
Comparing National Health Financing Strategies Amidst Increasing
Mobility Within ASEAN: Lessons from the Philippines and Indonesia
Jaifred Christian F. Lopez
1
, Ryan Rachmad Nugraha
2
, Don Eliseo Lucero Prisno III
3
1
Associate, Office of Research and Innovation,
San Beda College, 638 Mendiola St. San Miguel, Manila, Philippines 1005
2
Researcher, Center for Health Economics and Policy Studies, School of Public Health,
Universitas Indonesia, Depok City, West Java, Indonesia
3
Associate Professor, Xi’an Jiao Tong-Liverpool University, Suzhou, China
jaifredlopez@gmail.com
Keywords: ASEAN integration, Health financing strategy, Migrant health, Philippines, Indonesia.
Abstract: Health needs within the Association of Southeast Asian Nations (ASEAN) are expected to become more
mobile as a result of regional integration, thus highlighting the need for a regional consensus on providing
health services to migrants, the need to equip health systems, and the need to harmonize national health
financing strategies. We propose that this harmonization can be facilitated by a contextual comparison of
national health financing strategies, guided by the framework promoted by the World Health Organization.
Using an analysis matrix that synthesized insights generated from literature, we compared the health
financing strategies of the Philippines and Indonesia, two countries with important political and
socioeconomic similarities. Results show that the strategies are predominantly inward-looking, which focus
more on providing various levels of health coverage depending on socioeconomic status and employment,
while lacking mechanisms and a program framework to cover migrants. Thus, while considering the
diversity of government structures and health system capacities within the region, there is a need to develop
a common framework for universal health coverage for migrants, which has to be included in national
health financing strategies within ASEAN.
1 INTRODUCTION
Mobility across the members of the Association of
Southeast Asian Nations (ASEAN), specifically the
free movement of migrant workers and people
engaged in business, is now at its highest and is
expected to rise further. In 2015, the number of
international migrant workers coming from within
the region amounted to 6.78 million, an increase
from 6.5 million documented in 2013 (ILO, 2015).
This development may be attributed to policy
reforms liberalizing and harmonizing the conduct of
business, trade, education, and employment in the
region, amidst efforts among the ASEAN countries
towards economic integration (ASEAN, 2016a).
Accompanying this development is the need to
plan for emerging health concerns, and achieve
universal health care (UHC), a goal that is consistent
with a strategic measure to “promote strong health
insurance systems in the region (ASEAN,. 2016b).”
In view of the regional goal to facilitate mobility,
this goal implies that ASEAN citizens can freely
move between the member countries with assurance
that their health needs are covered anywhere within
ASEAN. Confirming this implied vision is the
ASEAN Socio-Cultural Community Blueprint,
which highlights regional strategies for
socioeconomic development, and specifically
mentions the need to “provide guidelines for quality
care and support” for migrants (ASEAN, 2016b).
Difficulty in developing such guidelines is expected,
however, in view of the diversity existing among the
ASEAN countries in terms of economic
development, healthcare situation, and existing
welfare systems for migrants as shown in Table 1,
thus complicating regional efforts.
222
Lopez, J., Nugraha, R. and Prisno III, D.
Comparing National Health Financing Strategies Amidst Increasing Mobility Within ASEAN: Lessons from the Philippines and Indonesia.
