
Uncovering Key Factors for a Hospital IT Change Strategy
Noel Carroll
1
, Ita Richardson
1,2
and Marie Travers
2
1
ARCH – Centre for Applied Research in Connected Health, University of Limerick, Limerick, Ireland
2
Lero – the Irish Software Engineering Research Centre, University of Limerick, Limerick, Ireland
Keywords Change Management, Healthcare, Hospital, Kotter’s Model, Quality.
Abstract Changing an Information Technology (IT) system within any organisation is a difficult and complex
process. However, within the hospital setting, additional complexities make such change more difficult.
These complexities include the protection of patient safety and privacy, improving the quality of the patient
experience, protecting information and supporting the clinician in their medical requirements. Our research
indicates that uncovering the process of hospital IT change management is not documented – making it
difficult to build on evidence-based research and instill a ‘lessons learned’ approach in publicly funded
hospitals. We address this gap in this paper. Using qualitative research methods we present the results of
observations carried out in healthcare settings as well as twelve structured interviews with hospital staff. We
employ the Kotter Change Model as a lens to understand this change process. While benefiting from the
structure that Kotter’s model provides, we argue for the need to extend this model in an effort to capture the
various influences of healthcare IT-enabled innovation which will, in turn, enable much needed change
within hospitals. Building on our findings, we introduce a Healthcare IT Change Management Model (HIT-
CMM).
1 INTRODUCTION
In recent years, much has been documented about
the crisis which healthcare systems currently face
due to growing demand and expectations from
traditional healthcare models. Healthcare
organizations now realize that innovation is
increasingly required to sustain a quality healthcare
service system (Cazzaniga and Fischer 2015). To be
successful, innovations through the implementation
and upgrading of Information Technology (IT)
systems should align with practice and support the
evolution of healthcare processes change.
Arguably, the healthcare system suffers from
similar issues experienced by other sectors when
implementing change through IT. For example,
while healthcare service providers commit to
improving a service and invest heavily in
technological infrastructures to reach improved
service levels, managing the change process of IT
innovation is a complex task. Healthcare IT must
protect patient safety and privacy, and in addition,
there are clinical, technical and software regulations
that need to be considered.
Thus, uncovering the process of IT change
management draws on examining a wide range of
perspectives to understand how change can be
successfully managed. There are numerous models
throughout the literature which guide the change
process. Kotter’s change model is one such change
management model. The authors build on a recent
study by Travers and Richardson (2015) which uses
Kotter’s change model (Kotter 2005) to examine
change processes within a private sector medical
device healthcare innovation context. Their study
documented a single case study in a medical device
company. They discovered that process
improvement should be managed through the use of
this model to ensure that change is implemented
systematically throughout the whole organisation. In
this paper, we use the same model as a basis to
understand how IT change has been managed in
public hospital departments. Our results
contextualise the change process within the hospital
domain and allows us to introduce a Healthcare IT
Change Management Model (HIT-CMM).
The next section is divided in two, namely
introducing IT systems in hospital settings and
Kotter’s model.
268
Carroll N., Richardson I. and Travers M.
Uncovering Key Factors for a Hospital IT Change Strategy.
DOI: 10.5220/0006124502680275
In Proceedings of the 10th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2017), pages 268-275
ISBN: 978-989-758-213-4
Copyright
c
2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

2 LITERATURE REVIEW – IT
CHANGE IN HOSPITALS
Change management requires a specific approach to
transition an organisation to a desired future state
(Benjamin and Levinson 1993). Within a hospital
context, the various steps required to achieve a
desired future state is of particular importance to
ensure that patient safety is a priority and quality is
not jeopardized (Cazzaniga and Fischer 2015). The
objective of change management is typically to
provide an approach to implementing change in a
controlled manner while adhering to specific
requirements such as functionality, budget and time
through various deliverables or milestones. Change
management is well documented throughout
literature. For example, Lewin’s Three Step Change
Theory (Lewin 1947) and ADKAR Model (Hiatt
2006) are all applied to various dimensions of the
change process.
