
Effects of a Neuromuscular Reeducation Program on the Postural
Control in Gymnasts with Chronic Ankle Instability
Marc Reis
1
, Raúl Oliveira
2
and Filipe Melo
2
1
Health School of Alcoitão, Portuguese Gymnastics Federation, Lisbon, Portugal
2
Technical University of Lisbon, Human Motricity Faculty, Lisbon, Portugal
Key Words: Chronic Ankle Instability, Gymnastics, Neuromuscular Reeducation, Postural Sway, Postural Control, Time
to Stabilization.
Abstract: Chronic ankle instability (CAI) is associated to the mechanical and/or functional instability of the ankle,
being described as often residual change after sprain. Objective: To analyze the effects of a neuromuscular
reeducation program for six weeks, in postural sway (PS) and time to stabilization (TS), in functional tests,
in asymptomatic gymnasts and in gymnasts with CAI. Methods: The postural variation was evaluated –
within sample of 24 gymnasts - 9 with CAI (experimental group) and 15 healthy ones (control group)
through a pressure platform, before and after applying the exercise program. Results and Discussion: In the
instability group it was observed an improvement in PS and TS in a single limb static stance with open and
closed eyes, and after a landing of an anterior jump, medial and lateral side. In the control group a decrease
of the PS in a single-limb static stance with eyes open and after the landing of a medial side jump was
verified; improvement of the time to stabilization in the landing of lateral and medial side jump, after
applying the exercise program. Conclusion: A neuromuscular reeducation program had a positive effect in
the improvement of the postural control in gymnasts with or without CAI.
1 INTRODUCTION
Chronic ankle instability (CAI) has been described
as the most common residual change of the ankle
joint after injury (Caulfield et al., 2006). The ankle
sprain is the most common injury in professional
gymnasts (Kolt and Kirkby, 1999). According to
Yeung et al., (1994) 40% to 70% of the individuals
that suffered a ligament injury developed CAI.
CAI is one of the major residual dysfunction
after an ankle sprain, being characterized as having a
mechanic and/or functional component. Symptoms
such as experiencing joint instability (giving away),
pain and deficit in functional activities associated
with recurrent injuries, establish a CAI scenario
(Delahunt et al., 2010). This presents a multifactorial
aetiology, where factors as joint laxity, muscular
weakness and diminishing of sensibility of the
proprioceptive mechanisms are related, originating a
structural and biomechanical change in the joint,
with a consequent deficit of the postural control
when compared with healthy individuals (Denegar
and Miller, 2002; Hubbard et al., 2006; Kavanagh,
1999; Willems et al., 2002).
According to Delahunt et al. (2010) CAI is a
term used to describe individuals that portray
mechanic and functional instability of the ankle,
experience joint instability for at least one year after
the injury and that have suffered from at least two
sprains of average/mild severity in the last two to
three years.
About 45% of all ankle injuries occur in landing
after a jump (McKay et al., 2001). Individuals with
functional instability (FI) of the ankle present
changes in the standard movement before impact
with the soil in the reception of a single-limb jump
when compared with healthy individuals (Caulfield
and Garrett, 2002). These differences can occur
because of changes in the control of the standard
movement due to earlier injury (Caulfield and
Garrett, 2004) or resulting dysfunctions. Single Leg
Jump Landing (SLJL) testing has been frequently
used to assess the CAI effects in postural sway
stability (Brown et al., 2004; Wikstrom et al., 2005).
CAI has been related with an increase in the
stabilization time (ST) in the frontal and sagital
plans and several studies support this as the
responsible factor for the changes and deficits that
56
Reis M., Oliveira R. and Melo F..
Effects of a Neuromuscular Reeducation Program on the Postural Control in Gymnasts with Chronic Ankle Instability.
DOI: 10.5220/0004618000560063
In Proceedings of the International Congress on Sports Science Research and Technology Support (icSPORTS-2013), pages 56-63
ISBN: 978-989-8565-79-2
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)

occur in the jump landing (Brown et al., 2004; Ross
et al., 2005). Brown and Mynark (2007) show that
individuals with CAI take more time stabilizing after
a dynamic activity than the non-injured control
group.