In Proceedings of the 4th Annual Meeting of the Indonesian Health Economics Association (INAHEA 2017), pages 222-227
ISBN: 978-989-758-335-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
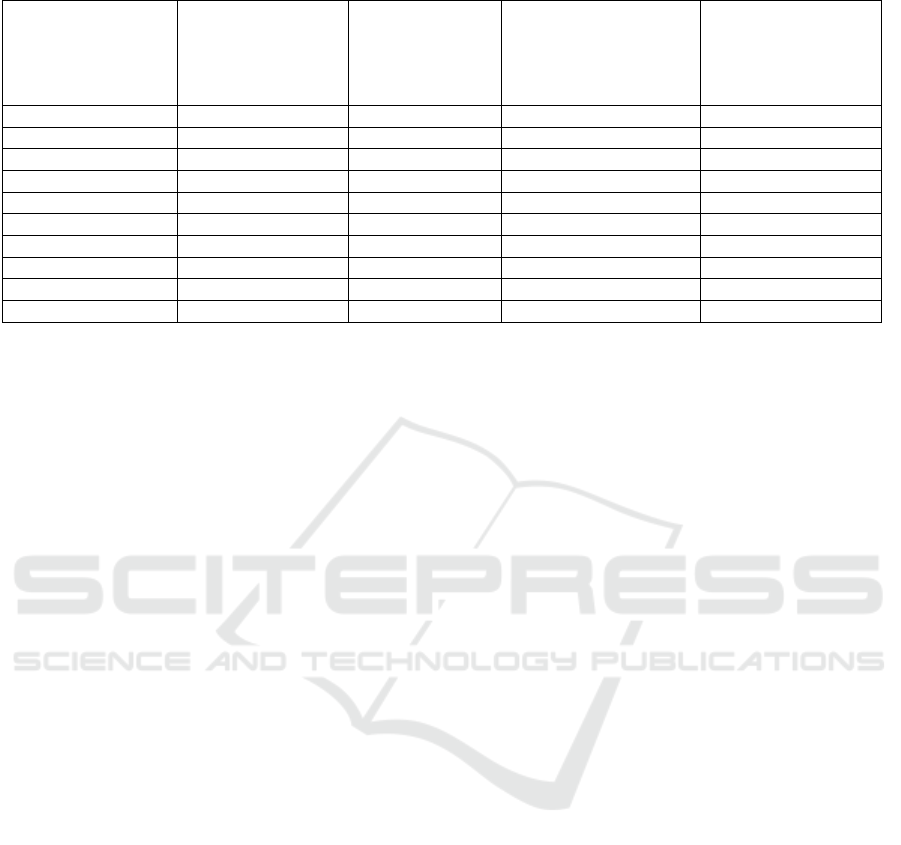
Table 1: Socioeconomic and health indicators of ASEAN member countries (Minh et al., 2014; ILO, 2015)
Population (000s),
2015
Gross National
Income per
capita, 2016*
Total government
expenditure on health as
% of general
government
expenditure, 2015
Out-of-pocket as %
total expenditure on
health, 2014^
Brunei 423 38 520 6.5 6.0
Cambodia 15 578 1 140 6.1 74.2
Indonesia 257 56
4
3 400 5.7 46.9
Lao PDR 6 802 2 150 3.4 39.0
Mala
y
sia 30 331 9 850 6.4 35.3
Myanma
r
53 897 1 190 3.6 50.7
Philippines 100 699 3 580 10.0 53.7
Sin
g
a
p
ore 5 604 51 880 14.1 54.8
Thailan
d
67 959 5 640 13.3 11.9
Vietna
m
93 448 2 050 14.2 36.8
*Determined through Atlas method, World Bank
At the national level, plans for funding UHC are
supposedly included in national health financing
strategies, which are documents that propose policy
directions and plans towards financing the health
needs of the population while preventing widespread
catastrophic health spending (Kutzin et al., 2017). In
keeping with the regional thrust to “provide
guidelines for quality care and support” for
migrants, ideally, national health financing strategies
should pave the way for providing health coverage
for outbound citizens in other ASEAN countries, as
well as addressing the health needs of incoming
ASEAN citizens. Since priority for addressing the
health needs of specific segments of the population
is most clearly manifested by how these are
considered in health policies, analyzing the national
health financing strategies of individual ASEAN
countries can provide valuable insights on
socioeconomic and political contexts that affect the
level of commitment of each member country to a
common UHC regional framework, and thus
facilitate consensus building and implementation.
However, in view of challenges present in the
region, among them the wide disparity of
socioeconomic status and the state of health care
services, this therefore leads to a hypothesis that
policies governing health needs of migrants within
the region only offer a semblance of protection
within the jurisdiction of the home country, without
considering the possibility of a region-wide scope of
health coverage.
