
A NEW MODEL FOR SUCCESSFUL CPOE DEPLOYMENT AND
IMPLEMENTATION IN HOSPITALS
Majid M. Altuwaijri
College of Public Health and Health Informatics
King Saud bin Abdulaziz University for Health Sciences (KSAU-HS), Saudi Arabia
Keywords: CPOE, CSF, CPR, PMO, and Knowledge barriers.
Abstract: In spite of the importance of information technology (IT) for many health organizations to help manage the
enterprise daily transaction, IT project failure rates still remain high. This suggests continued exploration of
new process model and organization structure to nurture strong project performance. In this paper we
propose a new model for successful implementation of IT projects. The proposed model calls for the
establishment of a program management office (PMO) to implement corporate strategy for project
management and to transform the organization into a learning one. The model is explained in details using
an example of a Computerized Physician Order Entry (CPOE) implementation.
1 INTRODUCTION
Between 50,000 to 100,000 Americans die each year
due to medical errors and about 1 million people are
injured (IMO, 1999). In response to these chocking
numbers reported by the Institute of Medicine
(IOM), some healthcare organizations embarked on
computerized physicians order entry (CPOE)
systems.
Health care organization leaders are becoming
well aware of the potential value of advanced
clinical information systems such as Electronic
Medical record (EMR) or computerized patient
record (CPR) to improve outcomes, reduce
medication errors, increase health care efficiency,
and eliminate unnecessary costs. Many health
organizations have invested significantly to plan,
procure, and implement these advanced systems,
including the current focus on computerized
physician order entry (CPOE) (Haux, 2006).
However, despite their knowledge, investments, and
best intentions, most healthcare organizations have
not realized a return on their investments (Berger,
2004). One probable reason for this problem is that
the key users – physicians and other clinicians – are
not using the technology to its greatest potential or,
in too many cases, have not begun to use the
technology at all. CPOE represents a monumental
step forward for healthcare organizations because it
embodies a shift from traditional, paper-based care
coordination activities to automation of the order
entry processes. This shift can be an agent for
change, eliminating confusing or illegible hand-
written order documentation, minimizing
transcription errors and fundamentally reducing
clinical mistakes (Snyder, 2006).
In this paper, a new model for successful
implementation of CPOE project in hospitals. The
model consists of three main components; the first
component is concerned with the stages taken by
organization to deploy new technology innovations
which is in turned composed of four stages:
visioning, matching vision, deployment, and
evaluation and improvement. The second component
deals with the main knowledge barriers to IT
innovation diffusion as suggested by literatures. The
third component is concerned with the critical
success factors of IT innovation implementation as
suggested by various literatures.
2 CPOE SYSTEM OVERVIEW
CPOE is a process of electronic entry of physician's
orders and instructions for the treatment of patients.
These orders are communicated over a CPR to the
179
M. Altuwaijri M. (2008).
A NEW MODEL FOR SUCCESSFUL CPOE DEPLOYMENT AND IMPLEMENTATION IN HOSPITALS.
In Proceedings of the First International Conference on Health Informatics, pages 179-185
Copyright
c
SciTePress
medical staff (nurses, therapists or other physicians)
or to the departments (pharmacy, laboratory or
radiology) responsible for fulfilling/documenting the
order.
CPOE is not a technology, rather it is a workflow
design (or redesign) of clinical processes that
integrates technology to optimize physician ordering
of medications, laboratory tests, etc. (AHRQ, 2001).
CPOE uses clinical decision support systems and
links to hospital systems to generate prompts and
alerts during the ordering session to notify of
potential errors such as contra-indicated medications
or routes or duplicate orders. Integration with other
hospital information technology systems including
electronic patient records, pharmacy, laboratory, and
other services provides the physicians with all
information necessary to develop and transmit an
effective, error-free order (Metzger, 2003).
