
USEFULNESS OF BRAIN SIGNALS FOR THE DETECTION OF
LOSS OF CONSCIOUSNESS IN ANESTHESIA
Overview of the Problem and Results from a Clinical Study
Carmen González
Instituto de Engenharia Mecânica, University of Porto, Rua Roberto Frias, Porto, Portugal
Marina Mendes, Pedro Amorim
Hospital Geral de Santo António, Porto, Portugal
Joaquim Mendes
Instituto de Engenharia Mecânica, University of Porto, Rua Roberto Frias, Porto, Portugal
Catarina S. Nunes
Division of Engineering, King’s College of London, Strand, London, United Kingdom
Keywords: General anesthesia, Loss of Consciousness detection, Bispectral index.
Abstract: Loss of consciousness (LOC) detection is essential for better anesthesia guidance. Clinical signs and brain
monitoring are currently used in operating rooms to assess the state of consciousness. However, a patient-
independent, accurate and reliable indicator of LOC is not currently available. We studied 69 patients
undergoing general anesthesia, investigating a possible relationship between loss of consciousness and BIS
and EMG signals registered during induction. Neither BIS and EMG values at LOC, nor their abrupt fall
proved to be good indicators of loss of consciousness. Further work needs to be done in order to reliably
detect loss of consciousness.
1 INTRODUCTION
Hypnosis, analgesia and muscular blockade are the
three components of general anesthesia. From all
three, hypnosis is the most important; it is a
pharmacologically induced sleep state, a reversible
state of unconsciousness (Bonhomme and Hans,
2004).
Loss of consciousness (LOC) detection has an
important role at induction of anesthesia. Identifying
the precise moment when it occurs will determine
the hypnotic dosage required for each individual
patient and provide important information to help
avoiding awareness episodes and overdoses.
Furthermore, detecting LOC is the first step in the
development of fully automated anesthesia delivery
systems based on the conscious state of the patients.
In this work, we investigated how the Bispectral
index (BIS), the most widely used anaesthesia
monitor of consciousness, reflects loss of
consciousness during induction of anesthesia. It has
been shown that BIS values at the moment of LOC
can vary widely (Tesniere et al., 2003). We
examined not only BIS values at LOC, but also the
abrupt fall that occurs in the BIS and
electromyography (EMG) signals during the
transition from the conscious state (awake) to
unconsciousness (“sleep”) at induction of anesthesia.
This paper is organized as follows: in section 2 a
short review of LOC detection methods is presented;
section 3 includes our clinical study and conclusions
are pointed out in section 4.
311
González C., Mendes M., Amorim P., Mendes J. and Nunes C. (2009).
USEFULNESS OF BRAIN SIGNALS FOR THE DETECTION OF LOSS OF CONSCIOUSNESS IN ANESTHESIA - Overview of the Problem and
Results from a Clinical Study.
In Proceedings of the International Conference on Bio-inspired Systems and Signal Processing, pages 311-315
DOI: 10.5220/0001546403110315
Copyright
c
SciTePress

2 SHORT REVIEW
Since the early days of anesthesia, several clinical
signs have been used for LOC assessment, such as
pupil diameter, sweat or tears production, heart rate
and muscular tone (Strickland and Drummond,
2001). Nowadays, in the clinical setting, LOC is
usually identified as the moment when the patient
looses the eyelash reflex or stops responding to
specific commands (proper name calling or tapping
in the forehead) or stimuli (pressing a button every
time they see a red light), which are very imprecise
and dependent on patient’s collaboration. These
methods have several disadvantages: assessment of
lack of response to name calling and mechanical
stimulus require the patient to be frequently
stimulated, so anesthesia induction cannot be smooth
and quiet; also any method based on a voluntary act
by the patient often fails because patients loose
critical judgement before losing consciousness.
In the last two decades, brain monitoring
techniques have been developed to assess the
hypnotic state of the patients. They were designed to
reflect real-time electrical activity of brain cells but
were not specifically created for LOC detection. In
clinical practice, they are used in combination with
clinical signs to provide as much information as
possible about the level of consciousness of the
patients.