2.1 Kotter’s Change Model
Introducing change must be a formalised planned
process (Forte 1997). Even though it is sometimes
considered that having a process can be an overhead,
change management techniques have shown that
when change is planned it is more likely to be
successful (Forte 1997). Therefore, most planning
models assume that changes in organisations are
planned changes (Hayes and Richardson 2008). The
models stipulate that, for successful change, certain
sequential steps need be executed. Kotter’s change
model is one such change management model
(Kotter 2005).
We examine Kotter’s change model (illustrated
in Figure 1) within a publicly funded hospital
setting. We refer to a publicly funded hospital as one
where most of its funding comes from state funds.
In our case study, state funding comes via the HSE.
Using Kotter’s eight steps, we conducted a case
study to answer the following research question:
How do clinical departments within a publicly
funded hospital setting successfully implement an
IT system?
Figure 1: Kotter’s Change Model (illustrated by authors).
3 METHODOLOGY
Qualitative research methods enjoy numerous
approaches to capture raw and rich data. For
example, adopting the case study method provided
us with the structure to devise specific procedures to
design a research strategy, collect data, analyse data,
and present and report the results. We opted to
undertake observational methods within a single
case study considering the unique opportunity to
capture an empirically rich account of specific
phenomena (Yin 2013) within a healthcare context.
The authors carried out one-to-one interviews.
The departments focused on were Radiology,
Dermatology, Quality, Physiotherapy and IT. The
interviews were held with twelve key staff members
who were all involved in IT change to various
degrees. Since the interviewees were healthcare
experts within public hospitals, some were difficult
to access. To overcome this, the authors employed a
snowballing sampling strategy (Grbich 1999). This
was used to identify other experts in this field within
the sample population. This proved to be useful
since each expert was able to recommend the next
relevant expert. Through a structured interview
technique, we were able to provide a more balanced
insight to uncover the change process. The
structured interviews supported our research
methodology by ensuring consistency, i.e. each
interviewee was presented with exactly the same
questions in the same order. The questions had to be
short since the health experts had limited time
available to partake in the case study. The questions
were as follows:
Create
Environment
forchange
• EstablishaSenseofUrgency
• FormaPowerfulGuidingCoalition
• CreateaVision
Engageand
Enablethe
organisation
• CommunicatetheVision
• EmpowerOtherstoActontheVision
• PlanforandCreateShort‐TermWins
Implementand
maintain
change
• ConsolidateImprovementsandProduce
StillMoreChange
• Institutionalisenewapproaches
Uncovering Key Factors for a Hospital IT Change Strategy
269

1. What are the current IT systems in place
within your department?
2. Give examples of how new IT systems or
processes were implemented? Specifically
how was the change process managed? Give
examples.
3. Kotter’s (2005) is a change management
model, which recommends 8 steps to follow
to manage change. Kotter’s Step 7
“Consolidate Improvements and Produce
More Change” recommends that
management or change advocates should be
become more involved in the process thus
ensuring continuation of changes. Kotter’s
Step 8 “Institutionalise New Approaches”
recommends that for success change has to
be implemented so that it is now part of the
organisations culture. Is this true in your
experience in regards to moving or changing
to new IT systems/processes? Give examples.
4. Were there any unexpected problems or
issues that affected such project changes?
Give examples.
5. What is your opinion of the new IT
system/process implemented?
6. What could or should have been done
differently? Give examples.
The interviewees’ answers were reliably
aggregated and comparisons were made between the
different interviewees. We identified a number of
emerging themes using open coding to categorise the
text – allowing us to build a story around specific
events, facts, and interpretations.
The interviewees’ work experience spanned from
4 to 30 years. Participant’s interview data (Table 1)
was analysed to understand the change process
within the case study. We reviewed the data within
the structure of Kotter’s change model steps 1 to 8,
which allowed us to understand how change had
been made within the hospital setting. This
facilitated our gaining a rich insight of the working
environment.
Analysing the findings from the hospital study
we identified key themes. We contextualized these
findings and their implications on Kotter’s change
model. Our results indicate that some aspects of
Kotter’s change model is useful to successfully
manage change but would need to be modified for a
healthcare context. This case study facilitates
analysis from a hospital perspective and the findings
informed and enhanced a proposed model, which we
call the HIT-CMM (see Table 3).
