
PATIENT JOURNEY OPTIMIZATION USING A MULTI-AGENT
APPROACH
Chung-ho Choi, William K. Cheung, Jiming Liu
Department of Computer Science, Hong Kong Baptist University, Hong Kong
Ian T. Cheung
Quality and Safety Division, Hospital Authority, Hong Kong
Keywords:
Multi-agent systems, Patient journey optimization, Scheduling algorithms, Health information systems.
Abstract:
With the increasing expectation from patients and the regulations enacted by the government, exploring ways
to shorten patient journey has caught increasing attention. Patient journey optimization typically involves
the coordination of treatment scheduling at multiple medical units. This decentralized nature of the problem
makes conventional centralized operation research methods hard to be applied and motivates the use of the
multi-agent approach. In this paper, we focus on cancer patient treatment. We model patients and medical
units as autonomous agents which interact locally via a bidding process and a coordination process for patient
journey optimization. With reference to a dataset containing more than five thousand cancer patient journeys,
the effectiveness of the proposed algorithm under different settings of implementation has been evaluated via
experimental simulations.
1 INTRODUCTION
Shortening the length of patient journey with unnec-
essary waiting time avoided is always an expectation
of patients. Also, it is one of the key performance in-
dicators for evaluating the effectiveness of healthcare
providers. In order to raise the standard for health-
care services, careful application of scheduling al-
gorithms is crucial (Vermeulen et al., 2006). While
conventional operations research methods have been
found effective for scheduling-related problems (Vis-
sers et al., 2005; Patrick and Puterman, 2008), most
of them take the centralized approach and are not de-
signed to be applied to decentralized situations (Ver-
meulen et al., 2006; Decker et al., 2000).
The multi-agent approach is characterized by em-
phasizing on local interaction and self-organization
of different entities being modeled. These proper-
ties make it especially suitable for tackling complex
tasks with a lot of stakeholders involved and the envi-
ronment is dynamic (Czap and Becker, 2003). Multi-
agent methods have found applications in a variety of
problem domains, such as airport resource schedul-
ing (Mao et al., 2007), load allocation in transporta-
tion logistics (Robu et al., 2008), supply chain man-
agement (Wang et al., 2008), etc. Recently, it has
also been applied to patient scheduling in (Paulussen
et al., 2003; Vermeulen et al., 2006) with some ini-
tial success demonstrated. And yet, there are lim-
itations. Paulussen et al. (Paulussen et al., 2003)
assumed that a health state can be accurately quan-
tified as utility measure for guiding the scheduling
process. Vermeulen et al. (Vermeulen et al., 2006)
assumed that temporal constraints between treatment
operations need not be considered during the schedul-
ing process.
The objective of this study is to explore the extent
to which patient journey can be improved by better
coordinating and mobilizing resources distributed at
different medical units. In particular, we formulate
the scheduling problem according to the cancer treat-
ment practice in Hong Kong. We propose the use of
a multi-agent approach in which autonomous agents
interact with each other to arrive an effective over-
all schedule with reduced waiting times. To evaluate
the effectiveness of the proposed approach, we have
carried out simulations with the proposed approach
given different settings of the environment. To initial-
ize the simulation environment, we made use of a pa-
tient identity anonymized data set collected by Hospi-
181
Choi C., K. Cheung W., Liu J. and T. Cheung I. (2010).
PATIENT JOURNEY OPTIMIZATION USING A MULTI-AGENT APPROACH.
In Proceedings of the Third International Conference on Health Informatics, pages 181-186
DOI: 10.5220/0002693901810186
Copyright
c
SciTePress

tal Authority in Hong Kong which contains 5819 can-
cer patient journeys with the admission period span-
ning over 6 months.
The rest of the paper is organized as follows. The
patient scheduling problem formulation is described
in Section 2. Sections 3 and 4 present the details of the
proposed agent-based scheduling algorithm. Section
5 presents some preliminary experimental results and
Section 6 concludes the paper.
2 PROBLEM FORMULATION
In this section, we first briefly describe the establish-
ment of the cancer clusters in Hong Kong. Then, we
formulate the patient scheduling problem for cancer
treatment as an optimization problem.
