
Towards Interoperability of EHR Systems: The Case of Italy
Mario Ciampi
1
, Angelo Esposito
1,2
, Roberto Guarasci
3,4
and Giuseppe De Pietro
1
1
Institute of High Performance Computing and Networking, National Research Council of Italy, Naples, Italy
2
Department of Engineering, University of Naples Parthenope, Naples, Italy
3
Institute for Informatics and Telematics, National Research Council of Italy, Rende, CS, Italy
4
Department of Linguistics, University of Calabria, Rende, CS, Italy
Keywords: Electronic Health Record, Interoperability, Architectural Model.
Abstract: The great benefits that Electronic Health Records are able to provide in terms of improvement of the quality
of care and reduction of costs have led many international organizations to implement enabling systems.
However, the systems designed and realized are very often not able to interoperate each other, due to several
reasons, varying from the existence of different local needs to the use of diverse health informatics standards.
The lack of interoperability among these systems can result in decreased levels of quality of patient care and
waste of financial resources. In Italy, the autonomy about healthcare delivered by the Italian Constitution to
each region caused the spread of heterogeneous regional EHR systems, thus not able to interoperate each
other. This paper presents the result of an effort made within a convention between the National Research
Council of Italy and the Agency for Digital Italy, for the specification of the Italian architecture for the
interoperability of regional EHR systems. Such an architecture has been defined according to the requirements
provided by Italian Laws recently issued and approved by a National Technical Board.
1 INTRODUCTION
In the last decades, many countries in the world have
made significant efforts to develop Electronic Health
Record (EHR) systems (Aminpour et al., 2014). The
main reasons are: i) improving the quality of care
services, and simultaneously ii) reducing health care
costs (Black et al., 2011; Shekelle et al., 2006). ISO
defines EHR as a “repository of patient data in digital
form, stored and exchanged securely, and accessible
by multiple authorized users”. It contains
retrospective, concurrent and prospective information
and its primary purpose is to support continuing,
efficient and quality integrated health care (ISO/TR
20514, 2015).
Despite such efforts in the realization of EHRs,
the systems developed, both at regional and national
level, are very often not able to interoperate each
other (Ludwick and Doucette, 2009), due to a
plethora of reasons. First, each country or regional
domain is characterized by its own legal
requirements, especially about privacy protection.
Second, countries or regions have typically different
needs, depending on their dimension, number of
citizens, number of healthcare facilities, etc. Finally,
the development of the systems have been started in
different periods, adopting or applying diverse
standards in different ways (Dogac et al., 2007).
The lack of interoperability among these systems
can result in decreased levels of quality of patient care
and waste of financial resources. In fact, when a
patient benefits from a health service outside her/his
health care domain, the health professional that treats
the patient is not able to access the patient health
information, due to the impossibility of cooperation
between the EHR system used by the health
professional and the one related to the patient.
Therefore, the health professional typically requires
the patient to repeat a clinical exam already executed.
With respect to interoperability, several levels of
interoperability have been defined in literature (Kalra
et al., 2007): technical interoperability, for which the
systems share the communication protocols making
possible, e.g., the exchange of bytes between them;
syntactic interoperability, which aims at making the
systems capable of communicating and exchanging
data through the sharing of data formats; semantic
interoperability, whose purpose is to enable systems
to exchange data and interpret the information
exchanged in the same way; organizations & services
Ciampi, M., Esposito, A., Guarasci, R. and Pietro, G.
Towards Interoperability of EHR Systems: The Case of Italy.
In Proceedings of the International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2016), pages 133-138
ISBN: 978-989-758-180-9
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
133

interoperability, where business processes are shared
between the systems.
The importance of making EHR systems able to
interoperate each other has motivated by the increase
of the phenomenon of the patient mobility for reasons
of care. For example, we can consider Italy where
570k hospitalizations are made by patients in a region
different from that they reside (Istat, 2015).
