
Review of Intracranial Meningioma in North Sumatera
Ridha Dharmajaya
1
1
Department of Neurosurgery, Universitas Sumatera Utara, Medan, Indonesia
Keyword: Intracranial Meningioma, North Sumatera.
Abstract: Meningioma, also known as meningeal tumor, is typically a slow-growing tumor that forms from the
meninges, the membranous layers surrounding the brain and spinal cord. Risk factors include exposure to
ionizing radiation such as during radiation therapy, a family history of the condition, and neurofibromatosis
type 2. The goal of management strategy in meningiomas is to keep the patient fully functional and provide
long-term relief or prevent intracranial tumor growth associated problems.
1 INTRODUCTION
Meningiomas has attracted the attention of surgeons,
anatomists, pathologists, and physicians for many
centuries. Given the tendency of these neoplasms to
cause thickening of the overlying calvarium,
meningiomas have left an unmistakable mark on
human skulls dated as far back as prehistoric times.
Harvey Cushing coined the term meningioma in 1922
to describe a benign neoplasm of the meninges of the
brain.
However, many other surgeons and
pathologists described and named this neoplasm as
well. In fact, naming of the tumor likely represents
one of the most frequently changed nomenclatures in
the history of medicine. Antoine Louis, born in Metz,
France, in 1723 into a family of surgeons, developed
an interest in surgery of dural tumors, which he
named tumeurs fongueuses de la duremere or fungoid
tumors of the dura mater. He included their
description in Memoire de l’Académie Royale de
Chirurgie in 1774. In 1854, Sir James Paget named
the neoplasm myeloid tumor (marrow like), based on
its gross appearance and less malignant behavior.
In 1863, Virchow was the first to describe the
granules in these tumors and named it psammoma
(sand-like). As Virchow was uncertain of the origin
of these bodies, he gave the neoplasm a descriptive
name. Subsequently, he changed the nomenclature
from psammoma to Sarkoma der dura mater to
describe these tumors.
Meningioma, also/ known as meninge j liglllsoal
tumor, is typically a slow-growing tumor that forms
from the meninges, the membranous layers
surrounding the brain and spinal cord. Risk factors
include exposure to ionizing radiation such as during
radiation therapy, a family history of the condition,
and neurofibromatosis type 2.
2 PATIENTS AND METHODS
This was a retrospective study carried out at the Haji
Adam Malik General Hospital serve as teaching
hospitals of the University of the Sumatera Utara, The
study was over a period of 6 years ( January 2013 –
December 2017). Haji Adam Malik General Hospital
is located within the city centre in Medan, North
Sumatera as one of the referral hospitals for
Provincial Hospitals in Indonesia.
Consecutive patients seen at the this hospital
with histologically proven intracranial meningioma
during the study period were recruited for the study.
We obtained data from the medical record. Diagnosis
was made after detailed history and careful physical
examination, neuroimaging including CT scan and or
MRI, and histological confirmation. All patients who
underwent neurosurgical operative intervention had
specimens removed at operative intervention and
subjected to histology for a final tissue diagnosis.
Patients who had non-operative intervention were
taken off the study due to the absence of a final
histological diagnosis data.
Dharmajaya, R.
Review of Intracranial Meningioma in North Sumatera.
DOI: 10.5220/0010084706990702
In Proceedings of the International Conference of Science, Technology, Engineering, Environmental and Ramification Researches (ICOSTEERR 2018) - Research in Industry 4.0, pages
699-702
ISBN: 978-989-758-449-7
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
699
3 RESULTS
During the 6 years study period, 171 consecutive
patients (out of 370 patients with primary brain
tumours) seen at Haji Adam Malik General Hospital
had histologically confirmed intracranial
meningioma with a hospital distribution of Frequency
of distribution of intracranial meningiomas among
primary brain tumours.
A total 171 patients records were reviewed,
which were diagnosed by histophatological reports in
the preiod between January 2013 – December 2017
seen in table.1. There were 52 (30.4%) in male
patients and (69.5%) in female patients. The age of
patients range from 1 to 68 years. The highest number
of patients was seen in the age-group of 40-59 years
in males and 20-39 years in females in table 2. The
histopathologic report intracranial meningiomas
based on WHO claasifications showed
Meningothelial meningioma is the most common
histopathology type in 70 patients (40.9%) in table.3.
