
Architectural Key Dimensions for a Successful Electronic Health Record
Implementation
Eduardo Pinto and Ant
´
onio Carvalho Brito
INESC TEC, Faculdade de Engenharia, Universidade do Porto
Rua Dr. Roberto Frias, 4200-465 Porto, Portugal
Keywords:
Electronic Health Record, e-Health, Systems Architecture, Information Systems Architecture.
Abstract:
The availability of patient clinical data can be vital to a more effective diagnosis and treatment, by an healthcare
professional. This information should be accessible regardless of context, place, time or where it was collected.
In order to share this type of data, many countries have initiated projects aiming to implement Electronic
Health Record (EHR) systems. Throughout the years, some were more successful than others but all of them
were complex and difficult to materialise. The research involves the study of four international projects – in
Canada, Denmark, England and France – launched with the goal of fostering the clinical data sharing in the
respective countries, namely by implementing EHR-like systems. Those case studies served as data to identify
the critical issues in this area. To address the challenge of sharing clinical information, the authors believe
to be necessary to act in three different dimensions of the problem: (1) the engagement of the stakeholders
and the alignment of the system development with the business goals (2) the building of complex systems of
systems with the capability to evolve and easily admit new peers (3) the interoperability between different
systems which use different conventions and standards.
1 INTRODUCTION
Healthcare is one of the areas where new Infor-
mation Technologies (IT) caused huge impact.
Throughout the years, the society’s dynamic changed
appearing an increasing necessity for sharing clinical
information among different healthcare institu-
tions (Haux, 2006). Several projects were launched
in many countries, such as in England or Canada
for instance, with the goal of creating the well-know
Electronic Health Record (EHR) systems. An EHR
is a “longitudinal collection of electronic health
information about individual patients and popula-
tions” (Gunter and Terry, 2005). The main objective
is to provide clinical information about a patient
where it needs to be consulted, independently of its
origin or location, helping to avoid clinical errors
or duplication of efforts and resources. Usually,
these initiatives are not confined to the EHR concept.
In this sense, the last years brought an emergent
paradigm in which the patients have the control
over the information about themselves as long as
their involvement in the process also grows (Ball
et al., 2007). The Personal Health Records (PHR) –
which are systems whereby individuals can access,
manage and share their health information which
can be accessed by others in a private, secure, and
confidential environment (Connecting for Health,
2003) – are the best example of it. On the other
hand, the excess of information might be a trouble in
different situations. For that reason, some countries
adopted concepts like Patient Summary (PS) (epSOS,
2012) which is a set of information that allows an
healthcare professional to have a quick and easy
overview over a clinical history.
This research intends to understand the extent
of the challenge that constitutes the implementation
of a system like an EHR as a facilitator of clinical
data sharing among several institutions, from an
architectural point-of-view. In order to do so, four
international cases were selected: Canada, England,
Denmark and France. Basically, these projects were
selected for different reasons: Canada has a lot of
information publicly available and that stands as
official information; the English project was always a
very famous, controversial and apparently not so well
succeeded project; Denmark is known as one of the
most successful countries in this area and France has
been investing in this field for the last decade. These
case studies were analysed and dissected based on
136
Pinto E. and Carvalho Brito A..
Architectural Key Dimensions for a Successful Electronic Health Record Implementation.
DOI: 10.5220/0004867301360143
In Proceedings of the 16th International Conference on Enterprise Information Systems (ICEIS-2014), pages 136-143
ISBN: 978-989-758-027-7
Copyright
c
2014 SCITEPRESS (Science and Technology Publications, Lda.)

information from official on-line documentation and
scientific articles. Along with that, the authors expose
the current methodologies, models and technologies
that better address those challenges.
The paper starts with a description of the interna-
tional case studies and their experience of these im-
plementations at Section 2. From that analysis, the
authors extract the main challenges in these projects
and describe the state-of-the-art that allows to respond
to those challenges, at Section 3. Finally, the paper’s
conclusions are presented at Section 4.
2 RELATED WORK
Several initiatives to implement EHR projects have
been created over the years in several countries. Some
countries have achieved more than others, but the
common experience says that it stands not only as a
technological challenge, but way beyond that (Ander-
son et al., 2006; Jha et al., 2008; Protti et al., 2009).
