
Statistical Analysis of Risk Factors for Generalized Cervical Diseases
Weiwei Wu
a
School of Light Industry, Beijing Technology and Business University, Beijing, China
Keywords: Cervical Cancer, Cervical Intraepithelial Neoplasia (CIN), Logistic Regression, Venezuela.
Abstract: The aim of this study was to investigate the risk factors of generalized cervical diseases, including cervical
cancer and cervical intraepithelial neoplasia (CIN). The data obtained in 2017 in Venezuela on 858 women
were analysed. Logistic regression analyses were conducted to data both before and after balancing
(oversampling) and data with different manipulation for missing values. 5, 4, 6 and 8 out of 9 variables were
screened respectively as important risk factors of cervical diseases after backward selection in four acquired
logistic regression models. Diagnosis of HPV infection, smoking and use of intrauterine device (IUD) were
all screened in four models while number of sexual partners and age were included in three models
separately. Diagnosis of HPV infection, use of IUD and number of sexual partners are positively correlated
with cervical diseases. Smoking was negatively associated with cervical diseases based on the data. More
variables were selected in model after data balancing. Model fitted to data after deleting missing values
performed better than the model fitted to data with imputation. It requires high public attention to prevention
of cervical diseases in Venezuela in terms of HPV infection, use of IUD and number of sex partners.
Logistic regression models in our study are able to estimate patients’ risks of cervical diseases and can be
used as a predictive tool for prevention.
1 INTRODUCTION
1
Cervical cancer occurs in the cells of the cervix
which links the uterus and vagina. It is a common
chronic disease among females with 66% 5-year
survival rate for all people (Cancer.Net 2018). Some
pre-cancerous changes of cervix, including cervical
intraepithelial neoplasia (CIN) and squamous
intraepithelial lesion (SIL), will developed into
malignant tumor if there is lack of proper treatment;
therefore, early detection of pre-cancerous is
necessary for prevention. Cervical cancers and its
pre-cancers are able to be detected by Paps
screening, Thinprep cytologic test (TCT), biopsy
and etc. Similar to human immunodeficiency virus
(HIV) for AIDS, human papilloma virus (HPV) is
considered as a main cause of cervical cancer in vast
investigations and approximately 95% of malignant
cervical lesions are detected with HPV DNA
(Gershenson 20004). The most common way of
HPV transmission and infection is through sexual
behaviours. A large body of clinical trials and
studies proved that HPV vaccine is a highly and
a
https://orcid.org/0000-0001-9816-7703
long-term efficient prevention of HPV infection,
cervical lesions and other relative anogenital warts
disease in both female and male (Drolet 2019).
Cervical cancer is the fourth leading cause of
mortality among cancers in women worldwide
(Sung 2021). It has caused 604,127 new cases and
341,831 deaths in 2020 all around the world.
Specifically, according to researches, estimated 80%
of cervical cancer occurred globally are recorded in
developing countries (Correnti 2011). The incidence
and mortality rate of cervical cancer is extremely
high in Latin America despite the availability of
Paps screening since women with low
socioeconomic status are less accessible to the
screening and less educated with the importance of it
(Villa 2012). In Venezuela, according to the
GLOBOCAN 2018 data, cervical cancer deaths
reached 2,210 or 1.34% of total deaths, which is a
relatively high rate compared to other developed
countries like the United States (Global Cancer
Observatory 2018). Moreover, Venezuela currently
provides nationwide cervical cancer screening
program including Paps for women of 25 to 65 years
old, but HPV vaccine has not been provided and
incorporated into national vaccination program,
396
Wu, W.
Statistical Analysis of Risk Factors for Generalized Cervical Diseases.
DOI: 10.5220/0011371100003438
In Proceedings of the 1st International Conference on Health Big Data and Intelligent Healthcare (ICHIH 2022), pages 396-403
ISBN: 978-989-758-596-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

which represents there is no adequate vaccine
coverage (Bardach 2017). Specifically, there is a
lack of access to prevention, early diagnosis and
even treatment that could be provided (Denny 2012).
Even though cervical cancer has been well
studied and discussed, there are still some problems
exist. To be specific, it is obscure for people to
analyse risk of generalized cervical diseases,
including CIN, cervicitis, cervical cancer, etc. The
occurrence and development of cervical cancer has a
gradual evolutionary process, which can take from
several years to decades. A huge body of evidence
indicates that chronic cervical diseases have
potential to develop into cancer. Therefore, it is
necessary to explore risk factors related to
generalized cervical diseases. Consequently, it is
useful for people to find this disease earlier and have
a better way to prevent disease than it used to be.
