
The Profile of Behavioral and Psychological Symptoms of Dementia
in Post-stroke Vascular Cognitive Impairment
Fasihah Irfani Fitri, Aldy S. Rambe, Aida Fithrie
Department of Neurology Universitas Sumatera Utara/ Adam Malik General Hospital
Keywords: Behavioral and psychological symptoms of dementia, Vascular cognitive impairment
Abstract: Behavioral are standard features of all types of dementia, irrespective of disease etiology and stage, including
vascular cognitive impairment (VCI). The study aimed to examine the BPSD profile in post-stroke patients
with VCI. This cross-sectional study involved 76 post-stroke patients with vascular cognitive impairment.
The mean age was 57.95±10.54 years old. Thirty patients (39.47%) had at least one symptom of BPSD. The
most common symptom was apathy and indifference (15 patients; 19.7%), followed by depressive and gloomy
mood (13 patients, 17.1%). The least frequently found symptom was a violent force, which was only seen in
2 patients (2.6%). There was no significant difference in BPSD profile between ischemic and hemorrhagic
stroke. BPSD was a common finding in post-stroke VCI, with apathy being the most common symptom. Early
identification may lead to better management and may increase the quality of life.
1 INTRODUCTION
Behavioral and psychological symptoms of dementia
(BPSD), also called neuropsychiatric symptoms
(NPS), are standard features of all types of dementia,
irrespective of disease etiology and disease stage.
[Dillon et al,2013; Gupta et al,2014; Mortbya et
al,2017; Tiel, 2015; Zhang, 2012]. The presence of
BPSD in vascular cognitive impairment (VCI) has a
significant impact on the patient's functional and
cognitive status. [Dillon et al,2013; Gupta M et
al,2014; Tiel, 2015]. BPSD are associated with high
caregiver burden, poor prognosis, and higher rates of
institutionalization and drug therapy; all of which
contribute to an increased social and economic impact
on people with dementia. [Dillon, 2013] Caregivers
of dementia patients report BPSD, especially
symptoms like aggression and screaming, to be the
most difficult problem to cope with.[Gupta, 2014].
BPSD are a heterogeneous group of non-cognitive
symptoms and behaviors and are observed in high
rates across the spectrum from mild cognitive
impairment to dementia. They are among the most
challenging and costly aspects of dementia, and, if
left untreated, are associated with hastened disease
progression, worsened daily functioning, impaired
quality of life, increased health care utilization, and
accelerated placement in residential care, increased
utilization of medical resources, more caregiver
stress, diminished quality of life for the persons with
dementia and their families, and higher economic
burden on the caregivers.[Mortbya, 2017; Zhang,
2017]. Vascular cognitive impairment (VCI) refers to
the entire spectrum of cognitive impairment
occurring as a result of the cerebrovascular disease.
The present concept of VCI encompasses not only
vascular dementia (VaD) but also mixed dementia
and vascular cognitive impairment-no dementia
(VCI-ND). VCI-ND refers to that subgroup of
patients who manifest cognitive deficits resulting
from cerebrovascular disease, but do not meet the
definition of dementia.[Gupta, 2014]. The
management of BPSD has the potential to alleviate
much of the suffering of dementia patients and their
caregivers, so early identification and assessment of
BPSD is an essential part of an evaluation of patients
with cognitive impairment. The present study aimed
to examine the profile of BPSD in post-stroke VCI.
2 METHODS
This cross-sectional study involved 76 post-stroke
patients which were recruited from the Memory
Clinic Neurology Department Adam Malik General
Hospital Medan North Sumatera Indonesia, between
Fitri, F., Rambe, A. and Fithrie, A.
The Profile of Behavioral and Psychological Symptoms of Dementia in Post-stroke Vascular Cognitive Impairment.