WHO Grade 1 is the most histological subtypes based
on WHO classifications seen in 131 patients (76.6%).
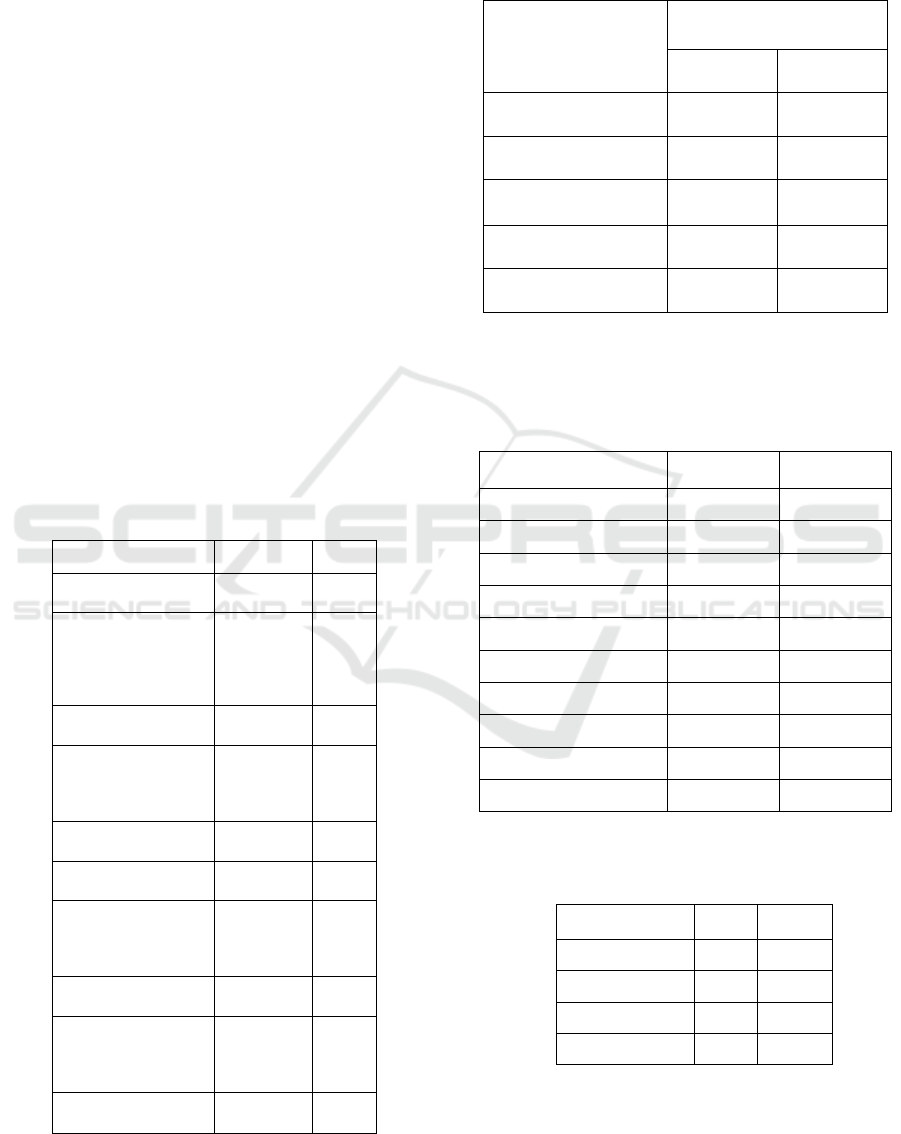
Table 1. Frequency of distribution of intracranial
meningiomas among primary brain tumours
Tumor Types
N %
Meningiomas
171 45.9
Metastatic Brain
tumo
r
76 78,1
Gliomas
59 15.9
Pituitary
21 5.6
Tumor of Nerves
and/ or Nerve
Sheath
17 4.5
PNET
13 3.5
Cysta
6 1.6
Other, more
bening pituitary
tumo
r
5 1.3
Pineal tumor
1 0.2
Other primary
tumors, including
skull
b
ase
1 0.2
Total
370 100.0
Table 2. Age of patients at presentation intracranial
meningiomas
Age Group
Gender
Males Females
0-19 years 4 (7.69%) 18 (15.1%)
20-39 years 12 (23.07%) 40 (33.6%)
40-59 years 21 (40.3%) 32 (26.8%)
> 60 years 15 (28.8%) 29 (24.3%)
Total 52 (30.4%) 119 (69.5%)
Table 3. Histopathology presentation intracranial
meningiomas based on World Health Organization
(WHO) Classification.
