
Piloting Collection Model of Health Insurance Contributions for
Informal Sector Members
Mahlil Ruby
1
, Eka Pujiyanti
1
, Euis Ratna Sari
1
, Gemala Chairunissa Puteri
1
, Riza Maulana
Putra
1
, Unun Hamida Qodarina
1
, Dinda Srikandi
1
, Mutia Anggun Sayekti
1
, Dedy Revelino
Pardamean Sirega
r
2
, Rizki Lestari
2
and Welly Gadistina
2
1
Center for Health Economics and Policy Studies (CHEPS) Faculty of Public Health, Universitas Indonesia, Depok,
Indonesia
2
The Indonesia Health Social Security Institution (BPJS Kesehatan), Central Jakarta, Jakarta, Indonesia
euisratnasari.jasmin@gmail.com
Keywords: Health insurance contributions, Informal sector, Promotor agent, JKN.
Abstract: Studies conducted by BPJS and CHEPS, 2015 showed that an active collection model through a third
party (a promoter agent) can improve the collectability status of informal sector members. This study
aimed to do a piloting collection model by a promoter agent (individuals, primary care facilities (PCF),
and local leaders) as well as informed about the ideal criteria of being agents with its challenges.
Methods: A quasi experimental design with non-equivalent group design (NEGD) was implemented
on two provinces with 1,509 households’ participants in Semarang and 1,193 households in
Balikpapan. Results: an individual promoter agent had 37.5% lowest proportion of being delinquent.
Multivariate regression analysis revealed that participants fostered by PCF and local leader as their
promoter agents had higher risk for being delinquent than those facilitated by individual promoter
agents. The effectiveness of the model differs between Semarang and Balikpapan with Individual
Agent Model showed a significant effect in Semarang. While in Balikpapan, there were no meaningful
models to improve the collectability. At last, the ideal individual agents have to hold: an experience
working in the community, have highly social skills as well as highly understanding of their
intervention regions.
1 INTRODUCTION
The number of participants BPJS Health up to
December 2016 has reached 171,048,734
participants equal BPJS Health achieves 68.5% of
the target of UHC and BPJS Health should be able
to cover about 75 millions of residents in the
remaining 2 years to 2019. From the contribution
aspect, the growth of informal sector members who
exceed this target ideally can support revenue
contribution of JKN, but in fact the realization of
contributions of informal sector members until the
end of 2015 and then reached 2.8 trillion rupias. This
amount is far above the initial target of the
determination of the receivables of informal sector
members estimated by BPJS Health at 1.8 trillion
rupias. The high receivables are contributed by the
low collectability of informal sector contributions
that only reached 60%. This will certainly affect the
national health financing cash flow, especially for
BPJS Health which can ultimately have implications
for financial management and services in health care
providers.
In the context of informal sector members, there
were four main reasons impact delinquency rate:
erratic income (23.6%), reluctant to queue (15.8%),
others reasoning (16.8%) such as (ATM Offline,
took a long time to pay at bank, forgot to pay
(12.8%), disappointed with provider or BPJS Health
(6,8%) (Ruby, 2016).
In Kusumasari & Widiastuti (2013), there are
four element can influence person’s behaviour to
pay health insurance contributions. Action is built on
the condition that a person wants or feels the need
for a health service guarantee, especially when they
sick (desired). However, when people health, it is
necessary to build an interest in informal sector
worker that make them interested in joining JKN
program, which in their perception can be a
protector of their risk from illness or risk of financial
burden due to illness (interest). To achieve these
perceptions, it is necessary to build awareness of in
informal sector members in the existence of JKN in
protecting themselves and their health (awareness).
242
Ruby, M., Pujiyanti, E., Sari, E., Puteri, G., Putra, R., Qodarina, U., Srikandi, D., Sayekti, M., Siregar, D., Lestari, R. and Gadistina, W.
Piloting Collection Model of Health Insurance Contributions for Informal Sector Members.
