
Towards Improving Modeling and Simulation of Clinical Pathways:
Lessons Learned and Future Insights
Mahmoud Elbattah and Owen Molloy
National University of Ireland Galway, Galway, Ireland
Keywords: Clinical Pathways, Conceptual Modeling, Simulation.
Abstract: Clinical pathways (CPs) have been increasingly recognised as an instrumental evidence-based artifact that
can support clinical decision making and care planning. However, research focusing on modeling and
simulation of CPs is still sparse, despite significant individual endeavours. Initially, the paper conducts a
systematic literature review with the aim of thoroughly inspecting the state-of-the-art in literature. Through
the review, potential improvements are investigated with regard to the application of modeling and simulation
within CPs. In view of that, we identify four thematic areas that emphasise how research in this space can be
further developed. Specifically, we propose the following directions: i) Development of a conceptual
reference model of CPs, ii) Adoption of a multi-perspective modeling approach that can integrate clinical,
operational, financial and demographic information of CPs, iii) Development of a generic semantic-based
model of CPs, and iv) Adoption of Linked Data concepts.
1 INTRODUCTION
Healthcare services are delivered in complex
environments involving interactions among many
care providers and stakeholders. In this regard,
numerous studies (Lowery et al., 1994; Lowery et al.,
1996; Harper et al., 2004; Brailsford et al., 2005,
Eldabi et al., 2009) aimed at identifying the particular
profile of healthcare problems and the way modeling
and simulation studies should approach them.
However, compared to non-healthcare sectors, there
is still an obvious shortcoming with respect to the
gains of simulation modeling for healthcare in
general, and for CPs in particular. A CP was defined
as a management plan that displays goals for patients
and provides the sequence and timing of actions
necessary to achieve these goals with optimal
efficiency (Pearson et al., 1995).The significance of
CPs substantially lies in the potential to standardise
the flow of information, processes and patients
through well-designed care plans (Every et al., 2000;
Renholm et al., 2002; De Bleser et al., 2006).
In this respect, this paper seeks to identify future
directions aiming to bridge some of the gaps exposed
in the literature. The proposed directions were
developed in accordance with an exhaustive
systematic review of the literature that addressed
modeling and simulation of CPs. In general, we argue
that there is an extensive need to embrace different
methodological approaches utilising CPs towards:
i) Developing new or improved models of patient-
centred care schemes, and ii) Building data-driven
decision models that can take advantage of the
massive amounts of clinical data. In particular, four
thematic arguments are discussed calling for
expanded attention from future studies towards
improving the practice of CPs modeling and
simulation.
Further, on the premise that healthcare can avail
of potentially applicable approaches or methods from
other matured business-oriented sectors, affirmative
exemplars from supply chains are invoked in line
with some of the proposed directions. We believe that
CPs and supply chains share the same problematic
characteristics of being highly dynamic, context-
sensitive, event-driven, knowledge-intensive,
distributed executed, and having multitude of
stakeholders.
2 REVIEW METHODOLOGY
The preliminary stage of the study adhered to a
systematic literature review using methods informed
by (Booth et al., 2011). The review endeavoured to
comprehensively include state-of-the-art approaches
and methods adopted for modeling and simulation of
CPs. To the best knowledge of the authors, existing
508
Elbattah M. and Molloy O..
Towards Improving Modeling and Simulation of Clinical Pathways: Lessons Learned and Future Insights.
DOI: 10.5220/0005568405080514
In Proceedings of the 5th International Conference on Simulation and Modeling Methodologies, Technologies and Applications (SIMULTECH-2015),
pages 508-514
ISBN: 978-989-758-120-5
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)
literature lacks a similar systematic review in this
context, which was an additional motivation.
2.1 Search Strategy
Initially, we posed the five investigative questions
presented in Table 1 in order to focus the review
process. However, the review process was
significantly challenged by the multiplicity of terms
associated with CPs. Acknowledged by many studies
(Every et al., 2000; Renholm et al., 2002; De Bleser
et al., 2006; Pearson et al., 1995; Vanhaecht et al.,
2010), CPs are also termed as “Integrated Care
Pathways”, “Care Pathways”, “Critical Pathways”,
and “Care Maps”. Therefore, all those terms had to be
incorporated within the search keywords in order to
ensure comprehensiveness. Specifically, the search
was conducted using five keywords as follows: i)
Clinical pathways modeling, ii) Critical pathways
modeling, iii) Care maps modeling, iv) Integrated
care pathways modelling, and v) Care pathways
modeling. The search process targeted four major
digital libraries, which also index the proceedings of
vital conferences (e.g. Winter Simulation Conf.),
including: i) IEEE Xplore, ii) ACM Digital Library,
iii) ScienceDirect – Elsevier, and iv) SpringerLink.