2.1 Cancer Patient Treatment - A Hong
Kong Scenario
In Hong Kong, there are seven cancer clusters estab-
lished and we denote them as C = {C
1
, C
2
, ..., C
7
}.
Currently, on-demand information exchange among
the clusters for patient scheduling is not yet exten-
sively used. That is why it is common for cancer pa-
tients to be scheduled to receivetreatments at only one
cancer cluster, even though some of the treatments
could be provided earlier by other clusters.
Generally speaking, once a patient is suspected to
have cancer, the doctor will specify the patient a treat-
ment plan which contains a sequence of treatment op-
erations. We denote the set of treatment operations as
Γ = {radiotherapy, surgery, chemotherapy}.
To carry out the treatment operations, medical re-
sources are needed. We denote the set of medical re-
sources (or units) as A = {radiotherapy unit, operation
unit, chemotherapy unit}. We assume that one treat-
ment operation can only be performed at one medical
unit of the corresponding type. A patient journey is
defined as the duration from the date of admission to
the date of the last treatment operation completed.
2.2 Formulation
Let K := A × C be the cartesian product of A and C
giving the complete set of medical units, M := K → Γ
be an one-to-one mapping between K and Γ specify-
ing the treatment type of the medical units, and P be
the set of cancer patients being scheduled.
Also, given a patient i, let N
i
Γ
denote the number of
treatment operations needed, D
i
0
denote the admission
date, D
i
j
denote the date of the j
th
treatment operation
where 1 ≤ j ≤ N
i
Γ
, V
i
j
∈ K be the unit at which the
j
th
treatment operation is performed, Tr
i
j
∈ Γ be the
type of treatment for the j
th
operation,C
k
be the daily
capacity (i.e. number of patients that could be treated)
of medical unit k ∈ K, T
t
be the duration (in days)
of treatment type t ∈ Γ, and Z be the set of dates on
which patient scheduling is being considered.
With the assumption that all the patients are be-
ing treated equally in terms of urgency, the scheduling
problem can be formulated as:
min
D
|P|
∑
i=1
N
i
Γ
−1
∑
j=1
(|D
i
j
− D
i
j+1
|) (1)
with the following constraints to be satisfied:
D
i
j+1
> D
i
j
+ T
Tr
i
j
(2)
∀d ∈ Z
{i : D
i
j
= d ∧V
i
j
= k∧ Tr
i
j
= M(k)}
≤ C
k
(3)
D
i
j
> D
i
0
> 0 (4)
The objective function in (1) is to minimize the
time lags between treatment operations for cancer pa-
tients. Constraint (2) ensures the temporal constraints
between treatment operations are not violated, con-
straint (3) is used to ensure all medical units are op-
erating within their capacities. Constraint (4) ensures
that patients would only be scheduled to receive treat-
ment operations after their admissions.
3 SCHEDULING FRAMEWORK
Theoretically, patient waiting times could be mini-
mized by optimizing (1). However, it is impractical
to do so as it is hard to assume that a cancer clus-
ter is willing to share its real-time resource allocation
related data (e.g., C
k
) with other clusters due to both
technical and managerial reasons.
Hence, in this section, we propose the use of a
multi-agent approach for our domain. Particularly,
in our proposed framework, there are two types of
agents, namely patient agents and resource agents.
3.1 Patient Agent
A patient agent is used to represent one cancer patient
and is denoted as P
i
with i = 1, 2, ..., |P|. It stores the
patient’s treatment plan. As it is common that some
treatment operations have to be performed in prior to
another, the set of treatment operations to be received
by a patient has to satisfy certain temporal constraints.
Hence, each patient agent P
i
maintains an ordered set
Tr
i
= {Tr
i
1
, Tr
i
2
, ...Tr
i
N
i
Γ
} as its treatment plan.
HEALTHINF 2010 - International Conference on Health Informatics
182
3.2 Resource Agent
A resource agent is used to manage a specific medical
unit. Here, we denote R
ab
as a resource agent rep-
resenting medical unit a ∈ A at cancer cluster b ∈ C .
Each resource agent has full access to the schedule of
the medical unit it represents, but not the others.