2.1 Canada Case Study
In Canada, its First Ministers created an non-for-profit
organization called Canada Health Infoway back in
2001 and the effort would exceed 1.5 billion dol-
lars (Canada Health Infoway, 2009). In order to
guide the development of the systems in each dif-
ferent province, Infoway provided a set of princi-
ples, guides and components, called EHRS Blueprint.
EHRS Blueprint advocated the creation of a shared
reference information source that is populated by sev-
eral health-care organizations around Canada and is
maintained externally from every health-care organi-
zation (or Points of Service, as designated in EHRS
Blueprint). The Points of Service (PoS) are able to
reference or pull data from the shared repository. In
fact, there is not one single EHR, there are several
(EHRi) replicated through the country, with the same
structure, that are responsible for interacting with the
local entities (PoS). The EHRi information is stored
as copy of the original one and the EHR Blueprint
was built following a Services-Oriented Architecture.
The critiques started to raise up when one of the
Infoway’s goals of having 50 per cent of Canadians
with an electronic health record available by 2010 was
not met. McGrail et al. (McGrail et al., 2010) ar-
gued that “after billions of dollars and nearly a decade
of work by Infoway and the provinces, Canada is
well back of the electronic records pack” and that
Canada’s “laggard position is certainly not a question
of software design or lack of access to user-friendly
technologies”. On the other hand, the same study
pointed out some issues of lack of clinicians engage-
ment, e-health policy and a focus on national perspec-
tive rather than the regional one. Along with that,
six provincial auditors joined and produced a report
raising the possibility that the programme needs more
funds (Legislative Audit Offices, 2010). More re-
cently, Webster (Webster, 2011) advocated a change
of strategy following British recommendations for not
keep going with a top-down approach that is crafted
with insufficient engagement of clinical users.
2.2 Denmark Case Study
At the end of 1994 the project organisation MedCom
was created and mandated to establish a nationwide
health care data network based on the Electronic Doc-
ument Interchange (EDI) concept. The project was to
be completed within a period of two years (The Dan-
ish Ministry of Health, 1996) and was the beginning
of the Danish Health Data Network. In Denmark,
the doctors known as general practitioners serve as
the “gatekeepers” of patients to other specialists and
health professionals (Kuo et al., 2010). This context
have enhanced the message-like solution that took
place later. More than a national-wide solution, the
programme was concerned about achieving value in
the local regions by allowing fast and simple com-
munication between the different stakeholders. The
communication flow was based on six interactions,
always with the general practitioner as a nodal point:
request laboratory results from hospital; prescription
with pharmacies; reimbursement by assurance pub-
lic health care; messages to emergency community
care; radiology exams; referral and discharge infor-
mation. This approach led to a “tremendous rise in
messaging from 3 million per month in 2005 to 5
million per month in 2009 was much higher than ex-
pected” (Protti and Johansen, 2010). Denmark has a
National Patient Registry (DNPR) which has served
as a data set of hospital contacts since 1977. Despite
of being an administrative tool, the DNPR allowed the
creation of a number of shared services, including the
National Patient Index (NPI) that gathers all relevant
information about individual patients.
Some authors argue that there were two key de-
velopments that led to the success of the Danish pro-
gramme: “(1) creation of a nation-wide electronically
accessible patient summary record, and (2) creation
of a secure national health data network” (Kuo et al.,
2010). Moreover, in 2006, Edwards (Edwards, 2006)
states some critical factors that led to success, such
as: monetary incentives to the adoption of MedCom
standards; precise standards worked out with the clin-
icians; gradual approach and realistic time frames;
ArchitecturalKeyDimensionsforaSuccessfulElectronicHealthRecordImplementation
137

incentives to vendors; culture of consensus and a
project-based approach. In the late years, Denmark
has shine with the national health network (MedCom)
being “used by over 3/4 of the healthcare sector, alto-
gether more than 5000 different organizations” (Protti
et al., 2009).
2.3 England Case Study
The National Health Service National Programme for
IT (NPfIT) was initiated in 2005. It was born as the
world’s largest civil information technology project,
committing 12.4 billion pounds over 10 years (Bren-
nan, 2005). The NPfIT was made of eight specific-
purpose systems: a big and national healthcare data
repository, a national healthcare network, an elec-
tronic appointment booking system and five local ser-
vice providers covering England’s territory. In order
to implement the five local clusters, five providers
were contracted and made responsible for deliver-
ing the local services. The program defined a set of
standards, frameworks and implementation to guide
and favour the interoperability between local systems
and across them, called NHS Interoperability Toolkit
(ITK). The step-by-step maturity model was meant to
allow the organization to incrementally progress from
sharing binary data to sharing fully-coded CDA docu-
ments. The NHS Care Records contemplated two dif-
ferent types of records: 1) Summary Care Records —
records held nationally and is an implementation of
the concept known as Patient Summary; 2) Detailed
Care Records — records held locally and a more com-
prehensive record which might store data from past
exams and details, avoiding the necessity for repeat-
ing them, for example.
