
AUTOMATING AUTHORIZATION PROPAGATION PROCESS
IN PERSONAL HEALTH RECORDS
Vassiliki Koufi, Flora Malamateniou and George Vassilacopoulos
Department of Digital Systems, University of Piraeus, 80, Karaoli & Dimitriou Str., Piraeus 18534, Greece
Keywords: Personal health records, Information availability, Access control, Emergency, Authorization propagation.
Abstract: Traditionally patient records are generated, maintained and controlled by the individual health care
providers where the patient has received care. This results in fragmented bits of data stored in diverse
information systems which, in many cases, are not interoperable. Hence, a complete picture of a person’s
healthcare record cannot be obtained when and where needed. A solution to this problem can be provided
by personal health records (PHR), that is electronic health records (EHR) whose architectures are based on
the fundamental assumptions that the complete records are centrally stored and that each patient retains
authority over access to any portion of his/her record. This paper deals with a particular security issue
arising in PHRs which is concerned with the process of granting (revoking) authorization to (from)
healthcare professionals without the patient’s involvement. This security issue is particularly important in
managing emergency cases. To deal with this problem, authorization propagation process is automated by
means of context-aware technology, which is used to regulate user access to data via a fine-grained access
control mechanism.
1 INTRODUCTION
Throughout their lives individuals receive care in
different parts of the health care system. This results
in patient health data being scattered around
disparate and geographically dispersed information
systems hosted by different healthcare providers
(Koufi and Vassilacopoulos, 2008;Tang, Ash, Bates,
Overhage and Sands, 2006). The lack of
interoperability among these systems impedes
optimal care as it leads to unavailability of important
information regarding patient health status when this
is mostly needed (e.g. in case of an emergency).
Recently there has been a remarkable upsurge in
activity surrounding the adoption of Personal Health
Record (PHR) systems for patients (Tang, Ash,
Bates, Overhage and Sands, 2006). A PHR is a
consumer-centric approach to making
comprehensive electronic medical records (EHRs)
available at any point of care while fully protecting
patient privacy (Lauer, 2009). Unlike traditional
EHRs which are based on the 'fetch and show'
model, PHRs’ architectures are based on the
fundamental assumptions that the complete records
are held on a central repository and that each patient
retains authority over access to any portion of
his/her record (Lauer, 2009; Wiljer, Urowitz, Apatu,
DeLenardo, Eysenbach, Harth, Pai, Leonard, 2008).
Thus an entire class of interoperability is eliminated
since the system of storing and retrieving essential
patient data is no longer fragmented. Hence, quality
and safety of patient care is enhanced by providing
patients and health professionals with relevant and
timely information while ensuring protection and
confidentiality of personal data.
Providing patients with access to their electronic
health records offers great promise to improve
patient health and satisfaction with their care, as well
as to improve professional and organizational
approaches to health care (Wiljer, Urowitz, Apatu,
DeLenardo, Eysenbach, Harth, Pai and Leonard,
2008). Although many benefits have been identified,
there are many questions about best practices for the
implementation of PHR systems (Wiljer, Urowitz,
Apatu, DeLenardo, Eysenbach, Harth, Pai and
Leonard, 2008). A number of these questions are
related to security issues arising in PHR systems.
As any other EHR system, PHR systems require
stringent privacy protections to prevent unauthorized
access or use (Yasnoff, 2008; Comini, Mazzu and
Scalvini, 2008; Win, Susilo and Mu, 2006). Most
PHR platforms currently deployed (e.g. Microsoft
82
Koufi V., Malamateniou F. and Vassilacopoulos G. (2010).
AUTOMATING AUTHORIZATION PROPAGATION PROCESS IN PERSONAL HEALTH RECORDS.
In Proceedings of the Third International Conference on Health Informatics, pages 82-89
DOI: 10.5220/0002747200820089
Copyright
c
SciTePress

HealthVault, ICW LifeSensor) meet these
requirements by assigning the patient with the
responsibility of granting access to information
comprising his/her health record while access to
important information (e.g. blood type, allergies etc)
is provided to medical staff in case of an emergency
by means of an emergency data set. Although this
information is valuable while providing first aid to
the patient, a more comprehensive view of the
his/her health data is required by the medical staff
upon arrival to the emergency department of a
hospital.
This paper deals with the particular security
issue arising in PHR systems which is concerned
with the process of granting (revoking) authorization
to (from) healthcare professionals without the
patient’s involvement. This security issue is
particularly important in managing emergency cases.
To deal with this problem, authorization propagation
process is automated by means of context-aware
technology, which is used to regulate user access to
data via a fine-grained access control mechanism.
The latter is a role-based, context-aware access
control mechanism that incorporates the advantages
of broad, role-based permission assignment and
administration across object types, as in role-based
access control (RBAC) (National Institute of
Standards and Technology, 2009), and yet provides
the flexibility for automatically adjusting access
permissions on a patient’s PHR on the occurrence of
unpredictable events (e.g. emergency case).