In May 2001, thirteen CPOE experts from around
the world gathered at a 2-day conference for the
purpose of developing recommendations for CPOE
implementation (Ash, 2003). A list of high-level
considerations was generated to benefit
organizations thinking about implementing CPOE as
follows:
Motivation for Implementing POE
Vision/Leadership/People
Costs
Integration/Workflow/Health Care Processes
Value to Users/Decision Support Systems
Technical Considerations
Management of Project
Training/Support/Help at the Elbow
Learning/Evaluation/Improvement
3 PROJECT MANAGEMENT
OFFICE
In this context, we adopt the PMO's definition
proposed by PMI (PMI, 2004): "An organizational
body or entity assigned various responsibilities
related to the centralized and coordinated
management of those projects under its domain. The
responsibilities of the PMO can range from
providing project management support functions to
actually being responsible for the direct management
of a project". A PMO focuses on the activities with
relation to projects including training, process
standardization, consulting, identifying of best
practices, project prioritization, and reviewing
project progress (Bolles, 2004).
4 INFORMATION SYSTEMS
SUCCESS
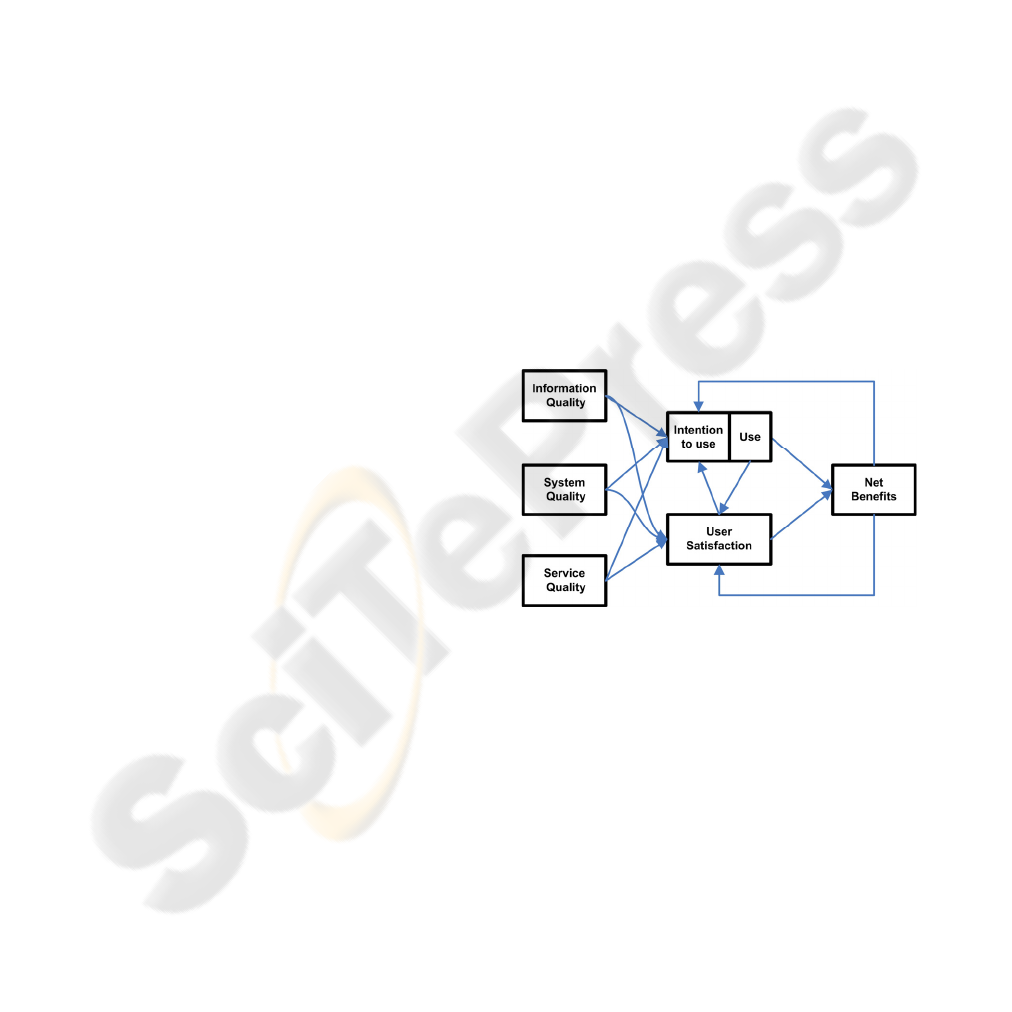
DeLone and McLean in 1992 conducted a
comprehensive review of IS success literature and
proposed a model of IS success (Delone, 1992). It
suggested that the success can be represented by the
system quality, the output information quality,
consumption (use) of the output, the user’s response
(user satisfaction), the effect of the IS on the
behavior of the user (individual impact), and the
effect of the IS on organizational performance
(organizational impact). An updated model was
proposed in 2003 (Delone, 2003) as shown in figure
1. The primary differences between the original and
updated models included:
The addition of Service quality category to
reflect the importance of service and support
in successful e-commerce systems,
The addition of "intention to use" to measure
user attitude, and
The merging of individual impact and
organization impact into one category
concerned with net benefits.
5 KNOWLEDGE BARRIERS
Various study researches highlighted several barriers
to innovation (Attewell, 1992; Tanriverdi, 1999;
Nambisan, 1999). The adoption and implementation
of complex IT solution is influenced by the
organization's ability to lower or remove the various
knowledge barriers. Knowledge barriers associated
with the adoption of larger-scale IT solutions can be
categorized into four categories: project/economic
barrier, technical barriers, organization barriers, and
behaviour barriers (Pare, 2007).
Figure 1: Updated Delone & McLean model of IS success.
HEALTHINF 2008 - International Conference on Health Informatics