Postural control is usually calculated by postural
sway, through the measure of the distance and
amplitude of the CoP´s displacement (Mattacola and
Dwyer, 2002). A decrease of the length and area of
the CoP´s displacement and a reduction of its
velocity of excursion indicate an improvement of the
efficiency of the postural control (Sefton et al.,
2009).
Several studies refer neuromuscular reeducation,
namely through platforms or unstable surface,
presenting positive results in the reintegration of the
postural control mechanisms (Mattalcola and
Dwyer, 2002; Baltaci and Kohl, 2003; Wilkerson
and Nitz, 1994).
The main goal of the present study is to analyze
the effects of a neuromuscular reeducation program
adapted to gymnastics, in postural sway and the time
to stabilization, in some dynamics or physical tests
in asymptomatic gymnasts and in gymnasts with
CAI.
2 METHODS
This is a quasi-experimental study, with a
framework of research of the pre-testing – post-
testing type with non-equivalent work group: there
was no random element distribution that belonged to
the two groups – the group of unstable subjects and
the group of healthy subjects.
The study sample is composed by 24 subjects, 9
(37,5%) males and 15 (62,5%) females; aged
between 15 and 24 years old (Average = 17,67 ±
2,85 years). It was selected by convenience out of a
population of gymnasts from Portugal’s Gymnastics
Federation and according to the following inclusion
criteria:
Experimental Group (EG): Inclusion Criteria
History of occurrence of, at least two ankle sprain
injury (grade II), from which resulted ligament
injuries with an edema/ecchymosis, pain,
temporary loss of function and that have occurred
in the last three years but more than three months
ago.
CAI history with symptoms of lack of confidence
in the joint and/or residual pain, diminished
function and momentary loss of control, even if in
minor episodes.
Experimental Group (EG): Exclusion Criteria
Ankle joint’s average gravity sprain in study in the
last three months (excludes acute and sub-acute
situations).
History of other injuries in the lower limbs (except
the ankle joint) in the six months before the data
collection and/or not totally recovered.
Neurologic symptoms or troubles.
Vestibular and visual disorders that affect the
balance.
Previous surgery history and/or lower limb
fractures.
Control Group (CG) – Inclusion Criteria
With no changes or previous injuries from the
musculoskeletal and neurologic nature in any of the
lower limbs. Asymptomatic gymnasts with no
functional or sportive limitations and in full
gymnastics activity.
The subjects were properly informed about the
study’s objectives, about all the procedures and were
only included in the sample after their formal
consent. Each subject also fulfilled an informed
permission form. In the cases when gymnasts were
underage, the form needed to be fulfilled by a tutor.
Two groups were created, the Experimental
Group (EG) – subjects with chronic ankle instability
(n=9) and the Control Group (CG) – healthy subjects
(n=15). The healthy group was randomly divided in
two sub-groups, a group of healthy individuals that
did an exercise program (n=7) – Control Group with
Exercises (CG1); and a group of healthy individuals
that was not subjected to the exercise program (n=8)
– Control Group without Exercises (CG2). All the
EG gymnasts were subjected to an exercise program.
The length and displacement area of the CoP
were measured – dependable variables, during six
seconds in the maintenance of the single limb static
stance (open and closed eyes) and after a jump’s
landing (anterior, lateral, medial). Moreover, the
first six seconds measured for each of these motor
tasks were analyzed in three distinct timeframes – in
the first two seconds (T1), from the second to the
forth seconds (T2); and from the forth to the sixth
seconds (T3). Having the concept of stabilization
time used by Ross e al. (2005) as basis and because
there is no consensus on the existing studies, about
its definition, we have approached the stabilization
time through the changes and postural oscillation
parameters’ evolution – area and length, in a
determined timeframe in comparison to other (ex.
T1_T2, which corresponds to the different values
obtained in the Cop in the timeframe T2 in
comparison to T1).
