
ONE WAY TO PATIENT EMPOWERMENT
The Proposal of an Authorization Model
Cátia Santos-Pereira
1,3
, Luis Antunes
4,5
, Ricardo Cruz-Correia
1,3
and Ana Ferreira
1,2,3
1
Center for Research in Health Technologies and Information Systems – CINTESIS, Porto, Portugal
2
Center for Informatics – CI, Porto, Portugal
3
Faculty of Medicine, University of Porto, Porto, Portugal
4
Institute of Telecommunications, University of Porto, Porto, Portugal
5
Faculty of Science, University of Porto, Porto, Portugal
Keywords: Patient Empowerment, Computer Security, Confidentiality, Electronic Health Records, Role Based Access
Control.
Abstract: American and European Legislation for protection of medical data agree that the patient has the right to play
a pivotal role in the decisions regarding the content and distribution of her/his medical records. The Role
Based Access Control (RBAC) model is the most commonly used authorization model in healthcare. The
first goal of this work is to review if existing models and standards provide for patients accessing their
medical records and customizing access control rules, the second goal is to define and propose an
authorization model based on RBAC to be used and customized by the patient. A literature review was
performed and encompassed 22 articles and standards from which 12 were included for analysis. Results
show that existing standards define guidelines for these issues but they are too generic to be directly applied
to real healthcare settings. The proposed authorization model combines characteristics of RBAC, ISO/TS
13606-4, temporal constraints and break the glass. With this model we hope to start bridging the gap
between legislation and what really happens in practice in terms of patients controlling and being actively
involved in their healthcare. Future work includes the implementation and evaluation of the proposed model
in a healthcare setting.
1 INTRODUCTION
A variety of new applications such as online social
networks and online healthcare databases are very
common nowadays and very often require the need
for consumers to use and define access control.
Within these applications personal and highly
sensitive data can be stored. There are great benefits
to be gained by making an individual’s medical
history available to healthcare providers and great
risks to making it available to stalkers (Reeder,
2011).
Both American Legislation (Health Insurance
Portability Accountability Act - HIPAA) and the
European legislation (Recommendation No R (97)
5) for protection of medical data, agree that the
subject of care (normally the patient) has the right to
play a pivotal role in the decisions regarding the
content and distribution of her/his medical records,
as well as the right to be informed of its contents
(U.S. Department of Health & Human Services,
1996), (Council of Europe, 1997), (Pereira et al.,
2011).
Some studies regarding the access of Electronic
Health Records (EHR) by the patient suggest modest
improvements in doctor-patient communication
adherence, patient empowerment and patient
education. This process makes patients more careful
in following medical recommendations. Although
patients may find some parts of their EHR difficult
to understand, patients who are offered a chance to
review their EHR are mostly satisfied with the
experience (Ross and Lin, 2003), (Honeyman et al.,
2005), (Ferreira et al., 2007a). On the other hand
healthcare providers also recognized the benefit of
patient’s ability to review and comment on their
medical information prior to a visit (Siteman et al.,
2006).
An authenticated user is authorized, within the
system, to perform only certain actions that are
associated to his or her functions e.g. to search
through certain medical records of only patients
249
Santos-Pereira C., Antunes L., Cruz-Correia R. and Ferreira A..
ONE WAY TO PATIENT EMPOWERMENT - The Proposal of an Authorization Model.
DOI: 10.5220/0003787902490255
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2012), pages 249-255
ISBN: 978-989-8425-88-1
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)

under his or her care (Shortliffe and Cimino, 2006).
The Role Based Access Control (RBAC) (Sandhu et
al., 2000) model is the most commonly used access
control model in healthcare (Beimel and Peleg,
2009), (Ferreira et al., 2007b) and has emerged as a
promising alternative to traditional Discretionary
Access Control (DAC) and Mandatory Access
Control (MAC) models (Giuri, 1996), (Joshi et al.,
2001), (Osborn et al., 2000). In large enterprise
systems, the number of roles can be in the hundreds
or thousands, and users can be in the tens or
hundreds of thousands. Managing these roles, users,
and their interrelationships is a formidable task that
is often highly centralized in a small team of security
administrators (Sejong and Ravi, 2002).
