
Patient-centric Handling of Diverse Signals in the mHealth Environment
Jan Sliwa
Bern University of Applied Sciences, Quellgasse 21, CH-2501 Biel, Switzerland
Keywords:
Mobile Health, Signals, Cyber-Physical Systems, Real Time.
Abstract:
In the context of the Mobile Health (or Telemedicine) many signals (data items) are exchanged between the
medical devices, data storage units and involved persons. They are often treated as a uniform mass of “medical
data”, especially in the Big Data community. At a closer look, they unveil various characteristics, like type
(single / continuous), required quality and tolerance for missing values. As in medical care time is crucial, real-
time characteristics are important, like the sampling rate and the overall reaction time of the emergency system.
The handling of data depends also on the severity of the medical case. Data are transferred and processed by
external systems, therefore the overall function depends on the environment and the persons involved: from
the user/patient to a dedicated medical emergency team. The collected data can be anonymously reused to
gain or verify knowledge, what calls for a fair trade-off between the interests of the individual patient and
the community. This paper discusses the semantics of mHealth data, like medical requirements, physical
constraints and human aspects. This analysis leads to a more precise mathematical definition of the required
data handling that helps to construct mHealth systems that better fulfill the health support function.
1 INTRODUCTION
A mobile health system, serving to treat a serious
medical case has to meet many demands. For a de-
signer, it is easy to be biased by his/her own experi-
ence. A developer of smartphone applications, a Big
Data analyzer, a sensorics specialist - each of them
has a different viewpoint and puts stress on differ-
ent aspects of the problem. As the technical issues
are truly challenging and crucial for the success, they
tend to play the dominant role, especially in small
and young enterprises. We will try to connect various
technical viewpoints with the medical perspective in
order to build a unified picture.
Mobile health systems generate and process large
amounts of data. It is important to see their medical
significance which is not equal for all of them. Some
of them are required in a predefined frequency, some
are helpful but optional. Some need a certain preci-
sion, some serve only as orientation values. Some
have to ensure guaranteed reaction times, for some
timing constraints are irrelevant. Some, when an-
alyzed statistically, need a well balanced, unbiased
sample, for some sheer quantity makes them valuable.
This paper takes a closer look at the above
mentioned aspects of mHealth data and brings to
a technically-oriented reader a better view on their
meaning. This semantic view allows in the next step
to formalize the requirements regarding time con-
straints and data extraction, conversion, transmission
and storage. The final goal is to help the reader to
construct better patient-centric medical systems.
Remark: We use here interchangeably the terms
signals or data (items). The word signal stresses the
capture from sensors, whereas data emphasizes the
information content. We also use the term patient,
although in the case of fitness tracking user would be
more correct. As the borders between the application
areas are not sharp, we stay with the first term.
2 RELATED WORK
There are several good overviews of today’s mobile
health technology and applications (Baig et al., 2015),
(Islam et al., 2015), (Silva et al., 2015), (Soh et al.,
2015). A detailed analysis of remote blood glucose
monitoring is given in (Lanzola et al., 2016). Car-
diovascular health and disease is discussed in (Eapen
et al., 2016). The authors also propose a roadmap for
mobile health in this area. An Android-based system
for ECG arrhythmia classification and heart rate vari-
ability analysis is presented in (Xue et al., 2015).
It is useful to look at the mHealth from the
medical perspective. (Itrat et al., 2016) discuss the
Sliwa J.
Patient-centric Handling of Diverse Signals in the mHealth Environment.
DOI: 10.5220/0006298505610568
Copyright
c
2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

telemedicine in prehospital stroke evaluation. (Ag-
boola et al., 2016) presents a bitter reality check for
smartphone apps. A top-selling app for managing and
diagnosing skin cancer was only able to accurately
classify 10 of 93 biopsy-proven melanomas. As for
insulin dose calculation, 67% of the apps gave inap-
propriate output dose recommendations that put users
at risk (Huckvale et al., 2015).
If we analyze the function of the systems not in
the lab, but in real life, practical experience is of
use. (Espinoza et al., 2016) present the design of a
telemedicine management system in Ecuador where
specific local challenges of a rural environment in a
less developed country had to be addressed.
3 SIGNAL TYPES
3.1 Basic Signals
We can divide the basic signals in following cate-
gories:
• Single measurements: (t, value)
• Point events: (t, type)
• Continuous waveforms: (y = f(t))
If we take a closer look, the divisions between
them are blurred. In the case of a chronic dis-
ease, single measurements form a sequence of values.
