
Efficacy, Safety and Immune Reactions Associated with COVID-19
Vaccines
Yuanlin Guo
a
Overseas Education College, Nanjing Tech University, Nanjing, Jiangsu, 210036, China
Keywords: COVID-19, SARS-Cov-2, Vaccines, Side Effects, Safety.
Abstract: COVID-19 is a disease caused by the SARS-CoV-2 virus that has spread into an worldwide pandemic. Quick
efforts into developing vaccines against SARS-CoV-2 took place, using both existing technologies or ones
newly released to the public. Side effects observed upon administration of previous vaccines or the unknown
associated with new vaccines have caused concern in large cohorts of population regarding their safety. In
this paper, we look with detail into the ingredients of existing COVID-19 vaccines and their side effects,
hoping to clear any concerns and claims that rose out of proportion. To obtain the presented data, we searched
and analyzed online reports and databases from vaccine developers and clinicians alike, as well as research
articles that covered the potential side effects of specific vaccine ingredients. Our research indicates that
existing vaccines against COVID-19 are safe for most of the population, with very small percentages of severe
side effects associated with it. The side effects of the vaccines largely outweigh the potential complications
arising from SARS-CoV-2 infection. Long term clinical trials for safety and efficacy are currently underway
to monitor any potential long term side effects.
1 INTRODUCTION
COVID-19 is a disease caused by the SARS-CoV-2
virus, that affects the respiratory system and a
multitude of other organs. It has a mortality rate of
around 2%, having caused about 4 million deaths
worldwide, and 200 million infections as of July
2021. SARS-CoV-2 virus has a surface spike protein
S that binds to the angiotensin converting enzyme II
(ACE2) in human cells, allowing the virus particle to
fuse with the host cell membrane and enter via
endocytosis. Currently, there is no approved
treatment that effectively reverses the course of
disease. As such, vaccines became a strong bet in the
fight against SARS-CoV-2. Several countries have
rushed to manufacture vaccines against the virus in
record times, starting in 2020 and as of July 2021, 20
vaccines against COVID-19 were approved
worldwide in different countries and 900 million
people have been vaccinated worldwide. (Vaccine
Tracker.2021)
With the development of new vaccines—some
with technology never used before in clinical
settings—several concerns about its safety profile
a
https://orcid.org/0000-0001-9721-0298
were raised. These concerns arise at times from
unfounded or false information from less reliable
sources, and leads to many individuals not taking the
vaccine, potentially increasing the spread of the
pandemic. In this article, we explored the possible
side effects and allergic reactions based on single
vaccine ingredients as well as complete vaccine
formulations. We explore and compare the current
vaccines against COVID-19, safety data, and
potential for immune reactions based on their
ingredients. These vaccines are described on Table 1,
showing the technology used for development and
their ingredients. In the following section, we
describe the different types of vaccines that are
developed against SARS-CoV-2.
2 COVID-19 VACCINE TYPES
2.1 Inactivated Virus Vaccines
Inactivated vaccines are developed by growing the
virus in a controlled laboratory environment using a
suitable cell culture as a host, and then deactivating it
314
Guo, Y.
Efficacy, Safety and Immune Reactions Associated with COVID-19 Vaccines.
DOI: 10.5220/0011368800003438
In Proceedings of the 1st International Conference on Health Big Data and Intelligent Healthcare (ICHIH 2022), pages 314-324
ISBN: 978-989-758-596-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
using a variety of biological, chemical, or physical
methods. The inactivated virus offers a strong safety
profile but it will still be recognized by the immune
system, which makes antibodies against it. (Sanders,
Koldijk, and Schuitemaker 2014) Inactivated virus
vaccines have been used for a long time and other
types include vaccines against polio, hepatitis A,
rabies, influenza, tick-borne encephalitis, injected
typhoid, cholera, plague, pertussis, among others. The
viral material in inactivated vaccines does not
replicate, making them virtually impossible to cause
pathological effects due to infection.
2.2 Adenovirus Vector
Adenoviruses are originally nonenveloped double-
stranded DNA viruses. They can be modified to
deliver genetic material in human cells and as such
have been used for decades in gene therapy research.