Histopathology N %
Meningothelial 70 40.9
Transitional 19 11.1
Fibroblastic 21 12.2
Clear Cell 9 5.2
Anaplastic 12 7.01
Atypical 9 5.2
Malignant 10 5.8
Metaplastic 11 6.4
Psammomatous 10 5.8
Total 171 100.0
Table 4. Distribution of intracranial meningiomas
based on World Health Organization (WHO Grading)
Histopathology N %
WHO Grade 1
131 76.6
WHO Grade 2
18 10.5
WHO Grade 3
22 12.86
Total
171 100.0
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
700

4 CONCLUSION
The goal of management strategy in meningiomas is
to keep the patient fully functional and provide long-
term relief or prevent intracranial tumor growth
associated problems. The clinical picture at
presentation is very variable, and very little is known
regarding the natural history of these tumors;
therefore the management strategy is not universal.
The initial dilemma that the surgeon faces starts with
the decision to treat or not to treat. Only then is this
followed by the decision of how to treat. Both
decisions are taken together with the patient and the
surgeon plays the role of an advisor, rather than
directly deciding for the patient.
Treatment choice in patients who present to
medical attention for the first time with a
symptomatic meningioma or in those with neural
compression is mostly straightforward. The goal is
well defined and the possible gains most commonly
far outweigh the risks. However; decision making is
not so easy in non- or marginally symptomatic
patients, for whom the risks of treatment should be
weighed against the risk of iatrogenic injury. The
mortality and morbidity of surgical treatment
decreased significantly and continuously in the last
century, mainly as a result of the application of
microsurgery, bipolar coagulation, and other new
technologies. A better appreciation of microsurgical
anatomy and increasing use of skull-base surgery
have further improved results. The advent and
popularization of alternative treatment modalities
such as radiation treatment and radiosurgery have
also made significant contributions. Finally, with
accumulating experience and scientific data much
more is known today about the biology of
meningiomas.
Even with all these advances, today’s
neurosurgeon still has very little clinical evidence on
which to base his or her clinical decisions. This
chapter aims to summarize the controversies,
discussing different management paradigms and thus
providing a general guideline for treatment (or
nontreatment) of meningiomas. Five factors influence
the treatment decision in meningiomas: operative
gains, operative risks, tumor biology, mass
effect/symptomatology, and the preference of the
patient. In short, the balance between the risks and
benefits of surgery is evaluated in light of the tumor’s
biology, mass effect/symptomatology, and preference
of the patient.
REFERENCES
Lusis E, Gutmann DH. Meningioma: an update.
Current Opinion in Neurology.
2004;17:687–692.
Campbell BA, Jhamb A, Maguire JA, Toyota B, Ma
R. Meningiomas in 2009: Controversies
and Future Challenges. A J Clin Oncol.
2009;32:73–85.
Drummond KJ, Zhu J, Black PM. Meningiomas:
Updating Basic Science, Management and
Outcome. Neurologist. 2004;10:113–130.
Claus EB, Bondy ML, Schildkraut JM, Wiemels JL,
Wrensch M, Black PM. Epidemiology of
Intracranial Meningioma. Neurosurgery.
2005;57:1088–1095.
Idowu O, Akang EEU, Malomo A. Symptomatic
Primary Intracranial neoplasms in Nigeria,
West Africa. Journal of Neurological
Sciences (Turkish) 2007;24:212–218.
Ohaegbulam SS. Geographical Neurosurgery.
Neurol Res. 1999;21:161–170.
Bondy ML, Ligon BL. Epidemiology and aetiology
of intracranial meningiomas: a review. J
Neurooncol. 1996;29:197–205.
Idowu OE, Apemiye RA. Delay in presentation and
diagnosis of adult primary intracranial
neoplasms in a tropical teaching hospital: A
pilot study. International Journal of
Surgery. 2009;7:396–398.