Since its beginning the project was the target of
many critiques. Back in 2004, John Powell advo-
cated the importance of involving the clinicians in
the changes as well as showing the value to patient
care (Powell, 2004). A report by the King’s Fund in
2007 also criticised the government’s “apparent reluc-
tance to audit and evaluate the programme”, question-
ing their failure to develop a capable strategy (Wan-
less et al., 2007). Several authors wrote about the
problems’ causes and things that could and should be
learned (Coiera, 2007; Clegg and Shepherd, 2007),
from lack of clinicians’ engagement till wrong met-
rics, weak political leadership and one-size-fits-all so-
lutions.
2.4 France Case Study
France is a country with one of the best healthcare
systems in the world, having been classified inclu-
sively as the “best health system in the world” by
the World Health Organization (WHO) in June 2000.
Following a set of initiatives in the late-nineties, in
2004 a law is approved to establish a Personal Medi-
cal Record (Dossier M
´
edical Personnel - DMP) which
aims to enable: (1) coordination of care (2) improve
quality of care (3) continuity of care. However, that
law was not only about the DMP, it had other direc-
tives to reform all the hospital sector that were “im-
portant enablers of healthcare delivery modernisation
in France” (Artmann and Giest, 2010). In 2009, the
“Rapport Fieschi” outlines semantic interoperability
as the key goal and challenge of health information
systems.
The General Practitioner (GP) assumed a criti-
cal role in the DMP, being able to access it via the
GP software or via the Internet but also accredited to
transfer important documents into the DMP and hide
document data upon request by the patient. Moreover,
a number of patient-centred services are also envis-
aged (Artmann and Giest, 2010): consumer portal al-
lowing the patient to access their healthcare record,
to see the list of professionals who accessed their
DMP and be informed of data updates; patient be-
ing able to manage the access rights of health profes-
sionals and update their personal information space as
well as masking data. In terms of the storage of the
EHR, France is “the best example of a country that
went with a host-based electronic health record sys-
tem” (Stroetmann et al., 2011). The French patients
are allowed to choose whichever data-host they want
for their health record. Obviously, as prescribed by
the French Decrees on Data Hosts, hosts have to be
certified in order to be allowed to store clinical infor-
mation. Another interesting fact is that, in France, an
electronic health record can only be created after the
consent of the patient (“opt-in” strategy). In terms
of standards, the French Dossier Medical Personnel
adopted the IHE standards that were combined with
the use of HL7 CDA for the Clinical Document Ar-
chitecture.
The Table 1 shows a brief summary of the four
countries presented, from an architectural perspec-
tive. There are four classification parameters: (1)
strategy - classify the process of implementation in
terms of management approach, (2) architecture - un-
derstand where it stands between the two extremes
(completely distributed or completed centralized), (3)
communication - state the approach used to allow the
share of information and (4) standards - some of the
used standards in that country either nomenclatures
or encoding ones. It is easy to understand the va-
riety of solutions that is possible to adopt only by
these four examples. In terms of strategy we have
ICEIS2014-16thInternationalConferenceonEnterpriseInformationSystems
138

Table 1: Brief summary of the four countries from an Architectural Perspective.
Canada Denmark England France
Strategy
Top-down Bottom-up Top-down Big-bang
Architecture
Distributed:
fetched in real-
time
Distributed
Hybrid: PS held
national; the rest
held locally
Distributed: host-
based, fetched in
real-time
Communication
SOA Message-oriented SOA
Document ex-
change
Standards
DICOM;
SNOMED CT;
HL7 v3; ICD10-
CA
EDI (internal);
CEN; SNOMED
CT; DICOM
HL7 CDA;
SNOMED CT
HL7 CDA; IHE
profiles; SNOMED
CT
two projects (Canada and England) that were con-
ceived from high-level to low-level contexts. By the
opposite, in Denmark the strategy sprouted from the
developments that were being made at a local level.