With the aim to gather evidence on whether
national health financing strategies envisioned
region-wide coverage for migrants within the
ASEAN region in keeping with the shared goals of
“promoting strong health insurance systems in the
region,” and “providing care and support for
migrants,” this study therefore compared the
national health financing strategies of two ASEAN
countries, the Philippines and Indonesia. These
countries are the primary sources of migrants within
the region, with the aim to identify aspects that can
facilitate the implementation of a regional UHC
framework for the benefit of migrant workers and
persons engaged in business and trade. This study
also reviewed published studies and grey literature
documenting current efforts towards a regional UHC
in both countries and in the region.
2 METHODS
In comparing the two countries, we retrieved the
national health financing strategy documents
published by the Philippine Department of Health
(DOH) and the Government of Indonesia, and used
the guide for developing national health financing
strategies endorsed by the World Health
Organization (WHO) as analytical framework, from
which a comparison matrix was developed. The
WHO guide focused on the following aspects: 1)
strategic interventions, which included revenue
raising, pooling revenues, purchasing services,
benefit design, rationing and entitlement basis, and
alignment issues; and 2) governance-related
concerns, which included implementation
arrangements, evaluation and monitoring plans and
capacity building (Kutzin et al., 2017). Special
attention was given to any provision that intended to
cover migrants and other outbound citizens.
Meanwhile, using PubMed and Google Scholar, we
searched the literature for any supporting studies on
the efforts of both countries in providing health
Comparing National Health Financing Strategies Amidst Increasing Mobility Within ASEAN: Lessons from the Philippines and Indonesia
223
coverage to their outbound citizens, as well as
similar efforts in other countries within the region.
For the purposes of this review, only English
documents were analyzed.
3 RESULTS
Generally, official documents, published data and
supporting literature showed that the national health
financing strategies of both countries confirmed the
hypothesis that policies for health insurance among
migrants are predominantly inward-looking, in that
the strategies focus on expanding coverage for the
uninsured, providing benefits for dependents of
migrants, and improving the system of
reimbursements and the implementation of benefit
packages and case rates. These efforts have been
spearheaded by the Philippine Health Insurance
Corporation (Philhealth) and the Badan
Penyelenggara Jaminan Sosial (BPJS Kesehatan),
which manages the Jaminan Kesehatan Nasional
(JKN, National Health Insurance). Membership
categories exist in both countries as shown in Table
2. This is in addition to the various private health
maintenance organizations (HMOs) in both
countries that offer health services in private
facilities.
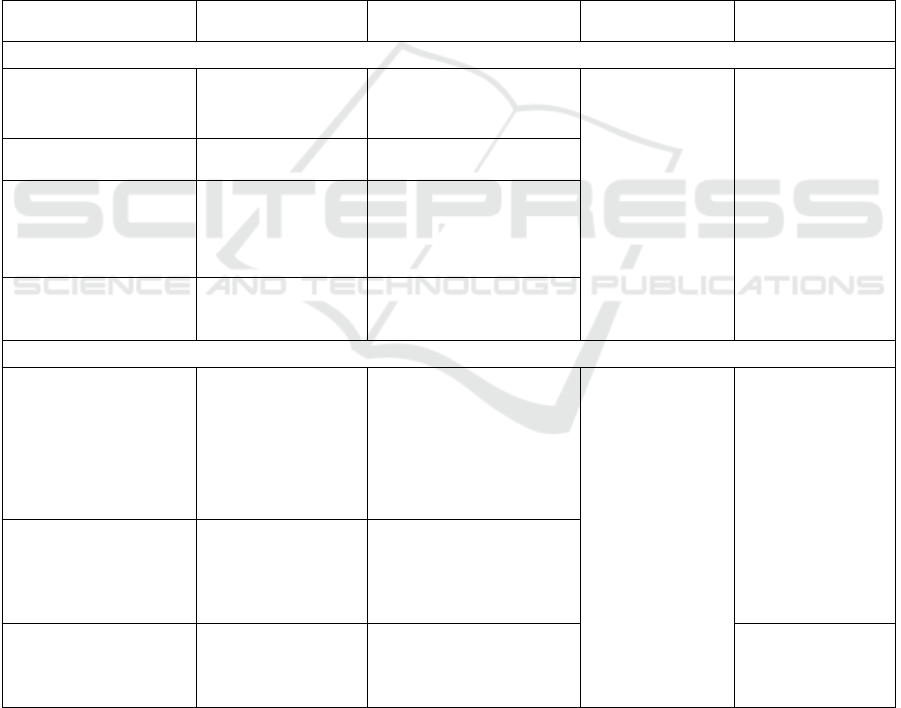
Table 2: Public health insurance membership categories in the Philippines and Indonesia (DOH, 2010; JLN, 2017; Pisani,
Kok and Nugroho, 2017)
Membership category Eligibility criteria Contribution Benefits Providers
Philippines
Formal sector (casual
and contractual)
Civil servants,
private employees,
military and police
Payroll contributions
Outpatient and
maternal care
benefit packages
(availed primarily
in accredited
facilities)
Inpatient case
rates
Philhealth-
accredited public
and private
facilities
Overseas Filipino
workers
Registered migrant
workers
Fixed premium
Informal sector
Informal workers,
independent
professionals,
foreign citizens
Voluntary payment of
fixed premium
Indigents (sponsored
program)
Certified poor
households based on
social welfare data
Shared subsidy between
local government unit and
national
g
overnment
Indonesia
Employees:
government/ private
sector
Civil servants,
entrepreneurs,
military, police
Salary deduction.