So, the first goal of this paper is to review if
existing models and standards provide for patients’
accessing their EHR and defining what healthcare
professionals can access within their EHR. The
second goal is to propose a patient authorization
model based on RBAC to be used and customized
by the patient.
2 PATIENT’S CUSTOMIZABLE
ACCESS CONTROL MODELS:
A SYSTEMATIC REVIEW
2.1 Methods
A literature review was performed in June 28, 2011
with searches in Pubmed, IEEE Xplore, ISI Web of
Knowledge and International Organization for
Standardization (ISO). The queries applied
were:“RBAC [All Fields] AND ("Health"[MeSH
Terms] OR "Health"[All Fields]) AND Model [All
Fields]” in Pubmed; “RBAC Health
Model<in>metadata” in IEEE Xplore; “Topic
(RBAC Health Model)” in ISI Web of Knowledge
and “Health Access Control Model” in ISO web
site.
The results from these queries were filtered
according to the following inclusion criteria:
language of the article (English) and review of title
and abstracts (adequate context).
The review was done in several stages. Initially,
the repeated articles in the various databases were
identified, they were then reviewed according to the
inclusion criteria and finally read and analysed. For
each article/standard, three relevant characteristics
were analysed: (a) if they referred to EHR; (b) if
they included within their access control policies the
possibility for patients to also access their EHR and
(c) if there was the capability for the patient
himself/herself to customize that model and define
his/her own access control rules, regarding their
EHR. Cited articles/standards were also included. A
total of 22 articles and standards were obtained from
the search queries. After applied the inclusion
criteria a total of 12 articles/standards were included
in the final review.
2.2 Results
From the 12 articles and standards that were selected
after the review, 10 presented RBAC extension
models while 2 described access control standards
and guidelines in healthcare.
The selected RBAC extensions were Motta and
Furuie model (Motta and Furuie, 2003) and Patrick
et al. model (Patrick, 2007 ) and the ISO standards
selected were ISO/TS 22600-2 (ISO/TS 22600-2,
2006) and ISO/TS 13606-4 (ISO/TS 13606-4, 2009).
The models by Motta and Furuie and by Patrick et
al. together with the standards ISO/TS 22600-2 and
ISO/TS 13606-4 include the patient in the set of
roles that can access the EHR. However only the
ISO/TS 13606-4 standard and the model by Motta
and Furuie introduce also, in a generic way, the
capability of the patients to customize access control
rules to their EHR. We consider the ISO/TS 13606-4
the most complete work in terms of our research.
Beyond these models, the Generalized Temporal
Role Based Access Control (GTRBAC) (Joshi et al.,
2002) and the Break The Glass Role Based Access
Control (BTG-RBAC) (Ferreira et al., 2009)
although not complying with the goals of the
systematic review, provide security mechanisms that
could integrate the new extension of the RBAC
model.
3 PROPOSAL OF A PATIENT’S
AUTHORIZATION MODEL
After performing the systematic review several
characteristics from various access control models
and standards were studied in order to define the
proposed patient authorization model. So, RBAC
security features (Core RBAC, Hierarchical RBAC,
Separation of Duties and Administration RBAC),
temporal constraints described in GTRBAC and
information sensivity definitions found in ISO
13606-4 will be included in the proposed model
because they provide confidentiality and privacy to
patient information and, on the other hand, break the
glass mechanisms, described in BTG-RBAC,
HEALTHINF 2012 - International Conference on Health Informatics
250

provide for availability of information in emergency
situations.
3.1 Model definition
3.1.1 The ISO/TS 13606-4
The ISO 13606-4 expresses the record components
that an EHR may integrate such as: Personal Care;
Privileged Care; Clinical Care; Clinical Management
and Care Management. It also describes which
functional roles (Subject of Care; Subject of Care
Agent; Personal Healthcare Professional; Privilege
Healthcare Professional; Healthcare Professional;
Health-related Professional; Administrator) can
access those record components.