EffectsofaNeuromuscularReeducationProgramonthePosturalControlinGymnastswithChronicAnkleInstability
57

A multi-station exercise plan was developed (see
Appendix). This frames a set of seven functional
strengthening and neuromuscular re-education
exercises, to control the dynamic balance, in a series
of motor tasks and functional activities related with
gymnastic tasks, mainly the single limb standing
stance on unstable surfaces and a jump’s landing, in
order to improve the feedback and feedforward
mechanisms. Research suggests (Konradsen et al.,
1997; Holmes and Delahunt, 2009) are important
and essential in the task’s motor control and injury
prevention. The created exercise plan was performed
with a total duration of six weeks, in a frequency of
three times per week and an average duration of
15/20 minutes per session.
3 MEASUREMENT TOOLS
In this study, the postural oscillation was measured
through a 0,5m Footscan
®
pressure platform to
measure the length (mm
2
) and area (cm
2
) covered by
the CoP´s displacement to the different study tasks.
The individuals studied were also subjected to a
characterization and evaluation in the Foot and
Ankle Outcome Score (FAOS), aimed at identifying
the existing differences about pain, other symptoms,
daily life functions, sports and leisure functions and
quality of life between the subjects.
4 PROCEDURES
All the subjects were informed not to take coffee,
alcoholic drinks and medication 24 hours prior to the
evaluation, as well as trying to sleep eight hours the
night before.
According to the design of this study’s research,
there were performed two moments of evaluation,
one before the application of the multi-station
exercise program – Baseline (O1), and another, six
weeks after its application (O2). The several tasks
were evaluated on the same day, choice of the order
of tasks done randomly, and for each of them there
were made three measurements. The average of the
three results was used throughout the treatment and
interpretation of the results. In case the subject
doesn’t complete one of the measurements with
success in time, by unbalance and loss of test
position, the test will be repeated as many times as
necessary until three valid measures are obtained for
each test. In the evaluated dynamic activities, each
subject had the opportunity to perform the required
test once, before its effective measure.
To measure the postural oscillation of a jump it
was determined a priori the value of the maximum
vertical impulsion for each gymnast. After
determining this value, the jump tasks were
performed at least at 50% of the maximum vertical
impulsion, this value being marked in the space with
a rubber band and serving as a reference for the
gymnast during the jump from the floor to the
platform.
5 DATA ANALYSIS
After data collection and process was performed, the
statistical treatment was of them was given through
a SPSS for Window V.19.0 statistic treatment
software. A statistic inference was used for the data
treatment. Due to the small number of the sample,
the collected data was subjected to a statistic
treatment using non parametrical tests. For
intragroup evaluation tests were used for grouped
samples and for intergroup evaluation, tests for
independent samples - Kruskal-Wallis, to a level of
significance of p ≤ 0,05.
6 RESULTS
In Tables 1 and 2 are presented the results of the
comparison between the intragroup and the
intergroup concerning the values obtained in O1 and
O2 in CoP´s length and displacement area in the
three timeframes analyzed – from zero to two
seconds; from two to four seconds and from four to
six seconds, in maintaining the balance and after the
jump’s landing. The results presented will be just the
ones with statistical significance (p≤0,05).
In the experimental group we saw statistical
significant improvements in all the tasks being
studied concerning the CoP´s displacement and its
stabilization time. The control group that did the
neuromuscular reeducation program (GC1) showed
significant statistic results in the displacement of the
single limb static stance with the eyes open and in
the length and area of the CoP's displacement after
the landing of a medial jump. When it comes to the
stabilization time, GC1 showed more improvement
in the medial and lateral jumps' landing. For the
control group that didn't performed the
neuromuscular reeducation program (GC2), we saw
significant statistical changes in the CoP's single
limb static stance with eyes closed and after an
icSPORTS2013-InternationalCongressonSportsScienceResearchandTechnologySupport
58

Table 1: Results obtained from comparasion of the O1´s
comparison with O2 CoP´s displacement length and area,
in the different tasks analyzed, in the three groups.
