
Cost of Hypertension Disease in Kediri Regency
Atika Binti Utari, Thinni Nurul Rochmah
Faculty of Public Health, Universitas Airlangga Mulyorejo, Surabaya, Indonesia
atika.binti-13@fkm.unair.ac.id
Keywords: Cost of Illness, Hypertension, Individual perspective.
Abstract: The incidence of hypertension is the highest non-communicable diseases in Kediri District. The prevalence
of hypertension in Kediri District is 27.9 %. Their increasing prevalence is threatening to cause significant
damage both to individuals and society. From the individual perspective, it is therefore necessary to
consider the economic impacts associated with hypertension diseases, and identify interventions that can
reduce the burden of these diseases. This cost of illness study aims to measure cost of hypertension disease
in Kediri District from individual perspective. This research is a quantitative research with cross sectional
method. Primary data collection is done by interviewing 100 hypertension sufferers in Kediri District. The
results estimated the direct costs is 6.220.470 rupiahs per capita and the indirect costs is 6.164.081 rupiah
per capita. Cost of illness caused by hypertension is about 12.384.551 rupiahs per capita. It can be
concluded that the cost of hypertension disease is very high. So it can be recommended to increasing
promotive and preventive efforts to reduce the incidence of hypertension disease
1 INTRODUCTION
Health problems in Indonesia is quite complex
which in the last ten years Indonesia had triple
burden disease. Infectious diseases are still very
high, but on the other hand occurring of an
increasing number of non-communicable diseases
and new emerging diseases. According to WHO
(2014), mortality rate from non-communicable
diseases will continue to increase worldwide. In
2030, estimated there are 52 million deaths from
non-communicable diseases. One of the non-
communicable diseases which counted as a public
health problem is hypertension. Not only happened
in developing countries but also happened in
developed countries.
Hypertension is commonly called by silent killer
because the symptoms are not known for sure. The
symptoms that appear can be vary depend on each
individual and almost the same as other diseases. In
addition, hypertension is also a risk factor for
deathly diseases such as stroke and coronary heart
disease. Riskesdas (2013) showed that nationally
25.8% of populations of Indonesia suffered from
hypertension.
The number of incidence of hypertension in
Kediri District increased from year to year. In 2016
the incidence of hypertension got a first place for
non-communicable disease in Kediri District.
Hypertension prevalence rate even reached 27.9 %.
This number was higher than the hypertension
prevalence rate of eastern Java which was 26.2 %.
Some of high and unreliable incidence of
hypertension can cause a loss not only economically
but also on productivity and complications of other
diseases. Increasing the number of incidence of
hypertension can have an impact on economic
burden, productivity loss and the complication
appearances.
So that important to conduct a study concern to
the costs which is covered by patient during illness.
According to Jo C (2014) Cost of illness is a study to
estimate the magnitude of the economic costs borne
by an illness. The purpose from this study is to
measuring cost of illness of hypertension that was
experienced by a patient with hypertension in Kediri
District from individual perspective.
2 METHODS
This research was a quantitative research with cross
sectional design. Population in this research was
total patient of hypertension in Kediri District in
2017 that is equal to 435,628 people. The sample
was calculated by using Slovin formula to obtain a
272
Utari, A. and Rochmah, T.
Cost of Hypertension Disease in Kediri Regency.
In Proceedings of the 4th Annual Meeting of the Indonesian Health Economics Association (INAHEA 2017), pages 272-276
ISBN: 978-989-758-335-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
large number of sample as many as 100 people who
has hypertension.
The sample in this research taken by cluster
random sampling. The first stage technique of
sampling began with determining the cluster by
using the working area of the Primary Health Care.
There was a consideration in selecting the working
area where to be sampled to represent the
population. That was by selecting the existing
primary health care in rural and mobile areas. 2
working area where to be chosen that meet the
criteria are Kandangan Primary Health Care (rural
village) and Pare Primary Health Care (crowded
area).