Considering the limited investigation of risk
factors and generalized cervical disease, we
investigated the risk factors of cervical diseases by
analysing the data from Hospital Universitario de
Caracas.
2 METHODS
2.1 Data Resource
The dataset was obtained from the UCI Machine
Learning Repository, which is a collection of
domain theories, data generators and databases from
various fields. It was established at UC Irvine in
1987 and was widely used as a public practice
source of machine learning algorithms all around the
world.
This dataset was collected at Hospital
Universitario de Caracas' in Caracas, Venezuela,
Latin-America and the study of the data collection
was published in 2017 (Fernandes 2017). The
dataset contains 36 relative variables and 858
patients, including feature information of historic
medical records, demographic information and
habits. Due to privacy concern, some patients
rejected to some questions during the data
collecting, which leads to some missing values in
this dataset.
2.2 Research Variables
Research variables are showed in Table 1
Dependent variable is ‘Diagnosis of cervical
diseases’ (Dx. Cervical), which is the combination
of diagnosis of cervical cancer and diagnosis of CIN.
It is a categorical variable which represents the
existence of cervical disease of patients. Number ‘1’
represents that a patient has confirmed cervical
diseases while number ‘0’ represents a patient is
cervical healthy.
Nine known variables were considered as
independent variables, which are ‘Age’, ‘Number of
sexual partners’, ‘Age of first sexual intercourse’,
‘Number of pregnancies’, ‘Smokes’, ‘Sexually
transmitted disease infection (STDs)’, ‘Dx. HPV’,
‘Intrauterine Device (IUD)’ and ‘Hormonal
Contraceptives’.
‘Age’ is a numerical variable with the minimum
of 13 and maximum of 84. ‘Number of sexual
partners’ is a numerical variable with the minimum
of 1 and maximum of 28. ‘Age of first sexual
intercourse’ is a numerical variable with the
minimum of 10 and maximum of 32. ‘Number of
pregnancies’ is a numerical variable with the
minimum of 0 and maximum of 11. ‘Smokes’, a
categorical variable, represents whether or not a
patient smoke. Number ‘1’ represents that a patient
smokes or used to smoke while number ‘0’
represents a patient has no smoking history. ‘STDs’,
a categorical variable, represents whether a patient
have sexually transmitted diseases. Number ‘1’
represents that a patient has STDs while number ‘0’
represents a patient does not have STDs. ‘Dx. HPV’,
a categorical variable, represents whether a patient
was diagnosed as HPV infection. Number ‘1’
represents that a patient was diagnosed as HPV
infection while number ‘0’ represents a patient was
not. ‘IUD’, a categorical variable, represents
whether a patient have used intrauterine device – a
device fitted inside uterus for birth control. Number
‘1’ represents that a patient uses or once used IUD
while number ‘0’ represents a patient has never used
IUD. ‘Hormonal Contraceptives’, a categorical
variable, represents whether a patient have used
hormonal medication for contraception. Number ‘1’
represents that a patient uses or once used hormonal
contraceptives while number ‘0’ represents a patient
has never used hormonal contraceptives.