2 RELATED WORK
During the last few years, there has been a growing
interest in the utilization of PHR systems as both
patients and healthcare organizations realized that
their use may entail a number of benefits, such as
better access to information, increased patient
satisfaction and continuity of care (Tang, Ash,
Bates, Overhage and Sands, 2006; Wiljer, Urowitz,
Apatu, DeLenardo, Eysenbach, Harth, Pai, Leonard,
2008). However, certain barriers to the integration of
PHR systems to the clinical practice have been
identified, most of them related to security issues
(Tang, Ash, Bates, Overhage and Sands, 2006;
Wiljer, Urowitz, Apatu, DeLenardo, Eysenbach,
Harth, Pai, Leonard, 2008). In recognition of these
barriers, a number of mechanisms have been
developed in an attempt to address several issues
mostly regarding access control over the health data
comprising a PHR (Røstad and Nytrø, 2008; Win,
Susilo and Mu, 2006; Comini, Mazzu and Scalvini,
2008.). Some of them are concerned with the
provision of access to important healthcare
information in case of an emergency.
In Case of Emergency Personal Health Record
(icePHR) (Metavante, 2009) and My Personal
Health Record (myPHR) (My Personal Health
Record, 2009) are applications which, among others,
ensure that life saving information is available when
most needed (i.e. in case of an emergency). To this
end, they provide patients with the ability to upload
important health information and then print their
own emergency card with information on how to
access their own unique, secure web page with this
emergency information. However, they don’t
provide mechanisms for ensuring instant availability
of a complete copy of a patient’s record to the
medical staff treating him/her without the patient’s
involvement.
The system architecture proposed in this paper
utilizes agent technology in an attempt to automate
authorization propagation process in cases that a
patient in incapable of being involved in this
process. To this end, a context-aware access control
mechanism has been developed which is triggered
when appropriate in order to derive and grant the set
of authorizations needed for the treatment of a
patient.
3 MOTIVATING SCENARIO
The basic motivation for this research stems from
our involvement in a recent project concerned with
designing and implementing a PHR system for the
provision of data access at any point of care while
fully protecting privacy. This involves providing
access to the appropriate people, based on patient
wishes, but also granting access to the patient’s data
in cases where his/her involvement in the
authorization propagation process is not feasible.
The stringent security needs of the system, where
sensitive patient information is used, motivated this
work and provided some of the background
supportive information for developing the prototype
presented in this paper.
Suppose a healthcare delivery situation that takes
place within a health district where an individual is
transferred to a hospital’s emergency department
(ED). Upon arrival to the ED, the individual is
registered as an emergency patient and undergoes a
brief triage in order for the nature and severity of
his/her illness to be determined. If his/her illness or
injury is considered to be serious he/she is seen by a
physician more rapidly than the patients with less
AUTOMATING AUTHORIZATION PROPAGATION PROCESS IN PERSONAL HEALTH RECORDS
83
severe symptoms or injuries. After initial assessment