Point events may be entered as such, like an epileptic
seizure or tumbling. If they are detected by sensors,
they are derived from other measurements, as shown
below. Continuous signals are created by sampling
a property, so formally they are sequences of values,
at a high sampling rate. When we speak of such sig-
nals like ECG (electrocardiogram) or EEG (electroen-
cephalogram), they may come from a single sensor (in
a very basic version) or from a set of sensors placed on
the chest or on the head in well defined locations. In
the latter case we obtain a set of synchronized wave-
forms.
3.2 Derived Signals
From the basic signals we can derive more condensed
information. It is especially useful in the case of con-
tinuous signals the volume of which is too large to
store or transfer. Equally, in the raw form it is not
yet very useful. For the electrocardiogram, a well
known condition is the ST Segment Elevation My-
ocardial Infarction (STEMI). The cardiac cycle has
characteristic points P-Q-R-S-T, and the elevation of
the S-T segment is a signal warning about the risk of
a myocardial infarction, i.e. heart attack. Similarly,
irregularities of the cycle frequency can be identified
as arrhythmia, in several variants, like tachycardia or
bradycardia (heartbeat too fast or too slow). For ar-
rhythmia to be detected, the basic signal has to be an-
alyzed over many cycles. The severity of the case de-
pends on the intensity and duration of the abnormal
condition.
As mentioned above, a point event can be detected
by sensors. For example, tumbling of the patient
can be detected by accelerometers, e.g. in a smart-
phone. In this case, an algorithm extracts a character-
istic waveform from a continuous signal.
When we monitor vital signals, we have to treat
adequately missing values. The fact that the measure-
ment is missing may be an information itself. For ex-
ample, missing a required value for a prolonged time
may indicate that the device is not working (e.g. bat-
tery empty), that something has happened to the pa-
tient or that the patient is not using the device because
it is obtrusive, he/she went on travel and: has forgot-
ten it at home / has left it because of its weight / has
no plug adapter for the charger. In a similar way, sys-
tematic outlier values may mean a health problem or a
wrong placement or poor body contact of the device.
We list those cases in order to stress that the same
observed situation may have very different causes.
Some of them may require intervention of the system
operator (hospital).
3.3 Complex Signals
Until now we have discussed signals coming from
single sources. From the medical point of view, it
is often useful to combine information from many
sources. One of the main reasons is making sharper
distinctions between the cases and eliminating false
alarms. There are many papers presenting methods to
detect patients’ falls with the use of the accelerome-
ters. Typically the accelerometers built in the smart-
phones are considered as described in (Sannino et al.,
2015). They are reasonably ubiquitous, however the
assumption that they are worn all the time seems not
to hold. In any case, if such a device detects the pa-
tient tumbling on the floor, it is useful to verify it with
more data. Especially if the detected condition is se-
vere, requires an action and this action is costly - like
sending an ambulance - it is crucial to detect only real
cases. False alarms, even not frequent, will erode the
confidence in the service.
If we want to design a novel architecture that con-
nects various devices from unrelated producers, we
face the problem of the interoperability. Such devices
- microphone, ECG sensor, EEG headset - typically

are delivered with a connection to the smartphone or
the cloud and visualization and/or analysis applica-
tion. If we want to connect them into a combined
device, we have to go on the level of the internal inter-
faces (rarely disclosed) and to write our own applica-
tion. The system described in (Sannino and De Pietro,
2014) detects fainting and falling of patients by con-
necting the heart rate variability in the ECG with the
information from accelerometers and other body and
environmental sensors. In this way the decisions gen-
erated by the system take the context into account
what increases their reliability.
Not only data formats may pose a problem, also
communication protocols may be different (periodic
sending / on demand), time and data granularity or
measurement precision. When detecting complex
events, we need synchronized data. If they come
marked by internal timestamps, we have to compen-
sate possible differences or to force the synchroniza-
tion of the clocks.
4 CASE SEVERITY
The treatment of the signal depends on the severity of
the medical case. We can list here following classes:
• fitness, general health, behavior modification
• chronic disease
– mild
– severe
• life saving
The influenced factors are:
• required quality
• necessity, sampling rate
• reaction time
If the devices are used for fitness improvement,
the measurements are performed or checked accord-
ing to the interest of the user. The value is rather
used for general information, and there are no tim-
ing requirements. The user often loses interest for
the measurements after a certain time. If in mean-
time he/she changed to a healthier lifestyle, the basic
goal has been achieved.