3.1.2 NIST RBAC
The Role Based Access Control model integrates the
Core RBAC, the Hierarchical RBAC, and
Constrained RBAC, which includes Separation of
Duties (SoD).
In the proposed model, the functional roles were
organized into 3 main groups: subject of care (Group
I), healthcare professionals (Group II) and
administrative access (Group III), which include role
inheritance (see Figure 1). Static Separation of
Duties will integrate the proposed patient
authorization model because the user will only be
able to use one exclusive role per session in order to
avoid conflicts between functional roles. The
administrator of the roles and permissions of an
EHR is associated with the patient of that EHR
(Sejong and Ravi, 2002). The patient will actively
manage the roles and permissions as well as give
permissions of administration to other roles, if
necessary.
Figure 1: Hierarchical functional roles divided into three
groups.
3.1.3 Break the Glass Access
Break the Glass (BTG) allows a user to override the
access control rules stated by the access control
manager and access what the user requests, even
though he was not previously authorized to do it.
When this is done, other BTG rules come into play
which may monitor, record or report the user´s
actions, thus making him responsible and oblige him
to justify what he did.
3.1.4 Temporal Constraints
The Generalized Temporal Role Based Access
Control (GTRBAC) model introduces a set of
language constructs for the specification of temporal
constraints on roles, including constraints
permissions. These constraints are also included
within the proposed patient authorization model in
order to restrict access to Groups II and III in terms
of temporal duration, for instance, during the
healthcare professionals’ shift.
3.2 Patient’s Healthcare Network and
Model Architecture
The concept of Patient’s Healthcare Network (PHN)
refers to all the healthcare institutions that the
patient usually attends as well as health centers,
referral hospitals, private hospitals, commercial
laboratories and health insurers. It is important to
define the institutions where the patient attends
consultations and treatments because only the
professionals that work in these institutions should
usually have access to that patient's EHR. All
professionals outside of the PHN are normally
excluded from access to the EHR of the patient.
However, the patient can define, within his/her
model, a temporary role for healthcare professionals
outside that PHN to access their EHR in a
predefined period of time, preferably in their
presence.
In some situations, when the patient integrates an
institution inside the PHN the providers of that
institution may wish to share information with other
providers (e.g. to get a second opinion) who do not
belong to the patient’s PHN. In this situation, if the
role provider has delegation permissions he could
attribute temporary access to a user outside the PHN
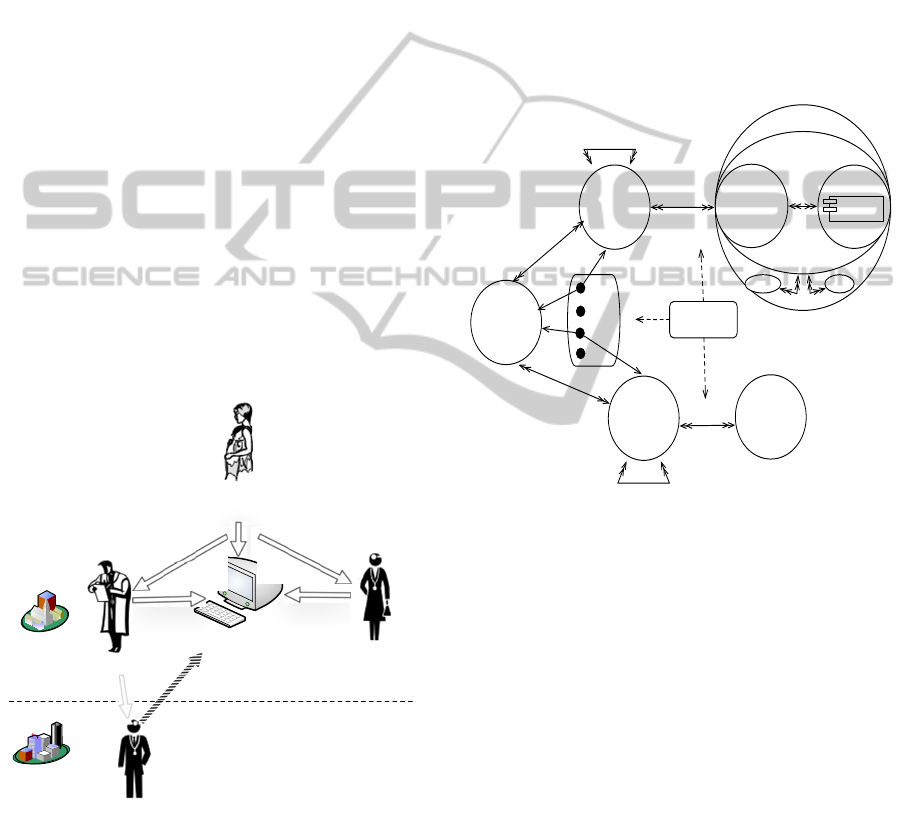
to obtain a second opinion. Figure 2 illustrates this
case with an example. Jennifer is a patient that is
being followed in Institution A (belongs to PHN),