180

Project/Economic barriers: This category is
concerned with the financing and project
management issues faced when acquiring
innovation.
Technological barriers: This category is
concerned with the lack of knowledge
required to carry out technical tasks needed to
adopt new innovations.
Organizational barriers: This category is
concerned with the difficulties of deploying a
new technology into existing practices and
processes.
Behaviour barriers: This group is concerned
with the resistance to change among
individuals affected by the implementation. It
is also concerned with organizational power
dynamics.
6 THE PROPOSED MODEL
Figure 2 shows a new model for successful
implementation. The model consists of three main
components; the first component is concerned with
the stages taken by organization to deploy new
technology innovations which is in turned composed
of four stages: visioning, matching vision,
deployment, and evaluation and improvement. In
visioning phase, institutions define the corporate
mission, objectives, and strategy. This phase is
mainly concerned with identifying and prioritizing
the organizational problems and opportunities that
form the basis of the need to acquire innovations
(Rogers, 1995). The second phase is concerned with
the fit between a need identified in the first phase
and the innovation proposed. In this stage we should
determine whether the innovation will truly solve (or
at least solve) one of the problems identified in the
first phase. At the end of this phase, the
organization decides weather or not to approve the
innovation project.
In the event that the project is approved, the third
phase of the process, deployment, begins. This phase
includes all decisions and actions related to the
deployment of the innovation. It includes also the
assimilation and the integration of the innovation
within the organization. At the end of this phase, the
IT innovation solution is deployed within the
organization. Evaluating performance is an
important step for ensuring the quality of the
innovation deployment. This phase emphasizes
process flow optimization and continuous expansion
of the system to gain competitive advantage.
The second component deals with the main
knowledge barriers to IT innovation diffusion. The
third component is concerned with the critical
success factors of IT innovation deployment as
suggested by various literatures (Ash, 2003).
After the successful deployment of innovation,
the list of benefits and lessons learned feeds a
knowledge base which in turn feeds all three
components described in the model. Knowledge
sharing behaviours facilitate learning among Project
team members and enable them to resolve problems
similar to situations encountered by others in the
past, thus enabling more successful projects.