In Proceedings of the 4th Annual Meeting of the Indonesian Health Economics Association (INAHEA 2017), pages 242-247
ISBN: 978-989-758-335-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

If the AIDA link to informal sector members has
been established it is not impossible that the level of
collectability of health insurance contributions in
this type of participants may increase. It takes a
method or model of collection contributions that
more than just provision of payment channels that
tend to be passive. It takes an officer or individual
who actively and directly interacts with the
participants to guide, educate and build awareness of
participants' behaviour in paying health insurance
contributions, which will be known as BPJS Health
Promoter Agent.
The general objective of this activity is the
implementation of the Piloting Collection Model of
Health Insurance Contributions for Informal Sector
Members to enhance the collectiveness and
sustainability of group contributions of informal
workers in the achievement of the National Health
Insurance (JKN) program.
2 METHODS
The design of this study used quasi-experimental
method. Quasi experiments are experiments that
have treatments, outcome measures, and
experimental units but do not use random
placements.
The quasi experimental design used in this study
is Non-Equivalent Group Design (NEGD). This is
because in the assessment to be done on the level of
collectability status that will be compared not only
between groups of intervention with the control
group alone, but also among fellow intervention
groups with different promoter model models.
Baseline collectability level compared to the end line
collectability level on each model as an intervention
agency and the intervention by the control.
The selection of both groups was done
purposively. A total of 300 informal worker
households were designated as intervention targets,
but due to field dynamics faced by agents, the
number of households reached for each agency was
at least 150 households. The number of households
that can be visited is 6 - 8 households per day per
promoter agent, so that within 1 month (25 working
days) will be achieved the visit of 150 households of
informal workers per month. While the control areas
were not intervened, 150 informal workers'
households in the control areas were adjusted to the
number of participants for each intervention and
observed their initial contribution rate (as baseline
data) and at the end of the program (end line).
The unit of analysis in this study was the
household of informal worker participants who
participated in the BPJS Health in one cluster (1
cluster, consisting of 150 households). Interventions
conducted at Central Java Province, Semarang City
and East Kalimantan Province, Balikpapan City
The population in this study was all households
of informal workers in the experimental model of
active dues collection model, namely Central Java
and East Kalimantan provinces. While the sample in
this study is the head of the family who became the
respondent survey of the collection model of
contribution stage 2 in 6 cluster points per province
(1 point cluster contains 150 households).
This trial was conducted 2 (two) stages. Phase 1
is held on October 20, 2015 until December 23,
2015. Stage 2 is held from April 2016 to 31 October
2016.
3 RESULTS
Data was analysed by univariate, bivariate, and
multivariate analysis. Variables were used consist of
number of family members, children under 5 years
old and oldest of family members, services class,
worker number of family members, sex, age,
education background, married status, smoking
behaviour, sector of work, head of household
income, health status at first registration, economic
status, catastrophic status, and respondents’
delinquency status in the baseline and end-line of the
research. Data was category and used SPSS software
to analyse.
The data was analysed by univariate to show the
frequency of all variables. Bivariate analysis was
done to show the relationship between collectability
status baseline and end-line and others variables
which had represented social economic, and
demography aspect. Bivariate analysis used chi
square test by city, rural urban cluster, and village
sample.
Besides, chi square was used to show the
differences increase of delinquency rate between
intervention and control members. So, it could show
the effectivity of intervention. Effectivity analysis
also described based on promoter agent model in
this intervention which shown the lowest proportion
of delinquency rate by the promoter agent model.
After found the affecting factor of collectability
rate, the data was analysed multivariate to show the
most affecting factor of collectability rate.
Multivariate analysed used logistic regression test by
looking the highest Odds Ratio (OR) value of
independent variables. Multivariate analysed was
done on city area sample level (Semarang and
Balikpapan)
Piloting Collection Model of Health Insurance Contributions for Informal Sector Members
243
In this study there are a total of 2702 household
heads of informal sector members who responded to
the trial of applying an active JKN dues collection
model through a promoter agent. This number
consisted of 1509 household heads in Semarang city
(55.8%) and 1193 household heads in Balikpapan
(44.2%).