In terms of architecture, at least with regard to these
cases, the tendency is clear about the distribution of
the data. That is, there is not a completely centralized
repository with all the clinical data. Usually, most of
the data is held locally, where it was produced, and
some set of it is selected to be accessible in a more
centralized and easy way. In terms of communica-
tion, the solutions vary a bit, since it is possible to
find a strategy based in messages like in Denmark,
two SOA-based solutions and France relying on the
exchange of structured clinical documents. Finally, in
terms of standards we can identify SNOMED CT as
the common one, but then it is difficult to find signifi-
cant similarities.
3 KNOWLEDGE DOMAIN
MODEL
The presented case studies show that the prob-
lems/challenges vary from high-level strategy to cho-
sen standards. Despite of some of the issues discussed
are not properly architectural problems, the fact is
that all these problems are coupled, depend or affect
some-how the architectural decisions. Therefore, the
authors summarized the fundamental problems into
three research questions:
• How to maintain the closeness between the sys-
tem and the business goals guaranteeing the sys-
tem’s acceptance/adoption?
• How to build such complex and component-
crowded systems in a way they would be able to
change and evolve?
• How to make such different systems to communi-
cate and understand each other bringing forth pa-
tient care value?
3.1 Aligning the Business Goals with the
System Development
Twenty years ago, the systems complexity was grow-
ing with an exponential velocity. The software devel-
opment was facing two problems at a time: in one
hand, the systems were becoming huge and hugely
complex; on the other hand, the systems were de-
veloped with few concerns about business orienta-
tion (Sessions, 2007). At that time, the concept of
Enterprise Architecture appeared to address this prob-
lem. A lot of enterprise architecture models ap-
peared and disappeared over the years. Three of the
most known Enterprise Architecture frameworks are:
The Zachman Framework, The Open Group Archi-
tecture Framework (TOGAF) and The Federal Enter-
prise Architecture Framework (FEAF). The Zachman
Framework (Zachman, 1987) aims to guarantee that
all stakeholders’ perspectives are being taken into ac-
count when developing a complex software system.
In general terms, it is important to understand if all
the artefacts are sufficiently focused and if the ex-
isting artefacts clarify all the players, from the busi-
ness owner till the database designer, keeping all the
visions aligned. First developed in 1995, TOGAF
was based on the US Department of Defense Tech-
nical Architecture Framework for Information Man-
agement (TAFIM) (Josey, 2011). TOGAF might be
seen as a process for building an Enterprise Archi-
tecture. This framework states this building process
as a continuous process of building multiple architec-
tures from highly generic to highly specific ones, un-
til reaching the organizational architecture level (Ses-
sions, 2007). Finally, the Federal Enterprise Architec-
ture Framework appeared with the objective of serv-
ing as a platform for sharing processes, information
and documentation among the U.S. Federal Agen-
cies and other government agencies. This framework
ArchitecturalKeyDimensionsforaSuccessfulElectronicHealthRecordImplementation
139

gathers two main characteristics of the two previous:
in one hand, it defines a taxonomy – similar to the
Zachman Framework – for artefacts classification; on
the other hand, it suggests a process for building and
implementing the architecture like TOGAF does.
3.2 Architecting Complex-Crowed
Systems
The concept of Systems-of-Systems (SoS) is closely
related to this idea of achieving value through the con-
necting and integration between several peer systems.
A system is classified as an SoS when there is an
“assemblage of several components which individu-
ally may be regarded as systems” and with two ad-
ditional properties (Maier, 1998): (1) operational in-
dependence of the components – each component is
able to fully continue operating even when disassem-
bled from the system (2) managerial independence of
the components – the component systems do operate
independently in fact. Maier suggests some architec-
tural principles to deal with this kind of system like
stable intermediate forms, policy triage, leverage at
the interfaces and ensuring cooperation. In addition
to the obvious dependence of several systems, the fact
of being a complex and large kind of project also de-
serves special attention and methodologies. In this
field, the Ultra-Large-Scale Systems (Northrop et al.,
2006) and the Large-scale complex IT systems (Som-
merville et al., 2012) are two terms that refer to the
same type of systems. Independently of the desig-
nation used, these are systems identified by extreme
size in every imaginable dimension: lines of code,
stakeholders, number of systems, etc. Northrop, et
al. state some characteristics as decentralized con-
trol,“unknowable” and conflicting requirements, con-
tinuous evolution and others (Northrop et al., 2006).