In Italy, the autonomy about healthcare delivered
by the Italian Constitution to each region caused the
spread of heterogeneous regional EHR systems. After
some national initiatives aimed at proposing a first
architectural model at national level, the emanation of
Italian norms has allowed defining both i) the national
architectural model of reference, and ii) the functional
and privacy requirements to be respected by all the
Italian regions. In this scenario, this paper presents
the Italian architecture designed for the
interoperability of EHR systems by a National
Technical Board, coordinated by the Agency for
Digital Italy (AgID) and the Ministry of Health, with
the technical support of the National Research
Council of Italy (CNR) and the participation of the
Ministry of Economy and Finance and Italian regions.
This paper is organized as follows. Section 2
provides a background on the main standards and
projects on e-health data interoperability. Section 3
describes the main features of the national
interoperability architecture, highlighting the cross-
border business processes. Section 4 presents the
technical details about the architecture. Finally,
Section 5 concludes the paper with some final
remarks and indications for future works.
2 BACKGROUND
2.1 Health Informatics Standards
HL7 is a non-profit organization involved in the
development of international health informatics
interoperability standards. Version 2 of the standard
is currently implemented in numerous health
organizations, whereas Version 3 is based on an
object-oriented model named Reference Information
Model (RIM). From the RIM, it was derived the
Clinical Document Architecture (CDA) standard,
which specifies the structure and semantics of clinical
documents. Currently, HL7 is involved in the
definition of a new health interoperability standard,
named FHIR, which combines the best features of the
previous versions (HL7 [online], 2016).
IHE is an international initiative founded by
RSNA and HIMSS with the goal of supporting the
integration of health information systems through
existing standards. IHE constantly defines integration
profiles, which aim to solve problems related to
specific use cases. In this context, the profile more
relevant in the IT Infrastructure domain is XDS,
which has the scope of facilitating the sharing of
patient electronic health records across health
enterprises (IHE [online], 2016).
2.2 International and National Projects
Canada Health Infoway is an independent, federally-
funded, not-for-profit organization with the
responsibility of accelerating the adoption of digital
health solutions across Canada. Along with the
Canadian provinces and territories, Infoway provided
a national framework called EHR Blueprint, with the
aim of guiding the development of the systems in
each different province. The key elements of the
framework, built following a Service-Oriented
Architecture (SOA) based on the HL7 Version 3
standard, are: gateways, data repositories, registry
services, infostructure, access mechanisms (Canada
Health Infoway [online], 2016).
U.S. Healtheway (now Sequoia) is a non-profit,
public-private partnership that operationally supports
the eHealth Exchange project. With production
starting in 2007, eHealth Exchange has become a
rapidly growing community of public and private
organizations, with the aim of facilitating the
exchange of health information in a trusted, secure,
and scalable manner. The exchange is realized
through Web Services conforming to specifications
based on IHE integration profiles. Finally, in order to
support the health information exchange at local and
national level, an open-source software named
CONNECT has been developed (The Sequoia Project
eHealth Exchange [online], 2016).
In Europe, each country has developed or is
developing its national EHR system. The aim of the
epSOS project, which involved 25 different European
countries, was to realize a large-scale pilot testing the
cross-border sharing of two kinds of health
documents: patient summary and electronic
prescription. To achieve such an objective, a service
infrastructure was designed, built, and evaluated. The
national EHR systems communicate each other by
means of gateways, named National Contact Points
(NCPs), by exchanging: i) messages based on IHE
specifications, and ii) clinical documents in the HL7
CDA format (epSOS Project [online], 2016).
In Italy, a first prototypal architectural model for
the realization of an interoperability secure EHR
infrastructure, named InFSE (Ciampi et al., 2012),
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
134

was defined and developed within three conjunct
projects between the Department of Technological
Innovation of the Presidency of the Council of
Ministers and CNR. The infrastructure, in absence of
a norm, was designed with the aim of enabling
interoperability among regional EHR systems. The
components of the infrastructure were implemented
and used in experimentations that have had the scope
of enable the interchange of clinical documents by
means of the interoperability of some regional EHR
systems. The software components of the InFSE
infrastructure were also used within the national IPSE
project linked to epSOS, in which 10 Italian regions
were involved. The aim of the project was to make
regional EHR systems able to interoperate each other
for the interchange of patient summaries.