1. Demography profile
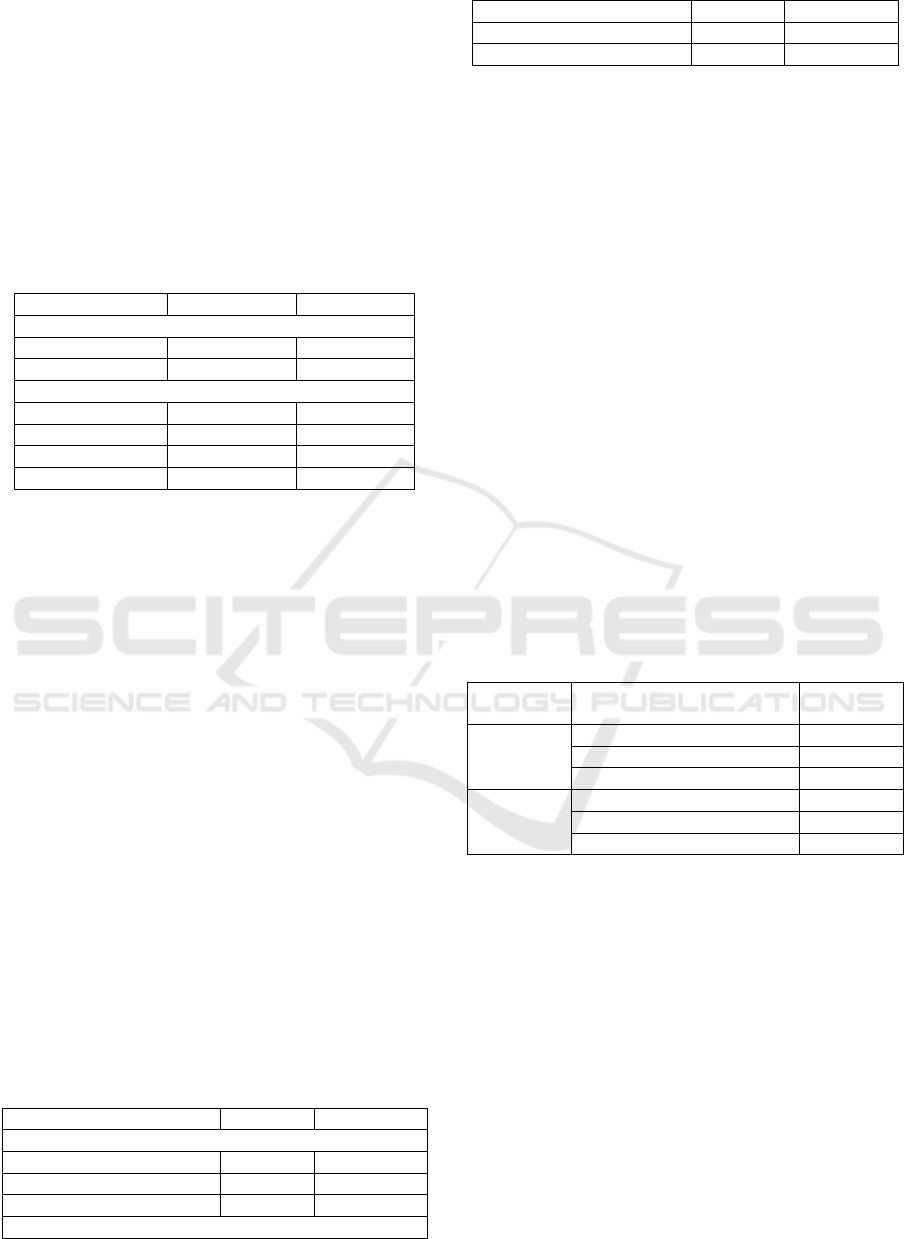
Table 1: Demography Profile of Respondents in Semarang
and Balikpapan 2016
Variables Semarang Balikpapan
Sex
Male 75.2% 80.9%
Female 24.6% 19.1%
A
g
e
<26 years ol
d
2.8% 3.5%
26-40 years ol
d
28.9% 27.4%
41-58 years ol
d
46% 47.3%
> 58
y
ears ol
d
22.4% 21.8%
Majority of the respondents are male which
were 75.2% in Semarang and 80.9% in Balikpapan.