There is however a risk that the user gets obsessed
with the fitness goals. Some people measure their
weight on bathroom scales many times per day, not
taking account of normal daily variation and measure-
ment errors. In the same way, trying to constantly in-
crease the daily step count, especially when compar-
ing to the group and obtaining (verbal) rewards from
the device, may pose a health risk. There is a certain
optimum and not always more is better. On the other
hand, the device typically just counts steps, so climb-
ing a mountain is like walking, or even of smaller
value, as the covered distance is smaller. Equally
swimming, when the device is left in a locker, does
not count at all. Therefore the user has to be aware
that his/her virtual health is only an imperfect model
of the real one.
This becomes a problem, if the user has an agree-
ment with an insurance company to have a healthy
lifestyle in exchange for lower primes. A simple de-
vice, like an accelerometer in a smartphone, registers
only certain types of activities. On the other hand, the
user may be tempted to cheat the device, by simulat-
ing realistic oscillations.
In a case of a chronic disease, the device is typ-
ically used to monitor the state of the patient, detect
the abnormalities and inform the doctor or hospital
that handles his/her case. For a mild condition, the
measurement can be done occasionally, more or less
periodically or if the patient does not feel well. There-
fore missing values are not problematic, possibly the
patient feels no necessity to act. He/she should not
be burdened too much by reminders. He/she can be
called for a periodic check, as it is for apnea patients
using a ventilator. The measurement should have a
reasonable precision, determined on the basis of the
medical science. It is necessary to eliminate the vari-
ability caused by imprecise placement of the sensor,
too high (or too low) humidity of skin, wrong oper-
ating mode of the device, or similar. If - as we as-
sume - the measurement is performed by the patient
at home, the handling should be entirely simple and
clear. The device has to be approved by the doctor
what eliminates most cheap sensors and easily down-
loadable smartphone applications.
For a severe chronic disease, the requirements for
quality and regularity of the measurements are more
stringent. Regular measurements may show the in-
creased risk before the actual event occurs and the pa-
tient may come for an extensive check or a preven-
tive hospital stay. As the deterioration of the health
state may be rapid and serious, time plays an impor-
tant role. Ergonomics has to be carefully designed,
as in an emergency the patient’s capabilities are im-
paired. For example, during an insulin shock the pa-
tient is dizzy and nervous and his/her vision is blurred.
If the patient is not able to act on his/her own and has
no assistance, an automatic communication with the
hospital is necessary.
For a life saving condition, the precision and re-
action times are even more important. Let us fix our
attention on a patient with a cardiac disease, having
one or more wearable / implantable devices connected
via a wireless Body Area Network (BAN) to a smart-
phone that can alarm the hospital in case of emer-
gency. The devices are active, i.e. can induce a life
saving action locally. As the patient is at risk, he/she
has to adapt his/her life habits accordingly. As the
emergency call system depends on functioning com-
munication, the loss of the phone signal or of data
roaming is a problem. This may occur in a rural area,
in a location not properly covered by the patient’s
provider or in a restaurant restroom in the basement
under a thick concrete floor. Therefore the patient
should avoid such locations, limit the stay and take
care. The current risk level may be evaluated by the
devices and communicated to the patient. In a better
phase less precautions have to be taken. The user in-
teraction design is delicate, as the patient has to know
about the increased risk but on the other hand should
not be overwhelmed by messages. Too many warn-
ings will themselves increase his/her anxiety or with
time will be ignored. An intervention is costly, pos-
sibly includes sending an ambulance, therefore mak-
ing a clear distinction between real and false alarms is
extremely important. When in doubt, the emergency
team may try to contact the patient. However, if the
risk condition is generated by a complex algorithm
combining many factors, the hospital emergency team
may know about the upcoming event earlier than the
patient him-/herself. This evidently is true if the mea-
surement system is reliable and the algorithm is cor-
rect. We see that taking quickly correct, resolute de-
cisions is not easy.
5 REAL TIME ANALYSIS
In the systems that handle serious medical conditions
where emergencies may occur, reaction time is essen-
tial. At the lowest level we treat basic communica-
tions issues, like network architecture, data quantity,
channel capacity and similar. Several papers discuss
these problems and propose various feasible architec-
tures (Thelen et al., 2015), (Castellano et al., 2015),
(Hossain and Muhammad, 2016), (Kang et al., 2015).