3 NATIONAL EHR
ARCHITECTURE
In Italy, the Laws 179/2012 and 98/2013, and the
subsequent decree DPCM 178/2015 (Decree 178,
2015), have provided the Italian legal system of a
definition of EHR, meant as the set of digital health
and social-health data and documents generated from
present and past clinical events, about the patient.
According to the norms, EHR can be used for three
finalities: a) prevention, diagnosis, treatment and
rehabilitation; b) study and scientific research in the
medical, biomedical and epidemiological field; c)
health planning, verification of the quality of care and
evaluation of health care.
The regulatory framework has permitted to a
National Technical Board to define a set of reference
guidelines for the implementation of the EHR
systems (Chiaravalloti et al., 2015). Then, a set of
technical specifications, which establish the main
requirements to be met by the regions, have been
defined to guarantee interoperability at different
levels: technical interoperability is assured by
sharing communication protocols among services
interfaces; syntactic interoperability is reached by the
use of common data formats; semantic
interoperability is guaranteed by adopting both same
data formats and coding systems; organizations &
services interoperability is enabled by the sharing of
common cross-border processes.
3.1 Key Principles of EHRs
Each regional EHR system is been developing in
accordance with the requirements specified by the
norm, guidelines and specifications. The main
architectural constraints imposed are the following:
Patient Consent: every patient can take
advantage of the functionalities offered by the
EHR system of the health care provider region
of the patient. To this aim, she/he has to express
two types of consent: i) a consent enabling the
population of the EHR with her/his clinical
documents by the health facilities; ii) a consent
enabling the consultation of the EHR by health
professionals. Specifically, the patient is
allowed choosing the professional roles
permitted to access her/his EHR by defining
specific privacy policies.
Index Metadata Model: the health care
provider region of the patient has the
responsibility of mantaining index metadata
related to all the documents related to its
patients, even if such documents are produced
and maintained by health facilities sited outside
the region.
Proxy-based Interoperability Model: the
system of the health care provider region has to
operate as a mediator with the other regional
systems in all the cross-border processes in
which its patients are involved.
First Implementation of EHRs: even if EHRs
can contain a multitude of tipologies of
information, the first mandatory kinds of
clinical documents to be accessible via EHR
are patient summary and laboratory report.
Then, in this first phase, only details about the
finality of care of the patient are defined.
3.2 Cross-border Processes
In order to enable communication among regional
EHR systems, cross-border services have to be
implemented according to a SOA paradigm.
Such services have to satisfy a set of national
business processes, according to them each region
may assume a different role: the health care provider
region assumes a role named RDA; the region that
stores a document of a patient, whose RDA is
represented by another region, takes the role of RCD;
the region that provides a health service to a patient
whose RDA is another region is named RDE; finally,
the region that does not act anymore as the health care
provider region assumes the role of RPDA.
The cross-border processes, shown in Figure 1,
are based on the assumption that a health professional
intends to consult the EHR of a patient whose health
care provider region is different from the one in which
the health professional operates.