Among all the developed indices, the Bispectral
Index (BIS) (Kelley, 2003) is the most well-known
and broadly used. It processes electrical activity
(electroencephalographic signal, EEG) detected in
the forehead by means of electrodes and shows a
value, from 0 to 100, which indicates the level of
hypnosis: 0 is associated to absence of electrical
activity and 100 corresponds to the awake state. The
BIS system uses a proprietary algorithm, based on
bispectral analysis, which performs amplification,
digitalisation and signal processing of EEG in order
to obtain the above mentioned index.
The BIS signal and the electromyopraphy of the
frontal muscle, produced spontaneously and also
acquired with the BIS unit, were the subject of a
clinical study presented in this paper, where their
relationship with the exact moment of LOC was also
analyzed.
3 CLINICAL STUDY
3.1 Patients and Methods
Adult patients scheduled for neurosurgical
procedures were studied during induction of general
anesthesia. Patients were monitored according to the
American Society of Anesthesiologists (ASA)
standards. BIS was also monitored in all patients. A
XP-Quattro sensor was applied to the forehead and
ASPECT A2000 or VISTA monitors were used. BIS
and EMG were recorded every 5 seconds using
Rugloop software. Anesthesia was induced with
Remifentanil (an opioid analgesic) and Propofol (an
hypnotic) administered intra-venously by Target
Controlled Infusion (TCI) using Rugloop software
and Asena pumps. During induction, LOC was
determined as the moment when patients failed to
open their eyes following name calling and a tap on
the forehead at every 15 seconds. The moment of
LOC was recorded for every patient.
BIS and EMG values collected during induction
were analyzed, as well as the moment of LOC. In
order to find another possible indicator of
consciousness on the BIS and EMG signals, the
moment when a significant fall in BIS and EMG
values occurred was assessed. Both signals were
processed using Matlab®. First, a moving average
filter of 11 samples was applied to the acquired
signals aiming to smooth them, and afterwards its
first derivative was analyzed. The minimum
derivative value corresponds to the abrupt fall
observed in the signals.
Once the falls were detected, we defined two
new variables: the difference of time between LOC
clinical detection and the moment when the falls in
BIS and EMG occurred (δ
BIS
and δ
EMG
respectively).
3.2 Results
We studied 69 patients of both genders; age was
51.5±14.7 years, height was 164.1±9.9 cm and
weight was 69.7±13.3 kg. The patients underwent
cranial or spinal surgeries.
BIS at LOC was 69,52±15,86 and EMG at LOC