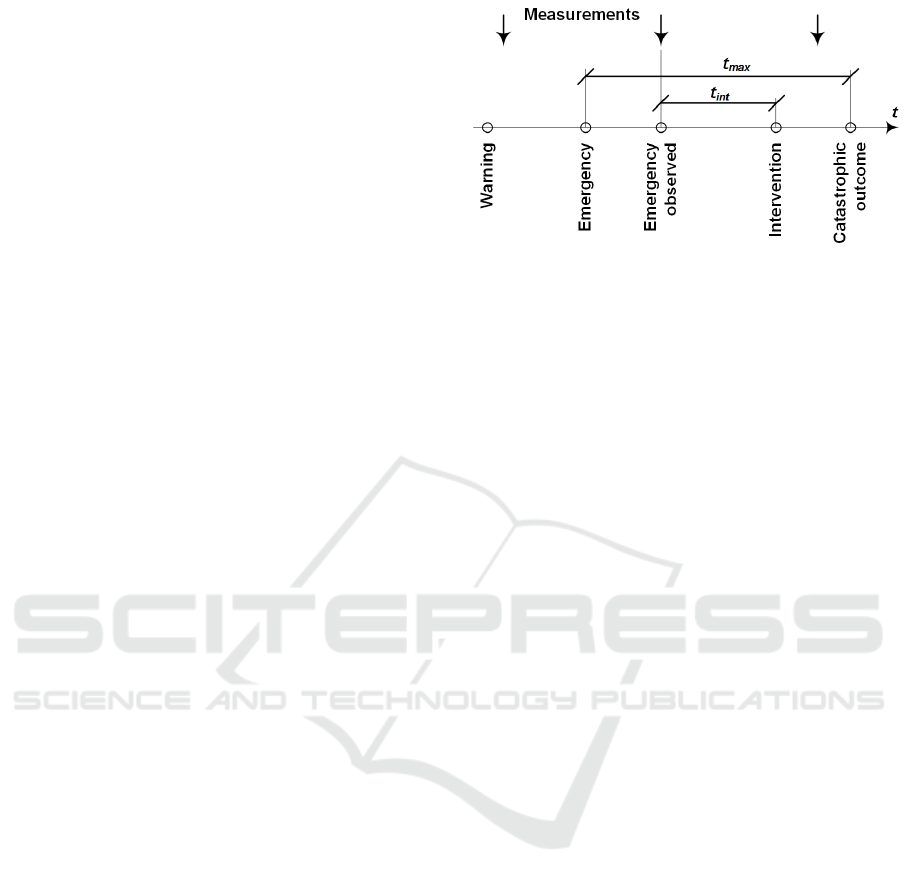
Let us analyze the sequence of events (Figure 1)
that if not handled on time, can lead to a catastrophic
outcome, like death or a durable health damage.
We monitor the health state of the patient with pe-
riodic measurements. The time from the occurrence
of the emergency state to a catastrophic outcome is
a medical fact, as well as the possible outcome itself
(risk level). The time from noticing the emergency to
an intervention depends on technology. The period of
the measurements has to be adapted adequately. For
fast events, like a heart attack, where the time limit
Figure 1: Timing of a medical intervention.
for an intervention is around one hour, the monitoring
should be continuous (measurement period reduced to
almost zero) and the intervention delay reduced to a
minimum. For slow events, like breast cancer, where
the disease develops in months, the measurement pe-
riod is decisive. Not observing this limits makes the
monitoring system virtually useless.
Under warning, as indicated in the figure 1, we un-
derstand some early signals that suggest an increased
risk (yellow alarm). Early warning permits to extend
our time reserve for action. As the indication in this
stage is less decisive, full scale intervention is not ap-
propriate. The patient may however reduce the risk by
taking a rest, performing additional tests or visiting a
doctor.
Breast cancer screening with mammography is a
well studied example of risk analysis (Wegwarth and
Gigerenzer, 2013). The authors show we should be
wary of overdiagnosis and overtreatment.
When deciding what and how to measure and
what actions to take, following factors have to be con-
sidered:
• disease
– development time
– medical risk when not treated on time
– cost of intervention
• measurements (possible overdiagnosis)
– cost (financial and organizational)
– medical side effects
• false positives (overtreatment)
– probability
– cost of unnecessary treatment
– medical side effects
The figure 2 depicts the basic trade-offs in this
process. Mobile health technology mainly permits to
reduce the cost of the measurement and in this way to
make more frequent measurements without visiting a
doctor - at home and in travel. It also permits to send

Figure 2: Trade-offs between various factors influencing a
successful intervention.
quickly the data and emergency alarms, allowing the
patient to maintain the same risk level even having an
active life.
In the case of a disease with high risk and short
required reaction times (like heart disease), it is im-
portant to design carefully the emergency service, en-
suring high reliability and respecting the time limits.
As this problem goes beyond the desine of the device
itself, it will be treated in the following section, re-
garding the Cyber-Physical-Social Systems.
6 CYBER-PHYSICAL-SOCIAL
SYSTEMS
It is important to see that mHealth systems consist of
more than the purely technical elements. They inter-
act intensely with the physical world. The sensors
themselves are material - they need electrical power,
their probes can break, sensing surfaces can have poor
contact to the skin, output nozzles can be clogged. If
we speak of Body Area Network, we have to remem-
ber that tissue and clothing damp the wireless signal.