Jennifer has the role subject of care and manager
senior in their own EHR. Dr. Jain is Jennifer’s
Gynecologist and has permissions to access
Jennifer’s EHR with the role Gynecologist. Dr.
Chen is Jennifer’s Neurologist and has the role
Personal healthcare
professional (PHP)
Privileged healthcare
professional (PrHP)
Healthcare professional
(HP)
Health-related
professional (HRP)
Subject of care (SC)
Subject of care agent
direct (SCA1)
Subject of care agent
indirect (SCA2)
GROUP I
GROUP II
Administrative
senior (AS)
Administrative
junior (AJ)
GROUP III
ONE WAY TO PATIENT EMPOWERMENT - The Proposal of an Authorization Model
251
Neurologist. Besides having the permissions
associated with the role Neurologist, Dr. Chen has
user delegation permissions as well. He needs a
second opinion for Jennifer’s treatment, about a drug
prescription. Dr. Chen contacts Dr. White for a
second opinion but the later does not belong to
Jennifer’s PHN. Dr. Chen temporarily delegates
permissions to access that patient’s EHR to Dr.
White. However the permissions delegated to Dr.
White, have the particular characteristic that is to
allow Dr. White access to that patient’s anonimyzed
medical information.
In this proposed model, for users to access the
EHR and its components they need only to provide
three pieces of information: a login (for
identification); a password (for authentication); and
a role (for authorisation). The first two are presented
initially and only if authentication is successful will,
a list of roles, that are associated to that user be
available. The user can only select one role for each
session. Each role has different permissions
associated to different parts of EHR components,
according to what the patient has previously defined
within the model. Moreover, the model predicts also
the utilization of a stronger authentication factor,
with the use of smart-cards or tokens whenever
needed.
Figure 2: Example of a user delegation outside of the PHN
performed by Dr. Chen to Dr. White.
The access permissions of a role to a specific
record component is going to depend on the
mapping that was previously made by the
administrator senior (usually the patient). A specific
role will have access to a record component if the
administrator would have defined any of the Create,
Read, Update and Delete (CRUD) operations or
BTG to be part of his/her access permissions.
Figure 3 presents the architecture of the
proposed authorisation model as the new relations of
the proposed model from the RBAC model (Sandhu
et al., 2000), that include (Ravi et al., 1999),
(Ferreira et al., 2009) and (Joshi et al., 2002). The
proposed model integrates both the specification of
access and the definition by the patient of
permissions to access his/her EHR. It puts the
patient in the centre of these operations. Patient as
an administrator senior can customize/manage the
permissions of all the other roles.
Figure 3: Architecture of the proposed patient
authorization model based on (Ravi et al., 1999), (Sandhu
et al., 2000), (Joshi et al., 2002), (Ferreira et al., 2009) and
(ISO/TS 13606-4, 2009).