Table 1: Investigative Questions and Motivations.
Question Motivation
Q1: What are the modeling
methodologies used to
conceptually model CPs?
Identify state-of-the-art
modeling methodologies
adopted for CPs.
Q2: Are there formal standards
for modeling CPs?
Identify whether there are well-
established standards to formall
y
depict CPs models.
Q3: What types of semantic-
based models were developed
for CPs?
Identify methods used to
conceptualise the knowledge
within CPs.
Q4: Is there a form of
standardised ontology develope
d
for CPs?
Identify whether there are
common ontology models used
to formalise CPs.
Q5: What are the implications o
f
CPs modeling approaches for
building simulation models?
Identify how the conceptual
models of CPs contributed to
produce simulation studies.
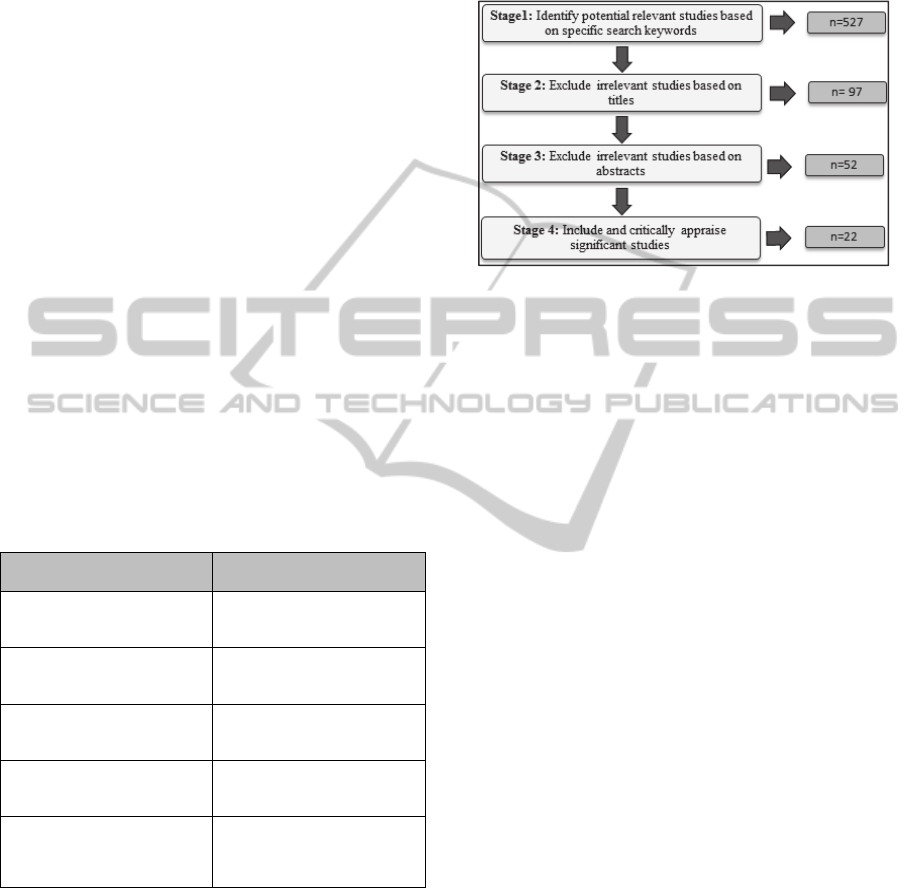
2.2 Stages of Review Process
The review process was accomplished through four
stages. Stage (1) included searching digital libraries
for potential relevant studies using the afore-
mentioned search keywords. Stage (2) excluded
irrelevant studies based on titles. Stage (3) excluded
irrelevant studies based on abstracts, including
studies that directly addressed modeling and
simulation of CPs. Stage (4) involved inclusion and
critical appraisal of the significant studies. The stages
of the review process are sketched in Figure 1, where
the number of included papers is identified at each
stage.
Figure 1: Stages of the review process.
3 PROPOSED DIRECTIONS
3.1 Development of a Conceptual
Reference Model
The role of conceptual modeling was constantly
recognised to be pivotal in simulation studies.
According to (Shannon et al., 1976), simulation
modeling is both art and science with conceptual
modeling lying more at the artistic end. Furthermore,
development of conceptual models is a necessary
phase to achieve abstraction and simplification prior
to simulation.
Nevertheless, literature obviously lacks a formal
modeling structure of CPs, acknowledged by (Yang
et al., 2012; Gupta et al., 2013; Yao et al., 2013).