TASKS EG CG 1 CG 2
SLSS_YO
A T3
(p=0,020)
A T2
(p=0,055)
----
SLSS_YC
L T3
(p=0,037)
----
L + A T1
(p=0,02;
p=0,008)
AJ
A T1
(p=0,037)
----
L + A T1
(p=0,027;
p=0,055)
LJ
L T1
(p=0,065)
L + A T3
(p=0,008;
p=0,002)
---- ----
MJ
L + A T1
(p=0,037;
p=0,027)
L + A T3
(p=0,04;
p=0,20)
L + A T1
(p=0,08;
p=0,08)
A T3
(p=0,023)
----
SLSS_YO – single limb static stance with eyes open; SLSS_YC –
single limb static stance with eyes closed; AJ – anterior jump; LJ
– lateral jump; MJ – medial jump; EG – experimental group; CG1
– control group with exercises; CG2 – control group without
exercises; A - the area of the CoP´s displacement; L – the length
of the CoP´s displacement; T1 – 0 to 2 sec; T2 – from 2 to 4 sec;
T3 – from 4 to 6 sec.
significant statistical changes in the CoP's single
limb static stance with eyes closed and after an
anterior jump's landing. Still in this group, we
verified improvement in the stabilization time after
an anterior jump.
By analyzing chart 1 we may verify that there
was a slight improvement in the score obtained by
the FAOS scale, in the EG Experimental Group,
after the exercise plan finished, at the level of the
other symptoms, sports and leisure functions and
quality of life connect to the foot and ankle. We
didn´t verify any differences by the FAOS scale,
when comparing observation 2 to 1, to the control
group with exercises (GC1).
7 DISCUSSION
SLJL tests have often been used to evaluate the
effects of FAI on the dynamic postural stability of
the ankle (Brown et al., 2004; Wikstrom et al.,
2005), and its improvement through exercise
programs in patients with CAI (Ross et al., 2005).
Several studies (Powers et al., 2004; Sefton et al.,
2011) report that statistically significant results in
improving postural sway on single leg standing,
Table 2: Results obtained from comparison of the O1´s
comparison with O2 time of stabilization, in the different
tasks analyzed, in the three groups.
TASKS EG CG 1 CG 2
SLSS_YO
L + A T2_T3
(p=0,037;
p=027)
---- ----
SLSS_YC
L T1_T3
(p=0,025)
---- ----
AJ
A T1_T2
(p=0,037)
A T1_T3
(p=0,037)
----
L T1_T2
(p=0,008)
LJ
A T2_T3
(p=0,006)
A T1_T2
(p=0,055)
----
MJ
A T2_T3
(p=0,027)
A T1_T3
(p=0,020)
A T1_T2
(p=0,055)
----
SLSS_YO – single limb static stance with eyes open; SLSS_YC –
single limb static stance with eyes closed; AJ – anterior jump; LJ
– lateral jump; MJ – medial jump; EG – experimental group; CG1
– control group 1; CG2 – control group 2; A - the area of the
CoP´s displacement; L – the length of the CoP´s displacement; T1
– 0 to 2 sec; T2 – from 2 to 4 sec; T3 – from 4 to 6 sec; T1_T2
difference of CoP´s values obtained in the interval T1 in
comparison to T2; T2_T3 difference of COP´s values obtained in
the interval T2 in comparison to T13; T1_T2 difference of CoP´s
values obtained in the interval T1 in comparison to T3.
through the assessment of static balance, following
the application of an exercise program were not
found. However, changes were found through
dynamic assessment (Sefton et al., 2011). Based on
these data and considering the fact that at the gym,
most ankle injuries occur on landings, it seemed
useful to assess the postural sway and stabilization
time dynamically on landings.
Graphic 1: Values obtained through the FAOS to the EG
in O1 and O2.
