
AUTHORIZATION IN CLOUD E-RADIOLOGY SERVICES
Vassiliki Koufi, Flora Malamateniou and George Vassilacopoulos
Department of Digital Systems, University of Piraeus, 80, Karaoli & Dimitriou Str., Piraeus, 18534, Greece
Keywords: Cloud Computing, Personal Health Record, eRadiology, Healthcare process, Authorization.
Abstract: The confidentiality of healthcare information is extremely important in any healthcare system. This paper is
concerned with the development of suitable authorization and access control framework for eRadiology
seen as a cloud computing service offered to healthcare professionals and patients alike. While eRadiology
is expected to improve many aspects of healthcare, these high expectations will be achieved only if provider
organizations pay continuing attention to the features that would most improve patients’ safety and health
and select systems that have such appropriate features, security being among the most prominent ones. In
particular, although the eRadiology workflow varies with the context, giving rise to specific ordering of task
executions, it is authorization that determines who can execute the various workflow tasks and what
information can be accessed during task executions. The main objective of this paper is to embed context-
aware access control into eRadiology workflows, operating in conjunction with a personal healthcare record
(PHR) system which has been implemented in a cloud computing infrastructure. The proposed model
enables authorization to be based not only on static rules and roles but also to be influenced by the workflow
execution context ensuring precise and tight access control. The resultant security system has been
incorporated into a prototype eRadiology workflow to enable authorized access to patient information when
and where needed.
1 INTRODUCTION
Healthcare providers are increasingly considering
migrating to cloud computing in order to exploit its
economic, technical, architectural and ecological
benefits (Andriole and Khorasani, 2010; Rosenthal
et. al, 2010). Cloud computing is an on-demand
service model for IT provision, often based on
virtualization and distributed computing
technologies; it refers to both the applications
delivered as services over the Internet and the
hardware and systems software in the data centers
that provide those services. The data center
hardware and software is what we will call a Cloud.
Thus, cloud computing may be divided into
Software as a service (SaaS), Platform as a service
(PaaS) and Infrastructure as service (IaaS) (Shimrat,
2009; van der Burg and Dolstra, 2009). Clouds may
also be divided into public, which are available
publicly (i.e. any organization may subscribe),
private, which are services built according to cloud
computing principles, but accessible only within a
private network and partner, which are cloud
services offered by a provider to a limited and well-
defined number of parties.
While cloud computing may seem like network
computing, a wide expanse of sky separates the two.
Networking involves a single entity and its servers.
Cloud computing encompasses multiple
organizations and their servers connected via the
Internet to build a more expensive network that can
facilitate potentially universal accessibility. The
concept has significant implications for medical
imaging and healthcare in general. Cloud computing
enables wider sharing (sending and receiving),
storage, access and manipulation of data, which can
be achieved in a cost-effective, secure and user-
friendly fashion (Buyya, Yeo, Venugopal, Broberg,
and Brandic, 2009; Armbrust, Fox, Griffith, Joseph,
Katz, Konwinski, et.al., 2009). Companies have
been offering cloud-based services such as archiving
and off-site backup for years. The off-site Picture
Archiving and Communication Systems (PACS)
archives that many firms offer are one example. A
new wrinkle unveiled in 2009 was using cloud-based
services to move healthcare information between
organizations – an approach to meeting the
interoperability objective. Hence, cloud computing
273
Koufi V., Malamateniou F. and Vassilacopoulos G..
AUTHORIZATION IN CLOUD E-RADIOLOGY SERVICES.
DOI: 10.5220/0003144402730279
In Proceedings of the International Conference on Knowledge Management and Information Sharing (KMIS-2010), pages 273-279
ISBN: 978-989-8425-30-0
Copyright
c
2010 SCITEPRESS (Science and Technology Publications, Lda.)

technology is changing the rules by enabling transfer
of medical images and associated information as
easily as sending an e-mail (Harvey, 2010).