If we lower the abstraction level, it makes sense
to refer some architecture styles like Service-Oriented
Architectures (SOA) and Resource-Oriented Archi-
tectures (ROA). SOA is an “architectural style that
emphasizes implementation of components as mod-
ular services that can be discovered and used by
clients” and that “emphasis on loose coupling be-
tween interacting services” (Srinivasan and Tread-
well, 2005). On the other hand, the ROA defines an
easy access to the entities as well as the way that ac-
cess should be done (Overdick, 2007).
3.3 Transforming Data into Information
Several registries are created and updated all over the
healthcare institutions. The process of transforming
that data into information is an essential step. Plus,
the share of that information creating the knowledge
necessary to offer better healthcare services is the ul-
timate challenge before creating real value to the pa-
tient. The pursuit of interoperability is not possi-
ble without a clear definition of common languages
and communication channels. In this sense, multiple
standards can be found and compared (Atalag et al.,
2010).
One of the most known organizations in this area
is Health Level Seven International (HL7), which
produced HL7 Messaging Standard. The Integrating
Healthcare Enterprise (IHE) Profiles are other exam-
ple, in this case these profiles define the systems in-
volved, the specific standards used, and the details
needed to implement the solution. Also, the Digi-
tal Imaging and Communications in Medicine (DI-
COM) is an worldwide used standard for medical
image communication, providing data structures and
services and allowing the exchange of medical im-
ages and related information. Another standard is
openEHR which develops specifications for imple-
menting full EHR systems, pronouncing more in per-
sistence as opposed to messaging, with the goal of
achieve lifelong, patient centred, secure and shareable
EHR. The standards referred above are more about
how to transfer the information. Another underlying
question is the codification of that clinical informa-
tion. In that case, the research is about terminologies
and ontologies: SNOMED CT, ICD, LOINC.
3.4 The Peer-Generated Value
Despite the healthcare arena is an old-fashion one, it
is interesting to understand how the new models of
development could fit it. As known, the businesses
are evolving from a product-oriented perspective to
a relation-oriented one. This change of paradigm
brought the client to the middle of the business, help-
ing to create value. The Metropolis Model (Kaz-
man and Chen, 2009) appears as an attempt of de-
scribing really huge complex systems built from
two basilar concepts: Open-source Software (OSS)
and Community-Based Service Systems (CBSS). The
Metropolis Model presents a new unified vision be-
tween the CBSS and the OSS, focusing deliberately
in the crowd value generation through the definition
of two levels: the kernel services and the periphery
services. In the healthcare, there is also a vast com-
munity ready to produce value and to be involved in
the improvements that need to be done. The question
is if the systems will be able to support and incentive
that contribute.
ICEIS2014-16thInternationalConferenceonEnterpriseInformationSystems
140
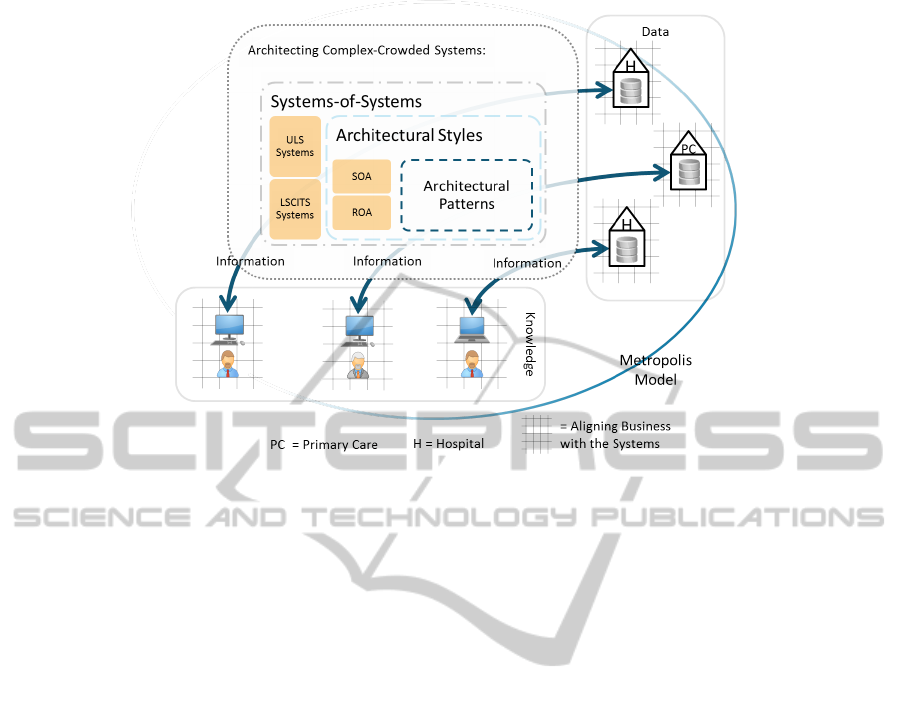
Figure 1: The Knowledge Domain Model proposed as an integrated view of the clinical data sharing domain.
