
Unit Cost Calculation as a Role of Cost Containment at Central
Surgery Installation of Hospital X
Setya Haksama
Faculty of Public Health, Universitas Airlangga, Mulyorejo, Surabaya, Indonesia
setyahaksama@fkm.unair.ac.id
Keywords: Central surgery installation, Unit cost, Activity-based costing.
Abstract: In regards to good health development services in terms of budgeting and financing, not all hospitals, such
as hospital X, have data on the production cost of services as the basis for determining the tariffs, because
this has not been calculated based on unit cost. The unit cost calculation of services in Central Surgery
Installation (CSI) Hospital X is the main purpose in this research, which used a cross-sectional with
descriptive observational approach and analysed using Activity-Based Costing (ABC) method. The results
showed that the unit cost calculation was divided based on eight qualifications of operation in minimum and
maximum unit cost intervals, as follows: (1) Minor: IDR 1.320.206 - IDR 2.805.815, (2) Moderate: IDR
2.057.070 - IDR 2.733.284, (3) Major: IDR 2.408.011 - IDR 3.995.652, (4) First Major: IDR 2,228,755 -
IDR 4,759,747, (5) Second Major: IDR 1.727.593 - IDR 5,523,273, (6) Third Major: IDR 3,049,093 - IDR
7,099,322, (7) Fourth Major: IDR 6,176,461 - IDR 7,512,786, (8) Fifth Major: IDR 1,711,223 - IDR
9,439,909. The existence of the unit cost calculations assists management to make accurate decisions on
budgeting and cost planning; hopefully, it can be developed in an integrated system for recording and
reporting.
1 INTRODUCTION
In the course of the development of health services,
the aspects of budgeting and financing of health are
essential, because it focuses the hospital’s attention
and how the budget can be used for investment,
operational purposes, improving the competence of
human resources and improving the welfare of its
employees. It should be considered in the
implementation of Security Agency of Health
(BPJS-Kesehatan) which has implemented tariffs in
accordance with the existing policy, namely
Permenkes Number 69 Year 2013 about Standard
Rates on Primary Health Care and Advanced Health
Facilities level in the Implementation of Health
Insurance Programs, where the determination of the
tariffs’ policy caused problems in its implementation
at this time
7
. In health care systems, hospitals
provide primary care, serve as referral institutes for
higher-level care, and train health care workers.
Those benefits are costly
(Baker, 1998).
General hospitals as health care organizations
should adjust the tariffs immediately into a variety
of management functions such as regulation,
planning, guidance, and supervision. In addition, it
should be realized that the hospital has many unit
production and supporting costs, whereby each unit
has to generate revenue and there is not a must have
list in terms of cost. Such diversity is sometimes
likely to cause a lack of accuracy of the actual costs
owned by the hospital. The unit cost as the basis for
calculating the budget does not necessarily reflect
the actual costs at the hospital. Therefore, a tally of
unit cost, actual cost and expense management
should be made in a normative order with respect to
the tariff policy of being rational and accountable
(Roztocki et al, 2004). A company which has
valuable information in comprehending and
identifying customers who are more profitable or not
will help advance the overall organizational
profitability
(Baker, 1998). Customer cost
information is considered very helpful in
maintaining the level of profits and retain customer
relationship.
In general, there has not been accurate data of the
hospital facilities and production costs of health and
medical services for use as a basis of determining
the tariff. This condition is not recommended
because the basis of current rates has not been
calculated as unit cost; basically, the hospital has
252
Haksama, S.
Unit Cost Calculation as a Role of Cost Containment at Central Surgery Installation of Hospital X.
In Proceedings of the 4th Annual Meeting of the Indonesian Health Economics Association (INAHEA 2017), pages 252-256
ISBN: 978-989-758-335-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

calculated the unit cost, but is still not rational. The
rationality level of the tariffs has many viewpoints,
such as the current rate being too expensive or too
low. Both conditions lead to different consequences.
If the current rate is too expensive, what the
consumer pays is not comparable with the output
obtained. Similarly, the lower rate could lead to the
hospital as a healthcare provider not reaching the
break-even point or even having a deficit
(Mulyadi,
2015). This situation should sensitize health care
providers to adopt a rational rate, in accordance with
the service received by consumers.