Table 1: Summary of Interviewee Profiles.
Interviewee Department
Yrs
Exp.
Specialty
1 Quality 23
Nurse and Risk
Manager with focus
on use of IT systems
2 Radiology 29
Administration with
focus on quality
3 Physiotherapy 17
General
Administration
4 HR 28 Project Manager
5 Dermatology 4 Clinician
6 Radiology 25
Clinician/Project
Manager
7 IT 30
Manager with focus
on hardware and
software deployment
8 Quality 19
Manager with focus
on rick management
9 Laboratory 28
Manager with focus
on deployment
10 Radiology 28
Clinician/Project
Manager
11 IT 20 Project Manager
12 Quality 10 System user
4 FINDINGS
Within the hospitals, we found that there were silos
of IT innovation in which a clinician or manager
championed IT change. Silos proved problematic
when patients had to move between departments.
The need for national or central rollout of projects
was identified as a solution. National or central
rollouts do take time so some departments would go
ahead and implement new systems thus creating IT
silos.
The interview findings identified various
conduits of information on the real-world IT change
management process, and enabled us to explain how
change management may be viewed as a product of
change leadership. Based on our analysis of the
observations and the interviews, we identified a
number of key themes, which we present as follows:
a) Requirement for Change
b) Attitudes towards new IT systems and
processes
c) Lessons Learned
We provide a discussion to contextualize these
findings and their implications on Kotter’s change
model.
HEALTHINF 2017 - 10th International Conference on Health Informatics
270

4.1 Requirement for Change
The need for change was clearly highlighted from
the interviews. For example, Interviewee 3
explained that “change is overdue as every evening
each patient and the interventions delivered to them
have to be input. This is very time consuming. Also
a big change that is needed is with the problem of
patients not having a unique identifier”. As a
solution to many of these issues, a number of
projects were rolled out to improve services in
Ireland and allow files to be viewed in more than
one hospital. Interviewee 6 confirms that the project
“was rolled out nationally with input locally”.
However, they caution that some form of “follow-up
should have happened as staff are not using all the
features of the system” (Interviewee 6). Targeted
training and proper scoping of projects was
identified as potential solutions by a number of
interviewees. The findings indicate within various
departments in the hospital, change is a forward
planning process, which is well documented and
audited through various stages. Change required a
cultural commitment from the organisation as a
whole to accommodate a new set of procedures, one
of which is the use of auditing.
Stemming from a discussion on change,
Interviewee 1 explained that change processes
should be linked back to the concept of ‘the Iron
Triangle’. They explained that the Iron Triangle
describes the relationship between cost, quality, and
access within the hospital’s department. The basic
premise here is that a change (positive or negative)
in one aspect of the triangle has a direct impact on
the remaining two areas (Kissick 1994). Thus, while
competing with each other, finding a balance and
identifying what specific areas the department can
trade-off becomes a key factor for change
management teams. In addition, the reverse is also
true – while improving one aspect of the Iron
Triangle, change can also have a positive impact on
the remaining two areas.
For the purpose of this research, we focus on the
quality aspects associated with implementing
change. The specific quality, safety and risk
management software used has different sections for
various quality documents on best practice.
Interviewee 1 suggests that the documents should
also link to audits to guide the change process. In
addition, risk assessments are also conducted to
provide a proactive management approach to assess
issues, which may provide future challenges. All of
these efforts support the hospitals quality
improvement plan to identify what implementations
are required and record incidences.
4.2 Attitudes towards New IT Systems
and Processes
The interviewees reported mixed views with the
introduction of new IT systems and processes. While
some seemed relatively pleased with the new
systems, others report disappointment with the
overall change and the manner in which the change
process occurred. Specifically, we revisit the Iron
Triangle to highlight how Access can improve
Quality, which is highlighted by Interviewee 4:
“overall it is an improvement as images can be view
from multiple locations”.