Given the cloud computing benefits, a Personal
Healthcare Record (PHR) architecture based on a
combination of the above categories may be used to
allow authorized access to patient information at the
point of care, anytime. Moreover, cloud PHR
architectures can be used to incorporate, through
loosely coupling interfaces, crucial healthcare
delivery applications, such as eRadiology, requiring
little or no manual data entry of patient information
(Andriole and Khorasani, 2010). Usually,
eRadiology provides teleradiology services to
hospitals, imaging centers and physician group
practices by using high speed, secure internet
connections, instant messaging and advanced
Radiology Information System (RIS) and PACS
(Benjamin, Aradia, Shreibera, 2010; Telemedicine
Information Exchange – TIE Europe, 2005). This
technology also allows referring physicians with
electronic access to their patient’s images and
reports via a secure web viewer on the internet.
eRadiology also has the expertise to offer assistance
with the selection and acquisition of imaging
equipment.
The view of an eRadiology system as a cloud
computing application that interfaces with a PHR
implies that eRadiology is seen as a comprehensive
web-based application that streamlines and
automates the physician’s medical order processes
by enabling the electronic transmission of
radiological orders from physicians to medical
centers and, also, that allows physicians to check
patient history and best practice protocols and much
more to ensure that the radiological procedures
requested is the safest and most effective choice for
the patient (Ash, Berg and Coiera, 2004; Terry,
2008; Steele and Lo, 2009). Besides, an eRadiology
system can be used to facilitate and enhance
communication and coordination between referring
physicians and radiologists (Reid, 2010).
One important consideration in developing an
eRadiology system as a cloud application is security
since security is a priority for many cloud customers
(i.e. healthcare organizations) and, on several
occasions healthcare organizations will make buying
choices on the basis of the reputation for
confidentiality (Bruening and Treacy, 2009;
Pearson, 2009; U.S. Department of Health and
Human Services, 2004). For example, patients need
assurances that radiological order or response data
will not be used to harm them—for example,
through disclosure to a prospective employer. Thus,
there is need for adhering to appropriate privacy and
security rules to provide the necessary protections
and, to this end, audit trails and role-based access
controls are strongly recommended (Cavoukian,
2008; IBM Corporation, 2009; Muttig and Burton,
2009).
This paper focuses on a context-aware access
control mechanism incorporated into a prototype
eRadiology application (NefeliRadiology) which is
based on a prototype healthcare portal, called
NefeliPortal, which automates the physician
radiological request process while it enables access
to a cloud PHR. The proposed access control
mechanism incorporates the advantages of role-
based access control (RBAC) and yet provides the
flexibility for adjusting role permissions on
individual objects according to context. Thus, at run
time contextual information is collected to adapt
user permissions to the minimum required for
completing a job. Relevant access control policies
are enforced at both web service and BPEL task
levels.
2 MOTIVATING SCENARIO
To illustrate the main principles of the security
architecture incorporated into the NefeliPortal,
consider a healthcare process scenario concerned
with radiological medical orders (e-radiology).
Suppose a healthcare delivery situation where a
patient’s physician wishes to issue a radiological
request for one of his/her patients. The request is
sent to the radiology department of an appropriate
medical center which schedules the radiological
procedure requested and sends a message to the
requesting physician notifying him/her on the date
and time scheduled. After performing the
radiological procedure requested, the radiologist
assesses the relevant part of the patient record and
writes a radiological report, incorporating both the
radiological images and the associated assessment,
which is sent to the referring physician.
This scenario shows an example of how a cloud
eRadiology service may work: A physician uses an
eRadiology application which is interfaced to a PHR
stored in a data center, reads the summary record of
his/her current patient and selects one or more
radiological procedures to be performed on a patient
based on an assessment of patients condition. Upon
selection of a radiological procedure by the
physician, the eRadiology application performs
validation checks (e.g. with regard to best practice
protocols) to either clear the radiology order or
KMIS 2010 - International Conference on Knowledge Management and Information Sharing
274
return notice information to physician. Then, the
physician sends the radiological request to the data
center where the whole eRadiology activity is
captured. Finally, the patient books an appointment
with a medical center of his/her own choice for
performing the radiological procedures requested by
his/her physician. After performing the radiological
procedures requested, the radiological report
(incorporating both medical images and text) is
stored into the patient’s PHR which is situated in the
data center which is based on a cloud infrastructure
while providing relevant access to the referring
physician.