But there are around twenty percent respondents are
female who act as head of household for informal
workers who become their household members. This
data show that the role family health insurance payer
majority are heads of families, fathers or sons who
are in the household. However, the table above
showed women role as family health insurance payer
is rising.
Most (3 of 4) payer contributions in the
households of informal workers in Semarang are at
working age (26 - 58 years). However, not a few
workers in informal workers' salaries are more than
58 years old (retirement age), 22%. This trend
occurs in all villages sample. Not much different
from the characteristics of the age of underwriters in
the city of Semarang, 3 of 4 underwriters in the city
of Balikpapan are also at the age of work and the
rest are at retirement age.
2. Social and Economic Profile
Table 2: Social Economic Profile of Respondents in
Semarang and Balikpapan 2016
Variables Semaran
g
Balik
p
a
p
an
Married status
Single 5.5% 4.3%
Marrie
d
82.5% 79%
Divorce 11.5% 16.5%
Education back
g
roun
d
< SHS 23.1% 48.4%
SHS
–
Vocation/ Bachelo
r
49.4% 48.9%
> Vocation- Doctoral 27.3% 2.7%
Most of the respondents are married 83% in the
city of Semarang and 79% of Balikpapan. Both in
Kota Semarang and Balikpapan, underwriters in
households of informal sector member are
dominated by heads of households with high school
education – Diploma (48%). This indicates that most
of the contributors in informal sector member
households are educated, although there are still
29% of respondents who have junior high school
education. In this group, potential contribution
arrears most occur.
From Semarang data in Figures and Balikpapan
in Figures 2015 indicates that 60% of the workforce
population in Semarang and 27% of the workforce
population in Balikpapan work in the informal sector
(PBPU). In workforce aspect, most of them work in
employment in services (71%) and 15% in trading.
Only 3% of them work in agricultural. Of those who
work, 58% work more than 40 hours a week.
Nevertheless, there are still 5% health insurance
payers are unemployed and 37% work less than 40
hours a week. In this group of households also the
potential contributions of arrears most occur.
Table 3: Income Profile of Respondents in Semarang and
Balikpapan 2016
Area
sample
Income Profile Category Percentage
Semarang < Rp 1,900,000 27.6%
R
p
1,900,000-R
p
4,500,000 52.4%
> R
p
4,500,000 6.4%
Balikpapan < Rp 2,200,000 53.2%
Rp 2,200,000-Rp 4,500,000 36.5%
> Rp 4,500,000 10.2%
84% of the participants of the informal sector
who responded to the pilot project in Semarang are
worked. Of those who worked, more than half of the
respondents earned between Rp 1,900,000 to Rp
4,500,000, only 6.4% of respondents earned more
than Rp 4,500,000 while 4 out of 10 respondents
were still earning less than the minimum regional
wage (UMR) of Semarang, Rp 1.900.000 (27.6%).
Meanwhile, in Balikpapan city, 86% of family
members of informal sector who participated in the
pilot project in this city are worked. Of those who
worked, 36.5% of the respondents earned between
Rp 2,200,000 to Rp 4,500,000, only 10.2% of
respondents earned more than Rp 4,500,000 while
almost 5 out of 10 respondents still earned less than
UMR in Balikpapan at Rp 2,200,000 (53.2%).