3.3 Scheduling Algorithm
We adopt a two-phase scheduling algorithm similar to
what being proposed in (Paulussen et al., 2003; Ver-
meulen et al., 2006). For each newly admitted patient,
a treatment plan is first designed and then the corre-
sponding treatment operations are initially scheduled
(initial assignment phase). Then, a timeslot-swapping
process is enforced for shortening the patient jour-
ney (rescheduling phase). Here we assume that any
two patient agents are willing to exchange their times-
lots as far as none of their schedules is worsen (as
suggested in (Vermeulen et al., 2006)) and none of
the temporal constraints as specified in Eq.(2) is vio-
lated.
1
4 AGENT COORDINATION
In this section, more details about the scheduling al-
gorithm are given, including 1) how the patient agents
interact with the resource agents, and 2) how some
“unnecessary” swappings can be rejected so as to fur-
ther improve the scheduling optimality.
4.1 A Bidding Process for Agent
Matchmaking
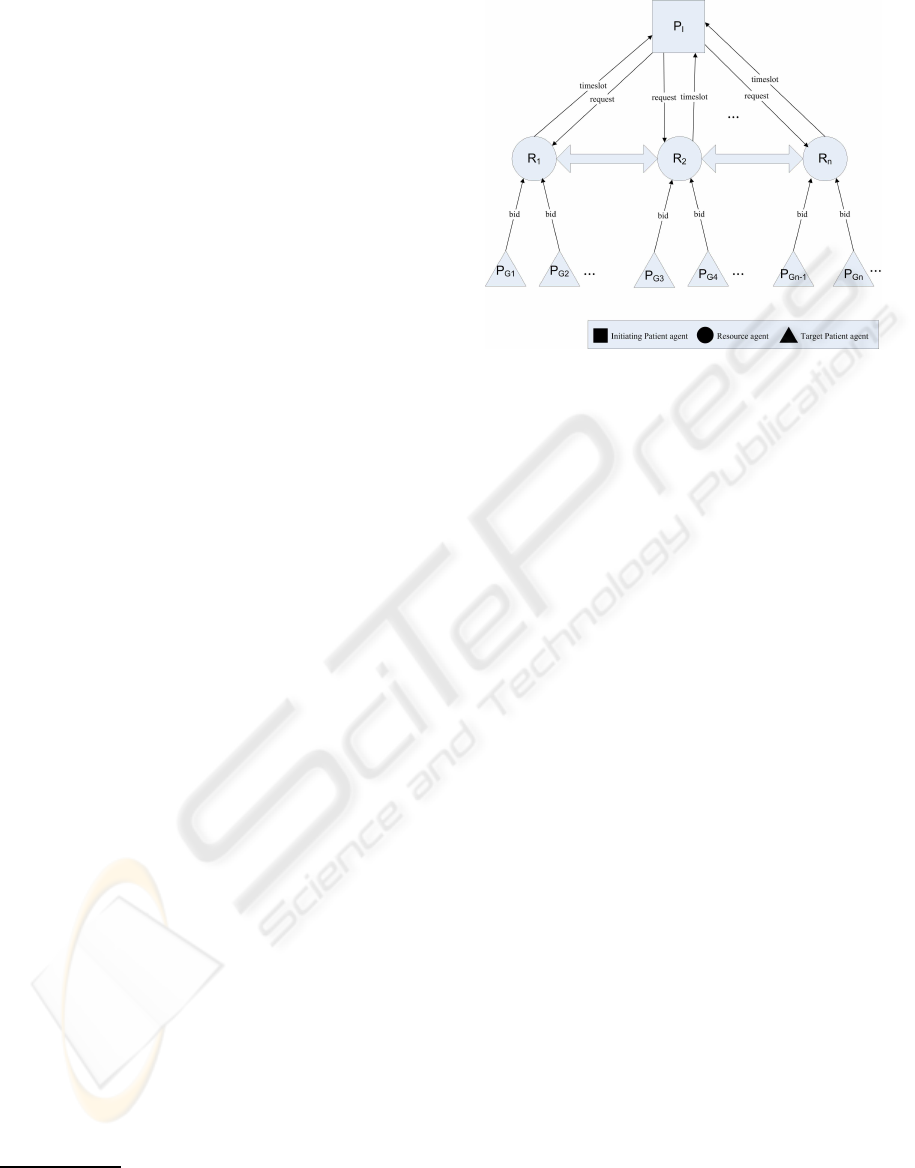
Figure 1 shows our proposed framework. As what
have been introduced earlier, there are two types of
agents, namely patient agents and resource agents.
