
COVID-19 Comorbidities: How Do Underlying Hypertensive and
Cardiovascular Conditions Affect the Prognosis and Therapies of
COVID-19?
Huiyi Xiong
a
Biomedical Engineering, Boston University, Boston, MA, 02215, U.S.A.
Keywords: COVID-19, Underlying Comorbidities, Cardiovascular System.
Abstract: The coronavirus disease 2019 (COVID-19), a contagious disease caused by the SARS-CoV-2 virus, spread
worldwide in a short period and affected the lives of billions of people. Recent studies have found that many
COVID-19 patients have underlying comorbidities that lead to acute disease prognosis and more severe
complications of COVID-19 symptoms. Among all common comorbidities, hypertension and cardiovascular-
related diseases appear more frequently in patients. In this review, we investigate the bidirectional interaction
between COVID-19 and the cardiovascular system by clarifying the effects of SARS-CoV-2 infection on
underlying hypertension conditions and cardiovascular disorders and how hypertension and cardiovascular
diseases affect the mortality and prognosis COVID-19. Combined with analysis of promising but currently
controversial remedies for COVID-19, such as anti-hypertensive therapies that use ARBs and ACE inhibitors
and other treatments of acute COVID-19 cardiovascular syndrome, we could better understand the
interactions between SARS-CoV-2 virus and hypertensive-cardiovascular related comorbidities to develop
safer and more effective treatments for COVID-19.
1 INTRODUCTION
COVID-19 is a contagious disease caused by SARS-
CoV-2. Researchers have found that SARS-CoV-2
has numerous similar biological characteristics to
SARS-CoV, which caused the 2002 outbreak. SARS-
CoV-2 binds the viral spike protein to ACE2 for cell
entry into human bodies (Allen, Altae-Tran, Briggs,
Jin, McGee, Shi, Lin, Bansal, Bosso, Thanaraj, Abu-
Farha, Alanbaei, Abubaker, & Al-Mulla 2020)
Comorbidities increase the severity of COVID-19
symptoms, prolong the viral clearance time, and
deteriorate acute disease prognosis, thus leading to
more severe forms and complications of COVID-19
in patients (De Cauwer, Ejaz, Alsrhani, Zafar, Javed,
Junaid, Abdalla, Younas, Esakandari, Nabi-Afjadi,
Fakkari-Afjadi, Farahmandian, Miresmaeili, &
Bahreini, Fang, Karakiulakis, & Roth 2020). Among
these factors, we found that hypertension and
cardiovascular diseases are associated with cardio-
cerebrovascular systems. The exceeding frequency of
COVID-19 patients with hypertension and
cardiovascular diseases implies the crucial role they
a
https://orcid.org/0000-0003-1449-3996
played in the prognosis of COVID-19 patients and
thus need to be investigated comprehensively.
This review will collect common comorbidities
found by various studies and evaluate the substantial
incidence of COVID-19. We will investigate the
mechanisms of how the SARS-CoV-2 virus affects
hypertension and cardiovascular conditions of
patients. The impacts of underlying hypertension and
cardiovascular diseases on the progression and
prognosis of COVID-19 will be collected as well,
especially factors that affect the morbidity and
mortality of COVID-19 (Fox, Akmatbekov, Harbert,
Li, Quincy Brown, & Vander Heide 2020), we also
analyze current treatments toward COVID-19 induced
comorbidities in line with ACE2 expression
mechanism. There are debates about whether using
RAAS inhibitors (ARBs and ACEI) in COVID-19
patients is effective, with some studies claiming they
could alleviate inflammatory responses (Fujihashi, &
Jones 2020) while other studies were arguing that they
would rise the severity of COVID-19 symptoms
instead (Garg, Kim, Whitaker, O'Halloran,
Cummings, Holstein, Fry 2020). The treatments
toward acute myocardial injury, a representative acute
584
Xiong, H.
COVID-19 Comorbidities: How Do Underlying Hypertensive and Cardiovascular Conditions Affect the Prognosis and Therapies of COVID-19?.
DOI: 10.5220/0011515700003438
In Proceedings of the 1st International Conference on Health Big Data and Intelligent Healthcare (ICHIH 2022), pages 584-590
ISBN: 978-989-758-596-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
respiratory syndrome associated with high mortality
of hospitalized COVID-19 patients, are also
investigated to show that current treatments toward
COVID-19 induced comorbidities involve complex
factors, and the efficacy of many treatments are still
uncertain.
2 COVID-19 CLINICAL
CHARACTERISTICS
COVID-19 patients could report various symptoms
ranging from mild symptoms to severe illness and
even death. COVID-19 symptoms usually begin
between 2 and 14 days after being infected, and the
incubation period is estimated to be approximately 5
days after exposure to the SARS-CoV-2 virus, similar
to SARS (Garg, S). The virus can be spread to others
from someone infected with the coronavirus but is in
the pre-symptomatic or asymptomatic state (Gasmi,
Peana, Pivina, Srinath, Gasmi Benahmed, Semenova,
Menzel, Dadar, & Bjørklund 2021, Gold, Guo, Fan,
Chen, Wu, Zhang, He, Lu 2020).