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
244
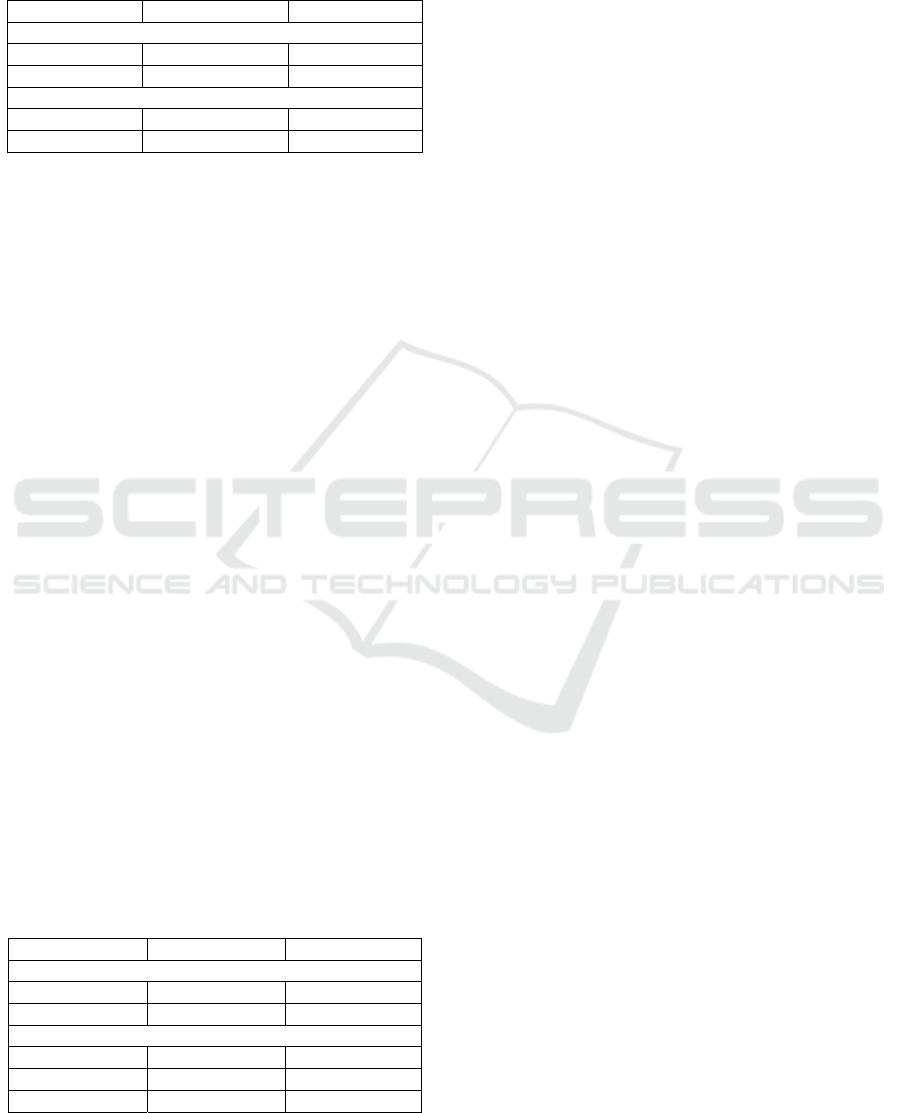
3. Other Social Economics Variables
Table 4: Economic Status and Catastrophic Rate in
Semarang and Balikpapan 2016
Variables Semaran
g
Balik
p
a
p
an
Catastro
p
hic rate
Yes 10.6% 22.1%
No 89.4% 77.9%
Economic status
Poo
r
12.7% 35.4%
No Poo
r
87.3% 64.6%
In this study also identified poverty status of
underwriters in informal sector members. Poverty
criterions were based on Social Ministry Policy
No.46 of 2013 about Fakir dan Orang Tidak
Mampu. The data showed that 12.7% of informal
sector member in the pilot project model of health
insurance contributions collection in Semarang
categorized as poor household in Semarang. In
addition, there are 10.6% of informal sector
household falls into the category of catastrophic
conditional, which is a household financial condition
where 30% of the income is charged to pay dues.