3.5 Discussion
From the literature review it was possible to find some
methodologies that address a subset of the three ques-
tions. For instance, the BITAM (Chen et al., 2005)
which stands as a methodology for aligning busi-
ness and IT strategy with special focus on “detect-
ing, gauging and ameliorating the effects of misalign-
ment”. In fact, it address in broad terms the first two
concerns elicited above but does not goes into details
of interoperability questions. However, we believe
that the three dimensions are critical. The Figure 1
presents an integrated view of how all this knowl-
edge can be gathered. With it, we pretend to show
that the process of transforming the existing clinical
data into information is, in fact, a very complex pro-
cess. It starts with the production of the data at a local
level, usually in an hospital or a primary care unit. At
this level, the main concern is about aligning the sys-
tems with the healthcare processes. That alignment is
what improves the quality and quantity of data avail-
able to be shared. The next step is about fetching the
information at the local repositories and transfer or
make it available to other professionals. Obviously,
this step requires a significant effort since it can re-
quire operations like locating the origin repository or
transform the information into a codification the des-
tiny will be able to interpret. Not to mention that this
central structure might need to balance a high volume
of requests. Thus, the construction of a platform like
this requires a wide knowledge from the concepts of
Systems-of-Systems to the Architectural Patterns that
work at a much lower level, as presented in the fig-
ure. All these processes aim to transform the data
into information, which basically means to present
the data in a way and within a proper context to be
consumed by a healthcare professional. The interpre-
tation and use of that information by the professional
is implicitly transforming it into knowledge and ulti-
mately into value to the patient when the healthcare
services are improved because of that. Once again,
when providing that information to the profession-
als one big concern must be the alignment between
those systems and the processes, otherwise all the ef-
fort may be in vain.
From the analysis of the English project, it is pos-
sible to say that the first dimension might have been
overlooked. The strategy followed (top-down) im-
plies from the beginning a certain distance between
the implementation team and the local stakehold-
ers. Despite the division of the project in 5 “local
providers”, it would be necessary a much greater ef-
fort to bring clinicians and other healthcare profes-
sionals to the centre of the implementation process.
Apparently, the lack of this engagement had as conse-
quence the raising of multiple resistances either sup-
ported in the system’s existing fails or the natural in-
ertia to change and adapt. The other two dimensions
– the architecture of the hole system and the inter-
operability – appear to have been better studied. Al-
though, some articles report the appearance of criti-
cal failures which might result from architectural is-
sues. The step-by-step maturity model to the adop-
tion of fully-coded CDA documents is an example of
the importance given to interoperability, indeed evi-
ArchitecturalKeyDimensionsforaSuccessfulElectronicHealthRecordImplementation
141

denced by the existence of the NHS Interoperability
Toolkit. Most of the critiques raised against the Cana-
dian project are related to the first dimension also, ac-
cusing the responsible of insufficient engagement of
clinical users. Plus, some authors criticized the focus
on national perspective rather than the regional one
which is highly influenced by the chosen architecture.
In terms of the third dimension, the chosen standards
and the architecture based on PoS was not subject to
major criticism and seemed a good concept. In Den-
mark, the lower-profile project was built from the lo-
cal perspective to a national one, which seems to have
facilitated the engagement of the stakeholders (first
dimension). Moreover, the standards and conventions
were negotiated with the clinicians and its use was
encouraged with monetary incentives. In fact, the
strategy was able to distribute the efforts between the
three dimensions making this project one of the most
successful case studies in this area. The French case
is another example of balance between the three di-
mensions. Despite the launching in a national reform,
the responsible were able to: 1) engage the different
players of the market by fostering a solution of local
hosts 2) find an interesting solution in architectural
terms to balance the data centralization/distribution
issue 3) select and define the standards of communi-
cation (IHE profiles and HL7 CDA).