Based on reviewed studies (Michalowski et al., 2006;
Zhang et al., 2008.; Li et al., 2008; Du et al., 2008;
Du et al., 2009; Alexandrou et al., 2009; Zhen et al.,
2009; Ye et al., 2009; Ozcan et al., 2011; Abidi et al.,
2012; Hashemian et al., 2012; Yao et al., 2013;
Combi et al., 2014; Braun et al., 2014), diverse
approaches exist in the area of conceptual modeling
with respect to CPs. Although those studies
contributed to investigate CPs modeling regarding
different perspectives, they are best described as case
studies, apart from few studies (Michalowski et al.,
2006; Zhang et al., 2008). Hence, we argue that
literature clearly lacks a standard formalism for the
representation of CPs in general.
In addition, there is a pronounced multiplicity of
concepts, terms and relationships within developed
CPs models, evident by the plethora of adopted
modeling methodologies. Specifically, there is no
TowardsImprovingModelingandSimulationofClinicalPathways:LessonsLearnedandFutureInsights
509

single modeling methodology or framework that
thoroughly covered all of the following issues
necessary for modeling CPs:
Comprehensively consider the various activities
of CPs including assessments, treatments, tests,
medications, hygiene and education.
Explicitly provide structured descriptions of pre-
operative, operative and post-operative activities
through treatment courses.
Enable to structure interventions with different
types of simple, atomic or composite processes or
activities.
Provide performance metrics/indicators that allow
analysis of time and resources within CPs.
In this respect, we draw attention to the need to
establish a common conceptual modeling method-
logy through the development of a reference model
for CPs. A reference model can yield many benefits
including: i) Standardise the abstraction of CPs via
progressively building consensus over concepts,
terms and process relationships of CPs, ii) Serve as a
robust base for developing ontologies or sematic-
based models, iii) Enable flexible dissemination of
good practice within stakeholders on an institutional
level, endorsed as one of the key ingredients for
successful adoption of simulation techniques (Terry,
2005), and iv) Facilitate stakeholders involvement as
a part of conceptual modelling process, recognised to
increase potentials for a successful simulation
implementation (Lehaney et al., 1995; Tako et al.,
2010).
However, development of a reference model
should take into account that healthcare-oriented
problems are better approached by forms of
resolutions and consensus (Maliapen et al., 2010). In
other words, a standard model should strike a
reasonable balance between modeling accuracy and
consensus. More importantly, a reference model can
be useful only if sustainably developed and
maintained by an active community, such as the
European Pathway Association (EPA) (e-p-a.org) for
example.
In this context, we invoke a related exemplar from
supply chains. The presented exemplar is the SCOR
(Supply Chain Operations Reference) model
(Bolstorff, 2007), regarded as one of the most widely
accepted and shared reference models for supply
chains. The SCOR model also has the advantage of
being continuously developed and maintained by the
Supply Chain Council (SCC) (apics.org/sites/apics-
supply-chain-council).The SCOR model contributed
to found a basis for building either abstract or
simulation models for supply chains in considerable
studies (Hermann et al., 2003; Haung et al., 2005;
Persson et al., 2009).
3.2 Multi-perspective Modeling
”Only by developing a well-rounded picture of the
clinical, financial and patient characteristics, it can
be possible to proactively address issues for clinical
outcomes, reducing costs, and patient satisfaction”,
emphasised by (Pol et al., 2000).
In this regard, CPs should be effectively endorsed,
whereas they were originally introduced to
comprehensively capture clinical and operational
practice through care schemes (Pearson et al., 1995;
Campbell et al., 1998; Zander, 2002). Furthermore,
the pathway-attributable economic gains were
delineated in numerous studies (Huber et al., 1998;
Pritts et al., 1999; Pitt et al., 1999; Porter et al., 2000;
Vanounou et al., 2007). For instance, (Vanounou et
al., 2007) observed an overall cost savings of $5,542
per patient using deviation-based cost modeling that
compared a pathway group of patients to another non-
pathway group. Moreover, another economic impact
of CPs was highlighted in promoting and
complementing the implementation of Diagnostic
Related Groups (DRG’s) (Collier 1997; Maliapen
2010). Consequently, CPs can and should be used as
a pro-active method to support healthcare decision
making.
However, in order to adequately depict
operational and clinical features of CPs, a multi-
perspective modeling approach should be embraced.
Particularly, CPs models should incorporate clinical,
operational, financial and demographic information.
The multi-perspective modeling of CPs can facilitate
integration within Clinical Decision Support System
(CDSS). The integration of CPs into CDSS was
considered of significant importance (Fieschi et al.,
2003; Karsh, 2009; Kawamoto et al., 2005; Wears et
al., 2005) for delivering evidence-based recommen-
dations by examining behaviour of patients and
identifying service bottlenecks.