2 METHODS
This study was an observational study descriptive
and there was no treatment on the sample.
Observational study emphasizes on activities in the
field as a data source and a research approach in
data collection in the form of primary and
secondary data, such as financial reporting
documents, the traffic data, annual reports, internal
data and other data. Based on the time of the study,
the study design was cross-sectional because pf the
timing of data collection and information research
conducted at one particular time and then an
analysis of data using Activity-Based Costing.
The data analysis technique used was Activity-
Based Costing, which is a method for calculating the
cost of production used to provide cost information
for managers as a basis for making strategic
decisions and other actions that affect the capacity
and fixed costs
(Blocer et al, 2000). The stages of
accounting by Activity-Based Costing are as follows:
(1) identification of activities; (2) organize activities
into cost centers; (3) identification element of main
cost; (4) analysis of relationship between cost
activities; and (5) identify cost drivers
3 RESULT
The effective working time in one year was
calculated based on 2013, which determined the
total of the number of effective days of each month.
Effective days are work days which were already
reduced by holidays and national holidays. Number
of days effective in one year were then converted
into units of minutes. The result of the calculation of
time effective for one year, based on research,
showed working hours per day for eight hours with a
total time of 1,960 hours or 117,600 minutes.
Throughout 2013, there were 6,809 medical actions
undertaken operative in Central Surgery Installation,
which was divided into 12 rooms of CSI, so that at
each CSI room could serve 2-3 patients per day.
From the results of field observations, relevant data
area of Central Surgery Installation of 518m
2
were
obtained. Magnitude of spacious CSI rooms can be
divided into 12 rooms, each of 42 m
2
, except room
10. Direct costs related to the place of the medical
action operative are the fees charged to patients
when performing medical procedure operatives as
cost replacement incurred by the hospital for
procurement and the maintenance of buildings
(Fauziah et al, 2014). The building is assumed to
have a lifetime of 20 years, so the function of
building was considered normally in 20 years of life.
After knowing the entire procurement cost of space
in CSI, the cost center of the main Central Surgery
Installation (CSI) building will be delivered. Based
on calculating the cost center of the Central Surgery
Installation (CSI), obtained from Annual Investment
Cost, and the the calculation of depreciation costs of
buildings, we get the total cost center for Central
Surgery Installation (CSI) of IDR 389,042,092.88.
The costs of procurement for each operating room
obtained from the calculation of the cost center of
Central Surgery Installation (CSI) were divided by
the effective working hours per operating room in
minutes to obtain the cost per-minute on each
operating room, which were then multiplied by the
duration of action per operative medical treatment.
The following is the calculation of the cost for
medical treatment operative place.
Note:
Effective : 245 days
Working Hours effective : 245 days x 8 hours x 60
minutes = 117 600 min
Cost center of the building : IDR 389,042,092.88
Then the cost of space per :IDR 389,042,092.88
/117 600
: IDR 3308.18
Furthermore, the cost will be multiplied by the
length of each operative medical treatment in CSI.
Human Resources (HR) is composed of medical
personnel, both specialist doctors, general
practitioners, nurses and other medical personnel,
who perform operative medical procedures and non-
medical personnel involved indirectly in Central
Surgery Installation. Cost of Medical Consumables
per operative action of the medical pharmacy depot
parts were obtained from CSI. Consumable Cost
fees in the pharmaceutical depot in CSI were
different from the central pharmacy depot. In the
central pharmacy depot, using a software that shows
Unit Cost Calculation as a Role of Cost Containment at Central Surgery Installation of Hospital X
253
pharmaceutical expenditure costs, as in the table
below.