In order to show clearly the coordination between
agents, we further categorize patient agents into ini-
tiating patient agents and target patient agents. Ini-
tiating patient agents P
I
are those patient agents who
initiate a request for timeslot exchange while target
patient agents P
G
are those who are willing to partic-
ipate in the exchanging process.
In order to shorten its patient journey, an initiat-
ing patient agent P
I
would first send out a request
for rescheduling to the corresponding resource agents
1
This assumption may imply that some policy-wise in-
centive has to be in place so that different medical units are
willing to share their resources in this manner, which how-
ever is not the main focus of our study.
Figure 1: The proposed agent coordination framework for
patient scheduling.
R
ab
. The request includes the earliest possible start
date (EPS) and the latest possible start date (LPS) of
its associated treatment operation. In order not to vi-
olate the temporal constraints between treatment op-
erations, the EPS can be defined as:
EPS
I
j
= D
I
j− 1
+ T
Tr
I
j−1
+ δ
1
. (5)
Note that δ
1
denotes how many days a patient should
be admitted (if needed) before a treatment operation
to be carried out. In our experiment, we set to be 1. In
practice, this value could be designated by healthcare
providers. With a similar argument, LPS is defined as:
LPS
I
j
= D
I
j
− 1. (6)
Once a resource agent receivesa request with EPS
and LPS, it will first check whether there are avail-
able timeslots released by deceased patients. If yes,
the released timeslot will be assigned to the initiat-
ing patient agent. If not, the resource agent will then
pass the request to those patient agents (target patient
agents, P
G
) which reserved resources of the same type
in the period from EPS to LPS. Those target patient
agents who have received the request will submit a
bid to the resource agent in response.
There are several factors needed to be considered
in computing the bid value.
• The target patient agent should not have its last
treatment operation to be exchanged; otherwise,
it would end up with a lengthened journey.
• As it is impractical to reschedule a patient’s treat-
ment operation without prior notification, we as-
sume that the exchange of timeslots would not
be considered if the patient will have less than a
PATIENT JOURNEY OPTIMIZATION USING A MULTI-AGENT APPROACH
183
week’s time of notification.
2
• The target patient agent has to ensure that the tem-
poral constraints between its treatment operations
would not be violated after the exchange.
Taking into account the above considerations, the
bid value submitted by P
G
is formulated as:
Bid
G
= (D
G
j
t
− EPS
I
j
i
) + Last + Noti+ Temp, (7)
where Last, Noti and Temp are three binary variables.
Last = 0 if the j
t
th operation is not the last one for P
G
,
or ∞ otherwise. Noti = 0 if a week’s time of notifica-
tion for the target patient agent to be notified, or ∞
otherwise. Temp = 0 if there are no temporal con-
straints violated, or ∞ otherwise.
Among all the target patient agents, the one with
the lowest bid value will be accepted and the timeslot
swapping between P
I
and P
G
will be confirmed. If
two bids are found to be numerically identical, the
resource agent will select one at random.