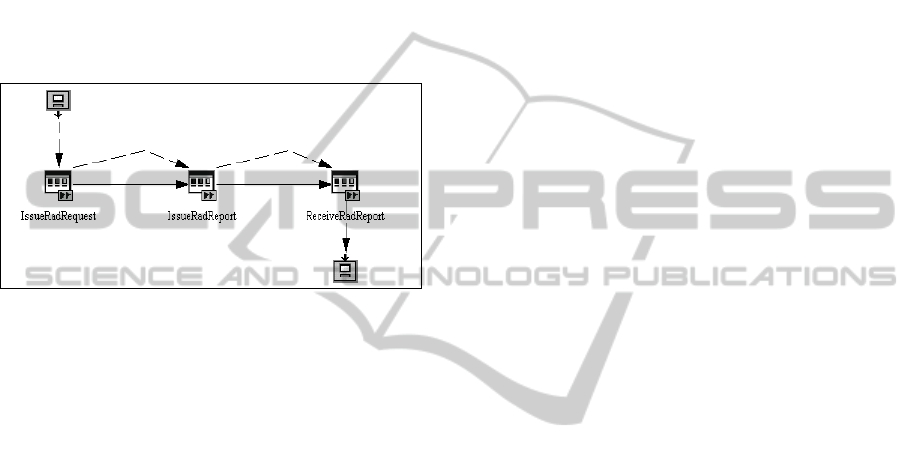
Figure 1: A high level model of an eRadiology process.
The benefits accrued from the implementation of
an eRadiology system are manifold: For example,
the service puts eligibility and insurance information
at the physician’s fingertips at the time of
radiological order. This enables physicians to select
the most effective radiological procedures for the
case in hand that are covered by the patient’s
insurance (Metfessel, 2007; Information Technology
in Healthcare, 2004). It also informs physicians of
lower cost alternatives. In addition, physicians can
access a timely and clinically sound view of a
patient’s history stored in patient’s PHR at the point
of care. This decreases the risk of preventable
medical errors (Metfessel, 2007; Kaelber, Shah,
Vincent, Pan, Hook, Johnson, et.al., 2008). Also,
radiological request routing replaces old, error-prone
approaches to sending new radiological requests
with the secure computer-to-computer exchange of
radiological requests between physicians and
medical centers. Routing new radiological requests
electronically reduces the risk of radiological
requests associated with poor handwriting, illegible
faxes and manual data entry. Using radiological
request routing to process radiological renewals
(radio-therapeutic services), saves physician time
and money by dramatically reducing the number of
phone calls and faxes typically associated with the
renewing authorization process (Collin, Reeves,
Hendy, Fulop, Hutchings and Priedane, 2008; Bell,
Cretin, Merken and Landman, 2004). Figure 1
shows a high-level view of the eRadiology process
using the IBM WebSphere Workflow build-time
tool (IBM Corporation, 2005). In this process two
healthcare providers are involved: the referring
physician and the radiologist.
From a role-based workflow authorization
perspective, the business process of Figure 1
surfaces several requirements with regard to task
execution and associated data accesses. These
requirements include the following:
Data Content - Some role holders should be
allowed to exercise a set of permissions on
certain data objects only. For example, during
the execution of the “IssueRadRequest” task, a
physician is allowed to read patient records
and issue (write, edit and send) radiological
requests only for his/her patients.
Permission Propagation - Some role holders
should receive additional permissions on
certain data objects in order to effectively
execute a task but these permissions should be
revoked upon successful execution of the task.
For example, for an effective execution of the
“IssueRadReport” task with regard to a
patient, a physician should receive the
permission to read the patient’s record but
he/she should not be allowed to retain this
permission after successful task execution.