We argue that the literature lags behind taking
advantage of integrating CPs within CDSS due to
lack of a multi-perspective view. Obviously, little
research (Cole et al., 1999; Yao et al., 2013) aimed at
modeling CPs on that basis. For instance, (Cole et
al.1999) developed a framework that considered CPs
of chronic obstructive pulmonary disease (COPD)
patients in UK. The framework incorporated CPs to
model probability of progression to multiple
readmissions, as a way to help healthcare providers in
the management of care. While another (Yao et al.,
2013) proposed a data-driven approach for decision
SIMULTECH2015-5thInternationalConferenceonSimulationandModelingMethodologies,Technologiesand
Applications
510

making to improve customisation of CPs. The
methodology applied semantic analysis and
reasoning to historical clinical data from the Navy
General Hospital in Beijing. Generally, the absence
of a multi-perspective modeling approach hampers to
conduct a robust analysis of raw healthcare data in
order to measure outcomes, cost and effectiveness of
care services.
3.3 Generic Semantic-based Modeling
It has become imperative to realise CPs-aware
healthcare systems involving the knowledge within
CPs as a centric component. In accordance with that,
the formalisation of CPs knowledge is inevitable to
attain knowledge sharing and interoperability among
heterogeneous stakeholders.
Based on literature, numerous studies (Abidi,
2009; Yang et al., 2012; Yao et al., 2013) embraced
ontology in order to develop semantic-based models
of CPs, as ontology is a formal explicit specification
of a shared conceptualization (Studer et al., 1998).
For instance, study (Daniyal et al., 2010) presented a
framework that formalised CPs using ontologies of
medical domain knowledge and workflow model,
separately. The medical domain knowledge was
captured as RDFS/OWL ontologies, while the
workflow model was described as an instantiation of
CPWMO, which is an OWL-based ontology for UML
activity diagrams. However, the framework lost sight
of the temporal relationships and variance-related
representations underlying CPs. Another important
study (Yao et al., 2013) proposed a novel framework,
referred as CONFlexFlow. The framework proposed
an integrated ontology model to capture contextual
knowledge and clinical guidelines using OWL and
SWRL rules. Additionally, adaptable clinical
processes were performed using Business Process
Execution Language (BPEL).
However, we argue that apart from very few
studies, such as (Yao et al., 2013), literature seldom
laid emphasis on developing a generic semantic
formalization of CPs. On the contrary, the produced
semantic models were mainly developed with regard
to disease-specific care plans or case studies.
Accordingly, the low-level conceptualisation of CPs
did not help to reach a semantic model that can
capture knowledge within CPs in a generic fashion.
Furthermore, semantic-based models should be
able to represent CPs in terms of: i) Common
concepts and terms of the medical domain, ii)
Structural and temporal relationships within
processes/activities, iii) Variance-related
representation, and iv) Contextual data that
characterise a specific clinical process or activity.
Literature endorsed those issues relatively
individually, and we could not identify a single
framework enabling all of them, to the best
knowledge of the authors.
3.4 Adoption of Linked Data Concepts
Healthcare-oriented problems have been always
characterised by the dilemma of process multi-
ownership and plurality of stakeholders, and CPs are
no exception. Generally, management of a patient’s
health involves dealing with a number of inter-related
CPs. Although a single CP can address a specific
clinical problem, it can be inter-dependent on
progress of other CPs.
Furthermore, the presence of “comorbidity”
through treatment schemes is an additional challenge
for CPs modeling. The term comorbidity refers to the
existence of medical conditions that concurrently co-
occur with a primary condition in the same patient
(Feinstein et al., 1970). For instance, Chronic Heart
Failure (CHF) is a common chronic condition that is
often associated with comorbidities such as Atrial
Fibrillation (AF), diabetes, chronic lung disease and
stroke (Abidi et al., 2012). Undoubtedly, the
complexity of CPs models can directly increase due
to the necessity of aligning activities/processes of
multiple disease-specific CPs, while ensuring clinical
suitability and patient safety.
However, the impacts of multiple CPs and
comorbidities have been slightly endorsed in
literature. Only studies (Abidi, 2009; Abidi et al.,
2012) considered the existence of comorbidities
within CPs. Specifically, (Abidi, 2009) presented a
framework for computerisation and merging of CPs
for comorbidities to provide point of care decision
support. The framework provided integration of
multiple CPs for comorbid diseases to realise a single
patient-specific trajectory.