4.2 A Coordination Process for
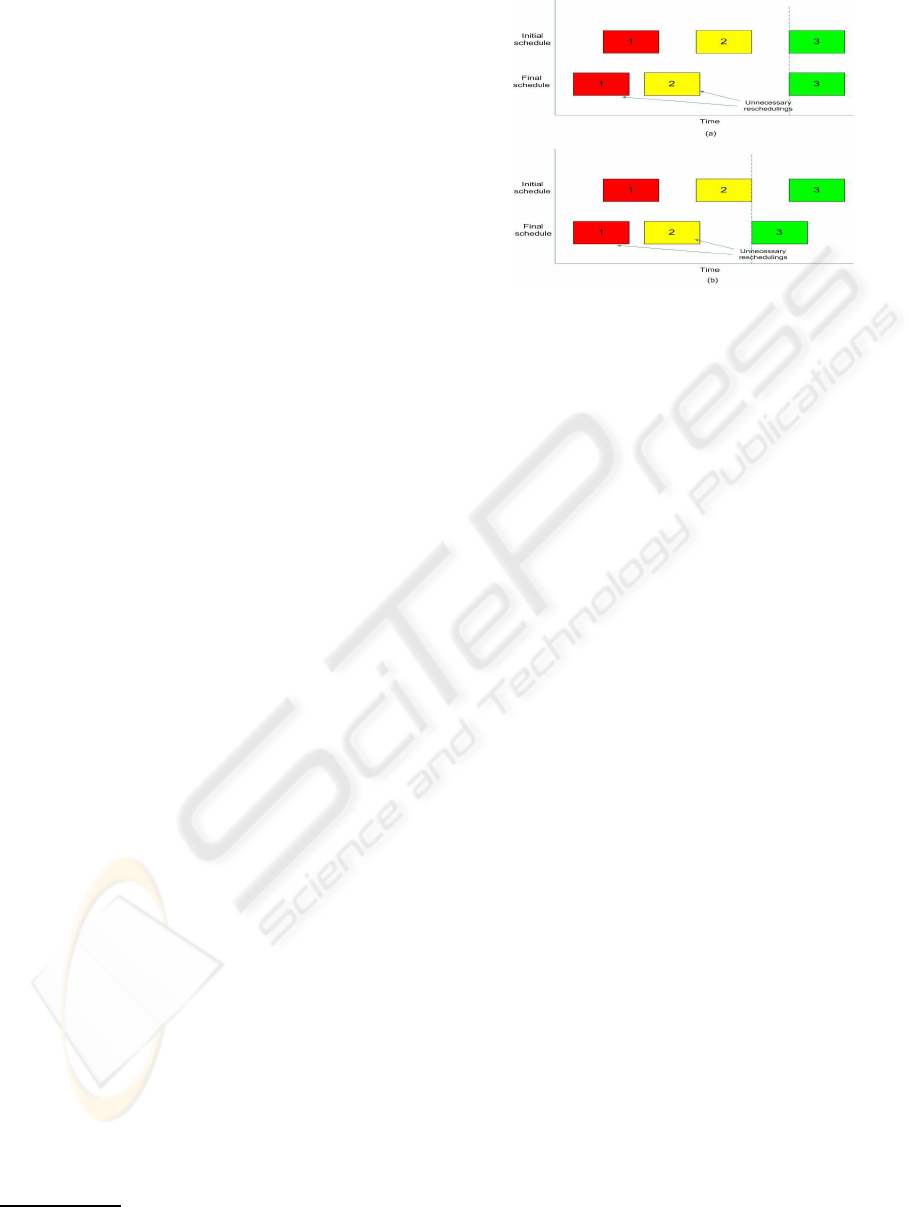
Rejecting Unnecessary Swappings
A timeslot swapping confirmed as described in the
previous section does not necessarily lead to a short-
ened patient journey. To illustrate that, suppose there
is a patient agent with 3 treatment operations to be
rescheduled. In case the last treatment operation
could not be rescheduled to be performed earlier, any
rescheduling of the first 2 are useless as the dura-
tion of the whole journey remains unchanged (see
Figure 2(a)). As another example, even a shortened
patient journey can be achieved, rescheduling of the
first 2 treatment operations could also be useless if the
rescheduling of the last one cannot be benefited from
the rescheduling of the first two (see Figure 2(b)).
In order to eliminate these useless swappings, a
resource agent after identifying the most optimal bid
among the target patient agents will not notify the
initiating patient agent immediately. Instead, it will
pass the bid to the resource agent which is responsi-
ble for the succeeding treatment operation of the ini-
tiating patient agent. Having received such a bid, the
resource agent could derive a new EPS, denoted as
(new)
EPS
I
j
i
+1
. Clearly, unnecessary swappings occur
if that resource agent could not find a bid such that
(new)
EPS
I
j
i
+1
≤ D
G
j
′
t
≤ EPS
I
j
i
+1
, where Tr
I
j
i
+1
= Tr
G
j
′
t
.