and treatment, the patients is either admitted to the
hospital (e.g. to a clinical department or the
Intensive Care Unit - ICU), stabilized and
transferred to another hospital for various reasons, or
discharged (Wikipedia, 2009).
Typically, a health district consists of one district
general hospital (DGH) and a number of peripheral
hospitals and health centers.
As many emergency department visits are
unplanned and urgent, there is a need to ensure that
information regarding the longitudinal patient health
condition (e.g., problems, allergies, medications,
diagnoses, recent procedures, recent laboratory tests)
is conveyed to ED physicians automatically upon
registration of a patient to an ED. Thus,
inefficiencies in care, in the form of redundant
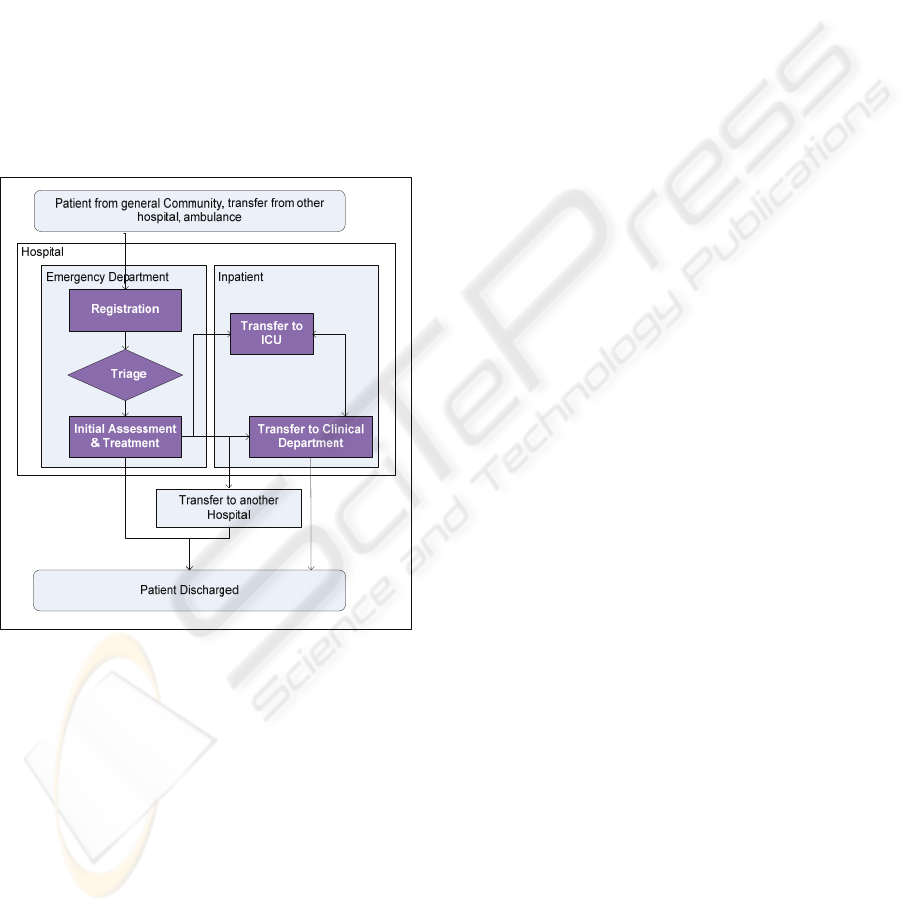
Figure 1: Patient Flow.
testing, care delays, and less-effective treatments
prescribed are eliminated and quality of care is
enhanced.
Figure 1 shows an indicative high-level view of
the patient flow from the time he arrives at a
hospital’s emergency department to the time he is
discharged. Some of the roles participating in the
patient’s treatment are physician, nurse, physician
assistant (PA), nurse practitioner with specialized
training in emergency medicine and in house
Paramedics and other support staff.
From an authorization perspective, the following
two requirements are of interest here.
Data access - A role holder should be allowed to
exercise a dynamically determined set of
permissions on certain data objects only. For
example, a patient’s personal physician, if
authorized by the patient himself, is allowed to
read certain parts of his/her medical record and to
update it.
Permission propagation - Some role holders
should receive additional permissions on certain
data objects in order to effectively treat the patient
but these permissions should be revoked upon
patient discharge. For example, for forming an
appropriate plan of care, an ED physician should
receive the permission to read the complete record
of a patient but he/she should not be allowed to
retain this permission after the patient has been
discharged.
The above requirements suggest that certain data
access permissions of the medical staff participating
in a patient’s treatment may change without the
patient’s intervention depending on the context (e.g.
in the case that an individual is registered as an
emergency patient). Moreover, contextual
information, such as time and location of attempted
access, can influence authorization decisions on
certain data objects comprising a patient’s PHR.
This enables a more flexible and precise access
control policy specification that satisfies the least
privilege principle by incorporating the advantages
of having broad, role-based permissions across data
object types, like RBAC, yet enhanced with the
ability to simultaneously support the following
features: (a) predicate-based access control, limiting
user access to specific data objects, and (b) a
permission propagation function to specific role
holders in certain circumstances.
4 SYSTEM ARCHITECTURE
The prototype system described here facilitates
access to comprehensive patient information which
is stored in a central repository. In this environment,
a robust security framework is in place in order to
ensure that health information follow patients
throughout their care in a secure manner and that
comprehensive information is made available to
appropriate people when this is mostly needed (e.g.