Wiemels J, Wrensch M, Claus EB. Epidemiology
and etiology of meningioma. J Neurooncol.
2010;99:307–314.
Das A, Chapman CAT, Yap WM. Histological
subtypes of symptomatic central nervous
system tumours in Singapore. J Neurol
Neurosurg Psychiatry. 2000;68:372–374. [
Fynn E, Khan N, Ojo A. Meningioma - a review of
52 cases. SA Journal of Radiology.2004:35.
Gasparetto EL, Leite CC, Lucato LT, Barros CV,
Marie SKN, Santana P, et al. Intracranial
meningiomas: magnetic resonance imaging
findings in 78 cases. Arquivos de Neuro
Psiquiatria. 2007;65:610–614.
Quiñones-Hinojosa A, Kaprealian T, Chaichana KL,
Sanai N, Parsa AT, Berger MS, et al. Pre
Operative Factors Affecting Resectability
of Giant Intracranial Meningiomas. Can J
Neurol Sci. 2009;36:623–630.
Jaggon JR, Char G. Epidemiologic Data on
Meningiomas in Jamaica: The First fro
the Caribbean. The Internet Journal ofThird
World Medicine. 2007;5 doi:
10.5580/1840.
Review of Intracranial Meningioma in North Sumatera
701

Mezue WC, Ohaegbulam SC, Ndubuisi CC, Chikani
MC, Achebe DS. Intracranial meningiomas
managed at Memfys hospital for
neurosurgey in Enugu, Nigeria. J Neurosci
Rural Pract. 2012;3:320–323.
Odebode TO, Akang EE, Shokunbi MT, Malomo
AO, Ogunseyinde AO. Factors influencing
visual and clinical outcome in Nigerian
patients with cranial meningioma. J of
Clinical Neurosciences. 2006;13:649–654.
Haddad G, Al-Mefty O. Meningiomas: An
overview. In: Wilkins RH, Rengachary SS,
editors. Neurosurgery. 2nd ed. New York:
McGraw-Hill; 1998. pp. 833–841.
Al-Mefty O, Abdulrauf S, Haddad GF.
Meningiomas. In: Winn HR, editor.
Youmans Neurological Surgery.
Philadelphia: Elsevier Saunders; 2011. pp.
1426–1449.
Sutherland GR, Florel R, Louw D, et al.
Epidemiology of primary intracranial
neoplasms in Manitoba, Canada. Canadian
J Neurol Sci. 1987;14:586.
Preston-Martin S, Henderson BE, Peterm JM.
Descriptive epidemiology of central
nervous system neoplasm in Los Angeles
Country. Annals NY Acad Sci.
1982;381:202–208.
Preston-Martin S. Descriptive epidemiology of
primary tumours of the brain, cranial nerves
and cranial meninges in Los Angeles
County. Neuroepidemiology. 1989;8:283
295.
Ameli N, Haddadian A, Kamalian N. Incidence of
intracranial tumours in Iran. A survey of
1500 verified cases. Neurosurg Rev.
1979;2:67–71.
Rockhill J, Mrugala M, Chamberlain MC.
Intracranial meningiomas: an overview of
diagnosis and treatment. Neurosurg Focus.
2007;23:E1.
Al-Hadidy AM, Maani WS, Mahafza WS, Al-Najar
MS, Al-Nadii MM. Intracranial
Meningioma. J Med J. 2007;41:37–51.
Longstreth WJJ, Dennis LK, McGuire VM,
Drangsholt MT, Koepsell TD.
Epidemiology of Intracranial Meningioma.
Cancer. 1993;72:639–648.
Al-Mefty O, Heth J. Meningiomas. In: Rengachary
SS, Ellenbogen RG, editors. Principles of
Neurosurgery. 2nd ed. New York: Elsevier
Mosby; 2005. pp. 487–500
Cushing H, Eisenhardt L. Meningiomas: Their
Classification, Regional Behaviour, Life
History and Surgical End Results.
Springfield, IL: Charles C Thomas; 1938.
Louis A. Mémoire sur les Tumeuers Fongueuses de
la Dure-mère.Mem Acad R Chir Paris
1774;5:1–59.
Cushing H. The meningiomas (dural
endotheliomas): their source, and favored
seats of origin. Brain 1922;45:282–316.
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
702