If the patient moves in the environment, the wire-
less signal connecting him/her with the server may be
blocked by obstacles (e.g. when visiting the restroom
in a restaurant’s basement). He/she can also move into
the area where his provider has a poor signal or data
roaming is impossible.
The emergency systems (Figure 3) are operated
Figure 3: Emergency service.
by humans (Human in the Loop) and depend on their
cognitive skills and information state. For example,
if a heart monitoring system issues an alarm and the
ambulance scheduler has no experience with auto-
mated systems, his/her thinking time adds directly to
the delay of the rescue. The hospital that sends the
ambulance is located near to the current position of
the patient is not necessarily the same that handles
his/her case and owns his/her health record. This re-
quires to arrange the cooperation in advance, includ-
ing a smooth interoperable data transfer and financial
agreements. In the case of a heart attack the whole
process has to be concluded during the golden hour
and leaves no reserve for doubts and clarifications.
This shows that we should ensure that our assump-
tions about the system reliability and availability are
not simplistic. We have to remember that in real life
even a trivial cause (empty battery of a sensor, dry
skin under the sensor patch, loosened contact of a ca-
ble) may have dramatic consequences for the patient’s
health. Therefore when analyzing the system with
formal methods we should be aware that the model
and the real object are different and imagination and
common sense will be helpful.
7 VERIFICATION OF
HYPOTHESES
Data generated in an mHealth supported therapy can
be reused to verify our assumptions and obtain new
knowledge. Let us consider a heart monitoring sys-
tem issuing alarms and warnings in emergency cases.
If the system is working continuously, it can detect
significant events also if the patient is not aware of
anything. They may consist of changed ECG wave-
forms, slower / faster / less periodic frequency or else.
The intensity and duration of such events may play a
role, as well as their sequence. Combining them with
other vital signals will make the detection more spe-
cific.
Figure 4: Using knowledge / hypothesis.
Normally, as shown in the figure 4, we assume that
we know the rules and just detect the characteristic
signals that indicate that an emergency event is immi-
nent.
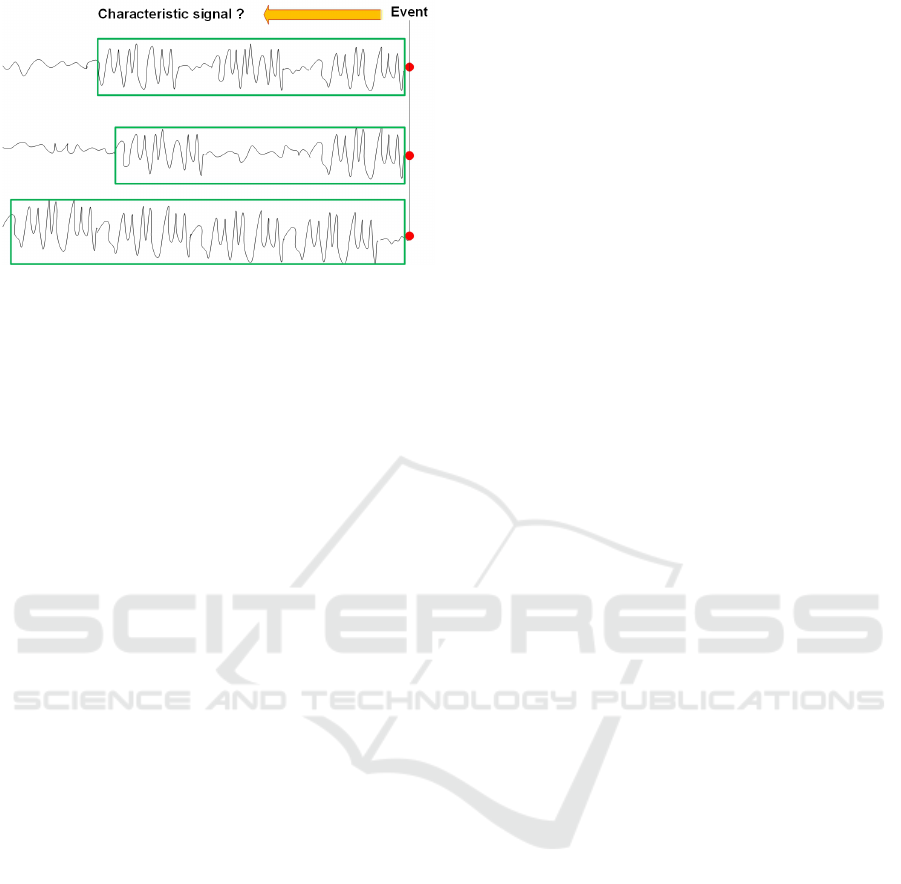
Figure 5: Searching for a new hypothesis.