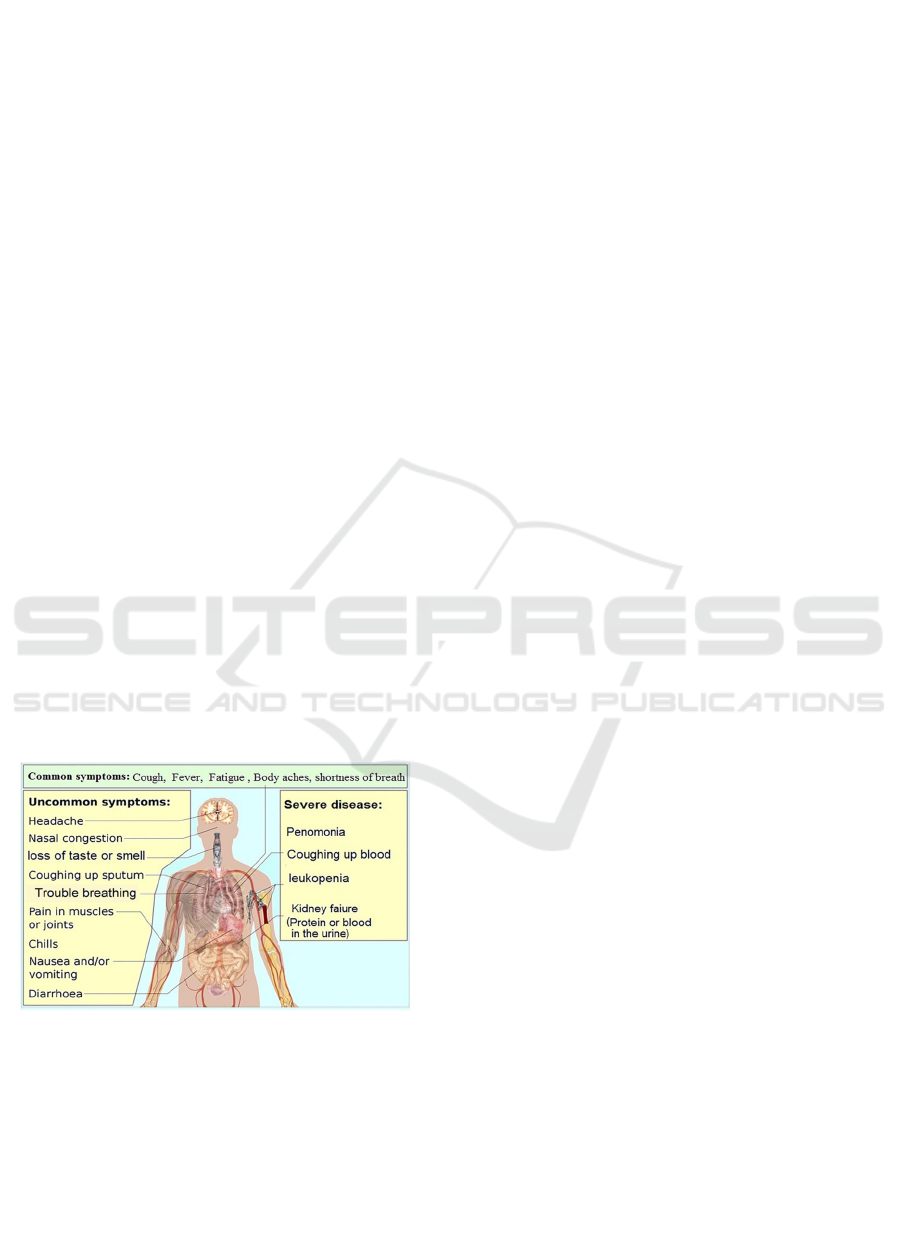
According to information from CDC as shown in
Figure 1, it would be necessary to seek emergency
medical attention if patients manifest severe
symptoms, (Guo, Fan, Chen, Wu, Zhang, He, Lu
2020, Hancox, Hasnain, Vieweg, Crouse, &
Baranchuk 2013). Based on 3,661,716 total responses
about COVID-19 symptoms collected in the United
States, the common symptoms reported by most users
(73%) (Hendren, Drazner, Bozkurt, & Cooper 2020).
Figure 1. The systemic disorders caused by COVID-19
(Lauer, Grantz, Bi, Jones, Zheng, Meredith, Lessler 2020).
COVID-19 could be especially life-threatening to
older adults and young children. The severity of
COVID-19 varies dramatically for patients of
different ages. Age as a risk factor seems to be
independent of common comorbidities (Liu, Huang,
Xu, Yang, Qin, Cao, Jiang 2020). Additionally, old
adults with severe underlying medical conditions
seem to have higher risks of developing more serious
COVID-19 symptoms (Hancox, Hasnain, Vieweg,
Crouse, & Baranchuk 2013). Children infected with
COVID-19 usually have a milder illness than adults.
Additionally, these children may also tend to
experience very rare complications of the
coronavirus, such as having abdominal symptoms
like skin changes or rashes (Maragakis 2021).