Statistical Analysis of Risk Factors for Generalized Cervical Diseases
397
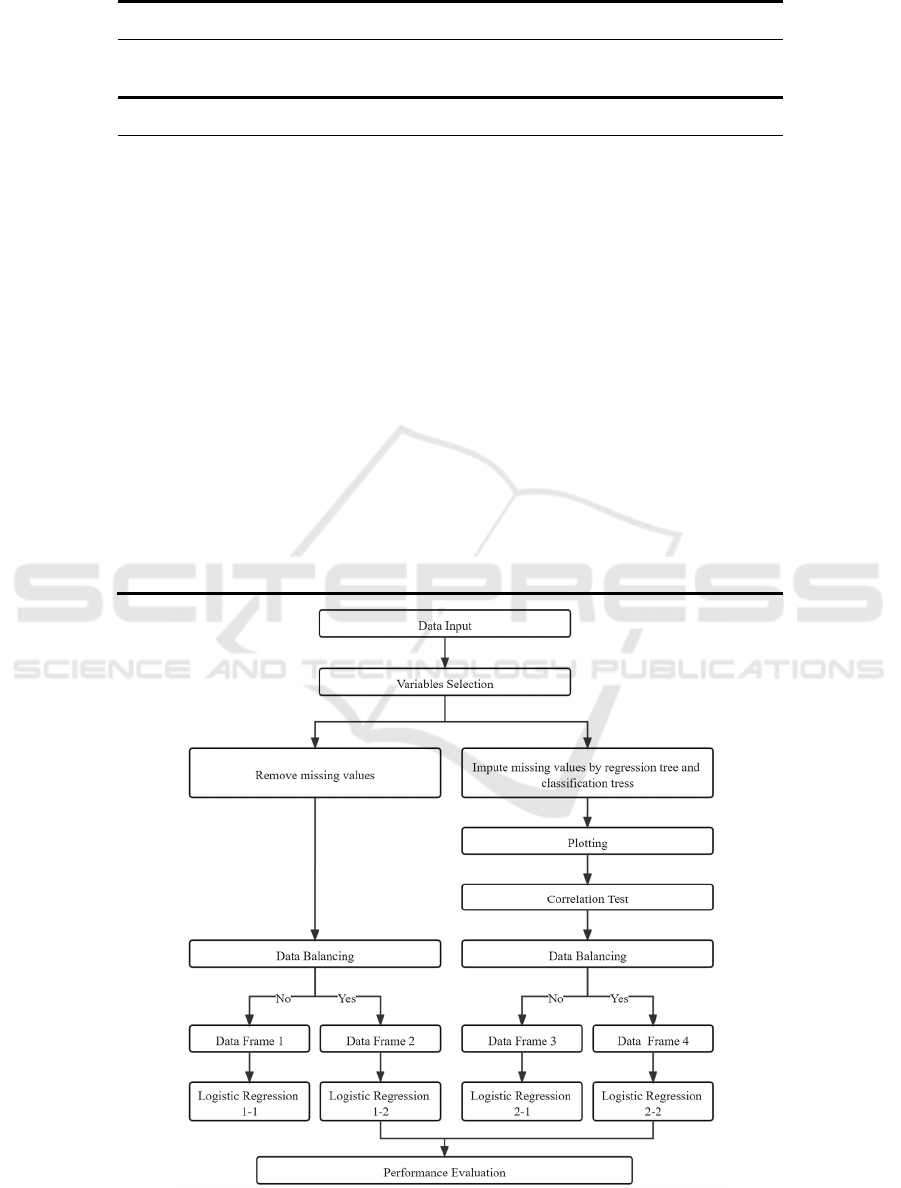
Table 1: Distribution of selected characteristics.
Dependent
Variable
Type Number Percent
(%)
Dx. Cervical Diseases categorical
Yes 27 3.14%
No 831 96.86%
Independent Variable Type Range/
Number
Percent
(%)
Number of sexual partners numerical 1-28
Age of first sexual intercourse numerical 10-32
Number of pregnancies numerical 0-11
Age numerical 13-84
Smokes categorical
Yes 124 14.45%
No 734 85.55%
STDs categorical
Yes 79 9.21%
No 779 90.79%
Dx. HPV categorical
Yes 18 2.19%
No 840 97.81%
Hormonal contraceptives categorical
Yes 565 65.85%
No 293 31.15%
IUD categorical
Yes 83 9.67%
No 775 90.33%
Figure 1: Implementation flow chat.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
398
2.3 Statistical Method
We opted the CSV file from UCI after a
comprehensive searching for well-quality data. The
process and manipulation of the data is presented in
Figure 1.
The CSV file was inputted to R Studio (R
version 4.1.1). The missing values in the dataset
were treated by two kinds of manipulations and two
new data frames were formed. One data frame
removed all missing values while another imputed
missing values by decision tree. Then, visualization
and correlation tests, including Chi-square test and t-
test, were performed to the second data frame. Data
balancing (Oversampling) was conducted to both
two data frames and two extra data frames were
acquired.
Logistic regression (LR) was used to analyse all
four data frames. Logistic regression is a
multivariate method which was invented for binary
outcomes (labelled as ‘0’ and ‘1’). It is used when
studies are concerned with whether an event
happened or not, which is appropriate for models for
decision making and estimate of disease occurrence
and thus is widely used in health and medical
researches. In logistic regression, the logarithm of
the odds ratio (log-odd) was converted into the
probability of outcomes by an algebraic
manipulation (Boateng2019, Glantz 2017, Hosmer
1989). Variables were selected by backward
stepwise method during analysis.