In that case, the resource agent will notify its an-
tecedent to discard the bid such that the corresponding
timeslots would not be exchanged.
2
In general, the time of notification can be adjusted ac-
cording to the real situation.
Figure 2: Unnecessary reschedulings.
5 EXPERIMENTAL VALIDATION
To evaluate the effectiveness of the proposed multi-
agent approach, we first obtained a dataset containing
5819 cancer patients who were treated at the 7 cancer
clusters in Hong Kong within an admission period of
6 months. The average length of the patient journey
among all cancer clusters is 90.7 days. Based on the
dataset, we had carried two groups of simulation.
For the first group of simulation, we made use
of the scheduled treatment plans in the dataset for
the initial assignment and studied to what extent the
multi-agent approach can improve the patient journey
as a whole.
For the second group of simulation, we aim to
make the simulation more flexible by making use of
only the statistics of the scheduled treatment plans
and the capacities of the medical units as revealed in
the dataset. The initial assignment strategy and the
reschedulingstrategy can both be specified by the user
for evaluation. Also, we tried to increase the capacity
value as revealed in the dataset by percentage so as to
see to what extent the patient journeycan be improved
with more resources injected.
5.1 Simulation with Initial Assignment
and Unit Capacity Fixed (Exp. A)
Four different settings had been used to demonstrate
various aspects of the proposed algorithm:
Setting 1: Patient agents are willing to exchange
timeslots with others whenever there is a Pareto
improvement.
Setting 2: It is assumed that only 20% of the pa-
tients of each cancer cluster are allowed to un-
dergo timeslot swapping.
HEALTHINF 2010 - International Conference on Health Informatics
184

Setting 3: It is assumed that only swappings between
two nearby cancer clusters are allowed.
Setting 4: Timeslots released by deceased patients
are allocated to the patient agents who have the
longest patient journeys at a time point.
Given the four aforementioned settings, Figure 3a
shows the average length of the patient journeys asso-
ciated with the seven cancer clusters in Hong Kong.
Figure 3: a) Average length of patient journey; b) Maximum
length of patient journey among the seven cancer clusters in
Hong Kong under 4 different settings in Exp. A.
The experimental results obtained show that, on
average, the average length of journey can be re-
duced by 9.8 days for those 5819 cancer patients if
no restriction is imposed on the exchange of times-
lots whenever there is a Pareto improvement (Setting
1). Given only 20% of patients per cancer cluster are
allowed for timeslot exchange (Setting 2), we found
that the average length of journey could still be re-
duced by an average of 6.1 days. With the geograph-
ical restriction on allowing only swappings between
nearby cancer clusters (Setting 3), the average length
of journey can also be reduced by 9.3 days.
However, it should also be noted that according to
Figure 3b, the maximum length of journey remains
unchanged. The reason is obvious as no one is will-
ing to swap with those with the longest length of jour-
ney. Reductions on the maximum length of journey
can only be observed for Setting 4 where the released
timeslots due to deceased patients are allocated to
those with the longest journey.
5.2 Simulation Revealing the Effects of
Varying Initial Assignment and Unit
Capacity (Exp. B)
Contrary to the group of simulation previously pre-
sented, we tried to simulate also the initial assign-
ment process using again the treatment plans of the
5819 cancer patients. However, all the treatment op-
erations were not scheduled according to the data but
simulated based on the statistics of the inter-operation
duration obtained from the dataset. In particular, dur-
ing the initial assignment phase, patient agents would
be assigned an initial schedule one by one based on
their admission orders. For each treatment operation,
each patient agent would be assigned with the next
earliest available timeslot. However, it is obvious that
there should be a minimum time lag between two sub-
sequent treatment operations due to different medical
reasons. We first used the average inter-operation du-
ration computed based on the dataset and then per-
formed the simulation. The average length of jour-
ney computed right after the initial assignment was
found to be 83.3 days. The improvements obtained
due to the different settings are not very much differ-
ent from those obtained in the previous section. Due
to the page limit, we would not show them here.