DOI: 10.5220/0010078205530556
In Proceedings of the International Conference of Science, Technology, Engineering, Environmental and Ramification Researches (ICOSTEERR 2018) - Research in Industry 4.0, pages
553-556
ISBN: 978-989-758-449-7
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
553
March and June 2018. This study included patients
with a history of stroke for more than three months to
two years, had a minor physical disability, fully
cooperative, speak Bahasa Indonesia fluently, able to
read and write, and gave written consent to be
included in the study. Exclusion criteria were:
subjects with major psychiatric disorders had aphasia
or history of dementia before a stroke. All subjects
underwent neurologic evaluation and cognitive
assessment using Montreal Cognitive Assessment
Indonesian Version (MoCA-INA) and complete
neuropsychological evaluation including assessment
of attention, memory, language, executive function
and visuospatial, as listed in CERAD (Consortium to
Establish a Registry for Alzheimer’s
Disease).(Fillenbaum, 2008; Husein, 2010;
Nasreddin, 2005). The neuropsychiatric symptoms
were evaluated using Abe BPSD Score (ABS) which
assessed 10 symptoms including wandering
in/outside home, eating or toilet problem, delusion or
hallucination, offensive and abusive words, day-night
reversal, excitation and agitation, apathy and
indifference, depressive and gloomy mood, violent
force and high irritability. [Abe, 2015]. All statistical
procedures were performed with SPSS. The Health
Research Ethical Committee Medical Faculty of
Universitas Sumatera Utara/H. Adam Malik General
Hospital approved this study.
3 RESULTS
This study included 76 subjects consisted of 44
(52.9%) males and 32 (47.1%) females. The mean age
was 57.95±10.54 years old. Most of the patients aged
between 51 to 55 years old (26.3%) and had 12 years
of education or finished high school (39.5%). There
were 70 patients (92.1%) with a history of ischemic
stroke and six patients (7.9%) with hemorrhagic
stroke. Most of the patients had a positive history of
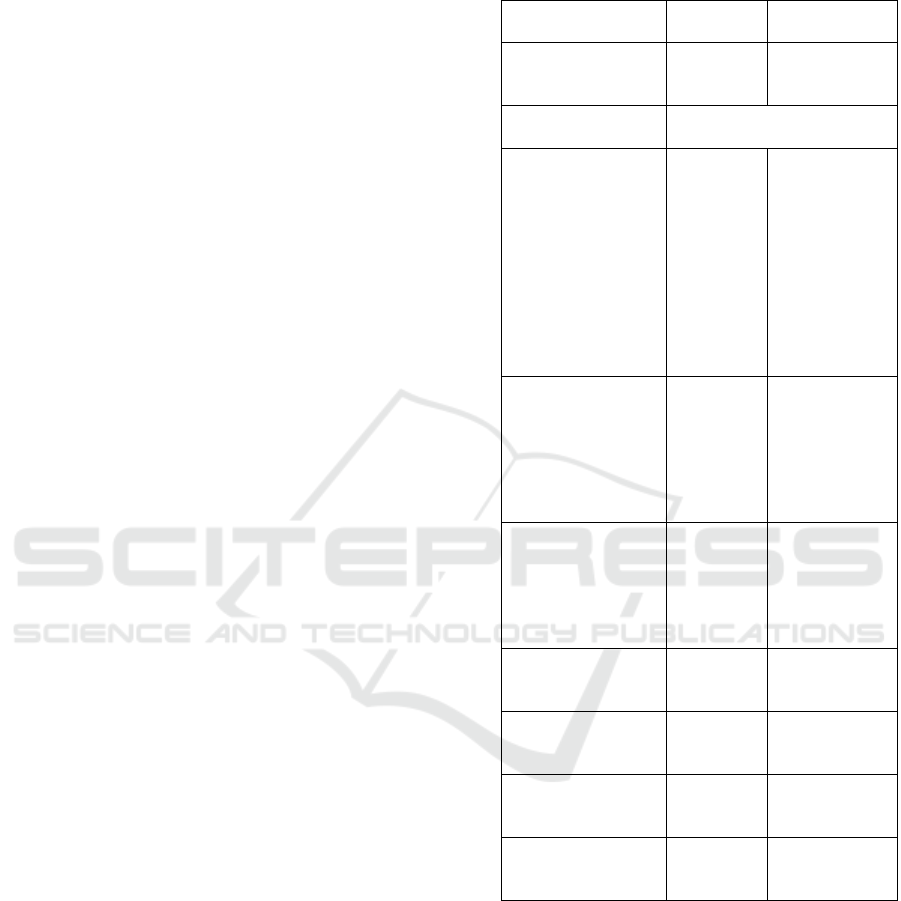