Also, on patient’s appointment with a medical
center for performing radiological procedures,
the attending radiologists are granted the
authorization to read patient records.
Restricted Task Execution - In certain
circumstances the candidates for a task
execution should be dynamically determined
and be either a sub-group of the authorized
users or only one, specific authorized user. For
example, when a radiological request issued
by a physician is stored in the data center and
relevant access rights are routed only to the
appropriate group of medical centers (e.g.
within a health district).
Table 1 shows an extract of workflow
authorization requirements regarding task execution
and related data access privileges assigned to the
“referring physician” and “radiologist” roles,
respectively. Similar requirements exist in many
healthcare workflow application fields where
request-service situations occur (Poulymenopoulou,
Malamateniou and Vassilacopoulos, 2005).
These authorization requirements suggest that
certain data access permissions of the eRadiology
workflow participants depend on the eRadiology
AUTHORIZATION IN CLOUD E-RADIOLOGY SERVICES
275
process execution context. In particular, contextual
information available at access time, like location or
user/patient relationship, can influence the
authorization decision that allows a user to perform
a task and access associated data objects. This
enables a more flexible and precise authorization
policy specification that incorporates the advantages
of having broad, role-based permissions across
workflow tasks and data object types, like RBAC,
yet enhanced with the ability to simultaneously
support the following features: (a) predicate-based
access control, limiting user access to specific data
objects, (b) a permission propagation function from
one role holder to another in certain circumstances,
and (c) determining qualified task performers during
an eRadiology process instance based on the role-to-
task permission policy. In addition, the model should
not incur any significant administrative overhead
and should be self-administering to a great extent.
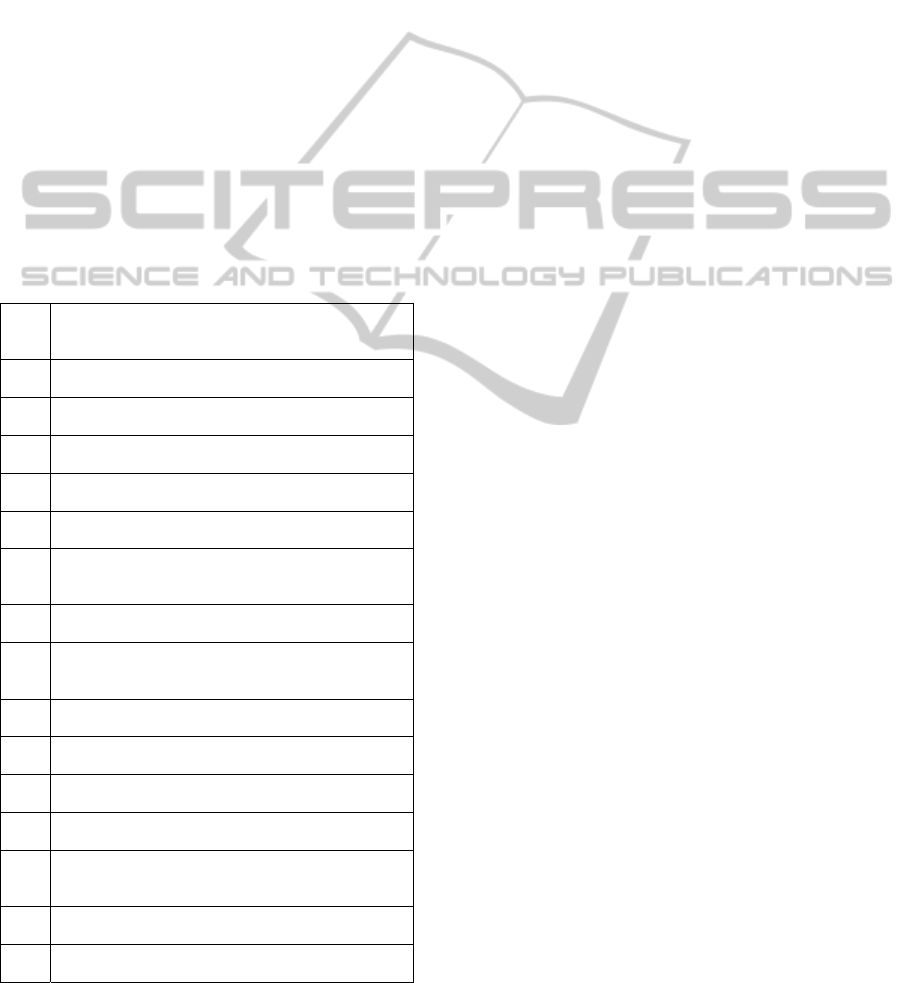
Table 1: Extract of authorization requirements for the
healthcare process of Figure 1 (Task execution and
application data access permissions).