In Balikpapan city 35.4% of respondents in this
city are identified as having poor status based on
Social Ministry Policy No.46 of 2013 about Fakir
dan Orang Tidak Mampu.. In addition, 22.1% of
informal sector member fall into the category of
catastrophic conditional, which was, the financial
condition of informal sector members with a
proportion of 30% contribution to income.
Percentage of participants in the informal workers
who fall into the poor category and experience
greater condensed catastrophic conditions in
Balikpapan than the percentage in Semarang. This is
allegedly because of the cost of living (living cost)
in the city of Balikpapan. Balikpapan is currently a
costly living city according to various references.
4. Healthy profile
Table 5: Healthy profile of Respondents in Semarang and
Balikpapan 2016
Variables Semarang Balikpapan
Health status at re
g
istration
Health 89.8% 96.6%
Sic
k
10.2% 3.4%
Services class
1
st
class 20.2% 16.8%
2
nd
class 36% 25.4%
3
rd
class 43.8% 57.8%
Most of the respondents in Semarang who
registered as member of BPJS Health were good
health (8.89%). This means, 1 out of 10 respondents
registered as BPJS health’s members were taken
sick. Based on the class of care taken, 43.8%
informal sector members who as respondents in
Semarang used 3
rd
class of services. In Balikpapan,
96.6% of informal sector members who participated
in the pilot project admitted being in good health at
the first registration as a participant and 57.8%
respondents chosen 3
rd
class of services.
5. Level of Contribution Collectability
In this pilot study conducted collection of dues
through the placement of promoter agencies BPJS
Health in some sub-districts which has been
established into the intervention area of study. In
each city, six sub-districts have participating
households in the largest informal worker group. In
the sub-district, each village was selected to
intervene. In each village a promoter agent is placed,
with one type between individual promotional
agents, promoter agencies working with FKTP and
promoter agencies in collaboration with village
officials.
To see the level of contribution collectability, the
researcher uses the respondent analysis unit is the
individual with a total of 7856 individuals
participating in the informal sector members who
participated as the respondents of this pilot project
actively through the promoter agent. This number
consisted of 4,282 individuals participating in
informal sector members in Semarang, Central Java
(54.5%) and 3574 members in Balikpapan, East
Kalimantan (45.5%).
In Semarang, respondents with informal sector
members who chosen third class of services were the
most participants (44%) except in Tlogosari Kulon
(30%) and the lowest participants chose first class
(19%). The amount of delinquency against total
participants at the baseline was 31% and increased
by 17% to 48% on the end-line. Participants who
chose first class of services became the highest
arrears followed by 2
nd
and 3
rd
class. In the baseline
data, villages with the highest total arrears were
Pudak Payung (38%) and lowest Krobokan (22%).
Then when viewed on the end-line data, the highest
arrears remain in Pudak Payung (54%) and lowest
Tlogosari (39%) and Krobokan (40%).
The rate of contribution collectability in the
Balikpapan city intervention area showed that
respondents in the informal sector members with the
third class of services were the largest participants
(61%) and the same for all villages, while the lowest
Piloting Collection Model of Health Insurance Contributions for Informal Sector Members
245

participants were in 1
st
class (16%) except in Batu
Ampar village by 23 %. Total Arrears to total
participants at the 24% baseline increased 22% to
45% on the end-line. Participants with 3
rd
class
(23.54%) became the highest arrears and followed
by 2
nd
class and 3
rd
class of services. The highest
arrears on baseline were Batu Ampar village (36%)
and lowest Karang Rejo (19%) became the lowest
percentage of influence was Karang Joang (18%).