Government employees:
3% paid by employer, 2%
by employee
Private sector: 4% paid by
employer, 0.5% by
employee
Comprehensive
coverage of
outpatient and
inpatient services
Public and selected
private facilities.
Options vary
according to
premium paid
Self-employed
members
Non-poor self-
employed
Monthly premium paid by
members
Class 1: IDR 25 500
Class 2: IDR 51 500 Class
3: IDR 80 000
Subsidized members
Poor and near-poor
classified by
Ministry of Social
Affairs
Fully subsidized by
national government
Public/select
private facilities
An important difference between the two
countries is how the Philippine national health
financing strategy document specifically mentions
the importance of covering the migrant worker
population, and how the DOH acknowledges the
need to expand benefits afforded them. Meanwhile,
roadmap documents produced by the Government of
Indonesia in partnership with third-party
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
224

development agencies show that while there is an
effort in including the Ministry of Manpower and
Transmigration in consultation meetings, there is no
directly stated goal or aspiration to cover for the
health needs of migrants (JLN, 2017). Thus, for the
purposes of this study, information on covering
Indonesian migrants was retrieved from other
published studies.
In both countries, revenue raising has been
carried out through collection of premiums, either
deducted from regular salaries or voluntarily
contributed, depending on status of employment. In
all these efforts, migrants have been included
through compulsory premium payments, as in the
case of the Philhealth Overseas Filipino Program
and the Indonesian Migrant Worker Insurance
Program (Guinto et al., 2015). Moreover, risk
pooling, which affects revenue raising and the
ability of the health insurance system to purchase
health services, is affected by the fragmentation of
revenue schemes in the two countries, but strategies
have been proposed in both countries to consolidate
these schemes into a unified health insurance fund,
thus reducing fragmentation (DOH, 2010; Pisani,
Kok and Nugroho, 2017).
Additionally, in the Philippines, entitlements
have been limited in a way that prevents the
depletion of pooled funds, thus leading to the
development of benefit packages. Unfortunately,
such limitations have led to insufficient payment for
health services rendered, thus requiring out-of-
pocket payment to cover for the remaining cost. This
is in contrast to a comprehensive coverage being
offered in Indonesia, but provided in specific
facilities depending on the amount of premium paid.
In the case of migrant workers from the Philippines,
while Philhealth provides a mechanism for revenue
collection and health insurance coverage for
dependents remaining in the country and even an
expense reimbursement system for overseas health
facilities, its coverage is mostly insufficient, thus
pushing affected migrants towards catastrophic
health spending, repatriation, and eventual
impoverishment (DOH, 2010) Amidst these
emerging problems, the governments of both
countries have entered into agreements with selected
destination countries to ensure that the health needs
of migrant workers are addressed (Guinto et al.,
2015).
In summary, a system for overseas health
expense reimbursement exists for Philippine migrant
workers enrolled in the national health insurance
program while a similar program is being developed
in Indonesia, but the reality of insufficient
reimbursements highlights the need for a more
effective health financing framework that is also
funded sustainably and sufficiently.