3 PROFILE OF COMORBIDITIES
Current studies have revealed that the severity of
COVID-19 is highly related to comorbidities (Mayo
Clinic Staff 2021). Comorbidities contribute to acute
disease prognosis, and increased risk of severe
symptoms and more comorbidities were found in
severe cases compared to non-severe cases (Bosso,
Thanaraj, Abu-Farha, Alanbaei, Abubaker, & Al-
Mulla 2020). In a research study, over 50% of
patients reported having at least one comorbidity,
and around 70% of ICU patients have been observed
to have comorbidities (De Cauwer 2020). Another
study conducted among 178 adult patients about
underlying conditions shows that 89.3% of patients
had one or more underlying conditions (McGonagle,
Plein, O'Donnell, Sharif, & Bridgewood 2020). To
be specific, different types of comorbidities need to
be investigated.
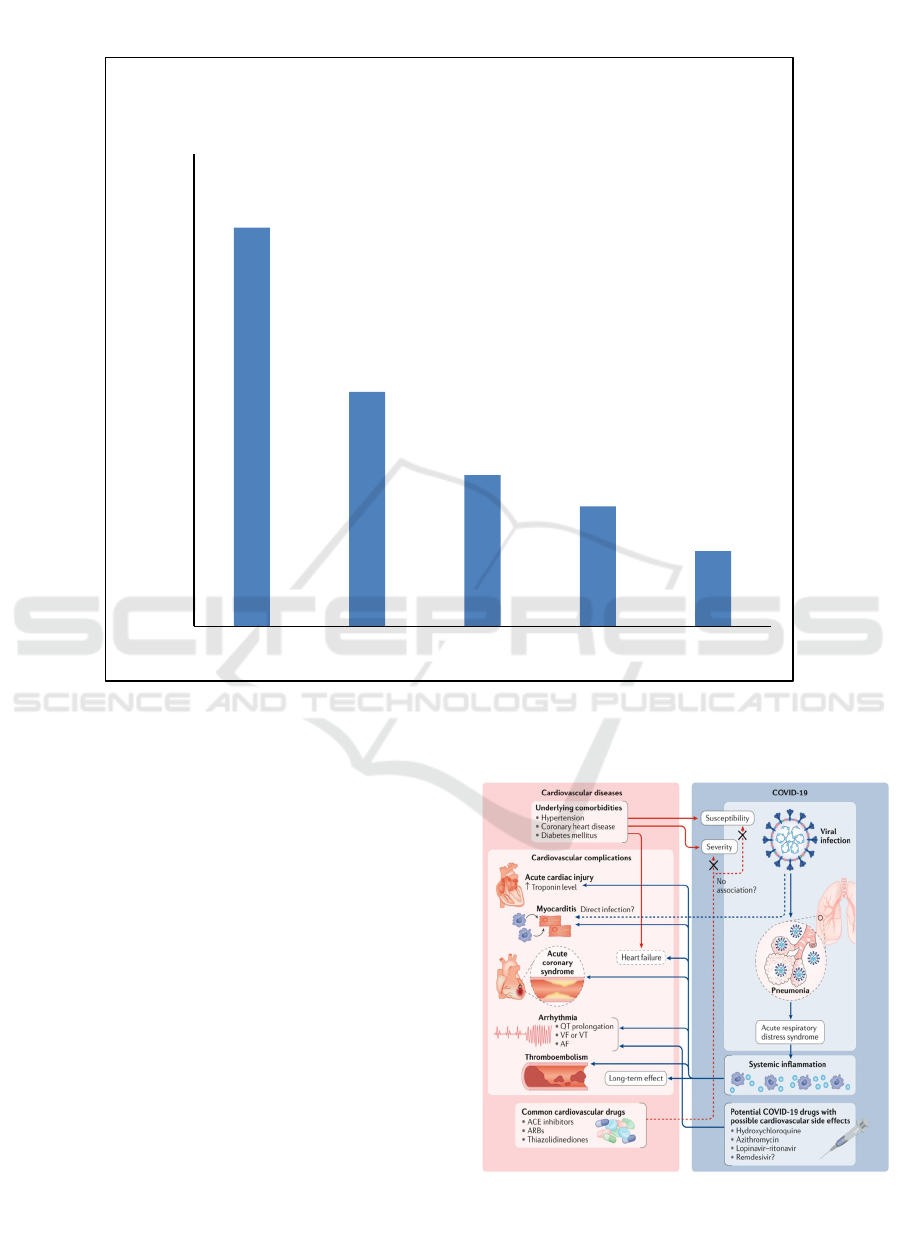
A study among 225 patients with severe COVID-
19 symptoms who were hospitalized in eight Georgia
hospitals during March 2020 reported comorbidities
including hypertension (67.5%), diabetes (39.7%),
cardiovascular disease (25.6%), chronic lung disease
(20.3%), severe obesity (BMI ≥40, 12.7%) (Mayo
Clinic Staff 2021).
The percentage of each type of
comorbidity is shown in Figure 2. These studies
show that hypertension, obesity, and cardiovascular
diseases are the top 3 comorbidities of COVID-19.
We have noticed that two of the three most common
commodities are related to a heart condition and
blood pressure (Meng, Xiao, Zhang, He, Ou, Bi,
Zhang 2020). This suggests that people with
preexisting high blood pressure may be at higher risk
of becoming severely ill with COVID-19 and may
induce further hypertensive heart conditions and
high blood pressure. The exceeding frequency
implies a causal relationship between hypertension
and COVID-19, leading to more severe
complications of COVID-19 in patients (Mueller,
McNamara, & Sinclair 2020). Therefore, this review
will mainly focus on hypertension and
cardiovascular problems, investigating how the
SARS-CoV-2 virus interacts with these underlying
COVID-19 Comorbidities: How Do Underlying Hypertensive and Cardiovascular Conditions Affect the Prognosis and Therapies of
COVID-19?