3.3 Proof of Concept
Two storyboards will be described next to better
understand how the proposed model can work in real
practice. Storyboard 1: “The patient corrects data in
this EHR” and storyboard 2: “The patient has the
need for medical care while travelling”.
Storyboard 1: John is 59 years old and resides in
Porto, Portugal. He has recently moved to another house
and needs do update his data on the EHR. He decides to
access it by inserting his authentication credentials (login
and password). He then chooses to update the
demographic data record components.
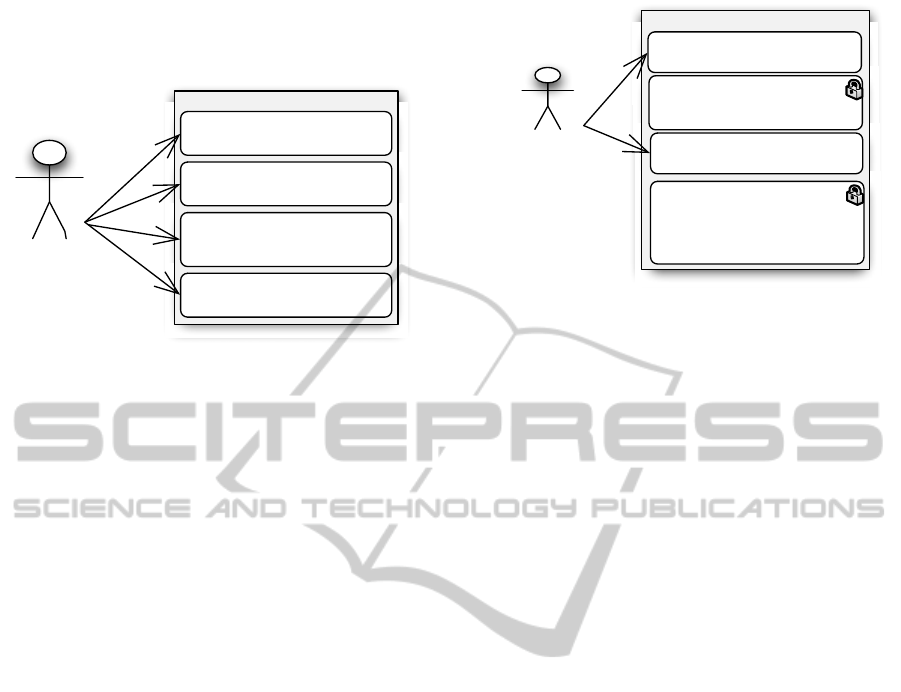
Figure 4 illustrates a use case that represents
storyboard 1. When user John accesses his EHR, as
Jennifer
Roles: Subj ect of car e and
Administrator senior
Jennifer's EHR
Dr. Chen
Role: Neurologist
Dr. Jain
Role: Gynecologist
Institution A
inside of the PHN
Dr. White
Role: Second opinion healthcare
profe
s
s
ional
Institution B
outside of the PH N
Defines roles
Defines roles
Access
A ccess
Delegation
Access
Temporary access
PA _BT G
APA
UA
USER ASSIGNM ENT
Temporal
Constraints
OBLGS
OPS
(OBTG OPS)
Create
Read
Update
Delete
OBS
BTGS
OPRMS_BTG
F_ROLES
FUNCTIONAL
ROLES
U
USERS
A_PERMS
ADMIN.
PE RM I SSI O NS
AUA
ADMINISTRATIVE
USER ASSIGNM ENT
S
SE SSI O NS
A_ROLES
ADMIN. ROLES
us e r
role
role
ADMIN. PERMISSION
ASSI G NM E NT
PE RM I SSI O N
ASSI G NM E NT
Record
Components
ARH
A
DMINISTR
A
T
O
RR
O
LE HIER
A
RCHY
RH
ROLE HIERARCHY
HEALTHINF 2012 - International Conference on Health Informatics
252
the functional role subject of care, he has
permissions to perform all the operations (CRUD) in
all the EHR record components.