Then, Performance evaluation was conducted to
the results of logistic regression. 75% of samples
was selected as training data and 25% was selected
as testing data at random. Evaluation process was
conducted 100 times for each model to reduce error
and average values was taken as results.
3 RESULTS
3.1 Study Population
858 participants were included in the data, 27
participants were diagnosed as Cervical diseases and
831 participants were cervical healthy in ‘Data
Frame 3’.
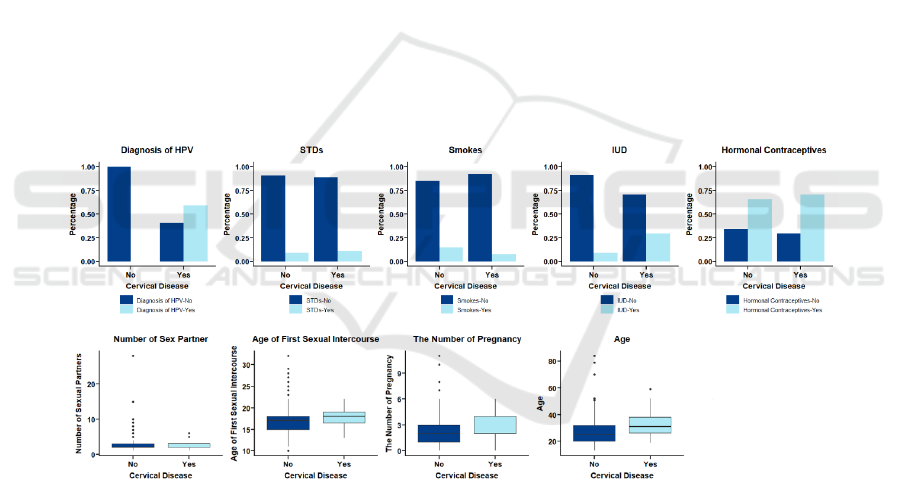
Figure 2: The bar chats and boxplot plots of association between cervical diseases and risk factors
Distribution and ranges of selected variables of
study population were showed in the Table 1. Most
of the women were nonsmokers (85.55%), not
diagnosed with STDs (90.79%), not infected with
HPV (97.81%), and never used IUD (90.33%). More
than half of them took hormonal contraceptives
(65.85%). The mean of age of study population is
26.82. The average number of pregnancies is 2.27.
Average age of first intercourse is 17.00. The mean
of the number of sexual partners of all participants is
2.53.
3.2 EDA
The association between cervical diseases and risk
factors were presents in the Figure 2. In the first bar
chart, a large proportion of people with HPV
infection also have Cervical Diseases, which proved
previous studies about HPV and these maladies. In
the bar chart of IUD, the percentage of IUD use is
greater in cervical diseases diagnosed patients than
in cervical health patients. In bar chart of Smokes,
cervical diseases patients have less proportion of
smokers. For STDs and Hormonal Contraceptives,
Statistical Analysis of Risk Factors for Generalized Cervical Diseases
399

the distribution of cervical diseases is nearly even.
From the box plot, the average age, number of
pregnancies and age of first sexual intercourse are
all slightly greater in confirmed cervical diseases
patients.
Table 2: Correlation tests between cervical diseases and each risk factor.
CHISQUARE TEST
Variable STDs Dx. HPV
Hormonal
Contraceptives
IUD
Smoke
s
x-square <0.01 415.21 0.09 10.46 0.61
df 1 1 1 1 1
p-value 0.99 <0.01 0.78 <0.01 0.44
T-TEST
Variable Age
Number of
sexual
partners
Age of first sexual
intercourse
Number
of
pregnancies
t score 6.19 2.25 3.13 2.25
df 87 23 41 21
p-value <0.01 0.03 <0.01 0.04
3.3 Correlation Tests
Results of correlation tests were presents in the
Table 2.
According to the p-value, ‘Dx HPV’, ‘IUD’,
‘Number of sexual partners’, ‘Age of first sexual
intercourse’, ‘Number of pregnancies’, ‘Age’ are
significant parameters for cervical diseases. ‘STDs’,
‘Hormonal Contraceptives’ and ‘Smokes’ are
insignificant.
3.4 Data Balance
For ‘Data Frame 1’, the data frame that removed all
missing values, after over-sampling, 648 diagnosed
cervical diseases patients and 648 none diagnosed
patients were obtained and formed ‘Data Frame 2’.