585
conditions and how these conditions impact the
progression and prognosis of COVID-19 (Muhamad,
Ugusman, Kumar, Skiba, Hamid, &, Aminuddin
2021).
Figure 2. Common comorbidities associated with COVID-19 infection collected from clinical outcomes of adult patients
hospitalized in Georgia (Mayo Clinic Staff 2021).
4 THE MECHANISM OF
COVID-19-INDUCED
DETERIORATION OF
HYPERTENSION AND
CARDIOVASCULAR DISEASE
The mechanisms underlying this interaction need to
be figured out to clarify the bidirectional interaction
between COVID-19 and the cardiovascular system.
Figure 3 shows how COVID-19 interacts with
underlying comorbidities and leads to cardiovascular
complications.
Figure 3. Bidirectional interaction between cardiovascular
diseases and COVID-19 (Allen, Altae-Tran, Briggs, Jin,
McGee, Shi, Lin 2020).
67,50%
39,70%
25,60%
20,30%
12,70%
0,00%
10,00%
20,00%
30,00%
40,00%
50,00%
60,00%
70,00%
80,00%
hypertension diabetes cardiovascular
disease
chronic lung
disease
obesity
COVID-19 Comorbidities in 225 COVID-19
patients in Georgia Hospitals
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
586

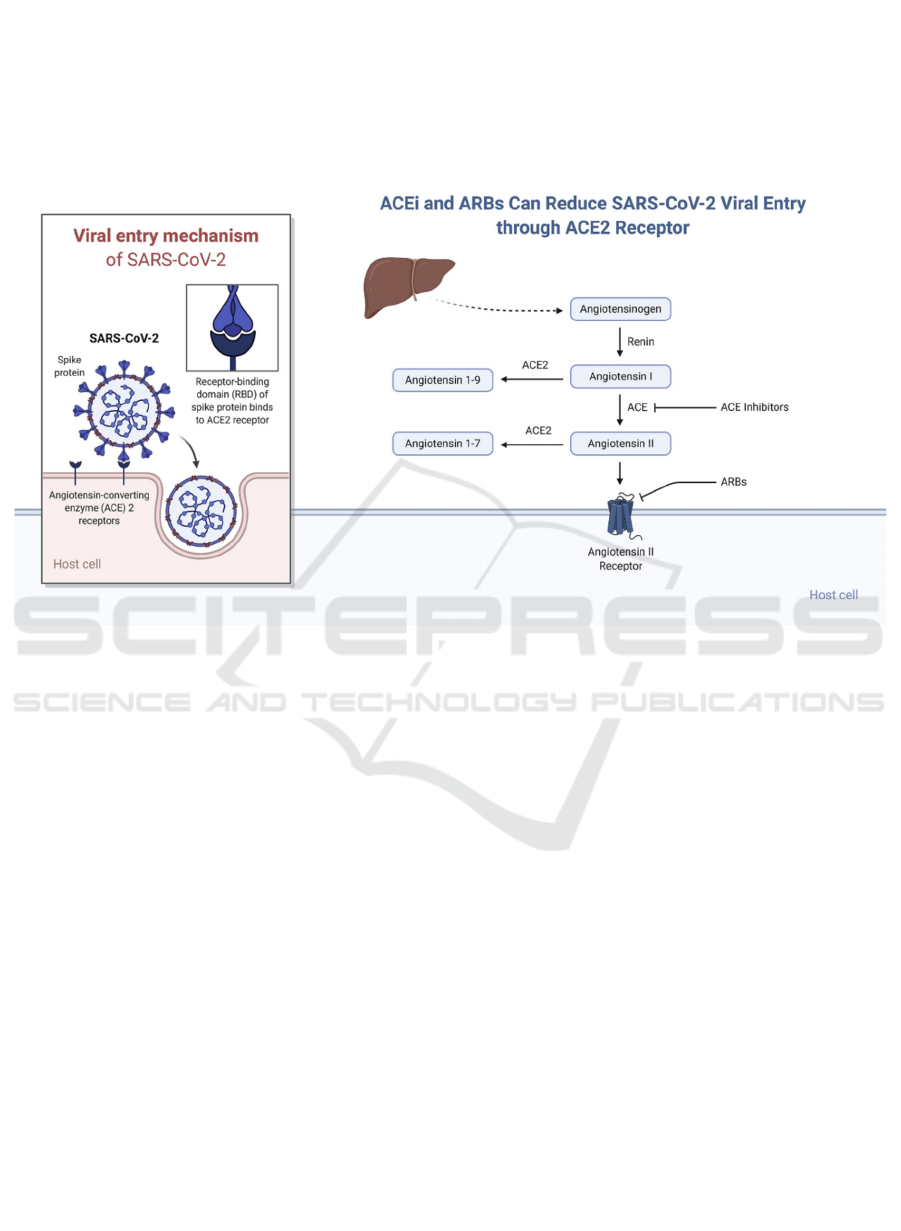
The mechanisms and pathophysiology underlying
the development of COVID-19-related
cardiovascular injury are currently unclear, but
ACE2, a surface protein for SARS-CoV-2 virus entry
and part of RAAS, is known to be a significant factor
involved in the biological mechanism of COVID-19
infection (Nishiga, Wang, Han, Lewis, & Wu 2020).