The area of continuous ECG analysis, especially
combined with other signals, is however fairly new.
Therefore such event detection rules have to be ver-
ified, possibly on many patients, in many situations.
Mobile health systems provide us such opportunity.
We can analyze the actually occurring events and look
back at the signals (Figure 5) searching for telltale
data events, determine their characteristics and ver-
ify if the correlation is significant. In this way, we
can create new hypotheses based on data. Evidently,
quantifying variability of continuous signals is not
easy, especially if we do not know beforehand what
are we looking for. This shows that storing raw data
(or extensive excerpts of them) for later analysis is
useful, even if the benefit is not immediately evident.
8 COMMUNICATION AND
STORAGE - SECURITY
Data collected from a mHealth device are sent to a
receiver. Locally, it may be a smartphone or another
data aggregator. A device can also have a direct con-
nection to a server in the cloud. It is interesting what
happens to those data later: where are they processed
and stored, who owns them, for which purposes can
they be used.
8.1 Architectures
Following factors are important in the analysis of the
transmission and processing of data:
• data quantity
• network independence
• local use of data
– user feedback
– local action
• data reuse at a server
• cost of local computation
• cost of transmission
Especially in handling continuous signals there is
a trade-off between storage, computation and com-
munications. For taking decisions, we are interested
in global parameters (pulse frequency, oxygen satura-
tion) or special states or events (arrhythmia). If the
rules to extract such condensed information are well
defined, it is better to do the processing locally on the
strongest device that can handle this task. This could
mean that the implanted sensor device sends raw data
to the smartphone, and the smartphone executes the
complex calculation. This reasoning is only an ex-
ample, in a specific case a precise analysis of compu-
tational power, transmission channel capacity, energy
costs, etc. has to be performed.
Measurements can be used for local action with
strong requirements for precision and reaction time,
like in glucose management system. It is essential to
ensure this function locally, also in the absence of the
connection with the remote system. In this case we
often speak of Fog Computing - like in Cloud Com-
puting we have storage and processing nodes but not
high in the sky, but rather locally, near to the ground
(Gia et al., 2015), (Chakraborty, 2016).
8.2 Security
As mobile health systems handle very personal data,
they have to be properly secured. This concerns both
data transmission and storage. It is easier said than
done. Sensor and actuator nodes are low power de-
vices and handling strong security is costly. Basically
all exposed networks should be properly managed -
this includes applying security patches if necessary.
However distributing software updates via network is
itself an attack vector.
We have a set of heterogeneous devices com-
ing from different sources, with different lifetimes.
Establishing secure communications with the Public
Key Infrastructure (PKI) is difficult. We have also to
be aware of the trade-off between security and func-
tion. On one hand, the devices should be sure they
talk to trusted partners. On the other hand, if the se-
curity certificate expires on a node and the communi-
cation is blocked, this would stop the proper function
of the device that may be critical for the health or life
of the patient.
Various architectural options, also in the context
of the Internet of Things (IoT) and cloud computing,
with the stress on the security aspects are presented
in (AlTawy and Youssef, 2016), (Gejibo et al., 2015),
(Samie et al., 2016), (Suciu et al., 2015), (Larburu
et al., 2016) and (Sukor et al., 2015).

9 INDIVIDUAL PATIENT AND
POPULATION - PRIVACY
Data regarding individual patients can be collected
and reused for many purposes. Fitness tracking ap-
plications typically permit to send own data to the
pool and to compare personal results with the com-
munity. This community has some basic stratifica-
tion, e.g. with respect to gender and age. The quality
of input data is unproven, no sources of bias are con-
sidered. The power of the solution lies in quantity of
data. Such comparison is used mostly for personal
satisfaction and motivation for further effort. It has
to be mentioned that more effort is not always good,
especially for elderly with osteoporosis and worn-
out knees. The competition may cause an addiction
where gaining points and virtual rewards count more
than the actual health.
In order to participate, the patient has to agree, i.e.
to express consent to share data. However, the exact
conditions of this consent, if published, are never con-
sulted. All detailed data reside on the servers of the
provider and the patient somehow assumes that exact
times and locations of his/her walks will not be dis-
closed to third persons or sold.
In the treatment of more serious medical cases,
data can be aggregated and analyzed in order to ob-
tain and verify knowledge. This can help to identify
risk factors or to issue recommendations for healthy
behavior.