in case of an emergency) without the patient’s
involvement. Figure 2 shows a high-level system
architecture, which is described by a three-tier
model, comprising of the terminal station used by
the medical staff at the department where the patient
is being treated (e.g. ED, ICU etc), the PHR
HEALTHINF 2010 - International Conference on Health Informatics
84
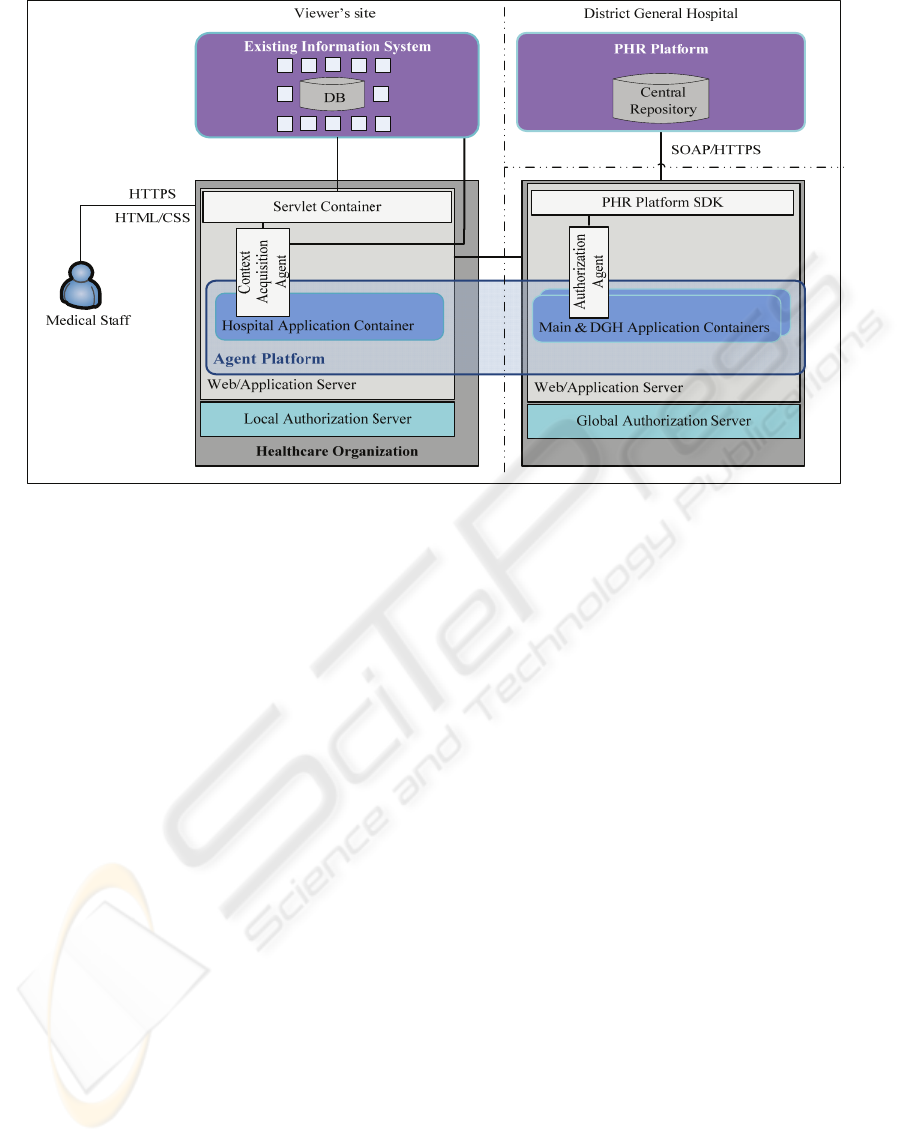
Figure 2: System Architecture.
platform and the application accessing the PHR
platform.
The first tier is the terminal station used by the
medical staff treating the patient (e.g. physician,
nurse etc.). The terminal contains an HTTP(S)-based
client, which is the terminal’s web browser and
provides user interaction with the system.
The second tier of the system architecture is the
platform used for the implementation of the PHR
system. This supports both patients in actively
managing their own health and the medical staff
(e.g. physicians) by ensuring the quick and secure
availability of a patient’s health data such as
diagnosis, therapy and prescription data. In such a
PHR system access authorization is exclusively
granted by the owner (patient) of the record or by a
“gatekeeper” he/she assigns (e.g. a relative) (ICW
eHealth Framework, 2009). Different read and write
permissions can be granted to and be withdrawn
from the various users at any time through a terminal
station.
The third tier is the application which is
distributed among several hosts residing at the DGH
and the other healthcare institutions. The
infrastructure of this tier consists of the following
components:
PHR Platform SDK: It is used for the simple
integration of our application into the PHR
infrastructure. It provides an Application
Programming Interface (API) which can be
accessed from JSP/Servlet pages.
Agent Platform: It is the software used for the
implementation of the agents which realize the
automation of the authorization propagation
process in order to support healthcare
professionals and frontline staff at the point of
care by ensuring instant availability of the
complete copy of a patient’s medical record.
Servlet Container: It provides a servlet
container that hosts and manages the servlets
delivering the system functionality. Essentially
these servlets provide a web-based front end to
the PHR system.
Web/Application Server: It provides the hosting
environment to the aforementioned components.
All web transactions are executed under the
Secure Socket Layer (SSL) via HTTPS. In addition,
security in communication among the agents of the
agent platform is ensured by setting up a secure,
confidential and mutually authenticated, connection
amongst containers of the agent platform by
leveraging TLS/SSL support provided by Java (Java
Agent Development Framework, 2008).