For ‘Data Frame 3’, the data frame that imputed
missing values by decision tree, after over-sampling,
831 diagnosed cervical diseases patients and 831
none diagnosed patients were obtained and formed
‘Data Frame 4’.
3.5 Logistic Regression
Four logistic regressions were calculated to predict
the occurrence of cervical diseases. Table 3 shows
the results of four logistic regression models for data
frames with different manipulation. LR 1-1, LR 1-2,
LR2-1, LR 2-2 were fitted to ‘Data Frame 1’, ‘Data
Frame 2’, ‘Data Frame 3’, ‘Data Frame 4’
separately. Data used for LR 1-1 and 2-1 are
imbalanced and for LR 1-2 and LR 2-2 are balanced
by oversampling.
Variables in these four models were all selected
by backward method. 5, 4, 6 and 8 variables were
screen respectively as meaningful risk factors of
cervical diseases in LR 1-1, LR 2-1, LR 1-2 and LR
2-2. The equation of LR 1-1 is
.
.. . ..
log ( ) ln( ) 5.6317 31.7832 2.2513
1
0.5737 0.5929 26.3415
Dx HPV IUD
No of sexual partners No of pregnancies Smokes
P
it P X X
P
XXX
==−+ +
−
+−−
(1)
and Akaike information criterion (AIC) of the model
is 66.13. ‘Age of first sexual intercourse’, ‘Age’,
‘STDs’, ‘Hormonal Contraceptives’ were removed
in LR 1-1. The equation of LR 2-1 is
.
log ( ) ln( ) 5.7685 6.9936 1.3372
1
0.0449 2.3251
D
xHPV IUD
Age Smokes
P
it P X X
P
XX
==−+ +
−
+−
(2)
and AIC of the model is 127.06. ‘Number of sexual
partners’, ‘Age of first sexual intercourse’, ‘Age’,
‘STDs’, ‘Hormonal Contraceptives’ are removed in
LR 2-1. The equation of LR 1-2 is
.
.. .
log ( ) ln( ) 2.2062 47.2360 2.4577
1
0.8233 0.0718 3.4499
38.0888
D
xHPV IUD
No of sexual partners Age STDs
Smokes
P
it P X X
P
XXX
X
==−+ +
−
+−−
−
(3)
and AIC of the model is 595.04. ‘Age of first sexual
intercourse’, ‘Number of sexual partners’,
‘Hormonal Contraceptives’ were removed in LR 1-
2.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
400
Table 3: Logistic regression analyses for cervical diseases.
LR 1-1 AIC = 66.13 LR 2-1 AIC = 127.06
Variable Estimate Pr (>|z|) Variable Estimate Pr (>|z|)
(
Interce
p
t
)
-5.6317 <0.0001
(
Interce
p
t
)
-5.7685 <0.0001
Number of sexual partners 0.5717 0.0659 Age 0.0449 0.1062
Number of pregnancies -0.5929 0.1771 Smokes -2.3251 0.0916
Smokes -26.3415 0.9912 IUD 1.3372 0.0468
IUD 2.2513 0.0320 Dx. HPV 6.9936 <0.0001
Dx. HPV 31.7832 0.9894
LR 1-2 AIC = 595.04 LR 2-2 AIC = 1182.8
Variable Estimate Pr (>|z|) Variable Estimate Pr (>|z|)
(
Interce
p
t
)
-2.2062 <0.0001
(
Interce
p
t
)
-0.1264 0.8409
A
g
e -0.0718 0.0002 A
g
e 0.0770 <0.0001
Number of sexual partners 0.8233 <0.0001 Number of sexual
p
artners 0.3330 <0.0001
Smokes -38.0888 0.9949 A
g
e of first sexual intercourse -0.1895 <0.0001
IUD 2.4577 <0.0001 Number of pregnancies -0.3767 <0.0001
STDs -3.4499 0.0014 Smokes -6.8497 <0.0001
Dx. HPV 47.2360 0.9937 Hormonal Contraceptives 0.2313 0.1475
IUD 1.1140 <0.0001
Dx. HPV 9.7419 <0.0001
Table 4: The performance of two logistic regression for cervical diseases.
Model Sensitivity (%) Specificity (%) Accuracy (%) Precision (%) AUC*(%)
LR 1-2 89.18(3.58) 92.79(2.27) 90.94(1.96) 92.66(2.23) 96.74(0.70)
LR 2-2 73.31
(
2.25
)
90.15
(
2.35
)
81.73
(
1.56
)
88.15
(
2.83
)
90.71
(
0.10
)
The equation of LR 2-2 is
.