1. Physicians may issue radiological requests for their
patients only.
(Issue_Rad_Request)
1.1 Physicians may write radiological requests for
their current patients.
1.2 Physicians may edit radiological requests for
their current patients before sent.
1.3 Physicians may send radiological requests for
their current patients.
1.4 Physicians may cancel radiological requests for
their current patients after sent.
1.5 Physicians may read patient records of their
patients only.
2. Radiologists may issue radiological reports for
patients on request by physicians.
(Issue_Rad_Report)
2.1 Radiologists may read patient radiological
requests issued by physicians
2.2 Radiologists may read patient records of patients
they are requested to issue radiological reports
for.
2.3 Radiologists may write patient radiological
reports.
2.4 Radiologists may edit patient radiological reports
before sent.
2.5 Radiologists may send patient radiological
reports to the requesting physicians.
2.6 Radiologists may read past patient radiological
reports prepared by them.
3. Physicians may receive patient radiological reports
issued by radiologists only if requested by them.
(Receive_Rad_Report)
3.1 Physicians may read the radiological reports
issued by radiologists on request by them.
3.2 Physicians may read patient records of their
patients.
Given a cloud computing PHR architecture,
where patient data are accessed via web services
deployed through BPEL, these authorization
requirements of the eRadiology process can be
translated into authorization requirements with
regard to web service invocations and associated
task executions. These requirements include the
following:
Restricted Web Service Invocation: Web
services for eRadiology and PHR access can
only be invoked (executed) by a dynamically
determined set of role holders subject to
contextual constraints (e.g. user/patient
proximity as well as location and time of
attempted access).
Restricted Task Execution: Given an
authorization for invoking a web service, role
holders can execute a dynamically determined
set of web service tasks subject to contextual
constraints (e.g. user/patient proximity as well
as location and time of attempted access).
3 ACCESS CONTROL
ARCHITECTURE
A major pain point in cloud computing is the lack of
delegated authorization. While some cloud services
provide for delegated strong authentication (e.g.,
Salesforce.com) that enables access control based on
user identity, few, if any, provide delegated
authorization to enable access control based on
contextual information and user roles. This
capability is turning out to be increasingly important
as fine-grained entitlements for authorization
management and control will be most essential.
Hence, more granular authorization is needed.
Authorization can be coarse-grained within an
enterprise or even a private cloud, but in order to
handle sensitive (such as medical) data and
compliance requirements, public clouds will need
granular authorization capabilities (such as role-
based controls and IRM) that can be persistent
throughout the cloud infrastructure and the data’s
lifecycle.