Towards Interoperability of EHR Systems: The Case of Italy
135
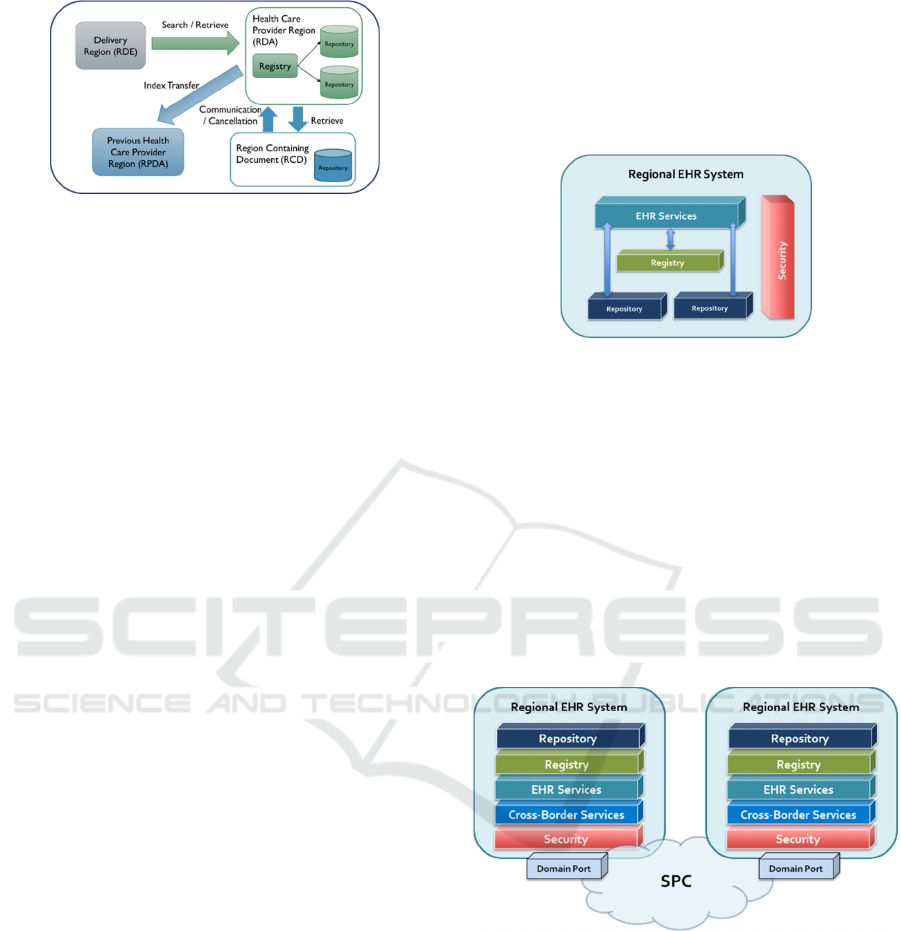
Figure 1: Roles in the cross-border processes.
All the business processes (described below),
before their execution, require to identify
preliminarly the patient and the health professional:
Searching for Documents: RDE requires RDA
to consult the EHR of the patient. RDA returns the
list of documents for which the user has access
rights.
Retrieving a Document: RDE, after obtaining
the list of documents, requires RDA retrieving a
document. RDA returns the document if the user
has access rights. Eventually, RDA forwards the
request to RCD if the document is available
outside.
Creating or Updating a Document: RDE
transmits to RDA the list of metadata of a
document created/updated for a patient of this one
(the document is stored in RDE, which therefore
serves as RCD). RDA stores the metadata in its
system.
Invalidating a Document: RCD requires RDA to
perform a logical deletion of metadata related to a
document, due to the invalidation of this one.
Transferring of Index: a new RDA requires
RPDA to transfer the index of the EHR (list of all
metadata and privacy policies) associated with the
patient. RPDA returns the index, which is
registered in the new RDA, and then disable it.
In order to achieve semantic interoperability,
several standards in different domains exists, e.g.
CIDOC-CRM (CIDOC-CRM [online], 2016) in the
cultural domain. Due to its specificity, to assure
semantic interoperability for the e-health domain,
suitable standards have been individuated: HL7 CDA
Rel. 2 specifies the structure and semantics of clinical
documents, whereas clinical content is represented by
using a set of coding systems, like ICD9-CM,
LOINC, ATC, and AIC.
3.3 Architecture Components
All the regional EHR systems are based on the
registry/repository paradigm. The clinical documents
produced by the health facilities are stored in
repositories and indexed in a regional registry by
means of appropriate metadata.
The mandatory metadata are: document type,
document state, document identifier, creation date,
author identifier, patient identifier, repository
reference.
Figure 2: Architecture of a regional EHR system.
The interoperability of the regional EHR systems
is based on a nationwide federated model, based on a
System-of-Systems approach, where each regional
system is realized by taking into account local needs.
In order to make the regional systems able to
interoperate each other, each EHR system exposes a
set of cross-border services, which preliminarly
verify the possession of the rights by the user and
provide all the functionalities needed to manage,
search, and consult metadata and documents.
The architecture of the distributed system at
national level is shown in Figure 3.
Figure 3: Architecture of the national system.