Interviewee 4 explains that “involvement of staff
is crucial for buy-in” which suggests that change
management is a much wider collaborative effort
within a department. Interviewee 5 highlights this
and explains that the implementation of some new
IT systems represents “silo thinking as lack of
understanding of standards, networking, eco-system
and health informatics”. In addition, to
accommodate a smooth change transition, training
on a new system is vital. Interviewee 7 also shares
similar concerns and highlights that “buy-in crucial
to generate enthusiasm” about a change in service
systems. In addition, they suggest “training should
be relevant and timely” which may hamper user
acceptance of IT-enabled innovation. Interviewee 10
also concurs “getting buy-in from stakeholders was
crucial and management had to communicate well to
do this. Without buy-in there is no engagement.
Open meetings are useful”.
We learn that with some projects there were “too
long a time delay from training to using the system”
(Interviewee 4) which can hamper the initial success
of an IT change management programme.
Interviewee 6 shares similar concerns regarding
training and suggests, “more frequent staff sessions
needed. Overall staff felt that training was not
sufficient and more difficult for older people. Staged
training sessions would have helped such as
introduction, advanced, super user training”. While
some projects provide standard operating procedures
(SOP) the inclusion of other software companies for
supporting services may cause concerns for some
users, for example, subcontracting support services
(Interviewee 6).
Our findings also suggest that communication
regarding the objective of implementing change is
critical. For example, Interviewee 7 raises the
question: “What are the objectives?” and goes on to
Uncovering Key Factors for a Hospital IT Change Strategy
271

explain, “there is no point in implementing centrally
and then letting people do what they want locally.
You might as well have two systems”. Interviewee
10 states “communication was good with staff and
team but could have been a lot better with the
general public”. Interviewee 8 also highlights the
importance of communication “very importantly for
bringing in change that communication and team
work essential”. This suggests that implementing
change requires improved planning and
communication strategies. This led us to consider
whether change management requires a specific
approach or whether it is a product of change
leadership, which we examine further in the next
section.
4.3 Lessons Learned
Interviewees were provided with the opportunity to
explain what they might do differently if they were
to undertake a similar change management task.
Interviewee 1 explained that they would like to have
more control of the chosen software vendors and
suggest that not all users were happy with the
software. Interviewee 2 raised more concerns with
the overall change process. For example,
interviewee 2 had concerns around the need to
rebuild a service network, the need to fill out
medical records (time-consuming) and the threat of
personnel moving department or institution and in so
doing, bring much needed competence out of the
department. Therefore, more engagement of all
parties and external expertise is a critical element of
success in change management. Interviewee 5
explains that they could have “engaged with
research centre…to get more visibility”. Building on
this comment, the interviewee suggests that it should
be a national competence approach to similar
projects and explains, “we need a centre such as a
medical software institute with wide stakeholder
representation to oversee projects”.
Interviewee 2 highlights the usefulness of using a
change model such a Kotter’s and indicates that the
eights steps is “what should be done…but plans can
change due to unexpected problems”. This suggests
that there may be a need to offer greater flexibility
or agility to change management models such as
Kotter’s. Interviewee 5 also suggests that models
such as Kotter offer a good basis to manage change.
For example, interviewee 5 further explains, “for our
system we were mobile and patient centric. We
understood the people and their motivations. That is
a platform for engagement and multi-disciplinary
teams”. Adopting an improved structured approach
was discussed by Interviewee 6 discusses this and
suggest that a “well-structured maintenance service
agreements especially out of hours service for
example the previous system came from [Global
Tech Company] and they had a person onsite to deal
with issues”. Interviewee 7 suggests that the success
in implementing change may be in the ability to
understand user’s requirements and foster a
relationship to ensure buy-in at the beginning of the
project: “to implement change you have to talk to
the end user and get buy-in. Start with what you
want and work back. Successful projects always had
buy-in”.
However, to facilitate an improved structured
process, Interviewee 2 indicated the need to
“encourage more trust” and avail of additional onsite
support for the technology providers. One of the
issues associated with the lack of support was the
different time zones (i.e. Ireland and the USA)
requiring out of office phone calls for long
durations. The level of support provided was often
unsatisfactory, for example, “they sometimes say the
problem is our network when the network is
working” (Interviewee 2). Interviewee 4 also shared
these concerns and explained that if they underwent
a similar project they would have “someone on hand
instead of having to ring California with issues”.
