHO).2016. Global
Tuberculosis Report 2015.
http://www.who.int/tb/publications/global_report/en/.
Xu, W., Lu, W., Zhou, Y., Zhu, L., Shen, H., & Wang, J.
(2009). Adherence to anti-tuberculosis treatment
among pulmonary tuberculosis patients: a qualitative
and quantitative study. BMC health services research,
9(1), 169.
Zhou C, Chu J, Liu J, Gai Tobe R, Gen H, Wang X, Zheng
W, Xu L. Adherence totuberculosis treatment among
migrant pulmonary tuberculosis patients in Shandong,
China: a quantitative survey study. PloS one. 2012;7,
e52334.
Bam, T. S., Gunneberg, C., Chamroonsawasdi, K., Bam, D.
S., Aalberg, O., Kasland, O., &Srisorrachatr, S. 2006.
Factors affecting patient adherence to DOTS in urban
Kathmandu, Nepal. The International Journal of
Tuberculosis and Lung Disease, 10(3), 270-276.
Analysis Social Determinant of Adherence to Treatment in Pulmonary Tuberculosis Patients in Medan City
945