In view of that, we propose the adoption of a
Linked Data approach in order to address the
challenges of multiple inter-related CPs. Generally,
Linked Data refers to a set of best practices for
publishing and connecting structured data on the Web
(Bizer et al., 2009). However, we see big chances for
CPs to avail of Linked Data practices. We argue that
knowledge within CPs can be best conceptually
conceived as Linked Data models. Particularly, the
network-based and context-intensive characteristics
of CPs information make it feasible to take advantage
of the Linked Data concepts and principles. In Figure
2, we conceive the knowledge stack of CPs models as
should be evolving towards Linked Data representa-
TowardsImprovingModelingandSimulationofClinicalPathways:LessonsLearnedandFutureInsights
511
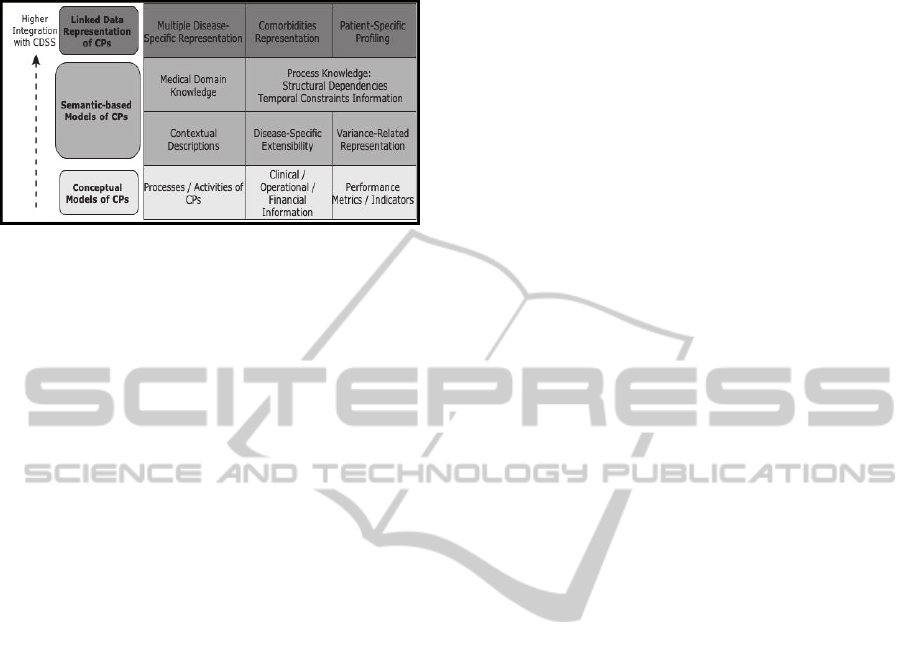
tion.
Figure 2: Knowledge stack of CP Models.
We expect the following gains by embracing Linked
Data concepts:
Realising conceptual amalgamation of knowledge
within multiple disease-specific CPs towards a
full-scale vision of a patient’s health.
Having the inter-related information of CPs in a
Linked Data form can compose a significant
powerful source of recommendations for clinical
decision making.
Storing CPs information as Linked Data can
considerably facilitate diagrammatic
representations of CPs.
Enabling potential usage of CPs knowledge in the
Open Data cloud (LOD).
Once more, we invoke an affirmative exemplar from
supply chains. A recent Study (Robak et al., 2013)
analysed the capabilities of using Linked Data
principles in business process management within
supply chains to tackle problems of information
interchange between independently designed data
systems. The study expected that the application of
Linked Data can substantially contribute to: i) Data
integration between diverse formats from the network
participants ii) Support the automated extraction of
the information.
4 CONCLUSIONS
The paper aims to convey considerations in relation
to improving the modeling and simulation of clinical
pathways (CPs). We formulate our view based on
observations and findings stemming from a
systematic literature review. A clear finding of the
review is that there is a need to establish a common
research agenda for modeling and simulation of CPs,
and for future studies to pay particular attention to fit
their research methods to the state of prior work.
Through this paper, we draw from literature a
summary of future directions as follows:
Development of a conceptual reference model for
CPs.
Adoption of a multi-perspective modeling
approach that can integrate clinical, operational,
financial and demographic dimensions of CPs.
Development of a generic semantic-based
modeling that can realise higher semantic
abstraction of CPs.
Adoption of Linked Data concepts and principles.
The paper discusses the above-mentioned directions,
and how they can considerably boost the integration
of CPs within the Clinical Decision Support System
(CDSS) in order to yield improved quality and lower
costs of healthcare services.
REFERENCES
Booth, Andrew, Diana Papaioannou, and Anthea Sutton.
Systematic approaches to a successful literature review.
Sage, 2011.
De Bleser, Leentje, Roeland Depreitere, KATRIJN DE
WAELE, Kris Vanhaecht, Joan Vlayen, and Walter
Sermeus. "Defining pathways." Journal of nursing
management 14, no. 7 (2006): 553-563.
Renholm, Marja, Helena Leino-Kilpi, and Tarja Suominen.
"Critical pathways: a systematic review." Journal of
Nursing Administration 32, no. 4 (2002): 196-202.
Every, Nathan R., Judith Hochman, Richard Becker, Steve
Kopecky, and Christopher P. Cannon. "Critical
pathways a review." Circulation 101, no. 4 (2000): 461-
465.