This would make a big difference.” The need for
improved planning and greater stakeholder
involvement was discussed. For example,
Interviewee 9 discusses a failed project and suggests
“it was not scoped well and users were not involved
enough”. Interviewee 11 also acknowledges
planning and suggests, “with any project there
should be time given to planning the project
timelines”. In addition, considering that one of the
core objectives was to streamline healthcare
processes, Interviewee 4 highlights their
disappointment in that the project in question, “it is
supposed to be paperless but it is not. Actually we
are using more paper and ink now.” Interviewee 6
explains that going live presented some unexpected
issues: “the initial go live took longer and also the
bedding in period took longer than expected and
more patient lists should have been cancelled
beforehand. So what happened were lots of people
waiting two weeks so it was not patient load
effective at the beginning”. Interviewee 6 goes on to
explain that planning and vision are often
problematic: “we plan things and it takes so long
that by the time it’s implemented the projects are too
old.” Interviewee 6 also highlights some general
issues associated with change management in the
public sector such as:
HEALTHINF 2017 - 10th International Conference on Health Informatics
272

Not enough long-term strategic planning;
Many projects are abandoned;
Need be more proactive rather than reactive;
Need to avail of informed expert opinion on
change management.
Interviewee 7 shares similar concerns and
suggests, “better long-term and short-term planning
is needed”. Thus, there is a clear indication that
implementing change requires a structured approach,
which communicates both the need and benefits of
supporting change.
5 DISCUSSION
This study demonstrates that the need to manage
such change is widely recognized. The interviewees
confirm that management need to lead change.
Reviewing Kotter’s change model and eight phases
of change, we learn that not all eight phases were
necessary to successfully implement change in the
hospital system. We highlight these as Strong
Evidence, Some Evidence and No Evidence as
detailed in Table 2. It also outlines the level of
evidence of Kotter’s change model using the eight
phases, which we identified within our case study.
Kotter’s Step 4 ‘Communicate the Vision’ stipulates
that communication of the vision should come from
senior management.
Therefore, staff were aware of relevant tasks to
be completed in the project and of their roles within
the project. This was not identified by any of the
interviewees as a necessity, yet the hospital
happened to successfully implement change and
raises many questions as to how it could be
improved and what key factors were in play from an
organisational change perspective.
Table 2: Evidence of Kotter’s 8 Phases.
Kotter’s Eight Phases Evidence
1. Establish a Sense of Urgency
2. Form a Powerful Guiding Coalition
3. Create a Vision
4. Communicate the Vision
5. Empower Others to Act on the
Vision
6. Plan for and Create Short-Term
Wins
7. Consolidate Improvements and
Produce Still More Change
8. Institutionalise new approaches
The following steps were strongly identified by
interviewees are being necessary during the
implementation process:
Step 1: Urgency. Hayes and Richardson
(2008) state that, the need for such a change
must be communicated to everyone in the
organisation at the outset. This was
confirmed by the interviewees, as there was
an inherent imperative requirement for
change to the current system in place.
Step 6: Plan. Change should have clear goals
and objectives and take place in small steps.
The interviewees stated that there were
clearly defined goals and that the objectives
were all agreed on to be rolled out nationally.
Step 8: Institutionalise. The interviewees
remarked that the new approach is now part
of normal way of working and is “bedded in
well”.
The following steps were identified by
interviewees as being necessary during the
implementation process but would require a greater
presence throughout the change process:
Step 2: Coalition. Kotter (2005)
recommends progressively involving
different members of the organisation in the
change to form a project team. This was seen
to be the case in one such project within the
hospital, which was ultimately successful.
Coalition was necessary as it involved
numerous team members in various
locations.
Step 3: Vision. Kotter (2005) recommends that a
clear vision and plan for implementing change is
required.
While Step 5: Empower Others to Act on the
Vision was not obvious from our interviews, Kotter
(2005) recommends that obstacles, such as
organisational structure should be removed. The
interviewees confirmed this as a requirement. For
example, while the interviewees mentioned the
various obstacles they would like to remove they
were not empowered to instigate change to act on
the vision.