If statistics based on collected data are used for
generating decisions (actionable knowledge), we have
to ensure adequate quality and statistical validity. Var-
ious aspect of medical data reuse are discussed in
depth in (Sliwa, 2016b). If the decisions apply to
the entire population, we should eliminate bias. If
the population shows strong variations, it should be
properly stratified, and the statistics for each category
have to satisfy the quality criteria. This is not easy,
as it is more practical to observe the population than
to execute a formal clinical trial. To put it simply: if
mostly young, technically oriented patients are will-
ing to share their data, those data should not be used
as a benchmark for the entire population, including
the elderly.
Evidently, the system provider has access to all
data and can use them at least to improve the ser-
vice. Due to the fast pace of the technical develop-
ment, much faster than the legislation, from formal
legal point of view the area of reusing mobile health
data is a gray zone. The question of data ownership
in a multi-party Internet of Things (IOT) system, with
smart medical devices as one of the examples, is dis-
cussed in (Sliwa, 2016a).
10 CONCLUSIONS AND FUTURE
WORK
The basic goal of this analysis is to raise awareness for
the semantic aspects of data processing in mHealth
systems. It is important to understand the properties
of the signals flowing from the sensors and their rel-
evance to the overall health support function of the
system. Their properties are determined by the med-
ical factors, like the severity of the case, the possible
outcome. the necessary intervention and its time con-
straints.
After the semantic analysis the elementary prop-
erties of the signals can be extracted, which permit to
build a formal model:
• data type
• conversion algorithm
• timing requirements
• data quantity
• duration and location of storage
• ownership and protection
Nevertheless, it has to be stressed that for complex
Cyber-Physical-Social-Systems, as in Mobile Health,
the formal model is only an approximation and has
to be constantly verified. The environmental condi-
tions are diverse, the technology changes rapidly and
human behavior is difficult to predict, therefore the
usage of such systems has to observed and the design
assumptions have to be periodically reviewed.
REFERENCES
Agboola, S. O., Bates, D. W., and Kvedar, J. C. (2016). Dig-
ital health and patient safety. JAMA, 315(16):1697–
1698.
AlTawy, R. and Youssef, A. M. (2016). Security tradeoffs
in cyber physical systems: A case study survey on im-
plantable medical devices. IEEE Access, 4:959–979.
Baig, M. M., GholamHosseini, H., and Connolly, M. J.
(2015). Mobile healthcare applications: sys-
tem design review, critical issues and challenges.
Australasian Physical & Engineering Sciences in
Medicine, 38(1):23–38.
Castellano, N. N., Gazquez, J. A., Salvador, R.
M. G., Gracia-Escudero, A., Fernandez-Ros, M., and
Manzano-Agugliaro, F. (2015). Design of a real-time
emergency telemedicine system for remote medical
diagnosis. Biosystems Engineering, 138:23–32.
Chakraborty, S. (2016). Data Aggregation in Healthcare
Applications and BIGDATA set in a FOG based Cloud
System. PhD thesis, University of Cincinnati.

Eapen, Z. J., Turakhia, M. P., McConnell, M. V., Graham,
G., Dunn, P., Tiner, C., Rich, C., Harrington, R. A.,
Peterson, E. D., and Wayte, P. (2016). Defining a
mobile health roadmap for cardiovascular health and
disease. Journal of the American Heart Association,
5(7).
Espinoza, J., Chandy, D., Ochoa, S., Jim
´
enez, J., Huerta,
M., Soto, A., Sagbay, G., and Avila, R. (2016). Design
of telemedicine management system in ecuador. In
Ecuador Technical Chapters Meeting (ETCM), IEEE,
volume 1, pages 1–6. IEEE.
Gejibo, S., Mancini, F., and Mughal, K. A. (2015). Mo-
bile data collection: A security perspective. In Mobile
Health, pages 1015–1042. Springer.
Gia, T. N., Jiang, M., Rahmani, A.-M., Westerlund, T.,
Liljeberg, P., and Tenhunen, H. (2015). Fog com-
puting in healthcare internet of things: A case study
on ecg feature extraction. In Computer and In-
formation Technology; Ubiquitous Computing and
Communications; Dependable, Autonomic and Se-
cure Computing; Pervasive Intelligence and Comput-
ing (CIT/IUCC/DASC/PICOM), 2015 IEEE Interna-
tional Conference on, pages 356–363. IEEE.
Hossain, M. S. and Muhammad, G. (2016). Cloud-assisted
industrial internet of things (iiot)–enabled framework
for health monitoring. Computer Networks, 101:192–
202.