The security model adopted is based on a Circle
of Trust among the regions. Each region is
responsible for the claims made in the process of
request of the cross-border services provided by the
other regions. In addition, all the communications
among the regional systems are exchanged through
the Public Connectivity System (SPC), the Italian
technological infrastructure for exchanging
information assets and data between Public
Administrations.
Specifically, every cross-border service is linked
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
136

to the SPC infrastructure by means of specific
software components called Domain Ports.
4 TECHNICAL DETAILS
4.1 Cross-border Services
The cross-border services to be implemented
according to the business processes described above
have to be able to exchange messages compliant to
IHE XDS.b transactions, opportunely localized at
Italian level. IHE XDS profile provides specifications
for managing the exchange of documents that care
delivery organizations have decided to share.
A brief description of the structure defined for the
communication with the services is provided below:
Document Search: allows authorized users
retrieving the index metadata related to
documents satisfying specified search criteria
(patient id, date, document type and status). The
communication protocol of this service is
compliant to the IHE ITI-18 transaction (Registry
Stored Query).
Document Retrieval: allows authorized users
retrieving a specified document from its id. The
communication protocol of this service is
compliant to the IHE ITI-43 transaction (Retrieve
Document Set).
Metadata Communication: allows authorized
users sending index metadata to the health care
provider region of the patient to which a
created/updated document refers to. The
communication protocol of this service is
compliant to the IHE ITI-42 transaction (Register
Document Set-b).
Metadata Cancellation: allows authorized users
requesting logic cancellations of index metadata
relating to a document invalidated. The
communication protocol of this service is
compliant to the IHE ITI-62 transaction (Delete
Document Set).
Index Transfer: allows transferring the index of
the EHR related to a patient from a regional
system to another, after the change of the health
care provider region by the patient. The
communication protocol of this service is
compliant to the IHE ITI-18 transaction (Registry
Stored Query).
4.2 Security Aspects
The main security aspects treated concern user
identification and access control, in that issues like
integrity, confidentiality and auditing are assured by
the use of the SPC infrastructure as a secure channel
of communication among the Italian Public
Administrations.
To this aim, the claims to be transmitted by every
region in the SOAP messages exchanged among the
cross-border services are attested by digitally signed
SAML 2.0 assertions. A brief description of such
assertions is reported below:
Identification Assertion: certifies the
identification data of a patient and her/his
health care provider region; the assertion is
issued by a national Identity Provider.
Attribute Assertion: certifies the data relating
to the user making the request, the operating
environment and the type of activities to
perform; the assertion is issued by the region
that intends to use a cross-border service
offered by another region.
Identity Assertion of the RDA: certifies the
identity of the health care provider region of the
patient (RDA). This assertion, issued by RDA,
is used in case of a request sent by RDE for
retrieving a document available in RCD,
through RDA, which acts as a proxy. RCD uses
this assertion to verify if the request is really
sent by RDA.
4.3 National Framework Services
In order to support the cooperation among the EHR
systems, a national technical framework providing a
set of central services has been realized by CNR in
collaboration with AgID.
The services offered by the framework have been
identified analyzing the needs indicated by the
regions in their project plans for the realization of the
EHRs. The purposes of these services vary from
managing service endpoints, to enabling the
homogeneous presentation of the clinical documents
represented according to the XML-based HL7 CDA
format by means of national style sheets, to handling
the terminologies.
Besides, in order to support the correct
development of the cross-border services by the
regions, a test environment realizing the business
processes described above has been implemented.
Such a test environment is able to simulate the
behavior of a typical regional EHR system and allows
regional domains verifying the correctness of the
request messages for the invocation of the cross-
border services.
Towards Interoperability of EHR Systems: The Case of Italy
137

5 CONCLUSIONS
In this paper, the architectural model of reference for
the realization of the EHR in Italy was presented. The
architectural model was formalized by a National
Technical Board in order to meet the organizational,
functional, privacy, and technical requirements
provided by Italian norms recently emanated.