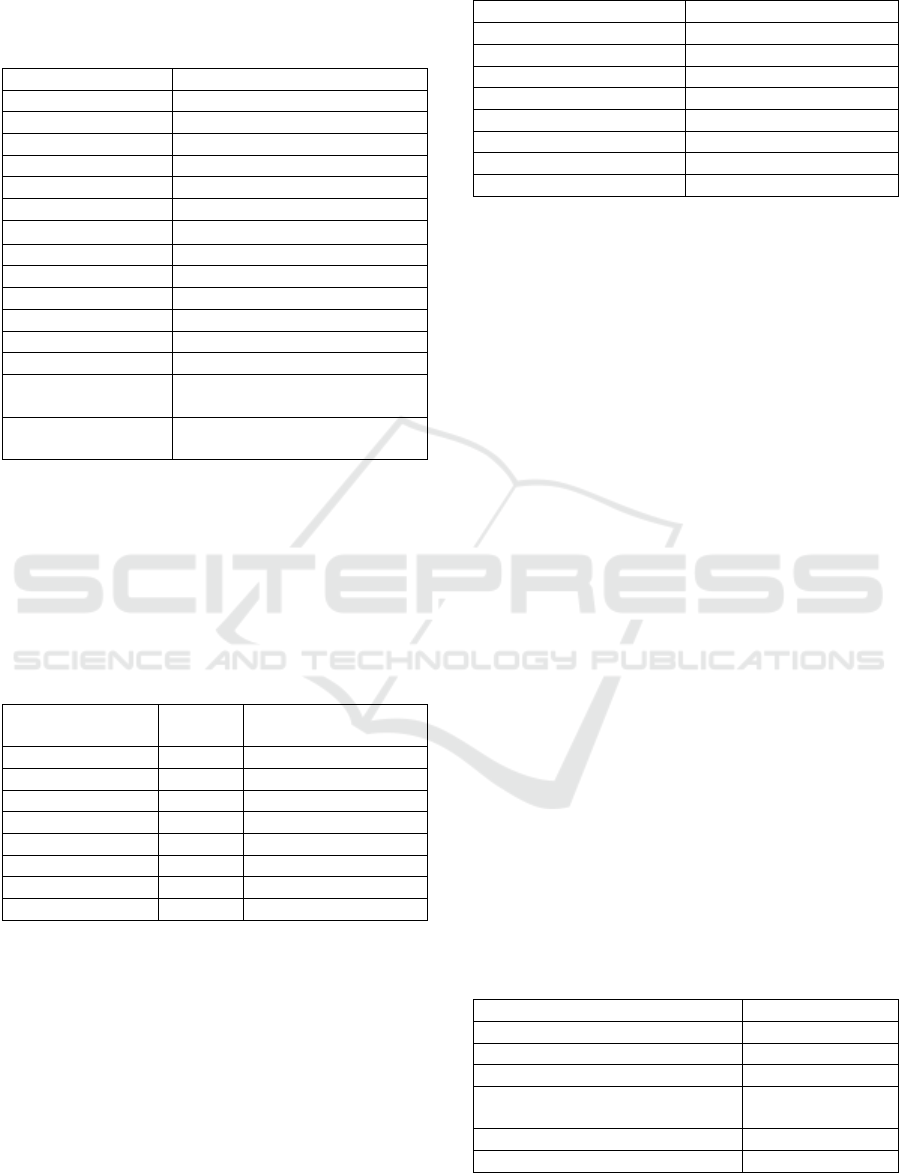
Table 1: Total Cost of Consumables
Month
Fees Consumable Cost (IDR)
January
449,181,603.00
February
449,181,603.00
March
449,181,603.00
April
449,181,603.00
May
449,181,603.00
June
449,181,603.00
July
449,181,603.00
Month
Fees Consumable Cost (IDR)
August
449,181,603.00
September
449,181,603.00
October
449,181,603.00
November
449,181,603.00
December
449,181,603.00
Total 1 year
Consumable Cost
5,390,179,236.00
Consumable Cost
Cost per action
791,625.6772
Source: Hospital pharmacy depot X
Furthermore, to obtain the value of consumable cost
per category action then a score was made according
to the category of the type of medical treatment
operative. Here the results of calculation of the
consumable cost were based on medical surgery
category.
Table 2: Cost of Consumable Per Qualifying Operation
Qualification
Operation
Score
Total Cost
Consumable Cost
Minor
1
791.626
Moderate
2
1,583,251
Major
3
2,374,877
Major 1
4
3,166,503
Major 2
5
3,958,128
Major 3
6
4,749,754
Major 4
7
5,541,380
Major 5
8
6,333,005
Waste of CSI can be divided into medical
waste and non-medical. The calculation of the unit
cost of processing medical waste obtained a sewage
treatment fee per kg of IDR 10111.09. Based on
interviews and dealing with operating personnel in
the CSI, the weight of solid waste for each action is
not always the same, but can be searched by
averaging suitably qualified operations, described as
follows.