4 DISCUSSION
Based on the result of chi square test with 95%
confidence level, it is found that the condition of the
respondent when registering as a participant of BPJS
Health in Semarang has an effect on the incidence of
arrears (P value = 0,002) with the highest proportion
57,9% respondents in this city registered in sick
condition. Respondents in sick conditions tended to
have dues delinquency, they do not continue to pay
dues when they have received services and returned
to health. This is allegedly because participants who
enrolled in good health tended to have sufficient
knowledge of the concept and philosophy of health
insurance for their lives, while those in sickness
tended to register due to their current needs. This
variable does not provide a meaningful relationship
to contribution in Balikpapan, however there is an
odds ratio value that can illustrate the role of this
variable against the risk of contributions arrears.
From the results of the odd ratios, the households of
informal workers in Semarang who are underwriters
are enrolled and / or their members are sickly, 2.1
times are at higher risk of delinquent JKN
contributions compared to those enrolled when they
are healthy. While in Balikpapan, informal sector
household whose underwriters are enrolled and/ or
their family members are sick, 1.4 times higher risk
of arrears JKN contributions compared to those
enrolled when healthy.
The contribution delinquency in Balikpapan also
was affected by number of family member (p values
0.000) and the highest proportion is households with
more than three persons in one family. So,
households with more than three persons in family
2.8 times higher risk of arrears JKN contributions.
Besides that, in Semarang the presence of
elderly has a significant relationship with the
incidence of arrears (P value = 0.0001), as well as in
the city of Balikpapan (P value = 0.0001). Therefore,
the informal sector households with elderly
household members or underwriters are heads of
families over the age of 58 should receive
government assistance. Not only about the
ownership of the elderly in the household, the
arrears of contribution in the informal sector
members in Balikpapan is also affected by the
ownership of children under five (P value = 0.006).
Toddlers are also a group of people who are
vulnerable to health problems from outside so that
the risk of exposure by disease agents to be high.
From the socioeconomic point of view, the
informal employment households in Semarang who
have catastrophic rates have a significant
relationship with incidents of arrears (P value =
0.034), as well as respondents in Balikpapan (P
value = 0.008).
Based on the intervention of the promoter agent,
it can be seen that the type of promoter agent has a
significant effect on delinquency status of informal
sector members in Semarang City with p values
0.000 and the proportion of participants in the lowest
arrears is the individual promoter agent of 37.5%.
Based on the analysis of multivariate regression,
participants of informal workers are supervised by
agents promoters working with primary health care
is 1.4 times more at risk for delinquent dues than
agents promoter individually while participants of
the informal workers who scouted agent promoter
who worked with village officers at risk 1.7 times
greater for delinquent JKN contributions compared
to individual promoter agencies.
Meanwhile, in Balikpapan the lowest proportion
of participants in arrears exists in individual
promoter agent by 44.4%. Based on a regression
analysis, informal sector members who had
supervised by promoter agent working with health
facilities and village officials 1 times greater risk of
delinquency than individual promoter agent.
One of the achievements of the promoter
agency's performance is the role of the agent in
maintaining the level of college participants'
collective contribution, both routine and routine (not
in arrears). Below shows the result that the presence
of a promoter agency in the middle of the informal
worker of BPJS Health in Semarang made almost
61% of the informal workers' households of the pilot
project participants still pay regularly. While in the
control area, where the fee payment model is
passively conditioned on the basis of the existing
payment channel, there are 30.77% of the informal
worker's households who remain delinquent in
payment of their health insurance contributions.
While in Balikpapan, the presence of promoter
agency in the middle of informal sector members of
BPJS Health keeps more than 50% of informal
sector households routinely pay from informal
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
246

workers. Whereas in the control area, where the fee
payment model is passively conditioned on the basis
of the existing channelling payment channel
(existing channel), there are 22.54% of the informal
worker's households who remain delinquent
payment of their health insurance contributions.