According to such requirements, a patient can choose:
i) whether she/he intends to benefit from the EHR
provided by her/his health care provider region, and
ii) the privacy policies that regulate the access to
her/his EHR. In order to support patient mobility,
regional EHR systems have to interoperate each other
in order to execute five main cross-border processes:
searching for documents, retrieving a document,
creating or updating a document, invalidating a
document, transferring of index. These processes are
realized by a set of cross-border services that every
regional EHR system has to make available. The
services have to be able to analyze SAML assertions
transmitted by the requesting regions in order to
verify if the user possesses the rights established by
the patient in exam. Then, some central services have
been realized and shared for supporting the
interoperability among the regional EHR systems and
the implementation of the cross-border processes. As
future work, it is planned to specify further technical
details about some relevant aspects, like digital
signatures, style sheets, patient identification. Some
critical aspects concerning the adoption of cloud
computing technologies for EHR services need a deep
investigation, in order to both i) individuate
appropriate deployment and service models, and ii)
assure suitable privacy level agreements. Finally,
additional work will concern the extension of the
architecture for executing processes able to use the
EHR for finalities of research and government, after
that a new decree will define the main requirements.
ACKNOWLEDGEMENTS
The work presented in this paper has been partially
supported by two joint projects between the Agency
for Digital Italy and the National Research Council of
Italy: “Interventions to support the realization of the
Electronic Health Record”, prot. CNR 25751/2014,
and “Realization of services of the national
interoperability infrastructure for the Electronic
Health Record”, det. AgID 61/2015.
REFERENCES
Aminpour, F., Sadoughi, F., Ahamdi, M., 2014. Utilization
of open source electronic health record around the
world: A systematic review. International Journal of
Research in Medical Sciences, vol. 19, no. 1, pp. 57-64.
Black, A. D., Car, J., Pagliari C., et al., 2011. The impact of
eHealth on the quality and safety of health care: a
systematic overview. PLOS Medicine, vol. 8, no.
e1000387.
Canada Health Infoway, 2016. https://www.infoway-
inforoute.ca/en/.
Chiaravalloti, M.T., Ciampi, M., Pasceri, E., Sicuranza, M.,
De Pietro, G., Guarasci, R., 2015. A model for realizing
interoperable EHR systems in Italy. 15th International
HL7 Interoperability Conference.
CIDOC-CRM, 2016.
http://www.cidoc-crm.org/official_release_cidoc.html
Ciampi, M., De Pietro, G., Esposito, C., Sicuranza, M.,
Donzelli, P., 2012. On federating health information
systems. GUT 2012: International Conference in Green
and Ubiquitous Technology, pp. 139-143.
Decree 178, 2015. http://www.gazzettaufficiale.it/eli/
id/2015/ 11/11/15G00192/sg.
Dogac, A., Laleci, G., Aden, T., Eichelberg M., 2007.
Enhancing IHE XDS for federated clinical affinity
domain support. IEEE Transactions on Information
Technology in Biomedicine, vol. 11, no. 2, pp.213 -221.
epSOS Project, 2016. Available at: http://www.epsos.eu/.
HL7 Int., Health Level Seven International, 2016.
http://www.hl7.org/.
IHE, Integrating the Healthcare Enterprise, 2016.
http://www.ihe.net/.
ISO/TR 20514, 2005. Health informatics -- Electronic
health record -- Definition, scope and context.
Istat, 2015. Le dimensioni della salute in Italia (Italian).
http://www.istat.it/it/files/2015/09/Dimensioni-
salute.pdf.
Kalra D., Blobel B.G., 2007. Semantic interoperability of
EHR systems. Studies in Health Technology and
Informatics, vol. 127, pp. 231-245.
Ludwick, D.A., Doucette, J., 2009. Adopting electronic
medical records in primary care: lessons learned from
health information systems implementation experience
in seven countries. International Journal of Medical
Informatics, vol. 78, no. 1, pp. 22–31.
Shekelle, P.G., Morton, S.C., Keeler, E.B., 2006. Costs and
benefits of health information technology. Evidence
Report/Technology Assessment, no. 132, pp. 1-71.
The Sequoia Project eHealth Exchange, 2016. Available at:
http://sequoiaproject.org/ehealth-exchange/.
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
138