Overall our findings suggest that there is a clear
need to introduce a new model to support the
implementation of change in a healthcare context.
While Kotter’s Steps 2, 3 and 7 were only partially
implemented in successful projects the aims of these
steps were achieved while carrying out other steps.
Uncovering Key Factors for a Hospital IT Change Strategy
273
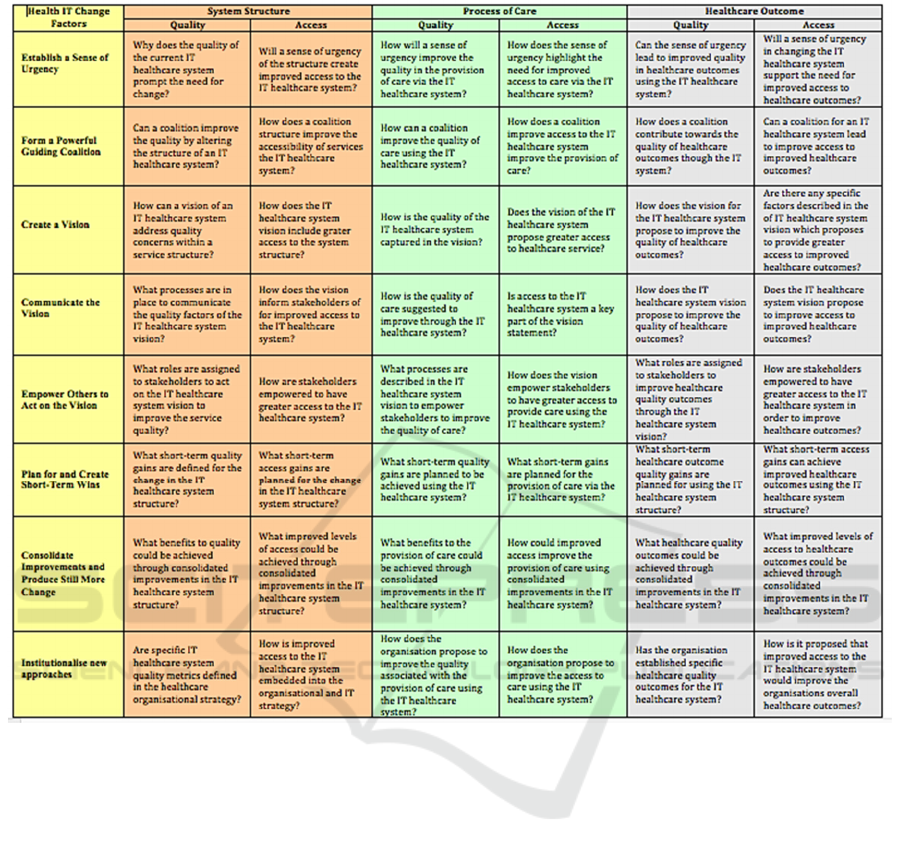
Table 3: HIT-CMM: Quality and Access.
5.1 HIT-CMM
To develop a change model we identified an
approach by O’Leary et al (2015) and Carroll et al
(2016) which examines primary stakeholders to
address their assessment needs from a multi-
perspective viewpoint. We adopted a similar
methodology to influence the development of HIT-
CMM: Quality and Access (Table 3). Cost will be
included in the next iteration of the model. The HIT-
CMM acknowledges that change is
multidimensional and occurs through a series of key
management stages, combining Kotter’s eight steps,
which require assessment as per the Iron Triangle at
various stages of the change management lifecycle.
The questions presented throughout Table 3 are
influenced case study data and constructed to
support the hospital IT change strategy at various
stages of the change process. We also found that
some aspects of Kotter’s change model is useful to
successfully manage change but there are some
shortcomings within a healthcare context. For
example Kotter’s step 5 Empower Others to Act on
the Vision was seen as unnecessary within the
medical device company while in the hospital it was
not obvious from our interviews. Within each of the
phases we assign the relevant Kotter steps to support
change management along with steps identified in
this case study such as Senior Management as
supporters and staff buy-in. Communication of the
vision was already identified as lacking in this case
study, if the HIT-CMM were then used the
assessment of this step should be in terms of cost,
quality, accesses, structure, process and outcome.