Data were collected randomly by door to door
way on patient who has hypertension in Pare
Primary Health Care and Kandangan Primary Health
Care. Instrument that used in this research is
questionnaires. the study was conducted from May
to July 2017. The cost of illness in this study used an
individual point of view. Variables to calculate the
cost of illness consists of direct cost and indirect
cost. Tool for data analysis in this research used
Ms.Excel.
3 RESULTS
According to WHO (2009) the cost of illness can be
divided into direct cost and indirect cost. Direct cost
is costs that are directly related to treatment of
hypertension, while indirect cost is costs that are not
directly related to the treatment of hypertension
borne by the patient during treatment for the illness.
3.1 Direct cost
Direct cost is costs that are directly related to the
treatment of hypertension. This cost is paid by
patients who has hypertension to check-up their
health. According to Istiqomah (2016) Direct cost is
divided into two categories, they are routine cost and
incidental cost. Routine Cost is the average of direct
cost that is routinely paid by patient as long as the
patient has the illness. This cost is calculated for one
year.
The cost which is a routinely direct cost is the
outpatient expense and other medical expenses.
Outpatient costs be obtained from the average
expenses for outpatient treatment by the patients for
one year. While other medical costs are showing the
average expenses of other treatments which is paid
by patients for one year. The other treatments which
being intended is a treatment that is not performed in
health services, like buying medicine in pharmacy
by themself or buying traditional medicine.
Incidental direct cost is a direct costs which paid
at any time during the treatment for the illness. Costs
that include incidental direct costs in this study is the
cost of hospitalization. The cost of hospitalization is
an average expenses for inpatient treatment for
hypertension patients.
The average of routine direct cost during illness
was derived from the multiplication of routine direct
cost over for a year with the average duration time
of illness. The average duration of illness of the
patient was calculated by reducing life expectancy of
Kediri District population which is 72 years old by
the age of the first time respondent has the illness
which is 55 years old. So the average value of the
duration of illness is 17 years.
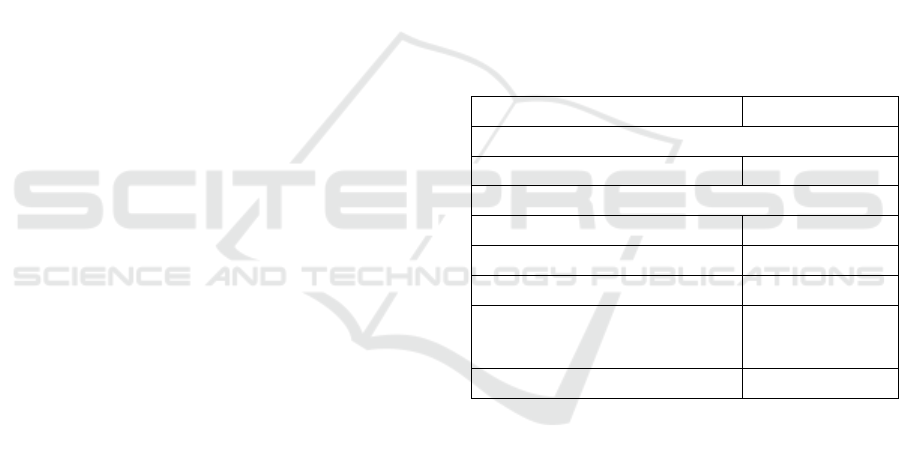
The following is a calculation result of direct
cost that can be seen in Table 1.
Tabel 1: Direct Costs on Hypertension Patients in Kediri
District
Statement
Cost (Rupiahs)
INCIDENTAL COST
Average of Inpatient Treatment
178.500
ROUTINE COST
Average of Outpatient Treatment
297.870
Average of Other Treatments
57.540
Average of Routine Direct Cost
355.410
Average of Routine Direct Cost
during Treatment for The Illness
(17 years)
6.041.970
TOTAL DIRECT COST
6.220.470
Based on Table 1 it can be concluded that the
direct costs which paid by hypertensive patients is
Rp 6.220.470, -. The biggest component in direct
costs is in a routine direct cost that is the expenses
for outpatient treatment.