The Knowledge Domain Model presented above
refers an extra dimension which we believe can im-
prove the implementation of these projects in terms
of adoption velocity and stakeholder participation.
From the case studies referred the only one where
this dimension might have been a bit explored was
in France. In fact, the establishment of standards
and the allowance of private certified hosts for clin-
ical data storage stands as a good small example of
what a more open strategy can bring to these complex
projects.
4 CONCLUSIONS
The implementation of an EHR or a project that aims
to foster clinical data sharing in a country is a chal-
lenge that congregates wide issues, from strategy and
business processes to technology and interoperabil-
ity problems. Despite the necessary technology ex-
ists, most country healthcare systems might not seem
ready to fully exploit all its benefits.
The authors believe that these projects have three
critical dimensions: (1) keep the stakeholders en-
gaged as well as guaranteeing the system to be aligned
with the business goals, using principles of Enterprise
Architectures (2) adopt an agile architecture that is
able to gathers new peers but also to allow the sys-
tem to evolve and get better, following research in
System-of-Systems and Software Architecture (3) al-
low the institutions (peers) to effectively share clin-
ical data creating value to the patient care services,
taking advantage of the several standards and conven-
tions existing in this area. It is not about technology
that needs to be invented, it is about how one is able
to bring all this knowledge together and deliver not
the “biggest computer program in the world” but the
most valuable one. From the literature review, most
of the projects usually addressed two of the three con-
cerns referred above. The more high-level ones usu-
ally describe the components of the system and may
or may not describe the strategies to engage stake-
holders. The ones more focused on local perspectives
are usually more concerned about defining the ways
of interaction and interoperability but fail to define a
transversal strategy.
4.1 Future Work
This work is the basis for the research project in which
the authors want to specify an Architecture Frame-
work (AF) for this area of clinical data sharing at a
large scale. Thus, the next steps involve a progressive
breakdown of this model towards the creation of that
AF as a guide to the implementation of these kind of
systems. The AF is expected to: 1) describe the model
in terms of a set of building blocks 2) show how the
building blocks fit together 3) provide a common vo-
cabulary 4) include a list of recommended standards
5) include a list of compliant products that can be
used to implement the building blocks. Meanwhile, a
Quality Attribute Workshop (QAW) (Lattanze et al.,
2003) with Information Systems specialists from Por-
tuguese healthcare institutions will be organized in or-
der to validate the main strategy and the key aspects
of the model. In addition, the validation process of
the framework may include the development of a pro-
totype.
ACKNOWLEDGEMENTS
The authors would like to thank to the Portuguese
Ministry of Health, specially to SPMS which has been
always very supportive. Also, thanks to FCT for fund-
ing this research (SFRH/BD/90838/2012).
ICEIS2014-16thInternationalConferenceonEnterpriseInformationSystems
142

REFERENCES
Anderson, G. F., Frogner, B. K., Johns, R. a., and Reinhardt,
U. E. (2006). Health care spending and use of infor-
mation technology in OECD countries. Health affairs
(Project Hope), 25(3):819–31.
Artmann, J. and Giest, S. (2010). Country Brief: France.
(October).
Atalag, K., Kingsford, D., Paton, C., and Warren, J. (2010).
Putting Health Record Interoperability Standards to
Work. electronic Journal of Health Informatics,
5(1):1–17.
Ball, M. J., Smith, C., and Bakalar, R. S. (2007). Per-
sonal health records: empowering consumers. Jour-
nal of healthcare information management : JHIM,
21(1):76–86.
Brennan, S. (2005). The NHS IT project: the biggest com-
puter programme in the world - ever! Radcliffe Pub-
lishing Ltd; 1 edition (April 2005).
Canada Health Infoway (2009). Building a Healthy Legacy
Together - Annual Report 2008/2009. Technical re-
port.
Chen, H.-M., Kazman, R., and Garg, A. (2005). BITAM:
An engineering-principled method for managing mis-
alignments between business and IT architectures.
Science of Computer Programming, 57(1):5–26.
Clegg, C. and Shepherd, C. (2007). The biggest computer
programme in the world. . . ever!: time for a change
in mindset? Journal of Information Technology,
22(3):212–221.
Coiera, E. W. (2007). Lessons from the NHS National Pro-
gramme for IT. The Medical journal of Australia,
186(1):3–4.