The proposed model calls for the establishment of
a program management office to implement
corporate strategy for project management. The
main goal of this office is to translate the
organization's strategic plan into projects and
programs. The PMO is accountable for enterprise-
wide distribution of project management best
practices. Therefore, for the model to work properly,
Organizations should invest in project management
training for the staff working in the PMO.
The main advantages of this model is the strategic
alignment of projects which bears on the synergy
created by the management of relations between
projects, and the ability to develop a better
understanding of the challenges faced in carrying out
information systems projects, the factors for success,
and the strategies required to take advantage of IT.
The acts of sharing are very important since a
project's knowledge will not have much impact on
the organization unless it is made available to other
projects. Such learning organizations would be
aware of the repeated knowledge barriers to
innovation adoption and a well defined plan to
address these barriers would be developed.
Moreover, the knowledge base will help these
organizations refine their strategies and prioritized
plans. This allows for focusing on preparation for
future projects which is rarely covered in literature.
7 APPLYING THE MODEL FOR
CPOE DEPLOYMEENT
Figure 3 shows the detailed model for CPOE
implementation as explained in the following
sections:
7.1 Visioning
Institutions should align the strategic vision process
with the budgeting process to produce a realistic
prioritized strategic plan. The strategic plan will be
used as an input to the IT strategic plan in order to
ensure that the IT plan is closely integrated with the
A NEW MODEL FOR SUCCESSFUL CPOE DEPLOYMENT AND IMPLEMENTATION IN HOSPITALS
181
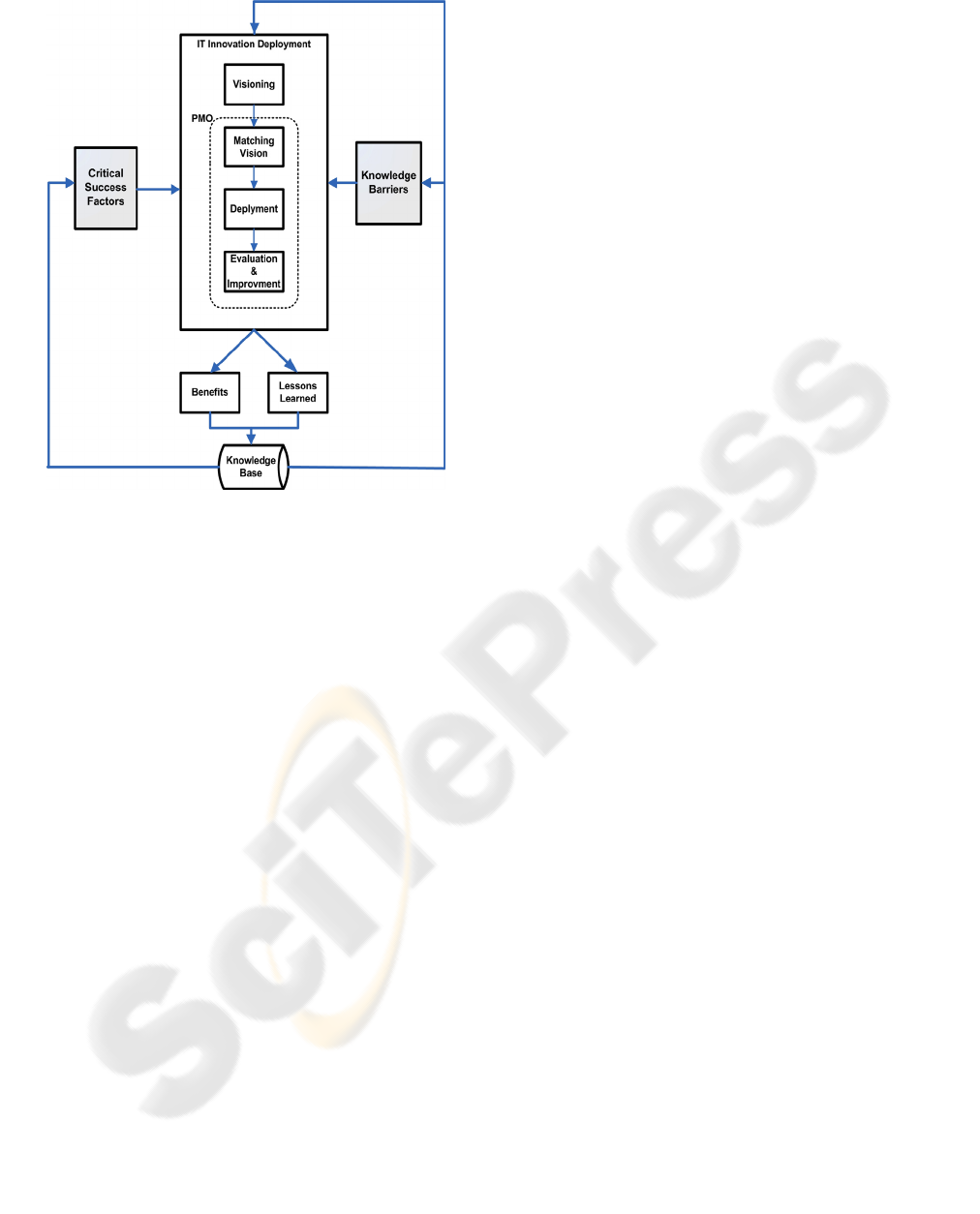
Figure 2: The proposed model for IT diffusion.
organization's strategic initiatives and business
directions and provides the opportunity to use IT as
a tool to enable systems integration as well as
deliver information as a strategic resource. The
visioning phase should address the Economic
barrier. Moreover, there are some strategic CSFs
related to this phase such as top management
support, business plan and vision, and cost/benefit