3.2 Indirect Cost
Indirect cost is costs that are not directly related to
the treatment of hypertension which paid by the
patient for the illness. Istiqomah (2016) state that
indirect cost is divided into two categories: routine
indirect costs and incidental indirect costs. Routine
indirect cost is an indirect cost which routinely paid
by the patient as long as the patient has the illness.
While incidental indirect cost is indirect costs which
Cost of Hypertension Disease in Kediri Regency
273
paid by the patient at any time as long as the patient
ill.
Routine indirect costs consist of outpatient
transport cost, outpatient productivity loss, and
outpatient companion productivity loss. While the
incidental indirect costs consists of inpatient
transportation cost, inpatients productivity loss, and
inpatient companion productivity loss.
Transportation cost represent transportation costs
incurred when visiting health services for the
treatment. Transportation cost is obtained by
multiplying the number of visits with the average of
one-way cost to the intended health service. The cost
of aids is a cost incurred to purchase aids as long as
patient suffers from hypertension. While the
productivity loss is the cost of productivity loss due
to the absences of the patient for leaving the job or
normal activities to undergo treatment. The cost is
obtained by multiplying the percentage of total
absences in a month with an average monthly
income.
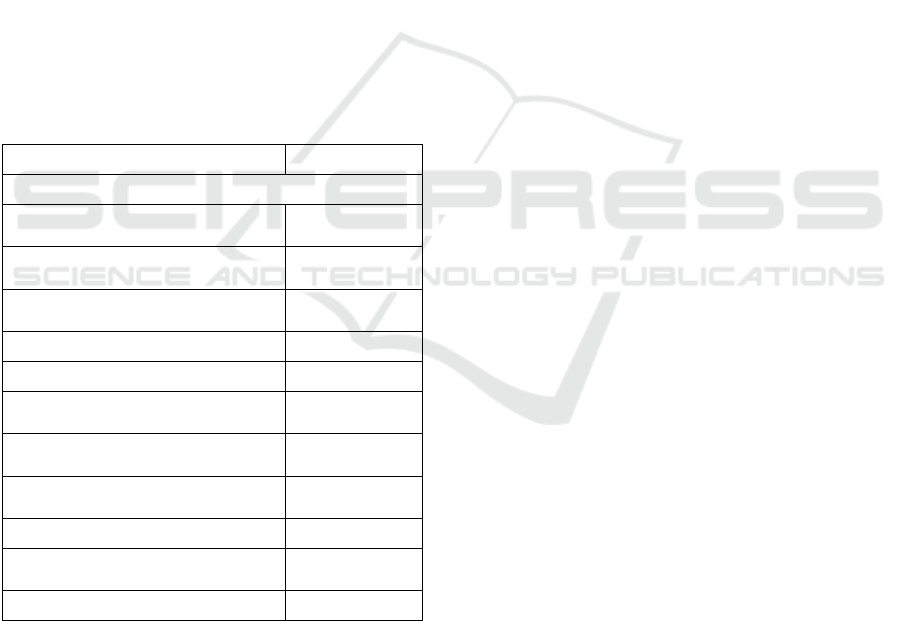
Tabel 2. Indirect Cost on Hypertension Patients in Kediri
Distric
Statement
Cost (Rupiahs)
INCIDENTAL COST
Average of Transportation of
inpatient care
48.440
Average of Productivity Loss on
patients of inpatients care
64.268
Average of Productivity Loss on
patient company of inpatient care
67.980
Average of Incidental Indirect Cost
180.687
ROUTINE COST
Average of Transportation of
Outpatient Care
162.020
Average of Productivity Loss on
patients of outpatients care
120.655
Average of Productivity Loss on
patient company of outpatient care
69.290
Average of Routine Indirect Cost
351.964
Average of Routine Indirect Cost
During the Illness (17 years)
5.983.394
TOTAL INDIRECT COST
6.164.081
Based on Table 2 it can be seen that amount of
indirect cost is 789,272, -. The largest component of
the routine cost is productivity loss costs for
outpatients and outpatient transport.