In terms of cost ratio in the implementation of
contribution collection by promoter agent, it can be
seen that the model of individual promoter agent in
Semarang City has the lowest cost ratio that is 1.57
whereas the biggest cost ratio in Semarang City is
promoter agent in cooperation with village officer
with the amount of 2.44. In the city of Balikpapan,
lowest expense ratio is the promoter agent who
cooperated with village officials with a ratio of 3.51
while the ratio of the largest costs in Balikpapan is
the agents who cooperate with healthcare facilities
with the amount of 3.98.
5 CONCLUSION
1. In general, all areas of both intervention and
control occur to increase arrears;
2. The effectiveness of models differs between two
areas: Individual Agent Model is more
meaningful in Semarang. While Balikpapan
does not have a meaningful model in the
increase of collectability;
3. Costs ratio is greater than the benefits so that
the cost of benefits is not efficient;
4. There is no general profile of agents that can
indicate performance fee collection: Semarang:
women and agents as main income, while in
Balikpapan: Male, age above 30 years, married,
has experience and this job as the main income.
5. Profile agent required to perform their functions
are have active experience in social activities so
that they can formulate strategies in the field;
having a high social spirit and good
communication skill; know the area very well,
so it can map the participants quickly and can
be accepted by the local community well.
6. The main obstacle is the presence of household
heads who are hard to find because of work
and are not willing to meet, the difficulties of
the agents coming to the night especially for
the female agent, for the housing area are not
given access to meet the families of informal
worker participants, resident participants, and
in rural areas difficult geographically
reachable.
REFERENCES
DJSN. 2012. Peta Jalan Menuju Jaminan Kesehatan
Nasional Tahun 2012-2019.
Fraenkel, Jack R dan Norman E. Wallen. 2006. How
to Design and Evaluate Research in Education.
New York: McGraw-Hill Inc.
Green, L. The PRECEDE-PROCEED Framework.
Retrieved March 21, 2016, from Faculty of
Medicine, Ottawa University:
http://www.med.uottawa.ca/courses/epi6181/im
ages/PRECEDE.pdf
Hasbullah Thabrany, Materi Sosialisasi Jaminan
Kesehatan, FKM UI, 2013.
ILO., 2009. Memperluas Cakupan Jaminan Sosial
Bagi Pekerja Sektor Perekonomian Informal. ILO.
(2010). Jaminan Sosial Bagi Tenaga Kerja di
Sektor Perekonomian Informal di Indonesia.
Kusumasari, A., & Widiastuti, N. E., 2013.
Kesadaran Wajib Pajak dari Sudut Tingkat
Pendidikan, Jenis Pekerjaan, Tingkat
Penghasilan, dan Moderenisasi Sistem
Perpajakan. Prosiding Simposium Perpajakan
Nasional 4. Jakarta.
Kwon, Soonman. 2008. Thirty Years of National
Health Insurance in South Korea: Lessons for
Achieving Universal Health Care Coverage.
http://heapol.oxfordjournals.org/
Law no. 24 Year 2011 on the Social Security
Administering Agency (BPJS).
Law no. 40 of 2004 on the National Social Security
System (SJSN). Law no. 3 Year 2011 on Fund
Transfers. World Bank. (2010). Employment
Reports in Indonesia
Margono, S., 2005. Metodologi Penelitian
Pendidikan. Jakarta: PT. Rineka Cipta
Pemaparan “Progress Kepesertaan BPJS Kesehatan
Sektor Informal” oleh Plt Direktur Perencanaan
Pengembangan dan Manajemen Risiko BPJS
Kesehatan, 13 Januari 2016 di Jakarta
Peraturan Presiden Nomor 111 tahun 2013 tentang
Jaminan Kesehatan.
Sedarmayanti and Syarifudin Hidayat. 2002.
Research methodology. Bandung: Mandar
Swaminathan 2009. Measuring The Informal
Economy in Developing Countries.
Zuriah, Nurul. 2006. Social and Educational
Research Methodology. Jakarta: Earth Literacy
Piloting Collection Model of Health Insurance Contributions for Informal Sector Members
247