Figure 2 shows a high-level view of the security
architecture implemented into NefeliRadiology. The
access control mechanism uses collected contextual
information to mediate between subjects (healthcare
professionals) and objects (web services and
associated tasks) to decide whether execution of an
object by a given subject should be permitted or
denied. The access control mechanism is certificate-
KMIS 2010 - International Conference on Knowledge Management and Information Sharing
276
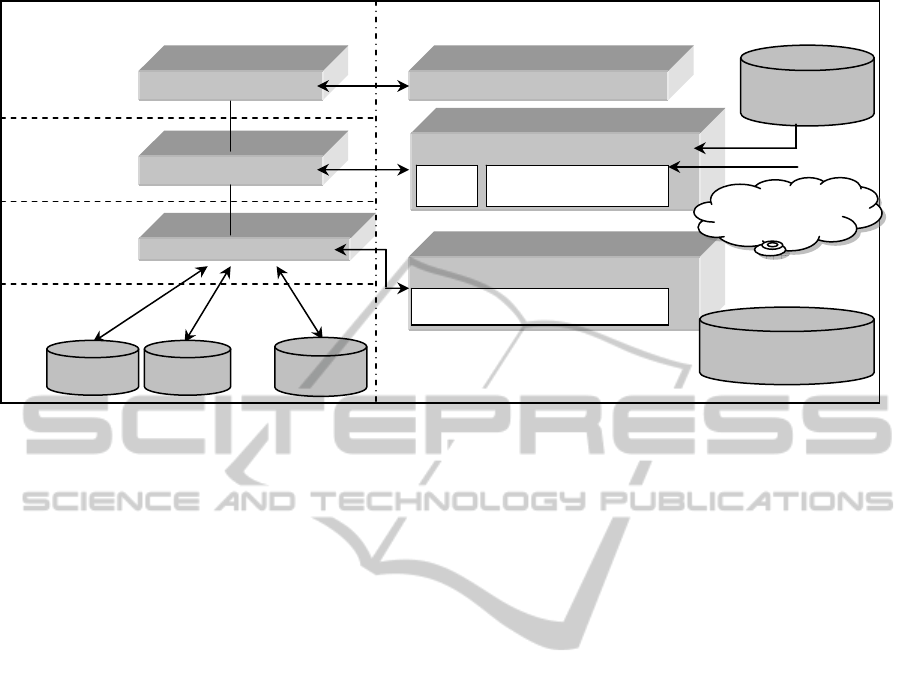
Figure 2: Security architecture in NefeliRadiology.
based as it relies on Community Authorization
Service (CAS) certificates issued to healthcare
professionals by a CAS server. These certificates
specify user-to-role assignments in the form of
security assertions, expressed in Security Assertion
Markup Language (SAML) (Pearlman et. al., 2002).
The role-to-permission (role-to-web service
invocation and role-to-task execution) mapping is
performed by means of access control policies
expressed by using the RBAC profile of eXtensible
Access Control Markup Language (XACML)
(OASIS Standards, n.d).
For example, upon submitting a request for
invoking a web service, the roles contained in the
CAS certificate accompanying the request are
extracted and their permissions regarding web
service invocations are specified using a file where
XACML policies have been stored. Then, during
web service execution, a request for executing one
of the associated tasks is issued which is
accompanied by the same CAS certificate. The roles
extracted from this certificate are used in order to
specify the permissions regarding BPEL task
executions using XACML policies which are stored
at each client node (i.e. healthcare organization).
Permissions on both web services and associated
BPEL tasks are dynamically adapted by the
constraints imposed by the current context.
In the NefeliRadiology prototype, the contextual
information is determined by a pre-defined set of
attributes related to the user (e.g. user certificate,
user/patient relationship), to the environment (e.g.
location and time of attempted access) and to the
client or healthcare organization (e.g. local security
policy). Contextual information is collected by a
Context Manager which consists of two kinds of
agents developed in JADE (Java Agent
Development Framework, n.d.):
Cloud Agent: Hosted on a cloud server and
manages user permissions on web services.
Task Agent: Hosted on a participating
healthcare organization server and manages
user permissions on BPEL tasks.
Each agent uses context collection services to
monitor context and interacts with a state machine
that maintains the permission subset of each role.
The state machine consists of variables that encode
state (permissions assigned to each role) and events
that transform its state. Upon an attempted access
(either to a web service or to an associated task), the
relevant agent generates an event to trigger a
transition of the state machine. Changes in user and
environmental context are sensed by both agents,
whereas changes in client context are sensed and
dealt with by the cloud agent of each client node.