was 42,04±7,60 dB (table 1). Typical tracings for
BIS and EMG trends during induction are shown in
figure 1.
BIOSIGNALS 2009 - International Conference on Bio-inspired Systems and Signal Processing
312
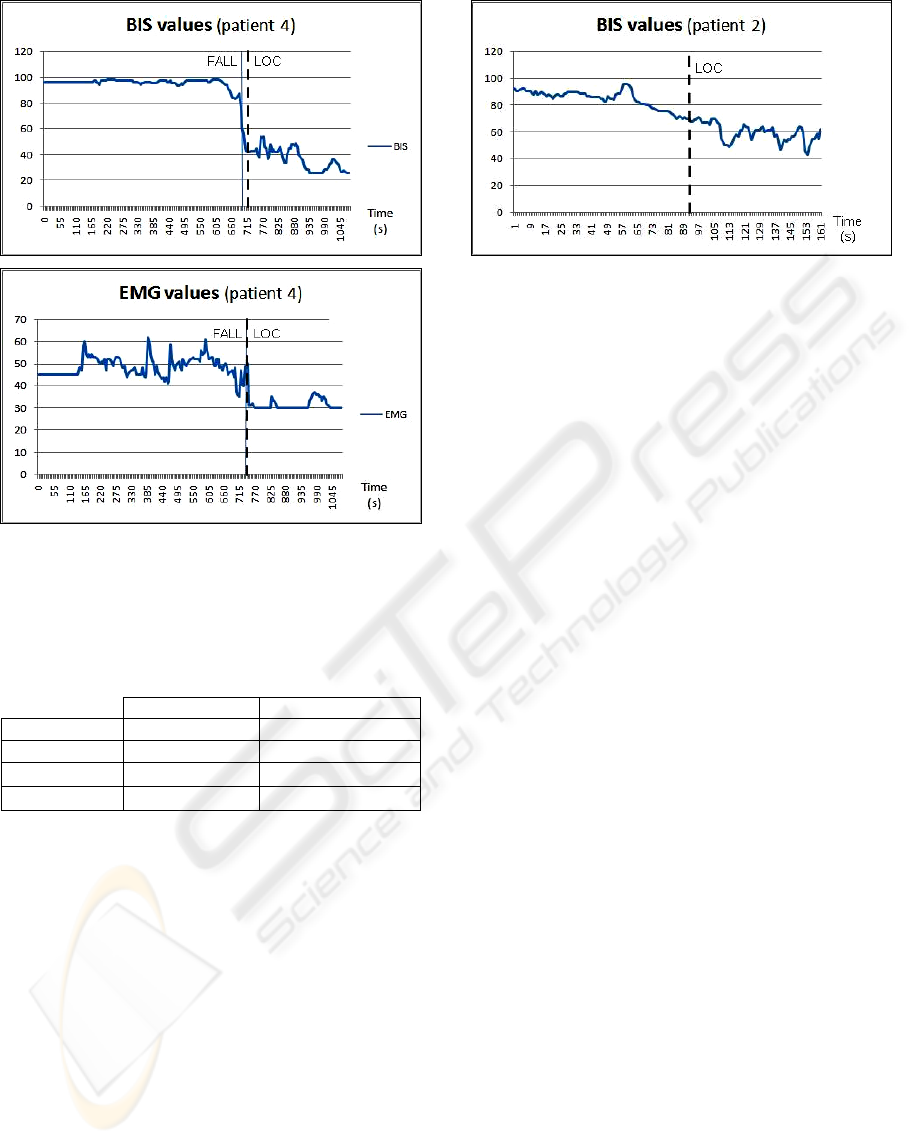
Figure 1: Example of BIS and EMG trends during
induction. The moment of LOC (dashed line) and of the
abrupt fall (straight line) are also indicated.
Table 1: Obtained values for EMG and BIS at LOC, and
for the difference of time between the moment of LOC
and the detected falls.
Mean Standard Deviation
BIS 69.52 15.86
EMG (dB) 42.04 7.60
δ
BIS
(s)
-0.79 34.45
δ
EMG
(s)
4.47 25.9
The difference of time between LOC clinical
detection and the moment when the falls occurred
was -0,79±34,45 seconds for BIS and 4,47±25,9
seconds for EMG (see table1). The fall detection
failed in 4 cases with BIS (5,7%) and 12 with EMG
(17,39%) because no abrupt fall clearly associated
with LOC existed in those cases (figure 2). The
statistical distribution of both variables is shown in
figure 3.
No significant correlation was found between
the new variables (δ
BIS
and δ
EMG
) and patient data,
such as age, sex, body mass index and the amount of
hypnotic administered until LOC. However, a
significant relationship was found between the
values of BIS at LOC and the difference of time
between LOC and BIS fall’s detection (figure 4).
Figure 2: BIS trend during induction and moment of LOC
in patient number 2: an abrupt fall in BIS cannot be clearly
identified.
Using a regression linear model, as shown in
figure 4, we confirmed the existence of a
relationship, with a P significance value lower than
10
-8
. No similar conclusion was obtained for EMG
signals and their abrupt fall.
3.3 Discussion
Some authors have previously reported BIS values at
the moment of LOC: BIS values in the transition
from consciousness to unconsciousness were: 78±14
(mean±standard deviation) (Tesniere, Billard, 2003);
82±10 (Kreuer et al., 2004) ; 73±18 (White et al.,
2006). Not only the BIS values at LOC were quite
different, but also a high standard deviation was
observed. Our results also show a high standard
deviation. This can be due to an existing inter-
subject variability or to a lack of ability of BIS to
reflect LOC. We investigated the possibility that
patients’ characteristics could influence BIS or EMG
performance to detect LOC, however, the fact none
of the demographic patient data showed significant
relationship with values at LOC suggests that BIS or
EMG do not perform well in this setting. Therefore,
it seems that there is not a BIS or EMG value
associated to loss of consciousness.