A study by Fellander-Tsai and Wredmark (1995)
found that most injuries in competitive gymnasts
occurred on landings. The gymnast’s ability to land
a jump or technical element skill, often on different
surfaces, and prepare for immediate take-off for
another skill, requires a high motor and postural
control of the gymnast. In case of CAI, deficits in
the neuromuscular mechanisms, inherent to postural
EffectsofaNeuromuscularReeducationProgramonthePosturalControlinGymnastswithChronicAnkleInstability
59

control, can lead to an increased risk of recurrent
injury. The specificity of the sport, with the more
emphasis on feedforward mechanisms, rather than
feedback mechanisms in postural control
(Konradsen et al., 1997; Holmes and Delahunt,
2009), led to the creation of an exercise program
with special focus on skills development for motor
pre-programming where the landing of jumps was
given special emphasis. According Delahunt (2007),
training exercises performed on unstable surfaces for
the training correct technique of landing, especially
on single leg, will emphasize the synergistic muscle
activity pre-programmed by feedforward
mechanisms in subjects with FAI. Thus, the study
also included in the program exercises that promote
specific mechanisms of postural control feedback
like single leg balance, with the need of constant
posture adjustments and where the reflex activity
plays a key role. Mynark and Brown (2007)
demonstrated in their study that individuals with
CAI take longer to stabilize after a dynamic activity
than the control group of subjects with no previous
injuries. This increase in stabilizing time can lead to
an increased recurrence of ankle injuries due to the
inability to properly execute the landing after a jump
(Ross et al., 2005). It at least it suggests that the
posture control mechanisms are less efficient. Based
on these studies, our program also included
exercises that develop balance and motor control in
plyometric tasks (different types of jumps in
different conditions and landing directions). The
program had six weeks duration with a weekly
frequency of three times a week. The determination
of the time set for its use is in line with previous
studies. Hale et al., (2007) in their study
demonstrated positive results in improving posture
control with an exercise program for four weeks five
times per week. Bernier and Perrin (1998);
Rosenbaum and Elis (2001); Burden and Clark
(2005), Powers et al., (2004); Docherty et al.,
(1998); Sefton et al., (2011) found positive results
with an experimental six weeks protocol, three times
a week.
Within the group of gymnasts with CAI -
experimental group - there was a significant
improvement in all the tasks in study, which
reinforces the effectiveness of the exercise program
in improving postural control and joint stability.
These results are in line with other studies, where
the application of an exercise program with
proprioceptive exercises, particularly balance
training on unstable surfaces, showed positive
results in the reprogramming of postural control
mechanisms in subjects with CAI (Mattacola and
Dwyer, 2002; Baltaci and Kohl, 2003; Wilkerson
and Nitz, 1994). Bernier and Perin (1998) had
statistically significant results with CoP´s
displacement on single leg balance with eyes closed,
in the CAI group, after application of an exercise
program for six weeks.
Gymnastics skills with postures in single leg
support are frequent (eg. static balance skills like
scales, stability posture after a jump for a relatively
long period). The results achieved in improving
single leg postural sway demonstrate the positive
effect of training, with the exercise program
performed. This aspect determines improved
stability, and thereby improving the performance of
the gymnasts.
For more dynamic activities, there were
improvements in postural sway and stabilization
time on landing, to the front and to the medial and
lateral sides, in subjects with CAI. These data reveal
an improvement of dynamic joint stability, both
anteroposterior and mediolateral stability after
completion of the exercise program. According
Sefton et al. (2009), a decrease in CoP´s length and
area displacement and a reduction of its velocity
indicate an improvement in postural control. In their
study, these authors reported an improvement in the
dynamic balance in the anteroposterior, medial and
posteromedial directions, after the application of a
proprioceptive exercise training program for six
weeks in subjects with CAI.
In the control group of healthy subjects, who also
performed the exercise program (GC1), there were
statistically significant improvements in single leg
balance with eyes open, and on the landing of an
medial lateral jump. These results demonstrate a
positive effect of the exercise plan, improving the
dynamic stability in healthy subjects. The
improvement in postural sway and stabilization time
in healthy subjects reported in this study, suggests a
possible implementation of this type of training for
injury prevention of the ankle and performance
improvement in gymnasts.
In a study of this nature, the kinematics and
EMG analysis could give more information. This
could be considered one of the limitations to this
study. Another methodological limitation of this
study relates to the size of the sample. However, the
value of the sample under study (n = 24), while
somewhat lower than in other studies appear to be
similar to the average sample used in some similar
studies carried out previously.
However, we consider our options are in line
with the goal set for the scope of this research. The
options seem appropriate, taking into account the
icSPORTS2013-InternationalCongressonSportsScienceResearchandTechnologySupport
60

specific context of the sample under study and
specificity of the sport.