Currently, there are several undergoing clinical or
preclinical trials using adenoviruses for vaccines
against different diseases and pathogens such as HIV,
Ebola, influenza, rabies, dengue, plasmodium
falciparum, mycobacterium tuberculosis. For
COVID-19 vaccines, these viruses were modified to
deliver DNA encoding the SARS-CoV-2 Spike
protein.
The adenovirus used in the vaccine lacks
replication because some genes necessary for
replication have been removed. Following
vaccination, the adenoviral vector enters the cell and
releases its genes, which are transported to the
nucleus, where the cellular machinery transcribes
messenger ribonucleic acid (mRNA) and translates it
into protein. Once released outside the cell, the
protein induces an immune response to generate
antibodies against it. (TATSIS, ERTL 2004)
2.3 mRNA Vaccines
mRNA molecules need to reach the cytoplasm or
endoplasmic reticulum ribosomes and be translated
into proteins, which is the concept of mRNA
vaccines. mRNA molecules can be encapsulated in
lipid nanoparticle (LNP) carriers to penetrate tissues
to facilitate the transfer of genetic information in host
cells, thereby initiating the synthesis of antigenic
proteins. (JACKSON, KESTER, CASIMIRO 2020)
In these vaccines, LNPs are used to protect RNA
against degradation, since this type of biomolecule is
more sensitive to degradation than DNA or proteins.
mRNA vaccines are new vaccine types that were not
tested before COVID-19. An advantage of these
vaccines when compared to adenovirus vector ones,
is that they can be produced in large scale more
quickly and at lower costs, since RNA encapsulation
in lipid nanoparticles is a more straight-forward
process. (PARDI, HOGAN, PORTER 2018)
2.4 Subunit Vaccines
Subunit vaccines are based on the direct delivery of
proteins, or parts of proteins, that mimic the ones in
SARS-CoV-2 and trigger an immune response to
these antigens. These vaccines are designed so that
their antigens lack pathogen-associated molecular
patterns (PAMPs) required by the host immune
system to recognize the antigen, reducing the
immunogenic potential of this vaccine approach.
(NIH 2019)
A potential problem with subunit vaccines is the
antigenic denaturation can occur, which can lead to
the production of different antibodies that do not
recognize the pathogen. This could potentially lead to
the protein binding to a different antibody than to a
specific antigen against the pathogen. Because the
antigens themselves normally only elicit a weak
immune response, when making this vaccine, non-
immunogenic materials are usually incorporated into
the vaccine formulation to improve the immune
response and enhance the efficacy of the vaccine.
These materials are called adjuvants.
Currently, a large number of protein subunit
vaccine candidates for SARS-CoV-2 are in human
clinical trials, with 2 on the market (see Table 1).
These candidates use a different immunogen, either
the whole Spike protein or a different form of its
receptor binding domain (RBD). RBD is the S protein
region that mediates the binding of the virus to the
ACE2 receptor of the target host cell.