The values obtained for the difference of time
between the moment of LOC and the abrupt fall in
BIS and EMG signals also show a very high
standard deviation. Again, this can be due to inter-
subject variability. Furthermore, precise fall
detection in EMG signals failed in 17,39% of the
cases. Our finding that high values of BIS at LOC
correspond to negative δ values ( LOC detection
occurs before the abrupt fall) and low values are
associated to positive δ values (LOC detection
occurs after the abrupt fall), although interesting, has
no clinical application for the real time detection of
LOC using data derived from the BIS signal.
USEFULNESS OF BRAIN SIGNALS FOR THE DETECTION OF LOSS OF CONSCIOUSNESS IN ANESTHESIA -
Overview of the Problem and Results from a Clinical Study
313
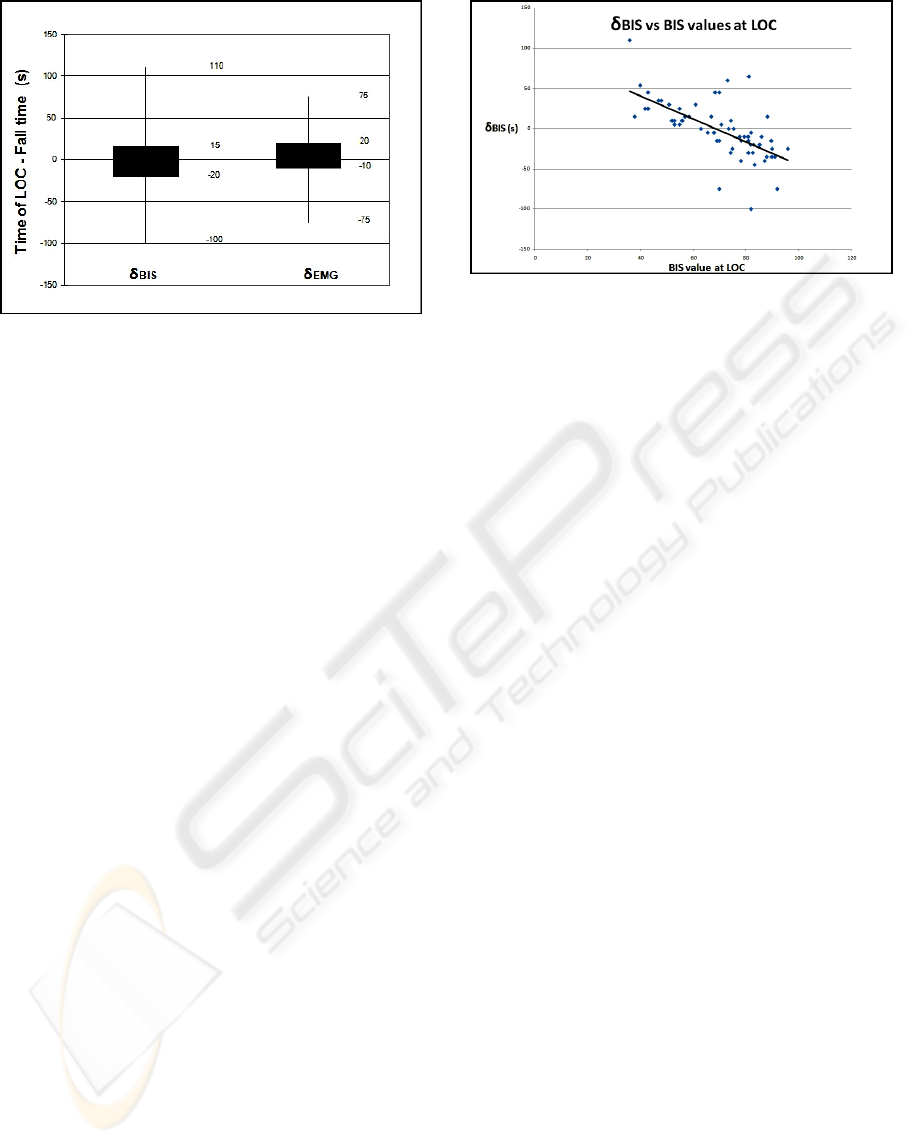
Figure 3: Boxplot of the difference of time between LOC
and the BIS fall, and LOC and the EMG fall. For each
variable, values for maximum, third quartile, first quartile
and minimum are shown.