It would be possible that SARS-CoV-2 could directly
infect multiple cardiovascular cell types. However,
since the expression of ACE2 in itself is not sufficient
for the virus to enter the cell, the interaction is more
likely to affect the cardiovascular system in an
indirect manner (Allen, Altae-Tran, Briggs, Jin,
McGee, Shi, Lin 2020).
The factors that trigger the impact of the SARS-
CoV-2 virus on hypertension conditions are
controversial. Some studies mentioned that that
originally target the Renin-Angiotensin System
(RAS) for anti-hypertensive purposes. In certain
studies, they are demonstrated to increase ACE2
expression and thus increase the severity of COVID-
19 symptoms (Garg, Kim, Whitaker, O'Halloran,
Cummings, Holstein, Fry 2020). In contrast, in other
studies, the use of ACEi/ARB drugs attenuates
inflammatory responses of COVID-19 patients by
inhibiting IL-6 cytokine levels (Osibogun, Balogun,
Abayomi, Idris, Kuyinu, Odukoya, Akinroye,
Pettersson, Manley, & Hernandez 2021).
5 IMPACTS OF HYPERTENSION
AND CARDIOVASCULAR
DISEASES CONDITIONS ON
THE PROGNOSIS OF
COVID-19
Many studies evaluating COVID-19 prognosis
demonstrated that cardiovascular diseases and
hypertension conditions significantly increase the
severity and mortality rate of COVID-19 patients
(Garg, Kim, Whitaker, O'Halloran, Cummings,
Holstein, Fry 2020). The impacts could be best
manifested in mortality rate data (Preventing the
spread of the coronavirus. 2021). Accordingly, the
case fatality rate (CFR) was also significantly higher
for patients with hypertension and CVD (Meng, Xiao,
Zhang, He, Ou, Bi, Zhang 2020). Additionally, a
research study suggested that hypertension and
cerebro-cardiovascular diseases could be critical
factors that lead to the higher mortality of COVID-19
patients.
To evaluate factors that cause the high mortality
rates for COVID-19 patients with hypertension and
cerebro-cardiovascular diseases, Sharon Fox el. from
the Lancet Respiratory Medicine demonstrates that
the high mortality rates could be attributed to severe
lung involvement, diffuse alveolar damage, and
pulmonary tissue destruction (Public Health Agency
of Canada. 2021). The infected alveolar ACE2+
(angiotensin-converting enzyme 2) cells with
extensive pulmonary vasculature lead to pulmonary
hypertension development due to a pulmonary
intravascular coagulopathy. Therefore, ACE2
expression on endothelial cells could cause virally
mediated endothelins linked to increased mortality
(Riphagen, Gomez, Gonzalez-Martinez, Wilkinson,
& Theocharis, Ruan, Yang, Wang, Jiang, & Song,
Sanyaolu, Okorie, Marinkovic, Patidar, Younis,
Desai, Altaf 2020). In another study in the scope of
150 patients, 32% of patients were reported to have
an acute myocardial injury with heart failure as a
contributing factor (Schiffrin, Flack, Ito, Muntner, &
Webb 2020). These data demonstrate that pulmonary-
related diseases and acute myocardial injury could be
the commonly observed complications leading to the
higher mortality of COVID-19 patients with
hypertension and cardiovascular diseases.
Some studies use the cardiac troponin T level as a
predictive prognosis parameter (Shi, Qin, Shen, Cai,
Liu, Yang, Huang 2020). Combined with other
studies, acute myocardial injury is an essential factor
in the death of COVID-19 patients, and the markers
of myocardial injury could be used to predict the risk
of in-hospital mortality in patients with severe
COVID-19.
6 TREATMENTS TOWARD
COVID-19 INDUCED
COMORBIDITIES
Among widely known treatments, many targeted the
mechanism of the interaction between SARS-CoV-2
virus and ACE2 molecules to alleviate hypertension-
related COVID-19 symptoms. Combined with other
studies that revealed the elevated expression of ACE2
in blood samples from COVID-19 patients
(Symptoms of covid-19. (2021), Turner, Hiscox, &
Hooper 2004, Wan, Shang, Graham, Baric, & Li
2020). While ACEIs/ARBs are proven to be effective
in preventing and treating COVID-19 infections in
some animal studies, limited clinical data in humans
could show that ACE-inhibitors or ARBs affect the
severity of COVID-19 patients with CVD
comorbidity, either improve or deteriorate (Wu, &
McGoogan 2020). By contrast, another retrospective
COVID-19 Comorbidities: How Do Underlying Hypertensive and Cardiovascular Conditions Affect the Prognosis and Therapies of
COVID-19?