5 SECURITY ARCHITECTURE
The movement towards PHR systems has created
new challenges for the sharing of health information
in a private and secure manner. In particular, when
situations occur where access to medical
AUTOMATING AUTHORIZATION PROPAGATION PROCESS IN PERSONAL HEALTH RECORDS
85
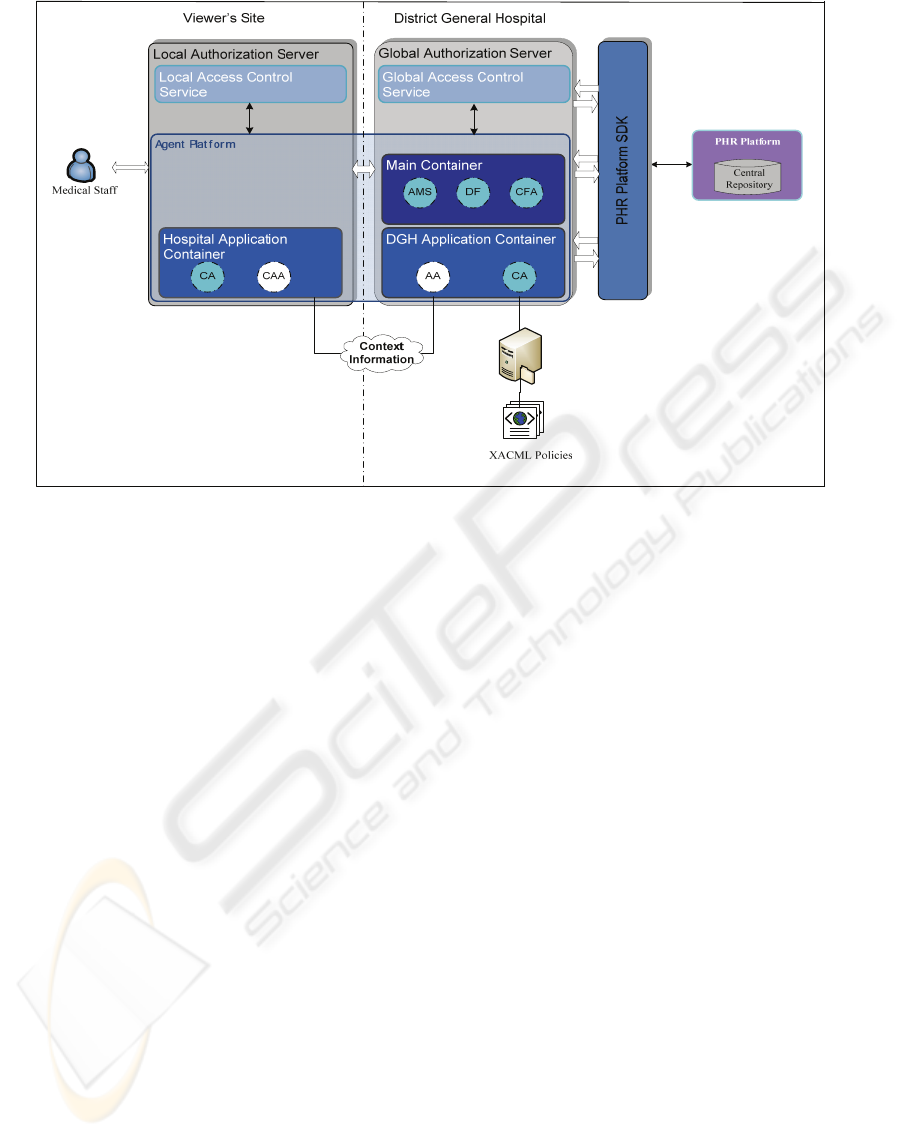
Figure 3: Security Architecture.
information is required but patients cannot grant
permissions to the medical staff needing the
information for treating them, effort should be put in
the development and enforcement of a mechanism
that automates the authorization propagation process
while ensuring privacy and security against
unauthorized access to the data.
The number, type and sophistication of tools that
protect information in PHR environments are
growing at an ever-increasing rate and provide the
opportunity to offer health privacy protections
beyond those in the paper environment. In many
cases, the utilization of role-based access controls is
considered as an effective means of limiting access
to a patient’s information to only those individuals
who need it for the patient’s treatment.
In our prototype system, a dynamic access
control mechanism is incorporated which is based on
the role-based access control (RBAC) paradigm and
is context-aware. As illustrated in Figure 3, this is
described by a two-tier model consisted of a global
access control service, residing on a server at the
DGH site, and one local access control service,
residing at the viewer’s site (i.e. any healthcare
organization within the health district). Both services
have been implemented using the Java
Authentication and Authorization Service (JAAS)
(Java Authentication and Authorization Service,
2008) and use a number of agents for context
management.
The access control mechanism developed is
middleware-based and its role is twofold. In
particular, it is employed to:
- Grant/revoke authorizations of given subjects to
(from) given objects by taking into account the
current context (e.g. upon registration of an
individual as an emergency patient). In order
for these authorizations to be determined a set
of access control policies are used by means of
which role-to-permission assignments are
specified.
- Mediate between subjects (healthcare
professionals) and objects (data objects) and
decide whether access of a given subject to a
given object should be permitted or denied
according to the context holding at the time of
the attempted access (e.g. when the physician
of the ED requests access to a patient’s PHR).