hypertension. Table 1 summarizes the clinical
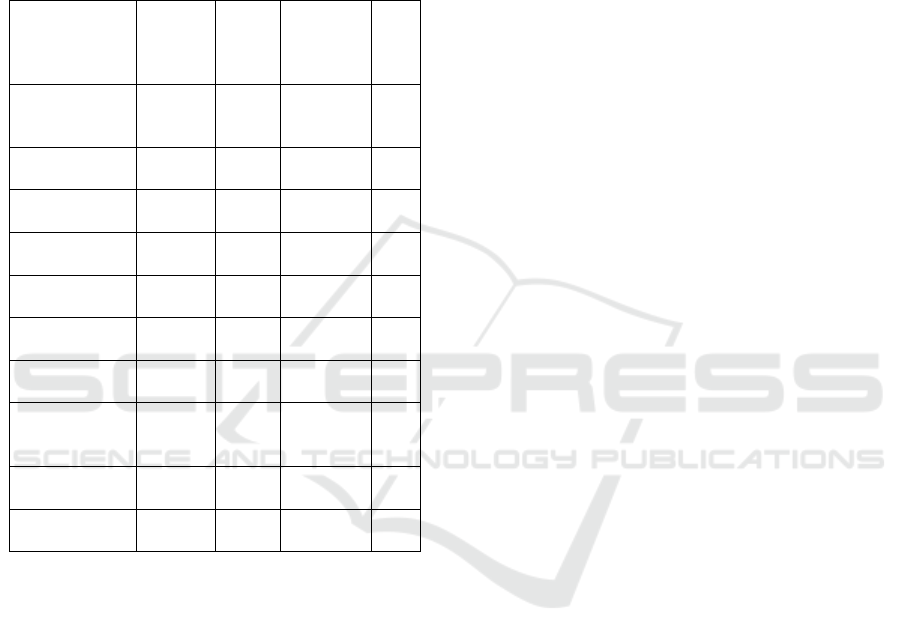
characteristics of the patients.Thirty patients
(39.47%) had at least one of the BPSD symptoms.
The most common symptom was apathy and
indifference (15 patients; 19.7%), followed by
depressive and gloomy mood (13 patients, 17.1%).
The least frequently found symptom was the violent
force, which was found only in 2 patients (2.6%).
There was no significant difference in the frequency
of BPSD symptom between patients with a history of
ischemic and hemorrhagic stroke. Table 2 shows the
frequency of BPSD in both groups.
Table 1. Demographic and Clinical Characteristics of
the Patients
Variables N
(
total 76
)
Percentage
(
%
)
Sex
Male
Female
44
32
52.9
47.1
Age (years), mean ±
SD
57.95±10.541
Age group, years
old
<45
46-50
51-55
56-60
61-65
66-70
71-75
76-80
>80
5
8
20
16
13
5
3
5
1
6.6
10.5
26.3
21.2
17.1
6.6
3.9
6.6
1.3
Educational level
Primary
Junior High
School
High School
Diploma
Universit
y
13
15
30
2
16
17.1
19.7
39.5
2.6
21.1
Occupation
Employee
Housewive
Entrepreneur
Farmer
Unem
p
lo
y
e
d
24
12
19
4
17
31.6
15.8
25.0
5.3
22.4
Stroke Aetiology
Ischemia
Hemorrhage
70
6
92.1
7.9
Hypertension
Yes
No
67
9
88.2
11.8
Diabetes Mellitus
Yes
No
30
46
39.5
60.5
Atrial Fibrillation
Yes
No
2
74
2.6
97.4
4 DISCUSSION
Our data show that BPSD in post-stroke cognitive
impairment was relatively common, occurring in
almost 40% of the patients. This number was lower
than previous studies that reported the occurrence of
BPSD was as high as 95% in VCI and VaD.[Chiu ,
2013;Gupta, 2013; Staekenborg, 2010]. This could
partly be explained by the fact that in our study we
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
554
included all post-stroke patients who had cognitive
impairment and we did not classify the patients based
on the severity of the VCI, nor did we differentiate
patients with VCI-ND from those with VaD. Thus, it
could affect the proportion of patients with BPSD
because the severity and occurrence of BPSD are
different in various stages of dementia.[Huang,
2017;Zhang, 2012].