Despite these limitations, the objectives set for
this study were achieved: to assess the effects of a
neuromuscular program in competitive gymnasts
with CAI, thus making a contribution to practice
evidence-based physiotherapy.
8 CONCLUSIONS
The application of a six weeks neuromuscular
program seems to have positive effects in improving
postural control in gymnasts with and without CAI.
Results suggest an improvement of postural control
on the sample subjects, stressing the relevance of the
use of rehabilitation programs to improve dynamic
and functional stability, in order to reduce the risk of
recurrence of injury and further improvement of
athletic performance.
Although many studies have been developed in
this area, we emphasize the importance of assessing
dynamic postural control, where the feedforward
mechanisms are especially important, as well as the
intervention with exercise programs that improve the
development of these neuromotor mechanisms.
REFERENCES
Baltaci, G. & Kohl, H. W. (2003). Does proprioceptive
training during knee and ankle rehabilitation improve
outcome? Physical Therapy Reviews, 8, 5–16.
Bernier, J. N. & Perrin, D. H. (1998) Effect of
coordination training on proprioception of the
functionally unstable ankle. The Journal of Orthopedic
and Sports Physical Therapy, 27 (4), 264-75.
Brown, N. & Mynark, R. (2007) Balance deficits in
recreational athletes with chronic ankle instability.
Journal of Athletic Training, Jul-Sep: 42(3), 367-73.
Brown et al. (2004) Assessing functional ankle instability
with joint position sense, time to stabilization and
electromyography. Journal of Sport Rehabilitation.
13(2), 122-134.
Caulfield, B., Delahunt, E. & Kenneth, M. (2006) Altered
neuromuscular control and ankle joint kinematics
during walking in subjects with functional instability
of the ankle joint. American Journal of Sports
Medicine, 34 (12), 1970-77.
Caulfield, B. & Garrett, M. (2004) Changes in ground
reaction force during jump landing in subjects with
functional instability of the ankle joint. Clinical
Biomechanics, 19, 617-621.
Caulfield, B. M. & Garrett, M. (2002) Functional
instability of the ankle: differences in patterns of ankle
and knee movement prior to and post landing in a
single leg jump. International Journal of Sports
Medicine, 23, 64-68.
Clark V. M., Burden A. M. (2005) A 4-week wobble
board exercise program improved muscle onset
latency and perceived stability in individuals with a
functionally instable ankle. Phys Therapy Sport, 6,
181-7.
Delahunt, E. et al. (2010) Inclusion Criteria when
Investigating Insufficiencies in Chronic Ankle
Instability. Medicine & Science in Sports & Exercise,
Nov: 42(11), 2106-2121.
Delahunt, E. (2007a) Neuromuscular contributions to
functional instability of the ankle. Journal of
Bodywork and Movement Therapies, 11, 203-213.
Denegar, C. R. & Miller, S. J. (2002) Can chronic ankle
instability be prevented? Rethinking management of
lateral ankle sprains. Journal of Athletic Training, 37,
430-5.
Docherty, C. L., Moore, J. H. & Arnold, B. L. (1998)
Effects of strength training on strength development
and joint position sense in functionally unstable
ankles. Journal of Athletic Training, 33, 310-14.
Eils, E. & Rosenbaum, D. (2001) A multi-station
proprioceptive exercise program in patients with ankle
instability. Medicine & Science Sports & Exercise, 33
(12), 1991-8.
Fellander-Tsai, L. & Wredmark, T. (1995) Injury
incidence and cause in elite gymnasts. Arch Orthop
Trauma Surg. 114 (6), 344-346.
Hale, S. A., Hertel, J. & Olmsted-Kramer, L. C. (2007)
The effect of a 4-week comprehensive rehabilitation
program on postural control and lower extremity
function in individuals with chronic ankle instability.
Journal Orthopedic & Sports Physical Therapy, 37
(6), 303-11.
Holmes, A. & Delahunt, A. (2009) Treatment of common
deficits associated with chronic ankle instability.
Sports Medicine, 39 (3), 207-224.