\
Table 3: Unit Cost Medical Waste
Qualifying Operating
Weight Solid Waste (g)
Minor
400
Moderate
500
Major
600
Major 1
1700
Major 2
2700
Major 3
3700
Major 4
4700
Major 5
5800
Activities of non-medical services in the
installation of the Central Surgery entail
management and administration activities performed
at the Central Surgery. The room used to perform
non-medical services has area of 1480m
2.
with cost
per m
2
of IDR 1,401,583.73 and then multiplied by
the area. So, from the calculation of the above
Annual Investment Cost, cost directly related to for
the site of management activities is IDR 50,373 per
action. Based on the calculation of infrastructure
maintenance costs, maintenance costs can be
calculated by load per-action with the total action in
2013 as many as 6,809 by dividing the total cost of
maintenance with the actions in 2013, so that it
shows the burden of indirect costs for treatment as
IDR 50,455.66. Furthermore, other costs include the
operating costs consist of expenditure on electricity,
water and telephone/ fax. In 2013 there already
exists a recap of telephone charges, water and
electricity by the hospital. By knowing the total area
of the hospital as 82,381.01 m
2
and total action as
many as 6,809, these are used to determine the costs
of electricity, water and telephone per action and can
be explained as follows. From the calculation of
operating costs, total other costs per action is IDR
14,584.99, while the results of calculating costs for
non-medical consumables are IDR 6,809.00 for one
year, and total expenses per action is IDR 4,303.81.
Below is a table of indirect costs in the Central
Surgery installation and direct costs of each
operative medical treatment activity.
Table 4: Indirect Costs
Components Indirect Costs
Total Costs
Place
50,373
HR Non-Medical
161,797
Maintenance
50,456
Operations (electricity, water,
telephone)
14,585
Consumable Cost
4,304
Total
281,514
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
254

4 DISCUSSION
Based on this study it can be seen that the results
calculation of Unit Cost in the Central Surgery
Installation is divided based on operation
qualification. Cost drivers used are old minimum
and maximum actions that ultimately produce
intervals of unit cost minimal and unit cost
maximum. The following summary table calculates
minimal and maximal unit cost.
Table 5: Unit Cost Result
Operations
Qualification
Unit Cost
Minimum (IDR)
Cost Unit
Maximum (IDR)
Minor
1,320,206
2,805,815
Moderate
2,057,070
2,733,284
Major
2,408,011
3,995,652
Major 1
2,228,755
4,759,747
Major 2
1,727. 593
5,523,273
Major3
3,049,093
7,099,322
Major 4
6,176,461
7,512,786
Major 5
1,711,223
9,439,909
Based on the table, the calculation of unit cost
uses Activity-Based Costing, generating minimal
and maximum unit cost divided by operation
qualification. The idea concepts of Activity-Based
costing is a cost accounting system that focuses on
activities performed to produce a product / service.
Activity is any activity which is the trigger of the
cost (cost driver) and acts as a causal factor in
spending in a production process. Activity-Based
Costing is able to present more accurate product cost
and information, and is a direct measurement of the
profitability of products that more accurately reflects
strategic decisions on the selling price, market
product lines and expenditure models. It also
obtained a more accurate measurement of the costs
triggered by activity, thus helping management
improve the product value and the value of the
process, thereby helping the information on costs for
decision making (Carter et al, 2012). The weakness
of Activity-Based Costing is that some costs were
allocated at random due to limitations in finding the
cost of the activity. It also ignores the cost of
analysis and requires extensive time and cost. The
Activity-Based Costing method can help to reduce
unnecessary cost effectively and reduce costs that do
not have added value and can even remove the cost
of unnecessary activity through activity analysis.
Analysis of activity should result in: (1) what
activities are carried out; (2) how many people are
doing the activity; (3) the time and resources
required to perform the activity; and (4) the
calculation of the value of the activity
5 CONCLUSION
Based on this study, it could be concluded that the
calculation of unit cost can be used in controlling
costs in health services provided by health agencies.