In our prototype, users authenticate themselves
by using X.509 certificates.
5.1 Access Control Policies
In our prototype system, the mapping of roles to the
relevant permissions is performed by means of
access control policies expressed by using the Core
and Hierarchical RBAC profile of eXtensible Access
Control Markup Language (XACML) (Organization
for the Advancement of Structured Information
Standards, 2008). These policies are expressed in the
HEALTHINF 2010 - International Conference on Health Informatics
86
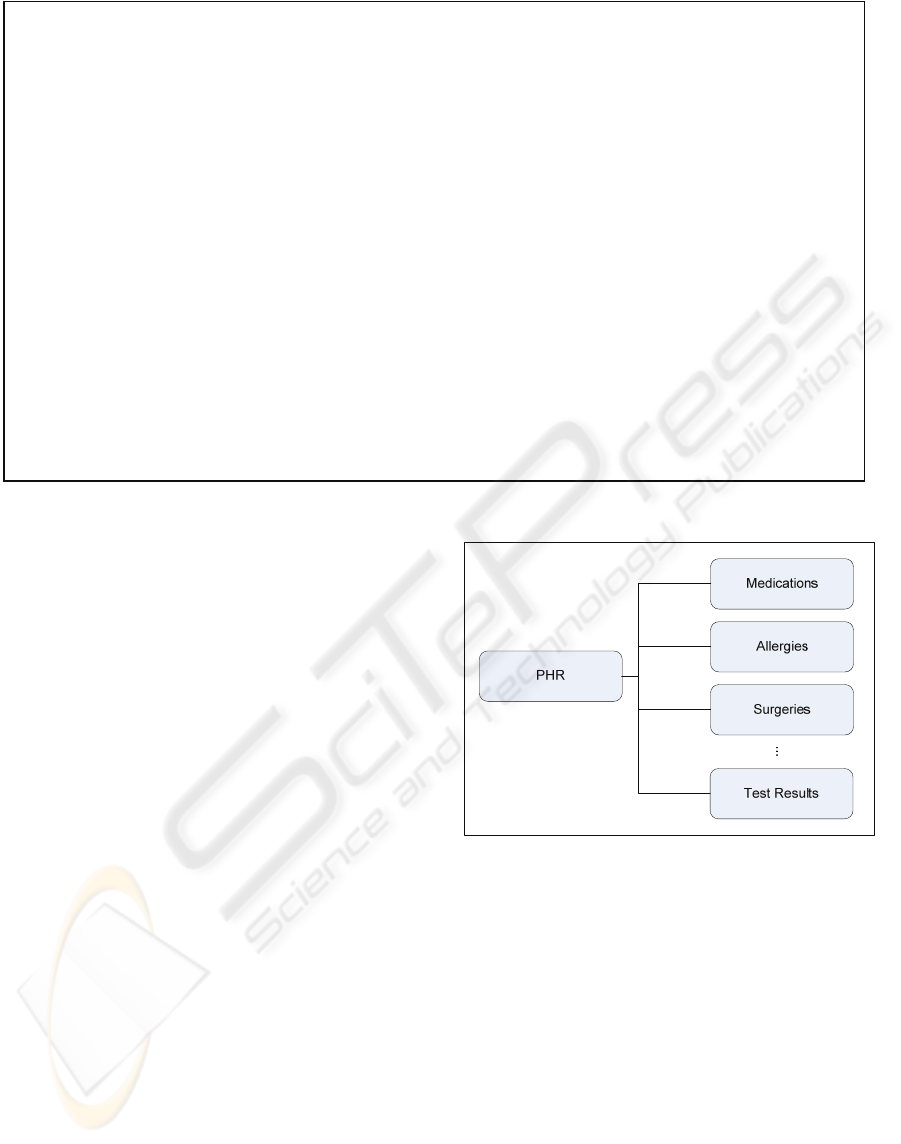
Figure 5: Sample Access Control Policy for Physician.
form of roles, role hierarchies, privileges and
constraints.
Due to the strict security requirements on
medical data comprising a PHR, the specification of
access control policies not for the entire record but
for its components (i.e. data objects) is of utmost
importance. Since the record is organized as a
hierarchy, when specifying policies on it the
hierarchical resource profile of XACML
(Organization for the Advancement of Structured
Information Standards, 2008) can be used for the
representation of these components. This profile
specifies how XACML provides access control for
resources that are organized as a hierarchy, such as
file systems, XML documents and databases.
According to this profile, non-XML data can be
represented by a URI of the following form:
<scheme>://<authority>/<pathname>
where:
<scheme> identifies the namespace of the URI
and can be either a protocol (e.g. “ftp”, “http”,
“https”) or a file system resource declared as
“file”.
<authority> is typically defined by an Internet-
based server or a scheme-specific registry of
naming authorities, such as DNS, and
<pathname> is of the form <root name>{/<node
name>}. The sequence of <root name> and
<node name> values should correspond to the
components in a hierarchical resource.