Huckvale, K., Adomaviciute, S., Prieto, J. T., Leow, M. K.-
S., and Car, J. (2015). Smartphone apps for calcu-
lating insulin dose: a systematic assessment. BMC
Medicine, 13:106.
Islam, S. R., Kwak, D., Kabir, M. H., Hossain, M., and
Kwak, K.-S. (2015). The internet of things for health
care: a comprehensive survey. IEEE Access, 3:678–
708.
Itrat, A., Taqui, A., Cerejo, R., Briggs, F., Cho, S.-M., Or-
ganek, N., Reimer, A. P., Winners, S., Rasmussen, P.,
Hussain, M. S., et al. (2016). Telemedicine in pre-
hospital stroke evaluation and thrombolysis: taking
stroke treatment to the doorstep. JAMA neurology,
73(2):162–168.
Kang, K., Wang, Q., Hur, J., Park, K.-J., and Sha, L. (2015).
Medical-grade quality of service for real-time mobile
healthcare. IEEE Computer, 48(2):41–49.
Lanzola, G., Losiouk, E., Del Favero, S., Facchinetti, A.,
Galderisi, A., Quaglini, S., Magni, L., and Cobelli, C.
(2016). Remote blood glucose monitoring in mhealth
scenarios: A review. Sensors, 16(12):1983.
Larburu, N., Bults, R., van Sinderen, M., Widya, I.,
and Hermens, H. (2016). Quality-of-data broker for
quality-of-data-aware telemedicine systems. IRBM,
37(4):210–218.
Samie, F., Bauer, L., and Henkel, J. (2016). Iot tech-
nologies for embedded computing: A survey. In
Hardware/Software Codesign and System Synthesis
(CODES+ ISSS), 2016 International Conference on,
pages 1–10. IEEE.
Sannino, G., De Falco, I., and De Pietro, G. (2015). A
supervised approach to automatically extract a set of
rules to support fall detection in an mhealth system.
Applied Soft Computing, 34:205–216.
Sannino, G. and De Pietro, G. (2014). A mobile system for
real-time context-aware monitoring of patients health
and fainting. International journal of data mining and
bioinformatics, 10(4):407–423.
Silva, B. M., Rodrigues, J. J., de la Torre D
´
ıez, I., L
´
opez-
Coronado, M., and Saleem, K. (2015). Mobile-health:
a review of current state in 2015. Journal of biomedi-
cal informatics, 56:265–272.
Sliwa, J. (2016a). A generalized framework for multi-party
data exchange for iot systems. In 2016 30th Interna-
tional Conference on Advanced Information Network-
ing and Applications Workshops (WAINA), pages 193–
198. IEEE.
Sliwa, J. (2016b). Reuse of data from smart medical devices
for quality control and evidence based medicine. In
Dobre, C. and Xhafa, F., editors, Pervasive Comput-
ing: Next Generation Platforms for Intelligent Data
Collection, chapter 9, pages 255–297. Morgan Kauf-
mann.
Soh, P. J., Vandenbosch, G. A., Mercuri, M., and Schreurs,
D. M.-P. (2015). Wearable wireless health monitoring:
Current developments, challenges, and future trends.
IEEE Microwave Magazine, 16(4):55–70.
Suciu, G., Suciu, V., Martian, A., Craciunescu, R., Vulpe,
A., Marcu, I., Halunga, S., and Fratu, O. (2015). Big
data, internet of things and cloud convergence–an ar-
chitecture for secure e-health applications. Journal of
medical systems, 39(11):1–8.
Sukor, J. A., Mohktar, M. S., Redmond, S. J., and Lovell,
N. H. (2015). Signal quality measures on pulse oxime-
try and blood pressure signals acquired from self-
measurement in a home environment. IEEE journal
of biomedical and health informatics, 19(1):102–108.
Thelen, S., Czaplik, M., Meisen, P., Schilberg, D.,
and Jeschke, S. (2015). Using off-the-shelf med-
ical devices for biomedical signal monitoring in a
telemedicine system for emergency medical services.
IEEE journal of biomedical and health informatics,
19(1):117–123.
Wegwarth, O. and Gigerenzer, G. (2013). Overdiagnosis
and overtreatment: evaluation of what physicians tell
their patients about screening harms. JAMA internal
medicine, 173(22):2086–2087.
Xue, S., Chen, X., Fang, Z., and Xia, S. (2015). An
ecg arrhythmia classification and heart rate variabil-
ity analysis system based on android platform. In
Future Information and Communication Technologies
for Ubiquitous HealthCare (Ubi-HealthTech), 2015
2nd International Symposium on, pages 1–5. IEEE.