The results showed that the unit cost calculation in
CSI Hospital X was divided into eight qualifications
based of operation, which resulted in minimum and
maximum unit cost intervals as follows: (1) Minor:
IDR 1,320,206 and IDR 2,805,815; (2) Moderate:
IDR 2.05707 million and IDR 2,733,284; (3) Major:
IDR 2,408,011 and IDR 3,995,652; (4) 1
st
Major:
IDR 2,228,755 and IDR 4,759,747;(5) 2
nd
Major:
IDR 1,727,593 and IDR 5,523,273; (6)
3
rd
Major:IDR 3,049,093 and IDR 7,099,322; (7)
4
th
Major: IDR 6,176,461 and IDR 7,512,786; (8) 5
th
Major: IDR 1,711,223 and IDR 9,439,909.
Calculation of unit cost is analyzed using many
approaches and methods, one of which is Activity-
Based Costing.
Therefore, the recommendations can be given as
follows. (1) There should be improvement in the
inventory records of medical devices and non-
medical, either in the form of soft files or hardfiles;
(2) improvement in the recording and reporting of
activities of medical in Central Surgery Installation
by developing an integrated system for recording
and reporting; (3) provision of services of medical
personnel according to their competencies, thus
incorporating elements of clinical pathways
becoming absolute in recording employee data; (4)
registration of consumables per action should be
through clear mechanisms ranging from pharmacy
depot or warehouse pharmacy to the pharmacy that
provides services; therefore it is necessary for the
manufacture and development of integrated
information systems; (5) the development and
strengthening of the integrated management
information system in any installation; and (6)
provide training to Human Resources to run the new
information technologies
REFERENCES
Baker, J.J. (1998). Activity Based Costing and Activity
Based Management for Healthcare. Aspen Publisher
Inc.
Blocer, Edwar J, Chen, Kung H, dan Lin, Thomas W.
(2000). Manajemen Biaya. Jilid I. Jakarta: Salemba
Empat
Carter, William K, Milton F. Usry. (2012). Cost
Accounting. 14
th
Edition. Translate by Krista. Jakarta:
Salemba Empat.
Fauziah, Ida, Dzulkirom A. R., Achmad, Husaeni. (2014).
Analisis Activity Based Costing (ABC) System
Unit Cost Calculation as a Role of Cost Containment at Central Surgery Installation of Hospital X
255

Sebagai Dasar Penetapan Harga Pokok Produksi.
Jurnal Administrasi Bisnis (JAB). 12 (02).
Mowen, MM & Hansen, D.R. (2006). Akuntansi
Manajemen. 7
th
Edition. Jakarta: P.T Salemba Empat.
Mulyadi. (2015). Activity Based Cost System, Sistem
Informasi Biaya untuk Pemberdayaan Karyawan,
Pengurangan Biaya, dan Penentuan Secara Akurat
Kos Produk dan Jasa. Yogjakarta: UPP STIM YKPN
Peraturan Menteri Kesehatan No 69 Tahun 2013 Tentang
Standar Tarif Pelayanan Kesehatan Pada Fasilitas
Kesehatan Tingkat Pertama dan Fasilitas Kesehatan
Tingkat lanjutan dalam Penyelenggaraan Program
Jaminan Kesehatan.
Roztocki, N. Porter, J. D, Thomas, RM Needy, K. L,
(2004). A Procedure for Smooth Implementation of
Activity Based Costing in Small Companies.
Engineering Management Journal. American Society
or Engineering Management. 16 (4).
Tandiontong, Mathius. (2012). Peranan Activity Based
Costing System dalam Perhitungan Harga Pokok
Terhadap Peningkatan Profitabilitas Perusahaan.
Akurat Jurnal Imiah Akuntansi. No. 05.
Trisnantoro, L. (2014). Memahami Penggunaan Ilmu
Ekonomi dalam Manajemen Rumah Sakit.
Yogjakarta: Gajah Mada University Press.
Yereli, Ayse Necef. (2016). Activity Based Costing and
Its Application in a Turkish University Hospital.
AORN Journal. 89 (3).
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
256