analysis.
7.1.1 Addressing the Economic/ Project
Barrier
Organizations deploying CPOE solutions should
address the financing issues faced when acquiring
the solution. These barriers include barriers
associated with project management skills.
Moreover, multi-site implementation of CPOE
presents special concerns. Firstly, each site had its
own processes which may not be consistent with
other sites. Secondly, multi-site organizations need
to choose whether the implementation is done
simultaneously in all facilities or in one facility at a
time.
7.1.2 CSFs for the Visioning Phase
Motivation for Implementation: The IT
strategic plan along with the organization's
strategies should provide a clear
communicated business plan and vision to
steer the direction of the CPOE project and
other IT projects. This factor influences the
funding, the political support, and the clinical
leadership.
CPOE Vision, Leadership, and Personnel:
Successful deployment of IT innovation
requires strong leadership, commitment, and
continuous support by top management. A
shared vision about the CPOE project should
exist throughout the organization.
Cost/Benefit Analysis: This analysis is
instrumental for organizations in order to
secure fund. This analysis would act as the
basis for defining the success criteria for the
CPOE project.
7.2 Matching the Vision
The PMO office plays an important role in matching
the fit between projects, proposed by departments,
and the organization vision and strategies. In this
phase the organization should decide if the projects
proposed match the vision or not. In case there is a
match, a decision is made to invest on the proposed
solution. If there is no match, the PMO office should
update the organizational knowledge base and
record the reasons. In some cases, the project
proposals need further research before a decision is
made. This phase is affected by the same barrier and
CSFs as in the previous phase.
7.3 CPOE Deployment
7.3.1 CPOE Package Selection
Organization should make an extensive review of
available CPOE Systems to select the package that
has the best match of the organization's vision and
strategies. The decision should be based on several
factors including price, supplier support, ease of
implementation, closeness to fit to organization’s
business, technological risks, and local experience.