587
study was conducted among 511 COVID-19 patients
with hypertension comorbidity to compare the
severity of SARS-CoV-2 infection for those who used
one of the anti-hypertension drugs and those who
used none (Yang, Tan, Zhou, Yang, Peng, Liu, He
2020). The implication of this study recommends
using treatments with ACEI and ARBs are
continuously in patients with hypertension or CVD to
reduce the morbidity and mortality of SARS-CoV-2
infection, especially in elderly COVID-19 patients
(Fujihashi, & Jones 2020). Therefore, anti-
hypertensive therapies such as ARBs or ACEI could
be a possible solution to COVID-19 patients with
hypertensive-related comorbidities, but the efficacy
and potential effects still need further investigation.
Figure 4. ACE2 in the Entry of SARS-CoV-2 into the Host Cell and the function of ACEi and ARBs to reduce SARS-CoV-
2 viral entry (Pettersson, Manley, & Hernandez 2021).
Besides treatments that aim to reduce
hypertension-related comorbidities exacerbated by
the SARS-CoV-2 virus, other treatments focused on
managing the acute COVID-19 cardiovascular
syndrome (Allen, Altae-Tran, Briggs, Jin, McGee,
Shi, Lin 2020). Due to the contagious nature of
COVID-19, the priorities in the diagnosis stage
include reducing staff/patient exposures by limiting
testing and patient transfer to avoid the delay of
diagnostic procedures, though this would reduce the
certainty of diagnosis. Therefore, it is essential to
minimize the staff/patient exposure for testing while
not changing clinical management that recognizes
syndromes when the most effective intervention.
One focus among acute respiratory syndromes
would be an acute myocardial injury, the comorbidity
that appears to complicate the symptoms of
hospitalized patients and is associated with high
mortality, as mentioned in the earlier paragraph
(Ruan, Yang, Wang, Jiang, & Song 2020). In some
cases, patients diagnosed with myocarditis relating to
COVID-19 were treated with extracorporeal
membrane oxygenation, steroids, intravenous
immunoglobulins, and antiviral therapy and
subsequently recovered.
Treatments need to vary according to the special
situations of patients. In multiple COVID-19 clinical
studies, Hydroxychloroquine and azithromycin,
drugs that show improved clinical recovery time,
body temperature recovery time, cough remission
time, and pneumonia-related symptoms compared to
traditional treatments, are also known to induce
arrhythmias, prolong the QT interval, and more likely
to have cardiac arrest (Allen, Altae-Tran, Briggs, Jin,
McGee, Shi, Lin, Zeng, Liu, Yuan, Wang, Wu, Li,
Liu, Zhang, Dong, Cao, Yuan, Yang, Yan, Gao
2020). Another drug combination Lopinavir–
ritonavir, should be carefully used in COVID-19
patients (Allen, Altae-Tran, Briggs, Jin, McGee, Shi,
Lin 2020). In sum, acute COVID-19 cardiovascular
syndrome management needs to consider complex
factors (Ruan, Yang, Wang, Jiang, & Song 2020).
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
588

7 CONCLUSIONS
Current studies have revealed that comorbidities and
underlying conditions are strongly associated with the
severity of COVID-19 symptoms, contributing to
more acute disease prognosis and increased risk of
severe symptoms. Among the most influential
comorbidities, hypertension and cardiovascular
diseases appear with exceeding frequency in COVID-
19 patients. The interaction between the expression of
ACE2 protein and the SARS-CoV-2 virus is a
significant factor involved in the biological
mechanism of COVID-19 viral entry and infection
and then affects the cardiovascular system.
Hypertension and cardiovascular diseases also impact
the progression and prognosis of COVID-19, which
are manifested in higher mortality rates and longer
viral clearance time. Major factors contributing to
high mortality rates of COVID-19 patients with
cardiovascular conditions include pulmonary tissue
destruction and acute myocardial injury. Potential
remedies for COVID-19 include ARBs (angiotensin
II receptor blockers) or ACE (angiotensin-converting
enzyme) inhibitors, which are anti-hypertensive
therapies, but the efficacy and further effects of these
treatments are still controversial. Other treatments
that focus on the management of the acute COVID-
19 cardiovascular syndrome, especially for acute
myocardial injury, need to vary according to different
situations of patients and consider complex factors.
Some treatments of COVID-19 have some known or
unknown cardiovascular adverse effects to be
noticed. Learned from imperfections of current
COVID-19 treatments, researchers may have a
clearer direction of drug development that improves
efficacy while reducing side effects.
REFERENCES
Allen, W. E., Altae-Tran, H., Briggs, J., Jin, X., McGee, G.,
Shi, A., . . . Lin, X. (2020). Population-scale
longitudinal mapping of COVID-19 SYMPTOMS,
behaviour and testing. Nature Human Behaviour, 4(9),
972-982.
Bansal, M. (2020). Cardiovascular disease and COVID-19.
Diabetes & Metabolic Syndrome: Clinical Research &
Reviews, 14(3), 247-250.
Bosso, M., Thanaraj, T. A., Abu-Farha, M., Alanbaei, M.,
Abubaker, J., & Al-Mulla, F. (2020). The two faces of
ace2: The role of ace2 receptor and its polymorphisms
in hypertension and covid-19. Molecular Therapy -
Methods & Clinical Development, 18, 321
De Cauwer, H. (2020). The sars-cov-2 Receptor, ACE-2, is
expressed on many different cell types: Implications for
Ace-inhibitor- AND angiotensin II receptor blocker-
based cardiovascular Therapies: Comment. Internal and
Emergency
Ejaz, H., Alsrhani, A., Zafar, A., Javed, H., Junaid, K.,
Abdalla, A. E., . . . Younas, S. (2020). COVID-19 and
comorbidities: Deleterious impact on infected patients.