After the calculation of direct and indirect
costs, it can calculate the cost of illness for each
individual patients who has hypertension follows:
Cost of
Illness
= Direct Cost + Indirect Cost
(1)
= 6,220,470 + 6,164,081
= 12.384.551 rupiahs
Based on the above calculation can be concluded
that the value of cost of illness which is borne and
covered by hypertension patient in Kediri District is
Rp 12.384.551, -.
4 DISCUSSION
According to WHO (2014) nearly 45% burden of
disease that occurring in low-income and middle-
income countries is caused by non-communicable
diseases. Hypertension is one of them which counted
as the major risk factors for global disability, death
and disproportionate impacts in low-income and
middle-income countries. Two-thirds suffer from
hypertension. In 2010 estimated that 9.4 million
deaths and 162 years are lost due to hypertension
worldwide. The prevalence of hypertension
continues to increase worldwide and it is estimated
to affect more than 500 million people by 2025.
Based on the health profile of Kediri District,
Hypertension is a non-communicable disease with
the highest number of cases in 2016.
This study showed that the routine direct cost of
hypertension in one year is obtained from outpatient
and other medical expenditure every month. Besides
outpatient visits in health services, some patients
also buy their own medicines at pharmacies, buy
traditional medicines and other alternative
treatments. The results showed there was a cost for
other treatments of Rp 57,540 per month.
Besides identifying the direct costs, cost of
illness analysis also needs to identify indirect costs.
In this study, indirect cost consist of outpatient and
inpatient transportation costs and productivity loss
during outpatient and inpatient care.
The value of transportation costs incurred by the
patient is influenced by the frequency of visits to
health services. The higher frequency of visits then
the higher also the cost of transportation cost. In this
study the patient uses a variety of transportation to
go to health services. For the example is
motorcycles, cars, public transportation or walk.
This study also found that some patients who live in
crowded population areas (working area of Pare
Primary Health care) go to health services by riding
a bicycle or walking. This is because the location of
health services is easily accessible. While
transportation in patients in rural areas (working area
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
274

Kandangan Primary Health Care) go to health
services by motorcycle.
Components that affect the value of patient
productivity loss is the frequency of visits and
income per month. This study found that the
percentage of unemployment patient is 22%. This is
because of most of them are elderly sufferers, so
they have no job and the final effect is the
productivity loss becomes low. If anyone at his
productive age suffer from hypertension, his work
activities will be distrubed due to the illness. In the
other hand, the work’s time will be reduced when he
had to undergo the treatment such as outpatient care
and hospitalization. According to Hyder et al (2012)
productive age is generally associated with people
aged 15
th
-64
th
years. At that age, people is
considered to spend more of his life to move and
work. At the under 15
th
years and age above 64
th
years it is considered a dependent in domestic life.
The elderly sufferer, who usually have entered
the age of retirement and not working, have lower
productivity loss than patient on productive age. At
this age, the patient has entered an old age that
caused organ function’s decreased. The process of
degeneration and disease suffered will increase the
severity of the illness. Therefore, the patient will
need the help from the others while visiting health
services for outpatient and inpatient.
When someone who has no money suffered from
hypertension, the cost of the treatment will depend
on his family. If the income is low then it will make
the economic situation of the family worse off.
Because of that, the JKN program will help public
ensure the health needs in order to remain the public
to check his health so it won’t get worse.