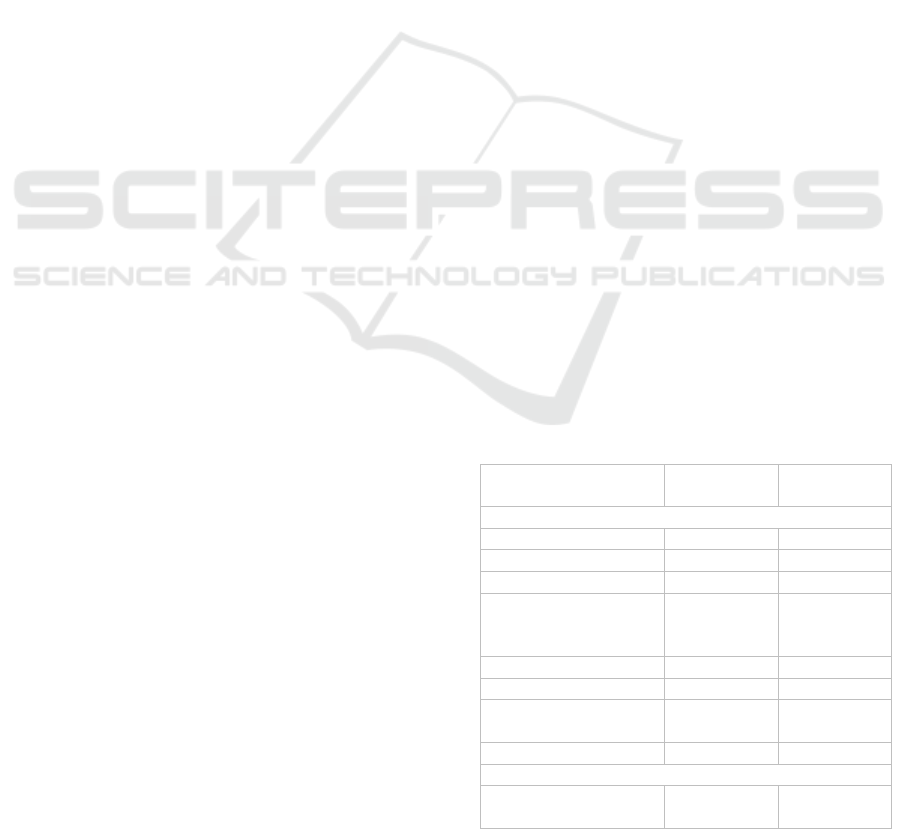
Table 1: Approved covid-19 vaccines (as of July).
Vaccine name
Country of
origin
Trial Start
Date
Inactivated virus vaccines
CoronaVac China 2020-09-16
BBIBP-CorV China 2020-4-29
WIBP-CorV China 2020-04-11
Minhai Biotechnology
Co: SARS-CoV-2
Vaccine
China 2020-10-07
Covaxin India 2020-9-8
KoviVac Russia 2020-9-21
QazVac
Republic of
Kazakhstan
2020-8-28
COVIran Barekat Iran 2021-3-13
Adenovirus vector
Ad26.COV2.S
United
States
2020-6-30
Efficacy, Safety and Immune Reactions Associated with COVID-19 Vaccines
315

AZD1222
United
Kin
g
dom
2020-3-19
Ad5-nCoV
China 2020-9-26
Sputnik V COVID-19
vaccine
Russia 2020-6-18
Sputnik Light Russia 2021-1-19
Covishiel
d
India 2020-08-15
mRNA vaccines
mRNA-BNT162b2
United
States
2021-3-25
mRNA-1273
United
States
2020-2-25
Takeda: TA
K
-919 Japan 2020-11-21
Subunit vaccines
ZF2001 China 2020-08-16
E
p
iVacCorona Russia 2020-8-26
CIGB-66 Cuba 2020-12-7
3 SAFETY DATA
Initial clinical trials for the vaccines excluded
volunteers with history of allergic reactions, diabetes,
cancer, among other pathologies. Despite that, several
volunteers suffered adverse reactions upon vaccine
administration that resulted in temporary disability or
even death, although in very low numbers. This
prompted us to look at vaccine ingredients with a
potential to cause adverse effects.
In the sections below, we describe the safety and
efficacy data for some extensive used vaccines.
4 INACTIVATED VIRUS
VACCINES
4.1 CoronaVac
CoronaVac is an inactivated vaccine candidate
against COVID-19, From July 21 to December 16,
2020, Brazil recruited a total of 12,396 volunteers to
receive CoronaVac and placebo in a phase 3 clinical
trial. (PALACIOS, BATISTA, ALBUQUERQUE
2021) The most common adverse reactions in the
vaccine group were pain at the injection site (60.3%),
swelling (5.8%) and itching (4.2%); the most
common systemic adverse reactions were headache
(34.3%), fatigue (16.0%) and muscle pain (11.7%).
Among the 4,953 people, 14 days after the second
vaccination, 85 cases of symptomatic infection were
detected; among 4870 people in the placebo group,
168 cases of symptomatic infection were observed.