4 DISCUSSION
Though limited by a lack of economic evaluation
and modeling, which may be the topic of a future
study, the study nonetheless presents two lessons for
discussion: 1) that the development of an effective
and sustainable regional UHC framework needs to
consider how it should equitably cover all citizens,
regardless of the economic status of their countries
of origin; and 2) that such a framework may follow
various health financing schemes adopted by similar
international and regional organizations. These
lessons lead to a common message: the need to
develop a common framework to be integrated in
national health financing strategies.
Designing a regional framework that covers both
industrialized and economically disadvantaged
countries must innovate ways to collect sufficient
revenue, create an equitable risk pool, and purchase
health services sufficiently, all while transcending
national boundaries. This leads to asking the classic
question on what kind of health financing system
should be adopted at the regional level: a “socialized
medicine” approach (Beveridge model) financed
through tax payments; a health insurance scheme
funded through salary deductions (Bismarck model);
or the National Health Insurance (NHI) model,
which combines elements of the two aforementioned
models by instituting a single payer mechanism
funded either by taxes or premiums (Wallace. As a
supranational entity, the ASEAN does not have any
authority to collect taxes, thus significantly limiting
the prospects of a socialized regional health care
financing system.
Another possibility is adopting models utilized
by international organizations for field employees.
Particularly, the United Nations offers its employees
a medical insurance plan implemented by a private
HMO through its network of accredited health care
facilities (United Nations, 2017). The ASEAN
Economic Community Blueprint seems to support
this direction as it advocated the involvement of the
private healthcare sector in efforts towards UHC and
the brokering of public-private partnerships for
health (ASEAN, 2016a).
Meanwhile, the European Union (EU), whose
model of economic integration serves as a pattern
for ASEAN, has developed a human rights-based
regional health services framework for migrants,
Comparing National Health Financing Strategies Amidst Increasing Mobility Within ASEAN: Lessons from the Philippines and Indonesia
225

guided by principles of “availability, accessibility,
acceptability and quality,” through the health-related
provisions of the 2007 Lisbon Treaty and the EU
Consolidated Treaty. These provisions encouraged
EU states to implement policies that are in keeping
with their respective interpretations of the rights
enshrined in the aforementioned treaties, while
preserving “complementarity of health services in
cross-border areas.” While these rights are upheld in
laws in both countries that implement health
insurance systems (DOH, 2010), at the regional
level, the ASEAN itself has developed a strategic
framework on health development where the health
of migrants was stated as a priority, though
regrettably this has not been translated to policy
reforms in all of the ASEAN countries (ASEAN,
2016a; Guinto et al., 2015; Government of
Indonesia, 2017; Fernando, 2011).
Given these considerations, it may thus be
appropriate that an insurance scheme similar to the
National Health Insurance model be considered as a
platform for complementarity between the health
systems of ASEAN countries, while agreeing on a
rights-based framework. The possibility of rolling
out a similar regional scheme may only be realized
through harmonized policy interventions that may
either establish a new system specifically for
ASEAN citizens, or integrate flexibly within the
existing system of the country of destination
(Nodzenski, Phua and Bacolod, 2016).
5 CONCLUSION
Therefore, considering the significant percentage of
migrant workers in ASEAN and the importance of
health coverage in ensuring sustainable economic
productivity, it is in the best interest of the region if
a regional UHC framework can be developed and
adopted, informed by a balance of economic
evaluation, consideration of how health financing
functions can be optimally implemented, and utmost
regard for human rights. Because these
considerations require substantial political will in
each of the ASEAN countries, these factors must be
made part of national-level policy discussions,
integrated in national health financing strategies for
further consideration of national level policy makers,
and included in the agenda for ministerial meetings
and in declarations being adopted in the ASEAN.
REFERENCES
Association of Southeast Asian Nations (ASEAN). 2016.
The ASEAN Economic Community Blueprint.
Available at:
http://www.asean.org/storage/images/2015/November/
aec-page/AEC-Blueprint-2025-FINAL.pdf [Accessed
30 Aug. 2017].
ASEAN. ASEAN Socio-Cultural Community Blueprint.