Based on research conducted by Catherine
(2016) it is estimated that the value of Dissability
Adjusted Life Years in almost all the world due to
high blood pressure ranks second after the risk of
illness due to diet. According to Chataut et al (2011)
in a study conducted in Nepal in 2011 mentioned
that gender and old age are independent factors or
hypertension risk factors that can not be changed. In
other hand, there are many risk that preventable.
Such as healthy diet, healthy lifestyle.
Based on the results of the research can be
concluded that the indirect costs which paid by
patients is not really different with the direct costs.
But in reality there are still many people who are
unaware that besides the direct costs of the
treatment, there are another economic losses such as
expenditures for transportation costs and
productivity loss.
5 CONCLUSION
The results showed that the cost of illness of
hypertension in Kediri District is Rp 12.384.551 per
capita. This means that every individual who suffers
from hypertension will bear the economic burden
which is Rp 12.384.551. Based on the analysis it can
be concluded that during suffered from hypertension
there are much of indirect costs that must be covered
by patient due to the illness. The indirect costs
which paid by patients is not really different with the
direct costs. But in reality there are many people
who do not realized that hypertension can caused the
economic loss which is indirectly affect the
economic conditions of households, regional even a
country.
The point is to make awareness to public for
increasing preventive and promotive of hypertension
disease. Preventive and promotive efforts need a
Government support. It can be done by increasing
the budget for the promotive and preventive efforts
to make more activity programs to reduce the
prevalence of hypertension. Preventive and
promotive efforts also require commitment and
active participation from the human resources of
health sector and the public to ensure the programs
can be done well.
REFERENCES
Catherine P, B., Gregory A, R., Andrew E, M., 2016. The
Global Burden of Disease Study and the Preventable
Burden of NCD.[e-journal] 11(04): 393-397, Tersedia
di http://ac.els-cdn.com/S2211816016307608/1-s2.0-
S2211816016307608-main.pdf?_tid=5eee7b0a-60a2-
11e7-9521-
00000aab0f02&acdnat=1499163795_7bc21522a748d
64c71b45caafbf79635 [diakses tanggal 4 Desember
2016]
Chataut J, Adjikari R.K.,Sinha N.P., 2011.Prevalence And
Risk Factors for Hypertension in Adult Living in
Central Development Regiaon in Nepal.Kathmandu
University Medical Journal, [e-journal] 33 (1) pp. 8-
13. Tersedia di: http://www.kumj.com.np/issue/33/13-
18.pdf [5 Juni 2017]
Hyder, A. A., Puvanachandra, P., & Morrow, R. H.
(2012). Measuring the Health of Populations:
Explaining Composite Indicators. Journal of Public
Health Research, 1(3), 222–228.
http://doi.org/10.4081/jphr.2012.e35
Istoqomah, AN.2016. Analisis Burden of Disease Akibat
Hipertensi Pada Masyarakat dengan Status PBI JKN
Cost of Hypertension Disease in Kediri Regency
275

di Kabupaten Pamekasan. Skripsi.Universitas
Airlangga
Jo C. 2014. Cost of Illness Studies: Concepts, Scopes, and
Methods. Clinical and Molecular Hepatology Journal.
[e- journal]. Vol 20: 4. Available from:
http://dx.doi.org/10.3350/cmh.2014.20.4.327.
[Accessed 5
th
, July 2017]
Riset Kesehatan Dasar, 2013. Riset Kesehatan Dasar.
Jakarta: Badan Penelitian dan Pengembangan
Kesehatan.
World Health Organization (WHO). 2009. WHO: Guide to
Identifying The Economic Consequences of Disease
and Injury. Geneva: WHO Departement of Health
System Financing Health System and Services.
World Health Organization (WHO).2014. Global Status
Report of Non Communicable Disease 2014.WHO.
Switzerland. Available from:
:http://apps.who.int/iris/bitstream/10665/41864/1/0965
546608_eng.pdf [6
th
, June 2017]
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
276