Therefore, the effective rate of Coronavac was
determined to be 50.7%. Fourteen days after
vaccination, the effective rate of preventing cases
where minimal medical intervention was required is
83.7%, and the effective rate of preventing moderate
to severe disease was determined to be 100%. All
severe cases (6 cases) are in the placebo group. There
are mainly three new coronavirus strains in Brazil,
namely B.1.1.28, P.1 and P.2. The first one is wild
type, and the latter two are variants. The main variant
of the institute in the region is P.2 The neutralizing
activity ratios of 45 volunteers' serum to B.1.1.28, P.1
and P.2 were 32 (71.1%) and 31 (68.9%),
respectively. In 36 people (80.0%), the study found
that the sera of the vaccinators had a consistent
neutralizing effect on all these variants. Overall,
Coronavac seems to be well tolerated.
4.2 BBIBP-CorV
BBIBP-CorV is a vaccine based on inactivated viral
particles. This candidate vaccine was developed by
Sinopharm Wuhan Institute of Biological Products
and the China Center for Disease Control and
Prevention. Two different SARS-CoV-2 strains,
WIV04 and HB02, were isolated from a patient at the
Jinyintan Hospital in Wuhan, China.
A large phase 3 clinical trial was conducted in
Asia, covering more than a dozen countries including
the United Arab Emirates (23.9%), India (14.0%),
Bangladesh (10.4%), China (9.8%), Pakistan (9.1%),
and others. The average age of volunteers was 36.1
years old, 84.4% were males, and 98.4% were 59
years old and below. Of the total 40,411 volunteers,
13,066 volunteers in WIV04 group, 13,086
volunteers in HB02 group, and 13,071 volunteers in
placebo group completed two injections. Within 1
week after vaccination, 44.2% (WIV04 group),
41.7% (HB02 group), 46.5% (placebo group) had
adverse reactions in each group, the most common of
which was injection site pain (24.3%, 19.4%, 27.9%
respectively) and headache (12.9%, 13.1%, 12.6%
respectively). As of December 20, 2020, after the
volunteers received the first injection (vaccine or
placebo), there were a total of 962 suspected cases.
After confirmation, there were 255 confirmed cases.
Among them, outside the monitoring period (the first
injection). In the 35th day afterwards, there were 113
confirmed cases, and within the monitoring period
(14 days after the second injection), there were 142
confirmed cases overall. (AL KAABI, ZHANG, XIA
2021) Among these 142 cases, 95 cases were in the
placebo group, 26 cases were in the WIV04 group,
and 21 cases were in the HB02 group. The calculated
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
316

effective rate of the WIV04 vaccine is 72.8%, and the
effective rate of the HB02 vaccine is 78.1%.
4.3 WIBP-CorV
WIBP-CorV is another inactivated virus COVID-19
vaccine also developed by Sinopharm, for which the
viral particles were obtained from a different SARS-
CoV-2 source. JAMA published the phase III clinical
interim results of both BBIBP-CorV and WIBP-CorV
at the same time. (AL KAABI, ZHANG, XIA 2021)
Peer-reviewed results show WIBP-CorV is 72.8%
effective against symptomatic cases and 100%
against severe cases. The safety profile of the vaccine
is similar to BBIPP-CorV.
4.4 COVAXIN
COVAXIN, also known as BBV152, is a COVID-19
vaccine developed by Bharat Biotech in India in
collaboration with the Indian Medical Research
Council (ICMR), part of the National Institute of
Virology (NIV). The vaccine is manufactured using
viral particles that were grown on Vero cells and
subsequently inactivated. (Bharat Biotech 2021)
Phase 3 clinical trials of Covaxin were conducted
in different locations across India. 24,419 individuals
received two doses of BBV152 (n = 12,221) or
placebo (n = 12,198). There were 24 infections in the
vaccine group and 106 infections in the placebo
group, reported at least 2 weeks after the second dose.
The overall vaccine efficacy was 77.8%. The two-
dose vaccine was also 93.4% effective in those with
severe disease and 63% protective in those with
asymptomatic infection. The preprint reveals that in
those 60 years and older, the vaccine was 67.8%
effective, while in younger people, the effectivity was
determined to be 79.4%. Adverse events were below
1% in both groups, with the most frequent being
headache, followed by fever, fatigue and myalgia.