7.3.2 CPOE Project Life Cycle (PLC)
Organizations implementing CPOE systems usually
modify business processes (as reasonably required)
to conform to “best practices” discovered during the
implementation of the CPOE project. These
opportunities for process improvements would be
identified during Business Process and Fit/Gap
Analysis workshops, consulting visits and by the
project team members as they become familiar and
comfortable with the software. Process change
HEALTHINF 2008 - International Conference on Health Informatics
182

proposals would be considered and approved by the
project management, steering and policy committees
as part of the governance of the project. This phase
is concluded when the CPOE solution is deployed
and is running within the organization.
7.3.3 Addressing Knowledge Barriers
Technical barriers: These include the technical
infrastructure readiness. Organizations might
need to upgrade their network infrastructure,
upgrade the data centre’s servers, and recruit
technical and functional analysts to support
the project. Data migration from legacy IT
systems to the new CPOE is an essential task
in this project. Finally, a maintenance contract
is required to ensure the availability of the
CPOE solution.
Organizational barriers: These include change
management processes to align the CPOE
with existing practices and processes.
Behaviour barriers: These include end-users
resistance to new innovations. Organizations
should conduct a lot of training sessions to
introduce the new innovation.
7.3.4 Critical Success Factors
Integration: Organization should have a clear
plan for integrating the CPOE into existing
environments and workflows. This factor is
also concerned with integrating the CPOE into
other hospital applications and possible legacy
systems.
Value to Users: Organizations should have a
clear change management strategy which
includes analysis of the current business
processes to identify the areas for
improvement. Physicians must be shown
CPOE benefits including the embedded
decision support logic that helps to improve
the quality of patient care.
Project management: Organizations should
appoint a dedicated full-time project manager.
The management of the project covers the
technical and functional aspects. A qualified
project manager manages five main functions;
managing scope, managing project team,
managing quality, managing cost, and
managing time.
Technology: Organizations should make sure
they have a good technical infrastructure
before “Go-Live”. The project team should
make a balance between customization and
standardization; where physicians of the same
specialty would have a common CPOE screen
which might be different than screens for
different specialties. Organizations should also
have a comprehensive system testing plan to
test the functionality of each module alone and
in conjunction with other modules.
Training and support: Organizations should
have a comprehensive training plan which
includes functional and technical aspects of
the project. In large organizations, "train the
trainer" approach is usually considered.
Additionally, Organizations should consider
proper support plan including 24*7 support
for at least several days post go-live.
7.4 Evaluation and Improvement
Finally, evaluation and improvement phase come
into action after the CPOE system is already
deployed within an organization. It is important that
organizations define the success criteria of the
CPOE project and use it to monitor the project.
CPOE system should be monitored forever and
should receive continuous improvement.
Organizations usually assume that their operational
performance will be improved immediately after the
"go-live". Instead, due to the complexity of CPOE
systems, organizations should expect an initial
decline in their performance. Once the system is
stable and users are more aware of its capabilities,
improvements will take place.
8 CPOE BENEFITS, LESSONS
LEARNED
After the CPOE system is already deployed, the
PMO should measure the benefits realized by the
project and tie them to the organizational strategic
goals. It is also important that the PMO assembles a
list of lessons learned from this project. The list of
project benefits and lessons learned are then fed into
the organization knowledge base. The knowledge
base will provide projects information back to the
organization visioning process and will be used to
refine the list of CSFs and knowledge barriers for
future projects. The feed back loop will transform
the organization to becoming a learning one.