.. . .
.. . .int
..
log ( ) ln( ) 0.1264 9.7419 1.1140
1
0.3330 0.2313
0.0770 0.1895
0.3767 6.8497
D
xHPV IUD
No of sexual partners Hormonal Contraceptives
Age Age of first sexual ercourse
No of pregnancies Smokes
P
it P X X
P
XX
XX
XX
==−+ +
−
++
+−
−−
(4)
and AIC of the model is 1182.8. ‘STDs’ were
removed in LR 2-2. Partial variables in models are
not significant (Pr > 0.05).
‘Diagnosis of HPV infection’, ‘Smokes’, ‘IUD’
were all screen as important risk factors in these four
models. Among them, ‘Diagnosis of HPV’ and
‘Smokes’ are highly associate with cervical diseases.
‘Smokes’ are negatively correlated with cervical
diseases. ‘Number of sexual partners’ and ‘Age’
were included in three models separately.
After an inverse operation of logistic transaction,
the value of P, which represents the probability of
occurrence of cervical diseases, was acquired. A
value of P that is closer to 0 was regarded as less
likely of cervical diseases, while that is closer to 1
was regarded as more likely of cervical diseases.
Comparison of LR 1-1 and LR 1-2 and
comparison of LR 2-1 and LR2-2 shows that more
variables were included in model after data
balancing. Comparison of models with different
manipulation, LR 1-2 and LR 2-2, shows that the
correlation of ‘Diagnosis of HPV infection’ and
cervical diseases are lower in model for imputed
data.
3.6 Performance Evaluation of Models
Results of the performance evaluation of LR 1-2 and
LR 2-2 are presented in Table.4.
For LR 1-2, 89.13% sensitivity, 92.79%
specificity, 90.94% accuracy, 92.66% precision were
observed. AUC of LR 1-2 is 96.74%. For LR 2-2,
73.31% sensitivity, 90.15% specificity, 81.73%
accuracy, 88.15% precision were observed. AUC of
LR 2-2 is 90.71%.
4 DISCUSSION
According to the results, HPV infection, use of IUD
and number of sex partners need high attention for
prevention of cervical diseases. Our results also
support the conclusion of previous studies that there
is a consistent correlation between HPV and
cervical. From the result of logistic regression, it is
apparent that there exists a negative correlation
between Smokes and cervical diseases. However,
according to previous study, it is apparent that
smokers have high risk of developing cervical
Statistical Analysis of Risk Factors for Generalized Cervical Diseases
401

cancer in US (Sierra-Torres 2003). To be specific,
there is a positive relationship between smoking and
diagnosis of cervical disease. The difference is
probably due to the varied situation of each country
that Venezuela is a low-income developing country,
but the United States is a developed country.
Specifically, not every woman in Venezuela may
have access to smoking due to the financial issue
and the high percent of excise tax in cigarette.
Compared to Venezuela, people in the U.S may have
easier access to smoking no matter what income
they have received. Moreover, Venezuela execute
more extensive and stricter ban on smoking and
enforce more bans on advertising than the U.S,
which may result in lower rate of smoking among
women (Venezuela 2019, United States Tobacco
Atlas 2021). Therefore, it can possibly explain the
negative correlation in Venezuela and the positive
correlation in the U.S. Further evidence and
comprehensive researches are needed to prove this
inference.
Different from previous studies that consider the
effects of risk factors on CIN or cervical cancer
separately, we focused on generalized cervical
diseases including both CIN and cervical cancers.
The combination of CIN and cervical cancer might
contribute to the early control and prevention of
generalized cervical diseases. We also compared
different models that were fitted to data both before
and after balancing (oversampling) and data with
different manipulation of missing values.
Nevertheless, our studies still have some
limitations to be considered. Due to the limitation of
our dataset, we only consider the diagnosis of CIN
and diagnosis of cervical cancer. If there is access to
data including more other cervical diseases, like
cervical polyp, cervical cyst etc., models are able to
be further improved and optimized. Moreover, since
our dataset was collected from Venezuela, it needs
to be cautious when generalizing the results and
conclusions to other regions. Venezuela is a low-
income country, so the data may only represent the
conditions in low-income country rather than other
developed or developing countries. In addition,
because of the privacy concerns of some women that
they did not share complete information in data
collection, biases were introduced into analyses.