Hubbard, T. J., Hertel, J. & Sherbondy, P. (2006) Fibular
position in individuals with self-reported chronic ankle
instability. Journal Orthopedic & Sports Physical
Therapy, 36, 3-9.
Kavanagh, J. (1999) Is there a positional fault at the
inferior tibiofibular joint in patients with acute or
chronic ankle sprains compared to normal? Manual
Therapy, 4, 19-24.
Kolt, G., Kikby, R. (1999). Injury in Australian female
competitive gymnasts: a psychological perspective.
Australian Physiotherapy, 42 (2), 121-126.
Konradsen, L., Voight, M. & Hojsgaard, C. (1997) Ankle
inversion injuries. The role of the dynamic
defense.mechanism. American Journal of Sports
Medicine, 25, 54-58.
Mattacola, C.G. & Dwyer, M.K. (2002). Rehabilitation of
the ankle after acute sprain or chronic instability.
Journal of Athletic Training. 37(4):413–429.
McKay, G. D., Goldie P. A., Payne W. R. & Oaks B. W.
(2001) Ankle injuries in basketball: injury rate and
risk factors. British Journal of Sports Medicine, 35,
103-108.
EffectsofaNeuromuscularReeducationProgramonthePosturalControlinGymnastswithChronicAnkleInstability
61

Powers, M. et al (2004) Six weeks of strength and
proprioception training does not affect muscle fatigue
and static balance in functional ankle instability.
Journal of Sport Rehabilitation, 1(3), 201-227.
Ross, S. E. & Guskiewicz, K. M. (2006) Effect of
coordination training with and without stochastic
resonance stimulation on dynamic postural stability of
subjects with functional ankle instability and subjects
with stable ankles. Clinical Journal of Sports
Medicine 16, 323–328.
Ross, S. E., Guskiewicz, K. M. & Yu B. (2005) Single leg
jump-landing stabilization times in subjects with
functionally unstable ankles. Journal of Athletic
Training, 40, 298-304.
Sefton, J. M. et al (2011) Six weeks of balance training
improves sensorimotor function in individuals with
chronic ankle instability. Journal of Orthopedic &
Sports Physical Therapy, 41 (2), 81-89.
Sefton, J. M., et al. (2009). Sensorimotor function as a
predictor of chronic ankle instability. Clinical
Biomechanics. 24, 451–458.
Wilkerson, G. B. & Nitz, A. J. (1994) Dynamic ankle
stability: mechanical and neuromuscular
interrelationships. Journal of Sports Rehabilitation, 3,
43-57.
Wikstrom, L. A. et al. (2005) Detection of dynamic
stability deficits in participants with functional ankle
instability. Medicine & Science Sports & Exercise.
37(2), 169-175.
Willems, T., Witvrouw, E. & Verstuyft, J., et al (2002)
Proprioception and muscle strength in subjects with a
history of ankle sprains and chronic instability.
Journal of Athletic Training, 37, 487-93.
Yeung, M., Chan, K., So, C. & Yuan, W. (1994) An
epidemiological survey on ankle sprain. British
Journal of Sports Medicine, 28, 112-116.