Table 2. Frequency of BPSD Symptoms
Symptoms Total
(76)
N (%)
Ische
mic
(70)
N
(
%
)
Haemorr
hage (6)
N (%)
P
Wandering
in/outside
home
9
(11.8)
8
(11.4)
1
(16.7)
NS
Eating or toilet
p
roble
m
10
(
13.2
)
9
(
12.9
)
1
(
16.7
)
NS
Delusion or
hallucination
7
(9.2)
7
(10)
0 NS
Offensive and
abusive words
7
(
9.2
)
7
(
10
)
0 NS
Day-night
reversal
10
(
13.2
)
9
(
12.9
)
1
(
16.7
)
NS
Excitation and
agitation
10
(13.2)
10
(14.3)
0 NS
Apathy and
indifference
15
(
19.7
)
13
(
18.6
)
2
(
33.3
)
NS
Depressive
and gloomy
moo
d
13
(17.1)
12
(17.1)
1
(16.7)
NS
Violent force 2
(2.6)
2
(2.9)
0 NS
High
irritabilit
y
6
(
7.9
)
6
(
8.6
)
0 NS
We found apathy and depression were the most
common symptoms of BPSD, and violent force was
the least common symptom. This is consistent with
several previous studies. Gupta. (2014) reported that
depression was the commonest BPSD at 73.3% and
apathy was found in 35% of the cases. Disinhibition
(8%), euphoria, and hallucinations (5% each) were
the least common of the BPSD on the NPI.[Gupta,
2014]. Apathy and depression were the most common
neuropsychiatric manifestation of VCI irrespective of
the subtype and the severity of the disease. A review
of the total of 82 studies which compared several
types of VaD found that apathy and depression also
occurred sometime during the disease. From 13
articles selected in that review, four compared BPSD
in Subcortical Vascular Dementia (SVaD) versus
Cortical-Subcortical Vascular Dementia (CSVaD),
three involved comparisons between SVaD and VCI-
ND, one study analyzed differences between CSVaD
and VCI-ND, while five studies assessed BPSD in
CSVaD. Subcortical and Cortical-Subcortical VaD
were associated predominantly with apathy and
depression. VCI-ND may present fewer behavioral
symptoms than VaD.[Tiel, 2015]. Despite
considerable advances in the detection of brain
vascular-related syndromes in recent years, the
association between vascular lesions and both
cognitive symptoms and BPSD in VCI remains
controversial. For instance, data in the literature
suggests that BPSD may occur in VCI, regardless of
the development of dementia. BPSD may also appear
at any stage, induced by cerebrovascular lesions
disrupting the cortical-subcortical circuits between
prefrontal cortex connections to limbic nuclei of the
basal ganglia and thalamus, and other limbic system
structures. This suggests that better characterization
of vascular-related BPSD, and the underlying
mechanisms of brain injury associated with these
features, is still needed to allow the adoption of
effective evidence-based prophylactic and
therapeutic measures.[Tiel,2015].
Apathy typically occurs following disruption
of circuits linking subregions of the prefrontal cortex
and subcortical structures, such as the basal ganglia,
implicated in reward processing and complex
planning. Clinical definitions of apathy have
distinguished between cognitive and emotional
aspects of goal-directed behavior. Anterior cingulate
atrophy has been associated with reduced initiation
while executive dysfunction has been associated with
the pathology of the dorsolateral prefrontal cortex and
reduced reward sensitivity with underactivation of the
orbitofrontal cortex. [Gallagher, 2017]. Apathy is
known to be common in subcortical ischaemic
vascular disease owing to the occurrence of white
matter lesions and/or lacunar infarcts in the basal
ganglia and thalamus, which lead to interruption of
cortico-subcortical circuits.[Gupta, 2014] Apathy in
the context of VCI has been associated with
‘‘vascular depression’’ and depression with executive
dysfunction. It is important to differentiate apathy
from depression as apathy may occur independently
from depression. In such cases, there is typically a
relative absence of distress and negative cognitions so
commonly observed in depression.[ Gallagher, 2017].
Several mechanisms might link depression,
anxiety, and cognitive decline. Depression has long
been associated with hypercortisolemia, and recurrent
depression has previously been associated with the
reduced hippocampal volume. Cerebrovascular
disease has been particularly associated with
depression in later life and may precipitate and
perpetuate depression via disruption of corticostriatal
The Profile of Behavioral and Psychological Symptoms of Dementia in Post-stroke Vascular Cognitive Impairment
555

tracts necessary for cognitive and emotional
regulation. Increased inflammation, decreased
secretion of trophic factors, and increased oxidative
stress are mechanisms that may link depression and
cognitive decline at a molecular level, while at a
behavioral level, physical inactivity and other adverse
health behaviors have been associated with
accelerated cognitive decline. [Gallagher,2017]
This study has several limitations. First, we did not
classify the patients based on the difference subtype
of post-stroke vascular cognitive impairment, which
may have a different pato-mechanism in causing
cognitive impairment. Second, we did not analyze the
presence of BPSD based on the severity of the
cognitive impairment or the impact on daily life
activities.
5 CONCLUSIONS
In conclusion, BPSD is very common in post-stroke
VCI, with apathy and depression being the most
common symptoms. Early identification and
assessment of BPSD in post-stroke patients may lead
to better management and may increase the quality of
life and lessen the caregivers’ burden.