Pearson, Steven D., Dorothy Goulart-Fisher, and Thomas
H. Lee. "Critical pathways as a strategy for improving
care: problems and potential." Annals of internal
medicine 123, no. 12 (1995): 941-948.
Vanhaecht, Kris, Massimiliano Panella, Ruben Van Zelm,
and Walter Sermeus. "An overview on the history and
concept of care pathways as complex interventions."
International Journal of Care Pathways 14, no. 3
(2010): 117-123.
Shannon, Robert, and James D. Johannes. "Systems
simulation: the art and science." Systems, Man and
Cybernetics, IEEE Transactions on 10 (1976): 723-
724.
Gupta, Ashish, and Ramesh Sharda. "Improving the science
of healthcare delivery and informatics using modeling
approaches." Decision Support Systems 55, no. 2
(2013): 423-427.
Yang, Xian, Rui Han, Yike Guo, Jeremy Bradley, Benita
Cox, Robert Dickinson, and Richard Kitney.
"Modelling and performance analysis of clinical
pathways using the stochastic process algebra PEPA."
BMC bioinformatics 13, no. Suppl 14 (2012): S4.
Yao, Wen, and Akhil Kumar. "CONFlexFlow: Integrating
flexible clinical pathways into clinical decision support
systems using context and rules. " Decision Support
SIMULTECH2015-5thInternationalConferenceonSimulationandModelingMethodologies,Technologiesand
Applications
512

Systems 55, no. 2 (2013): 499-515.
Ye, Yan, Zhibin Jiang, Xiaodi Diao, Dong Yang, and Gang
Du. "An ontology-based hierarchical semantic
modeling approach to clinical pathway workflows."
Computers in biology and medicine 39, no. 8 (2009):
722-732.
Hashemian, Nima, and Syed Sibte Raza Abidi. "Modeling
clinical workflows using business process modeling
notation." In Computer-Based Medical Systems
(CBMS), 2012 25th International Symposium on, pp. 1-
4. IEEE, 2012.
Zhen, Hu, Jing-Song Li, Yu Hai-yan, Zhang Xiao-guang,
Muneou Suzuki, and Kenji Araki. "Modeling of
Clinical Pathways Based on Ontology." In IT in
Medicine & Education, 2009. ITIME'09. IEEE
International Symposium on, vol. 1, pp. 1170-1174.
IEEE, 2009.
Li, Weizi, Kecheng Liu, Shuzhang Li, and Hongqiao Yang.
"Normative modeling for personalized clinical pathway
using organizational semiotics methods." In Computer
Science and Computational Technology, 2008.
ISCSCT'08. International Symposium on, vol. 2, pp. 3-
7. IEEE, 2008.
Alexandrou, Dimitrios, Fotis Xenikoudakis, and Gregoris
Mentzas. "SEMPATH: Semantic adaptive and
personalized clinical pathways." In eHealth,
Telemedicine, and Social Medicine, 2009.
eTELEMED'09. International Conference on, pp. 36-
41. IEEE, 2009.
Ozcan, Yasar A., Elena Tànfani, and Angela Testi. "A
simulation-based modeling framework to deal with
clinical pathways." In Proceedings of the Winter
Simulation Conference, pp. 1190-1201. Winter
Simulation Conference, 2011.
Abidi, Samina Raza, and Syed Sibte Raza Abidi. "An
ontological modeling approach to align institution-
specific Clinical Pathways: Towards inter-institution
care standardization." In Computer-Based Medical
Systems (CBMS), 2012 25th International Symposium
on, pp. 1-4. IEEE, 2012.
Du, Gang, Zhibin Jiang, and Xiaodi Diao. "The integrated
modeling and framework of clinical pathway adaptive
workflow management system based on Extended
Workflow-nets (EWF-nets)." In Service Operations
and Logistics, and Informatics, 2008. IEEE/SOLI 2008.
IEEE International Conference on, vol. 1, pp. 914-919.
IEEE, 2008.
Michalowski, Wojtek, Szymon Wilk, Anthony Thijssen,
and Mingmei Li. "Bayesian Belief Network Model of
the Radical Prostatectomy Pathway." In System
Sciences, 2006. HICSS'06. Proceedings of the 39th
Annual Hawaii International Conference on, vol. 5, pp.
92a-92a. IEEE, 2006.
Du, Gang, Zhibin Jiang, Xiaodi Diao, Yan Ye, and Yang
Yao. "Modelling, variation monitoring, analyzing,
reasoning for intelligently reconfigurable Clinical
Pathway." In Service Operations, Logistics and
Informatics, 2009. SOLI'09. IEEE/INFORMS
International Conference on, pp. 85-90. IEEE, 2009.