6 FUTURE RESEARCH
It is planned to further develop the HIT-CMM and
use it to guide change. This model would build on
HEALTHINF 2017 - 10th International Conference on Health Informatics
274

the specific needs identified such as longer term
strategic planning and more flexibility to manage
unexpected issues. In particular, we will include
Cost as the third element of the Iron Triangle.
The HIT-CMM will be incorporated into a more
detailed strategy model, which also examines the
process of innovation in healthcare. Specifically the
HIT-CMM has already supported us to uncover key
factors for a Healthcare Innovation Strategy and how
we could begin to explore innovation opportunities.
Given the small sample size a more complete picture
will be facilitated by interviewing a larger number of
participants.
7 CONCLUSIONS
This study demonstrated that the need to manage
change is widely recognized. Different perspectives,
methods and approaches (and the underlying
theories that drive them) that are aligned cannot
guarantee to deliver the required change in the time
and on the scale necessary. Reviewing Kotter’s
change model and eight phases of change, we learn
that not all eight phases are necessary to successfully
implement change. Therefore a more tailored yet
detailed framework was required. We present a
mode suitable model to manage healthcare IT
change through the introduction of our HIT-CMM.
ACKNOWLEDGEMENTS
We would like to thank all the participating
interviewees for their time and efforts.
This research is partially supported by Science
Foundation Ireland (SFI) grant no 10/CE/I1855 to
Lero (http://www.lero.ie), by Enterprise Ireland and
the IDA through ARCH – Applied Research in
Connected Health Technology Centre
(www.arch.ie), BioInnovate and by Science
Foundation Ireland (SFI) Industry Fellowship Grant
Number 14/IF/2530.
REFERENCES
Benjamin, R. I., Levinson, E., 1993. A framework for
managing IT-enabled change. In Sloan Management
Review, 34(4), 23-33.
Carroll, N., Travers, M. and Richardson, I., 2016.
Evaluating Multiple Perspectives of a Connected
Health Ecosystem. In 9th International Conference on
Health Informatics (HEALTHINF), Rome, Italy,
February.
Cazzaniga, S., Fischer, S., 2015. How ICH Uses
Organizational Innovations to Meet Challenges in
Healthcare Management: A Hospital Case Study. In
Challenges and Opportunities in Health Care
Management, Springer International Publishing, 355-
361.
Forte, G., 1997. Managing Change for Rapid
Development, In IEEE Software 14(6), 114–123.
Grbich, C., 1999. Qualitative Research in Health: An
Introduction, Sage Publications. California.
Hayes, S., Richardson, I., 2008. Scrum Implementation
using Kotter’s Change Model, 9th International
Conference on Agile Processes and eXtreme
Programming in Software Engineering, Limerick,
Ireland, Lecture Notes in Business Information
Processing 2008, vol 9, Part 6, 10th-14th June, 161-
171.
Hiatt, J. M., 2006. ADKAR: a model for change in
business, government and our community, Prosci
Learning Center. Loveland.
Kissick, W., 1994. Medicine's Dilemmas: Infinite Needs
versus Finite Resources, Yale University Press. New
Haven.
Kotter, J., 2005. Leading Change: Why Transformation
Efforts Fail, Harvard Business School Press. Boston.
Lewin, K., 1947. Frontiers in Group Dynamics: Concept,
Method and Reality in Social Science; In Social
Equilibria and Social Change. Human Relations, June,
1(36).
O'Leary, P., Carroll, N., Clarke, P. and Richardson, I.,
2015. Untangling the Complexity of Connected Health
Evaluations. In International Conference on
Healthcare Informatics (ICHI), October, 272-281.
IEEE.
Travers, M., Richardson, I., 2015. Medical Device
Software Process Improvement – A Perspective from a
Medical Device company, in 8th International
Conference on Health Informatics, (Healthinf),
Lisbon, Portugal, January.
Yin, R. K., 2013. Case study research: Design and
methods, Sage publications.
Uncovering Key Factors for a Hospital IT Change Strategy
275