Figure 4: Use case 1 for storyboard 1.
Storyboard 2: John is 59 years old and he resides in
Porto, Portugal. During his holidays in the Algarve John
feels sick with fever and cough. He goes to the hospital in
Faro and the doctor that treats him has no access to
John’s EHR because he is not within his PHN. The patient
has previously defined the role temporary privileged
healthcare professional and accesses his EHR with this
role. Since John will be the one to introduce the
authentication credentials, he decides to use a two- factor
authentication with a smartcard, to guarantee that his
credentials are not breached. After a successful
authentication John proceeds normally to choose the role
available from a list of roles, in this case the role
temporary privilege healthcare professional (TPrHP).
Now the provider attending the patient has permissions to
access the information that the patient defined for that
role, for a specific period of time and therefore assists in
his treatment
.
Figure 5 illustrates the use-case relating to
storyboard. Since the provider did not have access to
the patient’s EHR, the patient can access the system
by previously defining the role he wants to use for
that session. In this use-case, the patient chose the
role temporary privileged healthcare professional
and gave temporary access to the provider that was
treating him at that time. The provider can only
access (read- only) components Diabetes Mellitus II
and Penicilin Allergy of that EHR. The role TPrHP
has not defined the permissions to perform BTG in
any other component of the record so the healthcare
professional does not even know of any other
components’ existence. As the proposed
authorization model allows to define temporal
constraints, since this is a temporary role, John
associated a limited timeframe to be used (only
1hour).
Figure 5: Use case 2 for storyboard 2.
4 DISCUSSION
In spite of generically allowing the patients to access
or customize the access control rules of their
medical records, the models and standards that were
found in the review are too generic to be applied
directly to specific healthcare scenarios. The
analysed models and standards do not describe how
the patient can customize his/her EHR in more
specific scenarios. There is, therefore, a lack of
research within this area, so we propose an access
control model that can give the patients the needed
empowerment.
Regarding the proposed model the first
storyboard and use case presents a very common
scenario where the patient wants to access his EHR
in order to perform some operations within its record
components. This scenario shows how easy it can be
for the patient to access his EHR and perform all the
necessary operations to keep it up to date. In this
scenario one of the available record components is
“subject of care area”, so the patient has the
possibility to insert and manage his personal notes.
However this specific area will depend on the
structure of the EHR, so, if the EHR does not
include this feature could be integrated into other
Personal Health Records platforms such as
Microsoft Health Vault (Microsoft, 2011) and
myPHN (American Health Information Management
Association Foundation, 2011).
In the second use-case scenario with the use of
the role temporary privileged healthcare
professional, the provider does not belong to the
PHN so he would have to blindly treat the patient as
a newcomer, without any previous information. The
proposed patient authorization model allows the
healthcare professional to have a minimum
information content that can help in a faster and
User: John Adams
Functional role:
Subject of Care
Role: Patient
Example of John's EHR
Diabetes Mellitus II (DM II)
Type of record: diagnosis information
Sensitivity: privileged clinical
Color blindness (CB)
Type of record: genetic information
Sensitivity: privileged clinical
CRUD
Demographic data (DD)
Type of record: general data
information
Sensitivity: normal clinical
CRUD
Subject of care area (SCa)
Type of record: subject of care notes
Sensitivity: privileged information
CRUD
CRUD
CRUD
User: John Adams
Functional role: Privileged
healthcare professional
Role: Temporary Privileged
healthcare professional
Example of John's EHR
Diabetes M ellitus I I (DM I I )
Type of record: diagnosis information
Sensitivity: normal clinical
Color blindness (CB)
Type of record: genetic information
Sensitivity: privileged clinical
BTG option: no
Penicilin allergy (PenA)
Type of record: allergies information
Sensitivity: normal clinical
Age related macula degener ation
(AMD)
Type of record: ophthalmological
information
Sensitivity: privileged clinical
BTG option: no
R
R
Available during
1h
ONE WAY TO PATIENT EMPOWERMENT - The Proposal of an Authorization Model
253

more successful patient treatment.