4 CONCLUSIONS
Development of cloud computing applications that
provide readily access to healthcare information
introduces security risks especially with regard to
authorization and access control. One important
healthcare delivery application is eRadiology which
has been defined as the process of physicians (e.g.
clinicians in hospital and ambulatory settings,
general practitioners) directly entering radiological
Application Services
Presentation
Layer
Integration
Layer
Existing
Databases
Web
Services
NefeliPo
r
tal
BPEL Engine
Application Server
Authentication & Authorization Services
Authentication Service
Global Access Control Service
Task Agent
CAS
Local Access Control Service
Cloud Agent
Policy
Repository
Local Policy
Repository
Database
Database
Context
Information
Database
AUTHORIZATION IN CLOUD E-RADIOLOGY SERVICES
277

requests using computer applications that provide
decision support and can deliver the requests
electronically in structured form to appropriate
medical organizations (e.g. diagnostic centers,
hospitals). Moreover, the radiological reports
(incorporating image and text) are stored in a cloud
infrastructure while granting relevant access rights
to referring physicians. Hence, the term
"eRadiology" has been used regardless of whether
such radiological requests are subsequently printed
and given to the patient, faxed to a medical center,
or delivered through more structured electronic
transfer. In this framework, the proposed security
mechanism, embedded into an eRadiology cloud
portal application, ensures authorized invocation of
web services and execution of associated BPEL
tasks subject to the constraints imposed by the
execution context. One particular assumption of the
proposed system specifically calls for the integration
of eRadiology systems with PHRs and, possibly,
other external systems since systems integration is a
prerequisite for accurate safety alerts, patient
monitoring and other recommended capabilities. The
security framework proposed should aid eRadiology
developers in comparing alternative systems and in
prioritizing their development efforts. However,
there is an obvious need for its real world validation
before it is widely adopted. This requires setting up
a cloud computing infrastructure for eHealth
services, an endeavour that needs much more than
proven technological feasibility.
REFERENCES
Andriole, K.P., Khorasani R., 2010. Cloud Computing:
What Is It and Could it Be Useful?. In Journal of
American College of Radiology, Vol.7, No. 4, pp. 252-
254.
Armbrust, M., Fox, A., Griffith, R., Joseph, A.D., Katz, R.
H., Konwinski, A., Lee, G., Patterson, D.A., Rabkin,
A., Stoica, I., Zaharia, M., 2009. Above the Clouds: A
Berkely View of Cloud Computing. Technical Report
No. UCB/EECS-2009-28, http://www.eecs.
berkeley.edu/Pubs/TechRpts/2009/EECS-2009-
28.html.
Ash, J., Berg, M., Coiera, E., 2004. Some Unintended
Consequences of Information Technology in Health
Care: The Nature of Patient Care Information System
Related Errors. In Journal of the American Medical
Informatics Association,Vol. 11, No. 2, pp. 104-112.
Bell, D.S., Cretin, S., Marken, R.S., Landman, A.B., 2004.
A Conceptual Framework for Evaluating Outpatient
Electronic Prescribing Systems Based on Their
Functional Capabilities. In Journal of the American
Medical Informatics Association, Vol. 11, No. 1, pp.
60-70.
Benjamin, M., Aradia, Y., Shreibera, R., 2010. From
shared data to sharing workflow: Merging PACS and
teleradiology. In European Journal of Radiology, Vol.
73, pp. 3-9.
Bruening, P., Treacy, B, 2009. Cloud Computing: Privacy,
Security Challenges. In The Bureau of National
Affairs.
Buyya, R., Yeo, C.S., Venugopal, S., Broberg, J., Brandic,
I., 2009. Cloud computing and emerging IT
platforms:Vision, hype, and reality for delivering
computing as the 5th utility. In Future Generation
Computer Systems, Vol 25, pp. 599-616.
Cavoukian, A., 2008. Privacy in the clouds. In Identity in
the Information Society, Vol. 1, No. 1, pp. 89-108.
Collin, S., Reeves, B.C., Hendy, J., Fulop, N., Hutchings,
A., Priedane, E., 2008. Implementation of
computerised physician order entry (CPOE) and
picture archiving and communication systems (PACS)
in the NHS: quantitative before and after study. In
British Medical Journal, 337:a939.