According to the dataset, the minimum days be-
tween any two treatment operations was found to be
one only. This implies that treatment operation some-
times could be started one day after another if the re-
source is available. We had also tried to set the mini-
mum days to one in our initial assignment phase and
compared with the results obtained before. According
to Figure 4, while we observed some improvements
in performance, the enhancement however is not very
significant. Hence, setting some reasonable time lags
between treatment operations does not have too big
an impact on lengthening the patient journey.
For all the results presented so far, it is assumed
that the capacity of each medical unit is fixed. To
study the cost-effectiveness of increasing the units’
capacities for patient journey optimization, we in-
creased the capacity by the same percentage for all
the medical units. According to Figure 5, it can be
observed that when all the resource capacities are in-
creased incrementally (10%, 20%, 30%), the reduc-
tion on average length of patient journey will then
drop accordingly. In fact, such drop could be at-
tributed to the fact that when the resource capaci-
ties are increased, patients would then be scheduled
with less idle times between treatment operations; and
hence with less chance to exchange timeslots with
others.
PATIENT JOURNEY OPTIMIZATION USING A MULTI-AGENT APPROACH
185
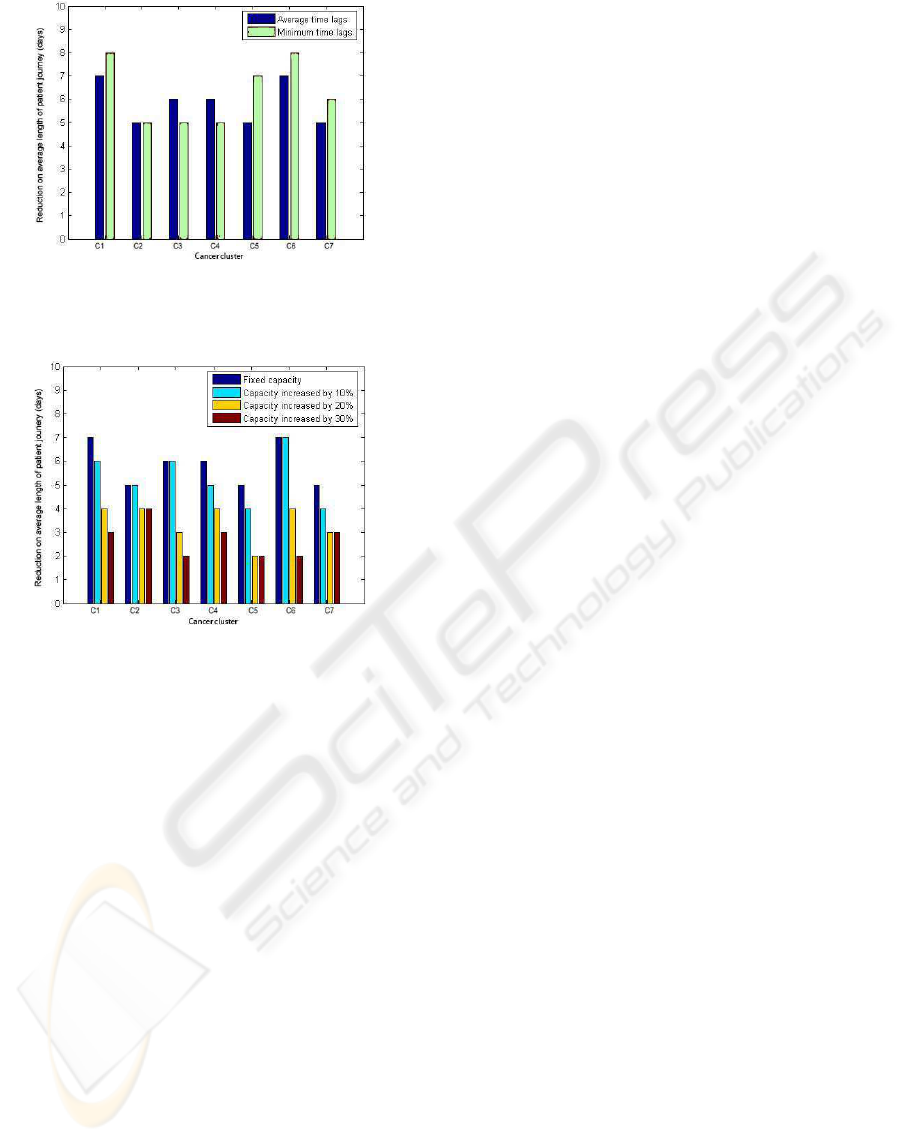
Figure 4: Reduction on average length of patient journey
(Setting 4) by varying the time lags between treatment op-
erations.