The proposed patient authorization model allows
for a greater participation, responsibility and control
over information security and contents of patient’s
EHR. This model is innovative as it allows the
patient to define access control permissions within
his PHN but also outside this network when
necessary, providing a better healthcare treatment at
the point of care. The functional roles subject of care
agent direct and indirect can also be beneficial
because they can allow patients’ relatives to also
take part and help in their treatment. Furthermore,
these can help treating patients’ relatives when, for
example, they can have access to relevant genetic
information about their parents or other relatives.
Even if this information is not directly accessible,
those functional roles could have the BTG
permission to access it and the owner of the EHR
would always be notified of the actions performed
within his/her EHR. The flexibility of access and
definition of access by the patient is not meant to
invade or compromise healthcare professionals’
workflows or privacy as there will be a restricted
area (EHR component) only to be used and accessed
by that healthcare professional. The temporal
constraint with the separation of duties integrated
within the authorization model allows to define the
level of patients’ privacy as fine-grained as the
patient desires. To access a patient’s EHR the user
should belong to the patient’s PHN, however a user
can also access the patient’s EHR if there are any
delegated permissions (user delegation) defined for
him or in emergency situations activating the
mechanism BTG.
However, in order to use this model, the patient has
to understand and use information technologies (IT)
and have basic IT skills to define and use a platform
that will integrate this new model. Problems with
this model include the fact that users may mistrust
what they are accessing as well as not being able to
access all they think should be available to them.
Also, the patient may not be capable of defining
proper access control rules and unwantedly hide
healthcare information that can be crucial to perform
effective treatments. However, this can also happen
no matter what type of record or access is made to
the EHR. The patient can always omit relevant
information for his/her treatment.
5 CONCLUSIONS
This paper constitutes the starting point to define a
RBAC based patient authorization model that can be
used in real practice. With this model we hope to
bridge the gap that exists between legislation (with
medical data protection definition) and what really
happens in practice. With the growth of new
technologies and the interest that patients have to be
in control and take an active part in their treatment,
the authors feel that the patients need to have a
simple but focused model that allows them to easily
define access permissions but also closely
collaborate and interact with their healthcare
professionals.
Future work includes the implementation and
evaluation of the proposed authorization model with
a specific case study in real healthcare practice.
ACKNOWLEDGEMENTS
This work is funded by FEDER funds (Programa
Operacional Factores de Competitividade –
COMPETE) and by National funds (FCT –
Fundação para a Ciência e a Tecnologia) through
project OFELIA – Open Federated Environments
Leveraging Identity and Authorization [PTDC/EIA-
EIA/104328/2008].
REFERENCES
American Health Information Management Association
Foundation. 2011. myPHR [Online]. American Health
Information Management Association. Available:
http://www.myphr.com/ [Accessed October 2011].
Beimel, D. Peleg, M. 2009. The Context and the SitBAC
Models for Privacy Preservation – An Experimental
Comparison of Model Comprehension and Synthesis.
IEEE Transactions on Knowledge and Data
Engineering
Council of Europe 1997. Protection of Medical Data -
Recommendation nºR (97) 5. In: committee of
ministers to member states (ed.). Europe.
Ferreira, A., Chadwick, D., Zao, G., Farinha, P., Correia,
R., Chilro, R. ,Antunes, L. 2009. How securely break
into RBAC: the BTG-RBAC model. Proceedings from
25th Annual Computer Security Applications
Conference - ACSAC 2009.
Ferreira, A., Correia, A., Silva, A., Corte, A., Pinto, A.,
Saavedra, A., Pereira, A. L., Pereira, A. F., Cruz-
Correia, R., Antunes, L. F. 2007a. Why Facilitate
Patient Access to Medical Records. Medical and Care
Compunetics 4, 127, 77-90.
Ferreira, A., Cruz-Correia, R., Antunes, L. ,Chadwick, D.