Figure 4: PHR Data Model.
Suppose that the data structure of a PHR is the
one illustrated in Figure 4. Then the data object
“Allergies” would be represented as follows:
“https://localhost:8443/PHR/Allergies”
The policies related to the permissions on data
objects a healthcare professional should acquire
while treating patient reside on a server at the DGH
site. An excerpt of an access control policy for role
“physician” is shown in Figure 5. This is a relatively
simple policy that states that an ED physician is
authorized to access the complete medical record of
each patient he treats. This is specified within the tag
<Resource> by means of the predicate “all” while
the predicate “all” within the tag <Action> means
that the physician has all kinds of permissions on the
<Resource>
<ResourceMatch MatchId="&function;string-equal">
<AttributeValue DataType="&xml;string">all
</AttributeValue>
...
</ResourceMatch>
</Resource>
...
<Action>
<ActionMatch MatchId="&function;string-equal">
<AttributeValue DataType="&xml;string">all</AttributeValue>
...
</ActionMatch>
</Action>
<Condition>
<Apply FunctionId="&function;string-equal">
<EnvironmentAttributeDesignator AttributeId="urn:oasis:names:tc:xacml:2.0:environment:terminal"
DataType="&xml;string"/>
<AttributeValue DataType="&xml;string">inPremises</AttributeValue>
</Apply>
<
/
Condition>
AUTOMATING AUTHORIZATION PROPAGATION PROCESS IN PERSONAL HEALTH RECORDS
87

patient’s medical record. Permissions on data
objects are dynamically adapted by the constraints
imposed by the current context. These are declared
within the tag <Condition> and for the role
“physician” is whether he/she is requesting patient
information using a terminal within the hospital
premises.
5.2 Context Information Management
In our prototype system, the management of context
information influencing authorization decisions is
performed by a Context Manager. Both the context
information model and the Context Manager are
described below.
5.2.1 Context Information Model
In our prototype system, the contextual information
influencing authorization decisions is determined by
a pre-defined set of attributes related to:
the user (e.g. user certificate, user/patient
relationship) and
the environment (e.g. client location and time of
attempted access)
the healthcare provider (e.g. physicians on duty)
For example, the permissions of an ED physician
accessing the system via a terminal, are adapted
depending on his/her identity (included in his
electronic Health Card) as well as the location of the
terminal and time of attempted access.
5.2.2 Context Manager
Context information is collected by a Context
Manager which has been implemented as a multi-
agent system. Thus, the Context Manager consists of
two kinds of agents, developed in JADE (Java Agent
Development Framework, 2008):
Context Acquisition Agent (CAA): It is hosted
on a server at the site of the healthcare
organization where the ED belongs and is
responsible for the acquisition of the contextual
information required for granting authorizations
and taking authorization decisions regarding
access on the data objects comprising a patient’s
PHR.
Authorization Agent (AA): It is hosted on a
server at the DGH and is responsible for
automatically granting (revoking) authorization
to (from) healthcare professionals without the
patient’s involvement. Moreover, it is
responsible for managing access to patients’
PHRs.
6 IMPLEMENTATION ISSUES
To illustrate the functionality of the proposed
architecture, a prototype system has been developed
which is based on the case scenario of Section 3.
The prototype implementation of the proposed
system and the security services incorporated in it
has been developed in a laboratory environment. In
our implementation Apache/Tomcat is used as
Web/Application Server while agents are developed
using JADE (Java Agent Development Framework,
2008). The databases used by the existing
information systems are developed using MySQL.
The PHR system is implemented using the ICW
Lifesensor Personal Health Record which can store
the owner’s complete medical information in one
convenient and secure location (ICW eHealth
Framework, 2009). The patient as owner of the
record authorizes health team members or care
providers to access their record and assigns specific
read and write privileges (ICW eHealth Framework,
2009). ICW Java SDK is used for the integration of
Lifesensor PHR to our application.
Upon arrival to the ED of a hospital, an
individual is registered as an emergency patient and
the authorization propagation process is triggered in
order for the required authorizations to be
determined and granted to the medical staff treating
him. To this end, the local access control service is
invoked which, in conjunction with the local
Context Acquisition Agent (CAA), is accessing the
local database(s) in order to retrieve the list of the
medical staff being on duty at the time. The pieces
of information retrieved include starting and ending
time of each person’s shift. As soon as the
information is retrieved, it is communicated to the
global access control service which, in conjunction
with the Authorization Agent (AA), is determining
the corresponding access rights for each person on
the list according to a number of XACML policies.
The latter are already defined and stored on a server
at the DGH site. Finally, the deducted authorizations
for each member of the medical staff are granted to
him/her by means of the ICW SDK’s
HealthRecordManager which essentially represents
the access to a given personal health record.