Journal of Infection and Public Health, 13(12), 1833-
1839.
Esakandari, H., Nabi-Afjadi, M., Fakkari-Afjadi, J.,
Farahmandian, N., Miresmaeili, S., & Bahreini, E.
(2020). A comprehensive review of COVID-19
characteristics. Biological Procedures Online, 22(1).
Fang, L., Karakiulakis, G., & Roth, M. (2020). Are patients
with hypertension and diabetes Mellitus at increased
risk FOR COVID-19 infection? The Lancet Respiratory
Medicine, 8(4).
Fox, S., Akmatbekov, A., Harbert, J., Li, G., Quincy
Brown, J., & Vander Heide, R. (2020). Pulmonary and
CARDIAC pathology in African American patients
with COVID-19: An AUTOPSY series from New
Orleans. The Lancet Respiratory Medicine, 8(7), 681-
686.
Fujihashi, A., & Jones, J. (2020). Association of treatment
With Hydroxychloroquine OR azithromycin WITH in-
hospital mortality in patients With COVID-19 in New
York State. The Journal of Emergency Medicine, 59(2),
333-334.
Garg, S., Kim, L., Whitaker, M., O'Halloran, A.,
Cummings, C., Holstein, R., . . . Fry, A. (2020).
Hospitalization rates and characteristics of patients
hospitalized with laboratory-confirmed Coronavirus
DISEASE 2019 — COVID-NET, 14 states, March 1–
30,
Garg, S., Kim, L., Whitaker, M., O'Halloran, A.,
Cummings, C., Holstein, R., Prill, M., Chai, S. J.,
Kirley, P. D., Alden, N. B., Kawasaki, B., Yousey-
Hindes, K., Niccolai, L., Anderson, E. J., Openo, K. P.,
Weigel, A., Monroe, M. L., Ryan, P., Henderson
Gasmi, A., Peana, M., Pivina, L., Srinath, S., Gasmi
Benahmed, A., Semenova, Y., Menzel, A., Dadar, M.,
& Bjørklund, G. (2021). Interrelations between
COVID-19 and other disorders. Clinical immunology
(Orlando, Fla.), 224, 108
Gold, J., Wong, K. K., Szablewski, C. M., Patel, P. R.,
Rossow, J., da Silva, J., Natarajan, P., Morris, S. B.,
Fanfair, R. N., Rogers-Brown, J., Bruce, B. B.,
Browning, S. D., Hernandez-Romieu, A. C., Furukawa,
N. W., Kang, M., Evans, M. E., Oosmanally,
Guo, T., Fan, Y., Chen, M., Wu, X., Zhang, L., He, T., . . .
Lu, Z. (2020). Cardiovascular implications of fatal
outcomes of patients With Coronavirus DISEASE 2019
(COVID-19). JAMA Cardiology, 5(7), 811.
doi:10.1001/jamacardio.2020.1017
Hancox, J. C., Hasnain, M., Vieweg, W. V., Crouse, E. L.,
& Baranchuk, A. (2013). Azithromycin, cardiovascular
risks, qtc interval prolongation, torsade de pointes, and
regulatory issues: A narrative review based on the study
of case reports. Therapeutic
Hendren, N. S., Drazner, M. H., Bozkurt, B., & Cooper, L.
T. (2020). Description and proposed management of the
COVID-19 Comorbidities: How Do Underlying Hypertensive and Cardiovascular Conditions Affect the Prognosis and Therapies of
COVID-19?
589

acute covid-19 cardiovascular syndrome. Circulation,
141(23), 1903-1914.
Jia, N., Zhang, G., Sun, X., Wang, Y., Zhao, S., Chi, W., . . .
Liu, D. (2021). Influence of angiotensin converting
enzyme inhibitors/angiotensin receptor blockers on the
risk of all‐cause mortality and other clinical outcomes
in patients with CONFIRMED
Lauer, S. A., Grantz, K. H., Bi, Q., Jones, F. K., Zheng, Q.,
Meredith, H. R., . . . Lessler, J. (2020). The incubation
period of Coronavirus DISEASE 2019 (COVID-19)
from publicly REPORTED Confirmed Cases:
Estimation and application. Annals of Internal M
Liu, Y., Huang, F., Xu, J., Yang, P., Qin, Y., Cao, M., . . .
Jiang, C. (2020). Anti-hypertensive angiotensin II
receptor blockers associated to mitigation of disease
severity in elderly COVID-19 Patients.
Maragakis, L. (n.d.).(2021). Coronavirus symptoms:
Frequently asked questions.
https://www.hopkinsmedicine.org/health/conditions-
and-diseases/coronavirus/coronavirus-symptoms-
frequently-asked-questions.
Mayo Clinic Staff. How covid-19 (coronavirus) affects
babies and children. (2021, August 25).
https://www.mayoclinic.org/diseases-
conditions/coronavirus/in-depth/coronavirus-in-
babies-and-children/art-20484405
McGonagle, D., Plein, S., O'Donnell, J. S., Sharif, K., &
Bridgewood, C. (2020). Increased cardiovascular
mortality in African Americans With covid-19. The
Lancet Respiratory Medicine, 8(7), 649-651.