2007b. Access Control: how can it improve patients'
healthcare? . Stud Health Technol Inform, 127, 65-76.
Giuri, L. 1996. Role-based access control: a natural
approach. Proceedings of the first ACM Workshop on
HEALTHINF 2012 - International Conference on Health Informatics
254

Role-based access control. Gaithersburg, Maryland,
United States: ACM.
Honeyman, A., Cox, B. ,Fisher, B. 2005. Potential impacts
of patient access to their electronic care records.
Informatics in primary care, 13, 55-60.
ISO/TS 13606-4 2009. Health informatics - Electronic
health record communication In: ISO/TS (ed.) Part 4:
Security. Switzerland: ISO/TC.
ISO/TS 22600-2 2006. Health Informatics - Privilege
management and access control In: ISO/TS (ed.) Part
2: Formal Models. Switzerland.
Joshi, J., Aref, W. G., Ghafoor, A., Spafford, E. H. 2001.
Security models for web-based applications. Commun.
ACM, 44, 38-44.
Joshi, J., Bertino, E., Ghafoor, A. 2002. Temporal
hierarchies and inheritance semantics for GTRBAC.
Proceedings of the seventh ACM symposium on Access
control models and technologies. Monterey,
California, USA: ACM.
Microsoft. 2011. Microsoft Health Vault [Online].
Available: http://www.microsoft.com/en-us/health
vault/ [Accessed October 2011].
Motta, G. H. M. B., Furuie, S. S. 2003. A contextual role-
based access control authorization model for electronic
patient record. Ieee Transactions on Information
Technology in Biomedicine, 7, 202-207.
Osborn, S., Sandhu, R., Munawer, Q. 2000. Configuring
role-based access control to enforce mandatory and
discretionary access control policies. ACM Trans. Inf.
Syst. Secur., 3, 85-106.
Patrick, C. K., Hung and Yi Zheng 2007 Privacy Access
Control Model for Aggregated e-Health Services.
Eleventh International IEEE EDOC Conference
Workshop (EDOCW'07).
Pereira, C., Oliveira, C., Vilaça, C., Ferreira, A. 2011.
Protection of clinical data - Comparison of European
with American Legislation and respective
technological applicability. HealthInf 2011 -
International Conference on Health Informatics.
Rome.
Ravi, S., Venkata, B., Qamar, M. 1999. The ARBAC97
model for role-based administration of roles. ACM
Trans. Inf. Syst. Secur. 1094-9224, 2, 105-135.
Reeder, R. W. 2011. Usable access control for all.
Proceedings of the 16th ACM symposium on Access
control models and technologies. Innsbruck, Austria:
ACM.
Ross, S. E., Lin, C. T. 2003. The effects of promoting
patient access to medical records: A review. Journal of
the American Medical Informatics Association, 10,
129-138.
Sandhu, R., Ferraiolo, D., Kuhn, R. 2000. The NIST
model for role-based access control: towards a unified
standard. Proceedings of the fifth ACM workshop on
Role-based access control. Berlin, Germany: ACM.
Sejong, O., Ravi, S. 2002. A model for role administration
using organization structure. Proceedings of the
seventh ACM symposium on Access control models
and technologies 1-58113-496-7. Monterey,
California, USA: ACM.
Shortliffe, E., Cimino, J. 2006. Biomedical Informatics -
Computer applications in Health Care and
Biomedicine, New York, Springer.
Siteman, E., Businger, A., Gandhi, T., Grant, R., Poon, E.,
Schnipper, J., Volk, L. A., Wald, J. S., Middleton, B.
2006. Clinicians recognize value of patient review of
their electronic health record data. AMIA ... Annual
Symposium proceedings / AMIA Symposium. AMIA
Symposium, 1101.
U.S. Department of Health & Human Services 1996.
Health Insurance Portability and Accountability Act
In: Services, U. S. D. O. H. H. (ed.).
ONE WAY TO PATIENT EMPOWERMENT - The Proposal of an Authorization Model
255