icSPORTS2013-InternationalCongressonSportsScienceResearchandTechnologySupport
62
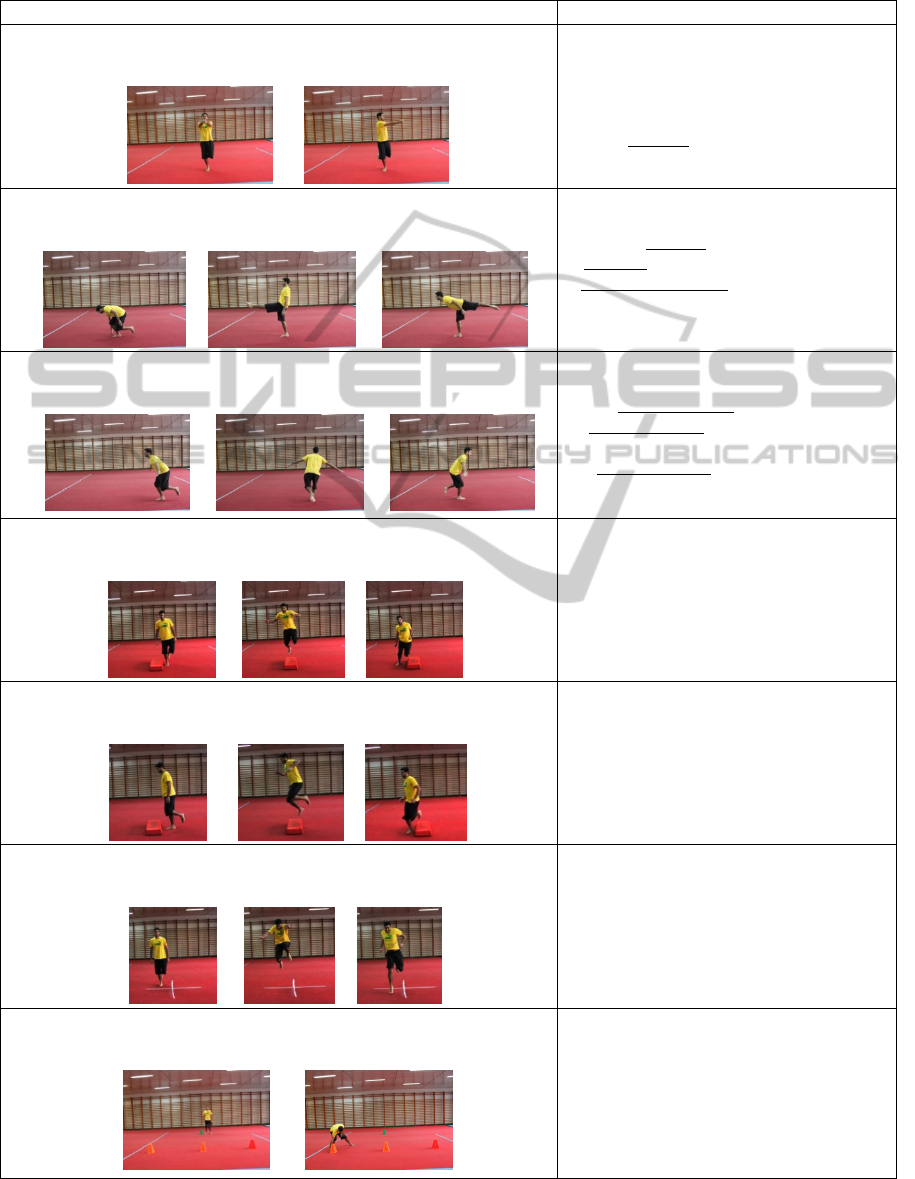
APPENDIX
Multi-Station Exercise Program Sets x Repetitions / Time between Sets
Exercise 1 – Rotation of the body in a single limb stance
1. 2.
1x 1 min – on the floor
1x1min – on the mat (medium density)
1x1min – on the Trampoline
Time between Sets - from 20 to 60s
6
th
week – with eyes closed
Exercise 2 – Sequence in a single limb stance
1. 2. 3.
2x 4 sequences
1
st
week – on the floor
2
nd
week - on the mat (medium density)
From 3
rd
to 6
th
week – on the trampoline
Time between Sets - from 20 to 60s
Exercise 3 - ¼ jump, stabilizing the landing
1. 2. 3.
2 x 12 jumps
1
st
and 2
nd
week – on the floor
3
rd
and 4
th
week - on the mat (medium
density)
5
th
and 6
th
week - on the trampoline
Time between Sets - from 20 to 60s
Exercise 4 – Lateral jumps
1. 2. 3.
2x 10 jumps
Time between Sets - from 30 to 60s
Exercise 5 – Antero-posterior jumps
1. 2. 3.
2x 10 jumps
Time between Sets - from 30 to 60s
Exercise 6 - Plyometric trainning with multidireccional jumps
1. 2. 3.
1x 2 sequences around
1x 2 sequences in 8
Time between Sets - from 30 to 60s
Exercise 7 – Running with direction changing
1. 2.
1x 1 min
EffectsofaNeuromuscularReeducationProgramonthePosturalControlinGymnastswithChronicAnkleInstability
63