ACKNOWLEDGEMENTS
Lembaga Penelitian Universitas Sumatera Utara
funds this research according to Kontrak Pelaksanaan
Penelitian TALENTA Universitas Sumatera Utara,
2018. Number: 2590/UN5.1.R/PPM/2018, March,
16
th
, 2018
REFERENCES
Abe, K., Yamashita, T., Hishikawa, N., Ohta, Y., Deguchi,
K., Sato, K et al. 2015 A new simple score (ABS) for
assessing behavioral and psychological symptoms of
dementia, J Neurol Sci
http://dx.doi.org/10.1016/j.jns.2015.01.029
Chiu, PY., Liu, CH., and Tsai, CH. 2007 Neuropsychiatric
manifestations in vascular cognitive impairment
patients with and without dementia Acta Neurologica
Taiwanica 16 (2) pp 86–91
Dillon, C., Serrano, CM., Castro, D., Leguizamon, P.,
Heisecke, SL., Taragano, FE et al. 2013 Behavioral
symptoms related to cognitive
impairment.http://dx.doi.org/10.2147/NDT.S47133
Fillenbaum, GG., Van Belle, G., Morris, JC., Mohs, RC.,
Mirra, SS., Davis, PC et al. 2008 CERAD
(Consortium to Establish a Registry for Alzheimer’s
Disease) The first 20 years Alzheimers Dement 4(2)
pp 96–109 doi:10.1016/j.jalz.2007.08.005.
Gallagher, D., Fischer, CE., Laboni, A. 2017
Neuropsychiatric Symptoms in Mild Cognitive
Impairment: An Update on Prevalence, Mechanisms,
and Clinical Significance The Canadian Journal of
Psychiatry / La Revue Canadienne de Psychiatrie
62(3) pp 161-169 DOI: 10.1177/0706743716648296
Gupta, M., Dasgupta, A., Khwaja, GA., Chowdhury, D.,
Patidar, Y., Batra, A. 2013 The profile of behavioral
and psychological symptoms in vascular cognitive
impairment with and without dementia Ann Indian
Acad Neurol 16(4) pp 599-602 doi: 10.4103/0972-
2327.120488
Gupta, M., Dasgupta, A., Khwaja, GA., Chowdhury, D.,
Patidar, Y., Batra, A. 2014 Behavioural and
Psychological Symptoms in Poststroke Vascular
Cognitive Impairment Behavioral Neurology
http://dx.doi.org/10.1155/2014/430128
Huang, SS., Wang, W., Liao, YC. 2017. Severity, and
prevalence of behavioral and psychological
symptoms among patients of different dementia
stages in Taiwan Arch Clin Psychiatry. 44(4) pp 89-
93
Husein, N., Lumempouw, S., Ramli, Y., Herqutanto. 2010
Uji validity dan reliability Montreal cognitive
assessment versi Indonesia (MoCA-Ina) Untuk
skrining gangguan fungsi kognitif Neurona 27(4) 15-
22
Mortbya, ME., Burnsa, R., Eramudugollaa, R., Ismail, Z.,
Anstey, KJ. 2017 Neuropsychiatric Symptoms and
Cognitive Impairment: Understanding the
Importance of Co-Morbid Symptoms Journal of
Alzheimer’s Disease 59 pp 141–153 DOI
10.3233/JAD-170050
Nasreddine, ZS., Phillips, NA., Bédirian, V., Charbonneau,
S., Whitehead, V, Collin et al. 2005 The Montreal
cognitive assessment, MoCA: a brief screening tool
for mild cognitive impairment J. Am. Geriatr. Soc.
53(4) 695-9
Staekenborg, SS., Su, T., Van Straaten, ECW et al. 2010
Behavioural and psychological symptoms in vascular
dementia; differences between small- and large-
vessel disease Journal of Neurology, Neurosurgery
and Psychiatry, 81 (5) pp. 547–551
Tiel, C., Sudo, FK., Alves, GS., Valente, LE., Moreira, M.,
Laks, J., et al. 2015 Neuropsychiatric symptoms in
Vascular Cognitive Impairment A systematic review
Dement Neuropsychol 9(3) pp 230-236.
Zhang, M., Wang, H., Li, T., Yu, X. 2012 Prevalence of
neuropsychiatric symptoms across the declining
memory continuum: an observational study in a
memory clinic setting Dement Geriatr Cogn Disord
Extra 2012;2:200–208. doi: 10.1159/000338410
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
556