Combi, Carlo, Mauro Gambini, Sara Migliorini, and
Roberto Posenato. "Representing business processes
through a temporal data-centric workflow modeling
language: An application to the management of clinical
pathways." IEEE Transactions on Systems Man
Cybernetics-Systems 44, no. 9 (2014): 1182-1203.
Braun, Richard, and Hannes Schlieter. "Requirements-
based development of BPMN extensions: The case of
clinical pathways." In Interrelations between
Requirements Engineering and Business Process
Management (REBPM), 2014 IEEE 1st International
Workshop on the, pp. 39-44. IEEE, 2014.
Zhang, Yunchuan, Kecheng Liu, and Guoxi Cui.
"Consensus Forming in Clinical Pathway
Development: Norm Based Modeling and Simulation."
In Computational Intelligence for Modelling Control &
Automation, 2008 International Conference on, pp.
931-936. IEEE, 2008.
European Pathway Association (EPA), http://www.e-p-
a.org.
Young, Terry. "An agenda for healthcare and information
simulation." Health care management science 8, no. 3
(2005): 189-196.
Tako, Antuela A., Kathy Kotiadis, and Christos Vasilakis.
"A participative modelling framework for developing
conceptual models in healthcare simulation studies." In
Proceedings of the Winter Simulation Conference, pp.
500-512. Winter Simulation Conference, 2010.
Lehaney, Brian, and Vlatka Hlupic. "Simulation modelling
for resource allocation and planning in the health
sector." The Journal of the Royal Society for the
Promotion of Health 115, no. 6 (1995): 382-385.
Bolstorff, Peter. Supply chain excellence: a handbook for
dramatic improvement using the SCOR model.
AMACOM Div American Mgmt Assn, 2007.
Supply Chain Council, http://www.apics.org/sites/apics-
supply-chain-council.
Huang, Samuel H., Sunil K. Sheoran, and Harshal Keskar.
"Computer-assisted supply chain configuration based
on supply chain operations reference (SCOR) model."
Computers & Industrial Engineering 48, no. 2 (2005):
377-394.
Hermann, Jeffrey W., Edward Lin, and Guruprasad
Pundoor. "Supply chain simulation modeling using the
supply chain operations reference model." In ASME
2003 International Design Engineering Technical
Conferences and Computers and Information in
Engineering Conference, pp. 461-469. American
Society of Mechanical Engineers, 2003.
Persson, Fredrik, and Mirko Araldi. "The development of a
dynamic supply chain analysis tool—Integration of
SCOR and discrete event simulation." International
Journal of Production Economics 121, no. 2 (2009):
574-583.
Hu, Zhen, Jing-Song Li, Tian-Shu Zhou, Hai-Yan Yu,
Muneou Suzuki, and Kenji Araki. "Ontology-based
clinical pathways with semantic rules." Journal of
medical systems 36, no. 4 (2012): 2203-2212.
Yang, Hongqiao, Weizi Li, Kecheng Liu, and Junping
Zhang. "Knowledge-based clinical pathway for medical
quality improvement. " Information systems frontiers
TowardsImprovingModelingandSimulationofClinicalPathways:LessonsLearnedandFutureInsights
513

14, no. 1 (2012): 105-117.
Daniyal, Ali, and Syed Sibte Raza Abidi. "Semantic Web-
based modeling of Clinical Pathways using the UML
Activity Diagrams and OWL-S." In Knowledge
representation for health-care. Data, processes and
guidelines, pp. 88-99. Springer Berlin Heidelberg,
2010.
Abidi, Samina Raza. "A conceptual framework for
ontology based automating and merging of clinical
pathways of comorbidities." In Knowledge
Management for Health Care Procedures, pp. 55-66.
Springer Berlin Heidelberg, 2009.
Studer, Rudi, V. Richard Benjamins, and Dieter Fensel.
"Knowledge engineering: principles and methods."
Data & knowledge engineering 25, no. 1 (1998): 161-
197.
Pol, Louis G., and Richard K. Thomas. The demography of
health and health care. Springer Science & Business
Media, 2000.
Campbell, Harry, Rona Hotchkiss, Nicola Bradshaw, and
Mary Porteous. "Integrated care pathways." BMJ:
British Medical Journal 316, no. 7125 (1998): 133.
Zander, Karen. "Integrated care pathways: eleven
international trends." Journal of Integrated Care
Pathways 6, no. 3 (2002): 101-107.
Fieschi, M., J. C. Dufour, P. Staccini, J. Gouvernet, and O.
Bouhaddou. "Medical decision support systems: old
dilemmas and new paradigms? Tracks for successful
integration and adoption." Methods of information in
medicine 42, no. 3 (2003): 190-198.
Karsh, Ben-Tzion. "Clinical practice improvement and
redesign: how change in workflow can be supported by
clinical decision support." Agency for Healthcare
Research and Quality, US Department of Health and
Human Services. Publication 09-0054 (2009).