4 CONCLUSIONS
The BIS index provides useful information about
hypnotic state, but not about LOC detection;
transition from consciousness to unconsciousness
cannot be identified by the index value. We can
detect the moment when an abrupt fall in BIS (and
EMG) in most patients occurs, but it is usually
different from the moment of LOC. Our results
suggest that neither BIS nor EMG derivatives can be
used to determine the moment of LOC with
precision. Clinical signs are not ideal for LOC
detection. Clinical assessment of LOC is not
accurate, consistent or precise: different criteria turn
up into different LOC detections, and clinical signs
are not continuously checked.
We can conclude from this study that BIS index
does not reflect LOC: the index value does not have
any direct relation with the transition from
consciousness to unconsciousness, and the BIS fall
can only be identified using future values, so it is not
a useful tool in real-time scenarios and has no
clinical use to guide anesthesia induction.
No existing technique can detect the moment of
LOC with precision and without interfering with a
smooth induction or independently of patient’s
cooperation. We can approximately know when
LOC occurs, but small errors in its identification can
turn into over or under doses that can have
deleterious effects for patients undergoing general
anesthesia.
Figure 4: Linear regression model for the difference of the
time between LOC and BIS fall and BIS values at LOC
(significance P < 10
-8
).
More precision in LOC detection is also an
important step for automated anesthesia delivery
systems. The closed-loop systems developed until
now are controlled by the index value (e.g. BIS), and
the majority of them can only be used during
anesthesia maintenance (Liu et al., 2007). A proper
LOC detection would allow the development of
closed-loop systems able to deal with inter-subject
variability and to be used also during induction.
Further work should be done in this area in
order to find a reliable, objective and rigorous
method of LOC detection for both improving patient
safety and new automated anesthesia delivery
systems.
ACKNOWLEDGEMENTS
This work was supported by Fundação para a
Ciência e Tecnologia (FCT), as being part of the
project PTDC/EEA-ACR/75454/2006.
REFERENCES
Bonhomme, V. and Hans, P., Monitoring depth of
anaesthesia: is it worth the effort? European Journal
of Anaesthesiology, 2004. 21(6): p. 423-8.
Tesniere, A., Billard, V., Hartl, D., and Bourgain, J.-L.,
BIS™ and Spectral Entropy™ To Predict Loss of
Consciousness during Induction and Recovery from
Anesthesia with Propofol and Remifentanil. American
Society of Anesthesiologists, 2003. A329.
Strickland, T.L. and Drummond, G.B., Comparison of
pattern breathing with other measures of induction of
anaesthesia, using propofol, methohexital and
sevoflurane British Journal of Anaesthesia, 2001.
86(5): p. 639-44.
BIOSIGNALS 2009 - International Conference on Bio-inspired Systems and Signal Processing
314

Kelley, S.D., Monitoring level of consciousness during
anesthesia and sedation. A clinician's guide to the
Bispectral Index. Norwood (MA) 2003, Aspect
Medical Systems.
Kreuer, S., Bruhn, J., Larsen, R., Bialas, P., and Wilhelm,
W., Comparability of Narcotrend index and bispectral
index during propofol anaesthesia. British Journal of
Anaesthesia, 2004. 93(2): p. 235-40.
White, P.F., Tang, J., Romero, G.F., Wender, R.H.,
Naruse, R., Sloninsky, A., and Kariger, R., A
comparison of state and response entropy versus
bispectral index values during the perioperative
period. Anesthesia & Analgesia, 2006. 102(1): p. 160-
7.
Liu, N., Chazot, T., Trillat, B., Dumont, G.A., and
Fischler, M., Titration automatisee du propofol guidee
par l'index bispectral. Annales Francaises
d'Anesthesie et de Reanimation, 2007. 26(10): p. 850-
4.
USEFULNESS OF BRAIN SIGNALS FOR THE DETECTION OF LOSS OF CONSCIOUSNESS IN ANESTHESIA -
Overview of the Problem and Results from a Clinical Study
315