5 ADENOVIRUS VECTOR
5.1 Ad26.COV2.S (Janssen)
The Janssen COVID-19 vaccine is a recombinant,
replication-incompetent adenovirus serotype 26
(Ad26) vector vaccine that has been modified to
contain the gene for making a protein found on
SARS-CoV-2. Vaccination with the Janssen COVID-
19 vaccine consists of a single 0.6 mL dose
containing 5 × 10
10
viral particles, administered
intramuscularly. (LIVINGSTON, MALANI,
CREECH 2021)
In the phase 3 clinical trial “ENSEMBLE”
(clinicaltrials.gov accession number NCT04505722),
the per-protocol population included 19,630 SARS-
CoV-2–negative participants who received
Ad26.COV2.S and 19,691 who received placebo.
Three deaths reports occurred in the vaccine group
but no case was related to covid-19 and not attributed
to the vaccine, and 16 in the placebo group, 5 of
which were determined to be caused to COVID-19.
(SADOFF, GRAY, VANDEBOSCH 2021)
Vaccine recipients experienced a variety of
adverse symptoms. However, most were mild to
moderate and resolved 1–2 days after vaccination.
These are more common in people aged 18-59 than in
people over 60. Severe local or systemic reactogenic
symptoms were more common among vaccine
recipients (2.2%) than placebo recipients (0.7%). The
FDA identified injection site pain, hypersensitivity,
and systemic reactogenicity as three adverse events
associated with vaccination. No specific security
issues were found after analysis.
Out of more than 6.8 million doses administered,
embolic and thrombotic events were observed,
including six cases of a rare and severe type of blood
clot in individuals following administration. (CDC
2021) (FDA 2021) Cerebral venous sinus thrombosis
(CVST) was observed in combination with low levels
of blood platelets (thrombocytopenia) in these cases.
Medical and scientific teams at the FDA and CDC
examined available data and determined these events
were thrombosis-thrombocytopenia syndrome (TTS).
After a brief suspension, and following a safety
review by the CDC’s Advisory Committee on
Immunization Practices and the FDA have
determined that use of Janssen vaccine would resume
in the United States, effective April 23, 2021.
Ad26.COV2.S protected against moderate to
severe–critical COVID-19 with onset at least 2 weeks
after administration, where 116 cases in the vaccine
group vs. 348 in the placebo group were observed,
resulting in an efficacy of 66.9%. It was more
effective against severe Covid-19, with an incidence
of 76.7% at least 14 days after administration and
85.4% after 28 days .
Rare cases of the neurological disorder Guillain-
Barré syndrome have also been reported following
vaccination with the Janssen COVID-19 vaccine.
Although the chances of developing the condition are
low, they appear to be three to five times higher
among recipients of the Johnson & Johnson vaccine
than among the general population in the United
Efficacy, Safety and Immune Reactions Associated with COVID-19 Vaccines
317

States, although a causal relationship has not been yet
established. (VOYSEY, CLEMENS, MADHI 2021)
A single dose of Ad26.COV2.S protected against
symptomatic COVID-19 and asymptomatic SARS-
CoV-2 infection and was effective against severe–
critical disease, including hospitalization and death.
5.2 AZD1222 Vaxzevria
(Oxford-AstraZeneca)
The Oxford–AstraZeneca COVID-19 vaccine is a
replication-deficient Simian adenovirus vector.
Between April and November 2020, 23,848
participants were enrolled and 11,636 participants
(7,548 in the UK, 4,088 in Brazil) were included in
the primary efficacy analysis. (SCHULTZ,
SØRVOLL, MICHELSEN 2021) In participants who
received two standard doses, vaccine efficacy was
70.4%. From 21 days after the first dose, there were
ten cases hospitalized for COVID-19, all of which in
the placebo group; two were classified as severe
COVID-19, including one death. 175 severe adverse
events occurred in 168 participants, 84 events in the
ChAdOx1 nCoV-19 group and 91 in the control
group.