Kawamoto, Kensaku, Caitlin A. Houlihan, E. Andrew
Balas, and David F. Lobach. "Improving clinical
practice using clinical decision support systems: a
systematic review of trials to identify features critical to
success." Bmj 330, no. 7494 (2005): 765.
Wears, Robert L., and Marc Berg. "Computer technology
and clinical work: still waiting for Godot." Jama 293,
no. 10 (2005): 1261-1263.
Vanounou, Tsafrir, Wande Pratt, Josef E. Fischer, Charles
M. Vollmer, and Mark P. Callery. "Deviation-based
cost modeling: a novel model to evaluate the clinical
and economic impact of clinical pathways." Journal of
the American College of Surgeons 204, no. 4 (2007):
570-579.
Porter, Geoffrey A., Peter WT Pisters, Carol Mansyur,
Annette Bisanz, Kim Reyna, Pam Stanford, Jeffrey E. Lee,
and Douglas B. Evans. "Cost and utilization impact of
a clinical pathway for patients undergoing
pancreaticoduodenectomy." Annals of Surgical
Oncology 7, no. 7 (2000): 484-489.
Huber, Thomas S., Lori M. Carlton, T. R. Hrward, Mildred
M. Russin, Paul T. Phillips, Betty J. Nalli, Timothy C.
Flynn, and James M. Seeger. "Impact of a clinical
pathway for elective infrarenal aortic reconstructions."
Annals of surgery 227, no. 5 (1998): 691.
Pritts, Timothy A., Michael S. Nussbaum, Linda V. Flesch,
Elliot J. Fegelman, Alexander A. Parikh, and Josef E.
Fischer. "Implementation of a clinical pathway
decreases length of stay and cost for bowel resection."
Annals of surgery 230, no. 5 (1999): 728.
Pitt, Henry A., Kevin P. Murray, Helen M. Bowman, JoAnn
Coleman, Toby A. Gordon, Charles J. Yeo, Keith D.
Lillemoe, and John L. Cameron. "Clinical pathway
implementation improves outcomes for complex biliary
surgery." Surgery 126, no. 4 (1999): 751-758.
Collier, Paul E. "Do clinical pathways for major vascular
surgery improve outcomes and reduce cost?." Journal
of vascular surgery 26, no. 2 (1997): 179-185.
Maliapen, Mahendran, and B. C. Dangerfield. "A system
dynamics-based simulation study for managing clinical
governance and pathways in a hospital." Journal of the
Operational Research Society 61, no. 2 (2010): 255-
264.
Cole L and Houston S. “Structured care methodologies:
evolution and use in patient care delivery”. Outcomes
Management for Nursing Practice 1999; 3(2): 88–94.
Bizer, Christian, Tom Heath, and Tim Berners-Lee.
"Linked data-the story so far." (2009).
Robak, Silva, Bogdan Franczyk, and Marcin Robak.
"Applying big data and linked data concepts in supply
chains management." In Computer Science and
Information Systems (FedCSIS), 2013 Federated
Conference on, pp. 1215-1221. IEEE, 2013.
Lowery, Julie C., Brian Hakes, Lou Keller, William R.
Lilegdon, Kal Mabrouk, and Frank McGuire. "Barriers
to implementing simulation in health care." In
Proceedings of the 26th conference on Winter
simulation, pp. 868-875. Society for Computer
Simulation International, 1994.
Lowery, Julie C. "Introduction to simulation in health care."
In Proceedings of the 28th conference on Winter
simulation, pp. 78-84. IEEE Computer Society, 1996.
Harper, P. R., and M. A. Pitt. "On the challenges of
healthcare modelling and a proposed project life cycle
for successful implementation&star." Journal of the
Operational Research Society 55, no.6 (2004):657-661.
Brailsford, Sally. "Overcoming the barriers to
implementation of operations research simulation
models in healthcare." Clinical and investigative
medicine. Medecine clinique et experimentale 28, no. 6
(2005): 312-315.
Eldabi, Tillal. "Implementation issues of modeling
healthcare problems: misconceptions and lessons." In
Winter Simulation Conference, pp. 1831-1839. Winter
Simulation Conference, 2009.
Feinstein, Alvan R. "The pre-therapeutic classification of
co-morbidity in chronic disease." Journal of Chronic
Diseases 23, no. 7 (1970): 455-468.
Abidi, Samina, Jafna Cox, Syed Sibte Raza Abidi, and
Michael Shepherd. "Using OWL ontologies for clinical
guidelines based comorbid decision support." In
System Science (HICSS), 2012 45th Hawaii
International Conference on System Sciences, pp.
3030-3038. IEEE, 2012.
SIMULTECH2015-5thInternationalConferenceonSimulationandModelingMethodologies,Technologiesand
Applications
514