Meng, J., Xiao, G., Zhang, J., He, X., Ou, M., Bi, J., . . .
Zhang, G. (2020). Renin-angiotensin system
INHIBITORS improve the clinical outcomes of
COVID-19 patients with hypertension. Emerging
Microbes & Infections, 9(1), 757-760.
Mueller, A. L., McNamara, M. S., & Sinclair, D. A. (2020).
Why does COVID-19 disproportionately affect older
people? Aging, 12(10), 9959-9981.
Muhamad, S., Ugusman, A., Kumar, J., Skiba, D., Hamid,
A. A., & Aminuddin, A. (2021). COVID-19 and
Hypertension: The what, the why, and the how.
Frontiers in Physiology, 12.
Nishiga, M., Wang, D. W., Han, Y., Lewis, D. B., & Wu, J.
C. (2020). COVID-19 and cardiovascular disease:
From basic mechanisms to clinical perspectives. Nature
Reviews Cardiology, 17(9), 543-558.
Osibogun, A., Balogun, M., Abayomi, A., Idris, J., Kuyinu,
Y., Odukoya, O., . . . Akinroye, K. (2021). Outcomes of
COVID-19 patients with comorbidities in Southwest
nigeria. PLOS ONE, 16(3).
Pettersson, H., Manley, B., & Hernandez, S. (2021,
September 7). Tracking COVID-19'S global spread.
https://www.cnn.com/interactive/2020/health/coronavi
rus-maps-and-cases/.
Preventing the spread of the coronavirus. (2021, August 9).
https://www.health.harvard.edu/diseases-and-
conditions/preventing-the-spread-of-the-coronavirus
Public Health Agency of Canada. (2021, September 07).
Government of Canada.
https://www.canada.ca/en/public-
health/services/diseases/2019-novel-coronavirus-
infection/symptoms.html
Riphagen, S., Gomez, X., Gonzalez-Martinez, C.,
Wilkinson, N., & Theocharis, P. (2020).
Hyperinflammatory shock in children During COVID-
19 pandemic. The Lancet, 395(10237), 1607-1608.
Ruan, Q., Yang, K., Wang, W., Jiang, L., & Song, J. (2020).
Clinical predictors of mortality due To COVID-19
based on an analysis of data of 150 patients from
WUHAN, CHINA. Intensive Care Medicine, 46(5),
846-848. doi:10.1007/s00134-020-05991-x
Sanyaolu, A., Okorie, C., Marinkovic, A., Patidar, R.,
Younis, K., Desai, P., . . . Altaf, M. (2020).
Comorbidity and its impact on patients with covid-19.
SN Comprehensive Clinical Medicine, 2(8), 1069-
1076.
Schiffrin, E., Flack, J., Ito, S., Muntner, P., & Webb, R.
(2020). COVID-19 and hypertension. American
Journal of Hypertension, 33(5), 373-374.
Shi, S., Qin, M., Shen, B., Cai, Y., Liu, T., Yang, F., . . .
Huang, C. (2020). Association of CARDIAC injury
with mortality in hospitalized patients With COVID-19
IN WUHAN, CHINA. JAMA Cardiology, 5(7), 802.
Symptoms of covid-19. (2021, February 22).
https://www.cdc.gov/coronavirus/2019-
ncov/symptoms-testing/symptoms.html
Turner, A. J., Hiscox, J. A., & Hooper, N. M. (2004). Ace2:
From vasopeptidase to sars virus receptor. Trends in
Pharmacological Sciences, 25(6), 291-294.
Wan, Y., Shang, J., Graham, R., Baric, R. S., & Li, F.
(2020). Receptor recognition by the novel
CORONAVIRUS From Wuhan: An analysis based on
Decade-long structural studies of SARS
CORONAVIRUS. Journal of Virology, 94(7).
Wu, Z., & McGoogan, J. M. (2020). Characteristics of and
important lessons from THE Coronavirus DISEASE
2019 (COVID-19) outbreak in China. JAMA, 323(13),
1239.
Yang, G., Tan, Z., Zhou, L., Yang, M., Peng, L., Liu, J., . . .
He, S. (2020). Effects of Angiotensin II receptor
blockers and ACE (ANGIOTENSIN-CONVERTING
Enzyme) Inhibitors on virus Infection, Inflammatory
status, and clinical outcomes in patients With
Yehualashet, A. S., & Belachew, T. F. (2020). ACEIs and
ARBs and their correlation with covid-19: A Review.
Infection and Drug Resistance, Volume 13, 3217-3224.
Zeng, J. H., Liu, Y., Yuan, J., Wang, F., Wu, W., Li, J., . . .
Liu, L. (2020). First case of COVID-19 infection with
FULMINANT Myocarditis COMPLICATION: Case
report and insights.
Zhang, J., Dong, X., Cao, Y., Yuan, Y., Yang, Y., Yan,
Y., . . . Gao, Y. (2020). Clinical characteristics of 140
patients infected with Sars‐cov‐2 IN WUHAN,
CHINA. Allergy, 75(7), 1730-1741.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
590