A NEW MODEL FOR SUCCESSFUL CPOE DEPLOYMENT AND IMPLEMENTATION IN HOSPITALS
183
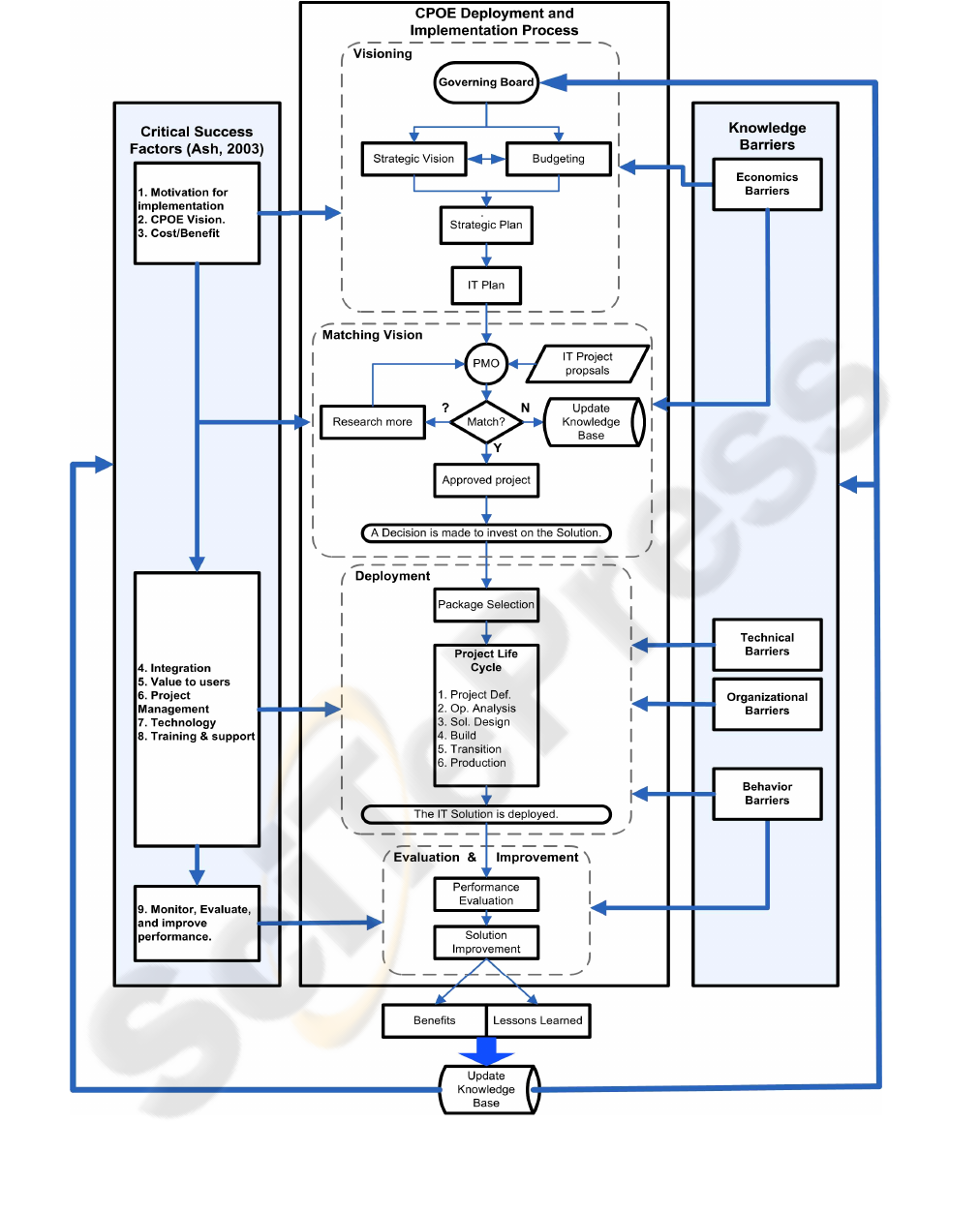
Figure 3: The proposed model for CPOE deployment and implementation in hospitals.
HEALTHINF 2008 - International Conference on Health Informatics
184

9 CONCLUSIONS
Enterprise-wide daily transactions are difficult to
manage due to their complexity and scope in terms
of rendering services to their clients. As a result,
many organizations employ Information Technology
(IT) to manage their enterprise-wide transactions
and to ensure quality of services. IT, when properly
selected and implemented, helps organizations
increase their efficiency and capabilities which
improves the organization’s competitive advantages.
In spite of the importance of information technology
(IT), IT project failure rates still remain high. This
suggests continued exploration of new process
model and organization structure to nurture strong
project performance.