Harvey, D., 2010. Record in the Clouds. In Radiology
Today, Vol. 11, No. 2, p. 10.
IBM Cloud computing White paper, 2009. IBM Point of
View: Security and Cloud Computing,
ftp://public.dhe.ibm.com/common/ssi/sa/wh/n/tiw1404
5usen/TIW14045USEN_HR.pdf.
IBM Corporation, 2005. IBM Websphere Workflow –
Getting Started with Buildtime V. 3.6.
Information Technology in Healthcare, 2004. Report to
the Congress: New Approaches in Medicare,
http://www.medpac.gov/publications/congressional_re
ports/June04_ch7.pdf.
Java Agent Development Framework,
http://jade.tilab.com/.
Kaelber, D.C., Shah, S., Vincent, A., Pan, E., Hook, J.M.,
Johnston, D., Bates, D.W., Middleton, B., 2008. The
Value of Personal Health Records, By the Center for
Information Technology Leadership (CITL),
http://www.citl.org/publications/_pdf/CITL_PHR_Rep
ort.pdf.
Metfessel, B.A., 2007. Financial and Clinical Features of
Hospital Information Systems. In Healthcare
Organizations, Journal of Financial Management
Strategies, Vol. 2, No. 3.
Muttig I., Burton C., 2009. Cloud Security Technologies.
In Information Security Technical Report, Vol. 14, pp.
1-6.
OASIS Standards, http://www.oasis-open.org/.
Pearson, S., 2009. Taking Account of Privacy when
Designing Cloud Computing Services. Proceedings of
the 2009 ICSE Workshop on Software Engineering
Challenges of Cloud Computing, Vancouver, Canada.
Pearlman, L., Welch, V., Foster, I., Kesselman, C.,
Tuecke, S., 2002. A Community Authorization
Service for Group Collaboration. Proceedings of the
3rd IEEE International Workshop on Policies for
Distributed Systems and Networks, Monterey, USA.
Polymenopoulou, M., Malamateniou, F., Vassilacopoulos,
G., 2005. Emergency Healthcare Process Automation
KMIS 2010 - International Conference on Knowledge Management and Information Sharing
278

using Workflow Technology and Web Services. In
International Journal of Medical Informatics, Vol. 28,
No. 3, pp. 195-207.
Reid, W., 2010. Managing the Flow of Radiology. In
Imaging Economics, May 2010.
Rosenthal, A., Mork, P. Li, M.H., Stanford, J., Koester,
D., Reynolds, P., 2010. Cloud computing: A new
business paradigm for biomedical information sharing.
In Journal of Biomedical Informatics, Vol. 43, pp.
342-253.
Shimrat, O., 2009. Cloud Computing and Healthcare, San
Diego Physician.org.
Steele, R., Lo, A., 2009. Future Personal Health Records
as a Foundation for Computational Health, In
Computational Science and Its Applications – ICCSA,
Vol. 5593, pp. 719-733.
Telemedicine Information Exchange-TIE Europe., 2005.
How e-radiology can help?,
http://tie.telemed.org/europe/toolkits/kitdom.asp?load
=toc&name=telerad.
Terry, M., 2008. Personal Health Records - Who are the
key PHR providers and how are they handling
laboratory results, Washington G2 Reports,
http://www.g2reports.com/issues/advisory/advisory/m
ark_terry/345-1.html.
U.S. Department of Health and Human Services, Office of
the Secretary, 2004. 45 CFR Part 162. Standard
Unique Health Identifier for Health Care Providers. In
Federal Register, Vol. 69, No. 15, pp. 3434–3469.
van der Burg, S., Dolstra, E., 2009, Software Development
in a Dynamic Cloud: From Device to Service
Orientation in a Hospital Environment. Proceedings of
the 2009 ICSE Workshop on Software Engineering
Challenges of Cloud Computing, Vancouver, Canada.
AUTHORIZATION IN CLOUD E-RADIOLOGY SERVICES
279