Figure 5: Reduction on average length of patient journey
(Setting 4) by varying capacities.
6 CONCLUSIONS
In this paper, a multi-agent approach was proposed
for patient journey optimization. Particularly, by ap-
plying the approach, the shortening of a patient jour-
ney will not lengthen the journeys of the others. Also,
all the temporal constraints among the treatment op-
erations for each patient would not be violated during
the scheduling process.
The effectiveness of the proposed approach has
been demonstrated by applying it to a dataset contain-
ing 5819 scheduled treatment plans of cancer patients
in Hong Kong. The effects of varying the initial as-
signment and the unit capacity on the overall reduc-
tion in length of patient journey are also studied.
Currently, since we are using a Pareto improve-
ment approach, it is assumed that no single patient
(agent) would get a lengthened schedule after swap-
ping timeslots with another. In the future, we are go-
ing to see whether there would be a greater improve-
ment in achieving a reduced average length of patient
journey when the above assumption for individuals is
relaxed.
ACKNOWLEDGEMENTS
This is to acknowledge Hospital Authority in Hong
Kong for providing the dataset to support this study.
REFERENCES
Czap, H. and Becker, M. (2003). Multi-agent systems
and microeconomic theory: A negotiation approach
to solve scheduling problems in high dynamic envi-
ronments. In HICSS ’03: Proceedings of the 36th An-
nual Hawaii International Conference on System Sci-
ences (HICSS’03) - Track 3, page 83.2, Washington,
DC, USA. IEEE Computer Society.
Decker, K., Li, J., and Demazeau, Y. (2000). Coordinating
mutually exclusive resources using gpgp. Autonomous
Agents and Multi-Agent Systems, 3:200–0.
Mao, X., Mors, A., Roos, N., and Witteveen, C. (2007).
Coordinating competitive agents in dynamic airport
resource scheduling. In MATES ’07: Proceedings
of the 5th German conference on Multiagent Sys-
tem Technologies, pages 133–144, Berlin, Heidelberg.
Springer-Verlag.
Patrick, J. and Puterman, M. (2008). Reducing wait times
through operations research: optimizing the use of
surge capacity. Healthc Q, 11(3):77–83.
Paulussen, T. O., Dept, I. S., Decker, K. S., Heinzl, A., and
Jennings, N. R. (2003). Distributed patient scheduling
in hospitals. In Coordination and Agent Technology
in Value Networks. GITO, pages 1224–1232. Morgan
Kaufmann.
Robu, V., Noot, H., La Poutr´e, H., and van Schijndel, W.-J.
(2008). An interactive platform for auction-based al-
location of loads in transportation logistics. In AAMAS
’08: Proceedings of the 7th international joint confer-
ence on Autonomous agents and multiagent systems,
pages 3–10, Richland, SC. International Foundation
for Autonomous Agents and Multiagent Systems.
Vermeulen, I., Bohte, S., Somefun, K., and La Poutre, H.
(2006). Improving patient activity schedules by multi-
agent pareto appointment exchanging. In CEC-EEE
’06: Proceedings of the The 8th IEEE International
Conference on E-Commerce Technology and The 3rd
IEEE International Conference on Enterprise Com-
puting, E-Commerce, and E-Services, page 9, Wash-
ington, DC, USA. IEEE Computer Society.
Vissers, J., Bekkers, J., and Adan, I. (2005). Patient mix op-
timization in tactical cardiothoracic surgery planning:
a case study. IMA Journal of Management Mathemat-
ics, 16.
Wang, M., Liu, J., Wang, H., Cheung, W. K., and Xie, X.
(2008). On-demand e-supply chain integration: A
multi-agent constraint-based approach. Expert Sys-
tems with Applications, 34(4):2683 – 2692.
HEALTHINF 2010 - International Conference on Health Informatics
186