After the authorizations have been granted, the
nurses and physicians of the ED authenticate
themselves in order to gain access to this patient’s
full medical record by using their credentials (X.509
certificate stored in his electronic Health Card -
eHC). Each access request is handled by the
corresponding local access control service which is
using CAA to acquire the context holding at the time
HEALTHINF 2010 - International Conference on Health Informatics
88

of the attempted access and forwards the request to
the global access control service which in
cooperation with the AA decides whether access
should be granted or denied to the requesting party.
If the requesting party has the required privileges a
connection to the corresponding PHR is established
and the corresponding part of the patient’s record is
provided to him/her.
After reviewing the patient’s medical record, the
ED physician forms the appropriate care plan for the
patient under treatment.
7 CONCLUDING REMARKS
Personal health records can address healthcare
information needs as they can provide each person
with a complete copy of his medical record. Thus,
PHRs constitute a valuable tool for supporting the
continuity of care and consequently the quality,
access and efficiency of health care delivery. As
PHR systems grow in popularity, it is important that
they be managed and maintained responsibly
without hindering accessibility to important
information in cases that it is mostly needed (e.g.
emergency cases). Hence, apart from the security
and privacy controls which are common to any
electronic health record system, in PHR systems a
suitable mechanism should be in place that will
automate the authorization propagation process
without the patients’ involvement. The prototype
system presented in this paper deals with this
security issue. In particular, a mechanism is
presented whereby the process of granting
(revoking) authorization to (from) healthcare
professionals on patients’ PHR is performed without
the patient’s involvement. To this end, context-
aware technology is used. Thus, both clinical and
administrative patient data are becoming
immediately available to people who need it via
accessible, secure and highly usable PHRs, fact that
constitutes an enabling factor of the patient-centred
shared care.
A number of issues related to the implementation
of systems like the one proposed in this paper
suggest directions for future work. The most
important concern the means used for patient
authentication as well as the way medical staff is
granted access to medical data in cases where patient
registration is performed after the patient has
received treatment, as is often the case in EDs.
REFERENCES
Koufi, V., Vassilacopoulos, G., 2008. HDGPortal: A Grid
Portal Application for Pervasive Access to Process-
Based Healthcare Systems, In PervasiveHealth’08,
2nd International Conference in Pervasive Computing
Technologies in Healthcare
Tang, P. C., Ash, J. S., Bates, D. W., Overhage, J. M.,
Sands, D. Z., 2006. Personal health records:
definitions, benefits, and strategies for overcoming
barriers to adoption. Journal of the American Medical
Informatics Association : JAMIA (2006) 13(2): 121-
126.
Wiljer, D., Urowitz, S., Apatu, E., DeLenardo, C.,
Eysenbach, G., Harth, T., Pai, H., Leonard, K. J.,
2008. Patient accessible electronic health records:
exploring recommendations for successful
implementation strategies. Journal of medical Internet
research, 10(4).
Lauer, G., 2009 Health Record Banks Gaining Traction in
Regional Projects,
http://www.ihealthbeat.org/features/2009/health-
record-banks-gaining-traction-in-regional-
projects.aspx
Yasnoff, W. A., 2008. Electronic Records are Key to
Health-care Reform, BusinessWeek.
Win, K. T., Susilo, W., Mu, Y., 2006. Personal Health
Record Systems and Their Security Protection, Journal
of Medical Systems (2006) 30: 309-315.
Comini, L., Mazzu, M., Scalvini, S., 2008. Security
aspects in electronic personal health record: data
access and preservation, Digital Prevention Europe,
Briefing Paper.
Røstad, L., Nytrø, Ø, 2008. Personalized Access Control
for a Personally Controlled Health Record, In
CSAW’08, 2nd ACM Workshop on Computer
Security Architectures
My Personal Health Record (MyPHR), http://myphr.ca/
National Institute of Standards and Technology (NIST),
2009. Role Based Access Control (RBAC) and Role
Based Security, http://csrc.nist.gov/groups/SNS/rbac/
Java Agent Development Framework,
http://jade.tilab.com/
Organization for the Advancement of Structured
Information Standards (OASIS), 2008. Core and
Hierarchical Role Based Access Control (RBAC)
Profile of XACML v2.0, http://docs.oasis-
open.org/xacml/2.0/access_control-xacml-2.0-rbac-
profile1-spec-os.pdf
Java Authentication and Authorization Service,
http://java.sun.com/javase/6/docs/technotes/guides/sec
urity/jaas/JAASRefGuide.html
ICW eHealth Framework, Lifesensor, 2009. http://idn.icw-
global.com/solutions/lifesensor/lifesensor.html
Wikipedia, 2009. Emergency Department,
http://en.wikipedia.org/wiki/Emergency_department
Metavante, In Case of Emergency Personal Health
Record, https://www.icephr.com/
AUTOMATING AUTHORIZATION PROPAGATION PROCESS IN PERSONAL HEALTH RECORDS
89