In this paper we propose a new model for
successful implementation of IT projects. The model
consists of three main components; the first
component is concerned with the stages taken by
organization to deploy new technology innovations
which is in turned composed of four stages:
visioning, matching vision, deployment, and
evaluation and improvement. The second component
deals with the main knowledge barriers to IT
innovation diffusion as suggested by literatures. The
third component is concerned with the critical
success factors of IT innovation implementation as
suggested by various literatures. The proposed
model calls for the establishment of a program
management office to implement corporate strategy
for project management and to transform the
organization into a learning one. The model is
explained in details thru an example of CPOE
implementation.
The acts of sharing are very important since a
project's knowledge will not have much impact on
the organization unless it is made available to other
projects. Although knowledge exists at different
levels of an organization, for instance, at the individ-
ual, team, and organization levels, sharing of
knowledge at the individual level is critical to an
organization.
It is expected as organizations use this model for
several projects; more knowledge would be gained
and used towards more successful project in the
future. Critical success factors would be refined
more and be closely tied with organization culture.
Such learning organizations would be aware of the
repeated knowledge barriers to innovation adoption
and a well defined plan to address these barriers
would be developed. Moreover, the knowledge base
will help these organizations refine their strategies
and prioritized plans.
REFERENCES
Institute of Medicine (1999). To Err is Human: Building a
Safer Health System. National Academy Press,
Washington, DC.
Haux, R. (2006). Health Information systems-past,
present, future. Int. J. of Med. Info., 75, 268-281.
Berger, R. G. & Kichak, J. P. (2004). Computerized
Physicians Order Entry: Helpful or Harmful. J. Am.
Med. Assoc., 11, 100-103.
Snyder, R., Weston, M., Fields, W., Rizos, A. & Tedeschi,
C. (2006). Computerized provider order entry system
field research: The impact of contextual factors on
study implementation. Int. J. of Med. Info., 75, 730-
740.
AHRQ (2001). Making Health Care Safer: A Critical
Analysis of Patient Safety Practices. Found in
http://www.ahrq.gov/clinic/ptsafety/
Metzger, J. & Fortin, J. (2003). Computerized Physician
Order Entry in Community Hospitals: Lessons from
the Field. California HealthCare Foundation and First
Consulting Group.
Ash, J. S., Savri, P. Z. & Kuperman, G. J. (2003) .A
Consensus on Considerations for a Successful CPOE
Implementation. J. Am. Med. Assoc., 10, 229-234.
Project Management Institute. A guide to the project
management body of knowledge 3rd edition. Newton
square, OA, 2004.
Bolles, D. (2004) Building project management centers of
excellence. AMACOM.
DeLone, W. H. & McLean, E. R. (1992). Information
systems success: the quest for the dependent variable.
Information Systems Research, 3(1), 1992, 60–95.
DeLone, W. H. & McLean, E. R. (2003). The DeLone and
McLean model of information system success: a ten-
year update. Journal of Management Information
Systems, 19(4), 9–30.
Attewell, P. (1992). Technology diffusion and
organizational learning: the case of business
computing. Organ, Sci. 3, 1-19.
Tanriverdi, H. & Iacono, C. S. (1999). Knowledge barriers
to diffusion of telemedicine. in proceedings (ICIS
20th), Charlotte, NC, 39-50.
Nambisan, S. & Wang, Y.-M (1999). Roadblocks to web
technology adoption? in Commun. ACM. Vol. 42(1),
98-101.
Pare, G. & Trudel, M.-C.(2007). Knowledge barriers to
PACS adoption and implementation in hospitals. Int.
J. of Med. Informatics, 76, 22-33.
Rogers, E. M. (1995). Diffusion of Innovations, 4th
edition, Free press, New York, NY.
A NEW MODEL FOR SUCCESSFUL CPOE DEPLOYMENT AND IMPLEMENTATION IN HOSPITALS
185