Lastly, risk factors were screened in our study by
using logistic regression, the results can be further
confirmed by using random forest subsequently.
5 CONCLUSIONS
‘Diagnosis of HPV infection’, ‘IUD’, ‘Number of
sexual partners’ and ‘Age’ are risk factors of
cervical cancer in Venezuela. Logistic regression
models in our study can estimate patients’ risks of
cervical diseases and can be used as a tool for
prevention. In the future, we will employ the
technique of random forest to analyse statistical
correlation between cervical diseases and all
independent variables discussed in this paper and
make comparison on these two statistical methods.
REFERENCES
Bardach, A. E., Garay, O. U., Calderón, M., Pichón-
Riviére, A., Augustovski, F., Martí, S. G., Cortiñas, P.,
Gonzalez, M., Naranjo, L. T., Gomez, J. A., &
Caporale, J. E. (2017). Health Economic Evaluation of
human papillomavirus vaccines in women from
Venezuela by a lifetime markov cohort model. J. BMC
Public Health, 17, 152.
Boateng, E. Y., Abaye, D. A. (2019). A Review of the
Logistic Regression Model with Emphasis on Medical
Research. J. Journal of Data Analysis and Information
Processing. 07, 190–207.
Cancer.Net. - Cervical cancer. (2021). Retrieved from
https://www.cancer.net/cancer-types/cervical-
cancer/statistic.
Correnti, M., Medina, F., Cavazza, M. E., Rennola, A.,
Ávila, M., & Fernándes, A. (2011). Human
papillomavirus (HPV) type distribution in cervical
carcinoma, low-grade, and high-grade squamous
intraepithelial lesions in Venezuelan women. J.
Gynecologic Oncology. 121, 527–531.
Denny, L. (2012). Cervical Cancer: Prevention and
Treatment. Retrieved from
https://www.discoverymedicine.com/Lynette-
Denny/2012/08/27/cervical-cancer-prevention-and-
treatment/.
Drolet, M., Bénard, É., Pérez, N., Brisson, M., Ali, H.,
Boily, M.-C., Baldo, V., Brassard, P., Brotherton, J.
M., Callander, D., Checchi, M., Chow, E. P., Cocchio,
S., Dalianis, T., Deeks, S. L., Dehlendorff, C.,
Donovan, B., Fairley, C. K., Flagg, E. W., … Yu, B.
N. (2019). Population-level impact and herd effects
following the introduction of human papillomavirus
vaccination programmes: Updated systematic review
and meta-analysis. J. The Lancet. 394, 497–509.
Fernandes, K., Cardoso, J. S., Fernandes, J. (2017).
Transfer learning with partial observability applied to
cervical cancer screening. J. Pattern Recognition and
Image Analysis. 10255, 243–250.
Gershenson, D. M., McGuire, W. P., Gore, M., Quinn, M.
A., & Thomas, G., 2004. Gynecologic cancer:
Controversies in management. Elsevier Ltd.
Philadelphia.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
402

Glantz, S., Slinker, B., Neilands, B., 2017. Primer of
Applied Regression and Analysis of Variance.
McGraw Hill. 3
rd
edition.
Global Cancer Observatory. (2018). Retrieved from
https://gco.iarc.fr/.
Hosmer, D. W., Lemeshow, S., 1989. Applied logistic
regression. New York: Wiley.
Sierra-Torres, C. H., Tyring, S. K., Au, W. W. (2003).
Risk contribution of sexual behavior and cigarette
smoking to cervical neoplasia. J. International Journal
of Gynecological Cancer. 13, 617–625.
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M.,
Soerjomataram, I., Jemal, A., & Bray, F. (2021).
Global cancer statistics 2020: Globocan estimates of
incidence and mortality worldwide for 36 cancers in
185 countries. J. CA: A Cancer Journal for Clinicians.
71, 209–249.
United States. Tobacco Atlas. (2021). Retrieved from
https://tobaccoatlas.org/country/usa/.
Venezuela. Tobacco Atlas. (2021). Retrieved, from
https://tobaccoatlas.org/country/venezuela/.
Villa, L. L. (2012). Cervical cancer in Latin America and
the Caribbean: the problem and the way to solutions. J.
Cancer Epidemiol Biomarkers Prev. 21, 1409–1413.
Statistical Analysis of Risk Factors for Generalized Cervical Diseases
403