Connecting for Health (2003). The Personal Health Work-
ing Group Final. Technical report, Markle Fundation.
Edwards, J. (2006). Case Study : Denmark’s Achievements
With Healthcare Information Exchange. Gartner In-
dustry Research Publication, (May).
epSOS (2012). epSOS: Patient Summary.
http://www.epsos.eu/epsos-services/patient-
summary.html. [Accessed: 11/11/2013].
Gunter, T. and Terry, N. (2005). The emergence of national
electronic health record architectures in the United
States and Australia: models, costs, and questions.
Journal of Medical Internet Research, 7(1).
Haux, R. (2006). Health information systems - past,
present, future. International journal of medical in-
formatics, 75(3-4):268–81.
Jha, A. K., Doolan, D., Grandt, D., Scott, T., and Bates,
D. W. (2008). The use of health information technol-
ogy in seven nations. International journal of medical
informatics, 77(12):848–54.
Josey, A. T. O. G. (2011). TOGAF Version 9.1 Enterprise
Edition. Group, pages 1–13.
Kazman, R. and Chen, H.-M. (2009). The metropolis model
a new logic for development of crowdsourced sys-
tems. Communications of the ACM, 52(7):76.
Kuo, M.-h., Kushniruk, A., and Borycki, E. (2010). Ad-
vances in Electronic Health Records in Denmark :
From National Strategy to Effective Healthcare Sys-
tem Implementation. In EFMI Special Topic Confer-
ence in Reykjavik, pages 96–99.
Lattanze, A. J., Stafford, J. A., and Weinstock, C. B.
(2003). Quality Attribute Workshops, Third Edition
(CMU/SEI-2003-TR-016). Technical Report August.
Legislative Audit Offices (2010). Electronic Health Records
in Canada - An overview of federal and provincial au-
dit reports. Technical report.
Maier, M. W. (1998). Architecting principles for systems-
of-systems. Systems Engineering, 1(4):267–284.
McGrail, K., Law, M., and H
´
ebert, P. C. (2010). No
more dithering on e-health: let’s keep patients safe in-
stead. CMAJ : Canadian Medical Association journal,
182(6):535.
Northrop, L., Feiler, P., Gabriel, R., Goodenough, J.,
Linger, R., Longstaff, T., Kazman, R., Klein, M.,
Schmidt, D., Sullivan, K., and Wallnau, K. (2006).
Ultra-Large-Scale Systems: The Software Challenge
of the Future. Software Engineering Institute,
Carnegie Mellon University, Pittsburgh, PA.
Overdick, H. (2007). The Resource-Oriented Architecture.
2007 IEEE Congress on Services (Services 2007),
pages 340–347.
Powell, J. (2004). NHS national programme for informa-
tion technology: changes must involve clinicians and
show the value to patient care. BMJ: British Medical
Journal, 328(7449):1200.
Protti, D. and Johansen, I. (2010). Widespread adoption
of information technology in primary care physician
offices in Denmark: a case study. Issue brief (Com-
monwealth Fund), 80(March).
Protti, D., Johansen, I., and Perez-Torres, F. (2009). Com-
paring the application of Health Information Tech-
nology in primary care in Denmark and Andaluc
´
ıa,
Spain. International journal of medical informatics,
78(4):270–83.
Sessions, R. (2007). A Comparison of the Top Four
Enterprise-Architecture Methodologies.
Sommerville, I., Cliff, D., and Calinescu, R. (2012). Large-
scale complex IT systems. Communications of the
ACM, 55(7):71–77.
Srinivasan, L. and Treadwell, J. (2005). An overview of
service-oriented architecture, web services and grid
computing. HP Software Global Business Unit, 2.
Stroetmann, K., Artmann, J., and Stroetmann, V. N. (2011).
European countries on their journey towards national
eHealth infrastructures. Technical Report January.
The Danish Ministry of Health (1996). A Danish Health
Care Data Network In Two Years. Technical report.
Wanless, D., Appleby, J., and Harrison, A. (2007). Our
future health secured. A review of NHS funding.
Webster, P. C. (2011). Centralized, nationwide electronic
health records schemes under assault. CMAJ : Cana-
dian Medical Association journal, 183(15):E1105–6.
Zachman, J. a. (1987). A framework for information sys-
tems architecture. IBM Systems Journal, 26(3):276–
292.
ArchitecturalKeyDimensionsforaSuccessfulElectronicHealthRecordImplementation
143