2016. Available at:
http://asean.org/storage/2016/01/ASCC-Blueprint-
2025.pdf [Accessed 30 Aug. 2017].
Department of Health, Philippines (DOH). 2010 Toward
Financial Risk Protection:Health Care Financing
Strategy of the Philippines 2010-2020. Health Sector
Reform Agenda – Monographs. Manila, Republic of
the Philippines - Department of Health..(DOH HSRA
Monograph No. 10)[Accessed 30 August 2017].
Fernando F. 2011. ASEAN Strategic Framework on Health
Development (2010-2015): Increase Access to Health
Services for ASEAN People. Available
at:http://www.searo.who.int/thailand/news/asean_healt
h_cooperation_increasing_access_to_health_people_d
r_ferdinal.pdf[cited 30 August 2017].
Government of Indonesia. 2017. Roadmap toward the
National Health Insurance of Indonesa (Ina
Medicare). Available
at:http://www.health.bmz.de/events/In_focus/Indonesi
a_roadmap_to_universal_health_coverage/THE_BRIE
F_EDITION_Roadmap_toward_INA_Medicare.pdf
[Accessed 30 August 2017].
Guinto R, Curran U, Suphanchaimat R, Pocock N. 2015.
Universal health coverage in ‘One ASEAN’: are
migrants included?Glob Health Action8:25749.
doi:10.3402/gha.v8.25749 [Accessed 30 August
2017].
International Labour Organization. 2015. Migration in
ASEAN in figures: the international labour statistics
(ILMS) database in ASEAN [online]. Available at:
http://www.ilo.org/wcmsp5/groups/public/---asia/---
ro-bangkok/---sro-
bangkok/documents/publication/wcms_420203.pdf[cit
ed 30 August 2017].
Joint Learning Network for Universal Health Coverage.
2017. Indonesia: Approaches to covering poor,
vulnerable, and informal populations to achieve
universal health coverage. Available at:
http://www.jointlearningnetwork.org/resources/downl
oad/get_file/ZW50cnlfaWQ6MzU0M3xmaWVsZF9u
YW1lOnJlc291cmNlX2ZpbGV8dHlwZTpmaWxl
[Accessed 30 August 2017].
Kutzin J, Witter S, Jowett M, Bayarsikhan D. 2017.
Developing a national health nancing strategy: a
reference guide. Geneva: World Health Organization;.
(Health Financing Guidance No 3) Available
at:.http://apps.who.int/iris/bitstream/10665/254757/1/9
789241512107-eng.pdf [Accessed 30 August 2017].
Minh H, Pocock N, Chaiyakunapruk N, Chhorvann C,
Duc H, Hanyoravongchai P, Lim J, Lucero-Prisno D,
Ng N, Phaholyothin N, Phonvisay A, Soe K,
INAHEA 2017 - 4th Annual Meeting of the Indonesian Health Economics Association
226

Sychareum V. 2014. Progress toward universal health
coverage in ASEAN. Glob Health Action [online], 7:
25856.doi: 10.3402/gha.v7.25856. [Accessed 30
August 2017].
Nodzenski M, Phua K, Bacolod N. 2016. New Prospects
in Regional Health Governance: Migrant Workers’
Health in the Association of Southeast Asian Nations.
Asia & the Pacific Policy Studies [online];3(2): 336–
350. doi:10.1002/app5.113 [Accessed 30 August
2017].
Pisani E, Kok M, Nugroho K. 2017. Indonesia’s road to
universal health coverage: a political journey. Health
Policy and Planning; 32:267–276.doi:
10.1093/heapol/czw120 [Accessed 30 August 2017].
United Nations. 2017. The UN Worldwide Health
Insurance Plan. [online]. Available at:
http://www.un.org/insurance/plans/un-worldwide-
health-insurance-plan[Accessed 30 August 2017].
Wallace L., 2013 .A view of health care around the world.
Ann Fam Med.; 11(1): 84. doi: 10.1370/afm.1484
[Accessed 30 August 2017].
Comparing National Health Financing Strategies Amidst Increasing Mobility Within ASEAN: Lessons from the Philippines and Indonesia
227