An article published on The New England Journal
of Medicine reported five cases of severe venous
thromboembolism in unusual sites and concomitant
thrombocytopenia that occurred 7 to 10 days after
vaccination with AZD1222. (EUROPEAN
MEDICINES AGENCY 2021) Four of the patients
had severe cerebral venous thrombosis with
intracranial hemorrhage, and the outcome for three of
them was fatal. Thrombotic thrombocytopenic
purpura and immune thrombocytopenic purpura are
not suspected because there was no hemolysis and the
platelet transfusion response was normal. What all
five patients have in common is high levels of PF4-
polyanion complex antibodies. The researchers
suggest that these cases represent vaccine-related
variants of spontaneous heparin-induced
thrombocytopenia, which they call vaccine-induced
immune thrombotic thrombocytopenia (VITT).
After a period of suspension, AZD1222
Vaxzevria was authorized in the EU to prevent
COVID-19 as the benefits of Vaxzevria outweigh its
risks in adults of all age groups from adverse events
including thrombosis in combination with TTS. The
frequency of TTS events was observed to be very rare
based on current reporting.
(LOGUNOV,
DOLZHIKOVA, SHCHEBLYAKOV 2021)
5.3 Sputnik V (Gam-COVID-Vac)
COVID-19 vaccine
The Gam-COVID-Vac vaccine, also known as
Sputnik V, was developed by a government-
sponsored team of cell microbiologists at the
Gamalaya Institute for Epidemiology and
Microbiology in Russia. Gam-COVID-Vac is based
on two human adenoviruses that contain a gene that
encodes the full-length spike protein S of SARS-
CoV-2 to stimulate an immune response.
In the Phase 3 trial, 21,977 adults were randomly
assigned to the vaccine group (n = 16,501) or the
placebo group (n = 5,476). From 21 days after the first
dose of vaccine, the day on which dose 2 was
administered, 16 (0.1%) participants in the vaccine
group and 62 (1,3%) in the placebo group were
confirmed to have COVID-19. Based on the second
interim analysis of data obtained 28 days after
administering the first dose, 7 days after the second
dose, vaccine efficacy was determined to be over 95%
42 days after the first dose, no life-threatening
adverse events were observed. (LOGUNOV,
DOLZHIKOVA, SHCHEBLYAKOV 2021)
The vaccine induced robust humoral and cellular
immune responses among individuals of all ages,
indicating a strong potential to prevent severe disease
in individuals over the age of 60.
An article published by Lancet claimed
discrepancies and substandard reporting of data on
the Sputnik V phase 3 trial. According to the trial
data, 35,963 individuals were screened and 21,977
individuals were randomized, but there disclosure as
to why 13,986 participants were excluded. The
authors also claim inconsistencies in the numerical
data related to vaccine efficacy. (BUCCI,
BERKHOF, GILLIBERT 2021)
6 mRNA VACCINE
6.1 Pfizer–BioNTech COVID-19
Vaccine (BNT162b2)
The Pfizer-BioNTech COVID-19 vaccine is
developed by the German company BioNTech, a
novel type based on encapsulated mRNA, that
encodes for the full SARS-CoV-2 Spike protein S.
In their press release issued on November 18
2020, Pfizer and BioNTech stated that the final
interim analysis data was 95% effective against
COVID-19 within a week of the candidate receiving
both inoculations. (Pfizer 2020) This data is based on
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
318

the assessment of 43,448 participants, 170 of whom
developed COVID-19 during the assessment period.
Of these, 162 were in the placebo group and 8 were
in the vaccine candidate group. Vaccine efficacy is
consistent across age, gender, race, and ethnic
demographics. In addition, the efficacy observed in
the inoculated individuals over the age of 65 was over
94%. With regard to the safety of BNT162b2, no
serious safety issues have been reported. The more
frequent event compared to the placebo group is
fatigue. Based on these results, Pfizer and BioNTech
became the first company to submit a request for a
vaccine against SARS-CoV-2 to the FDA.
One ingredient found in mRNA vaccines of
particular concern for allergic reactions is a chemical
called polyethylene glycol (PEG). In mRNA
vaccines, PEG is used to coat mRNA molecules and
support their entry into cells. Since PEG is generally
not a component of previous vaccines, there is limited
information on its allergic effects.
An article on the journal Pediatrics reported 7
cases of clinical myocarditis or myopericarditis that
developed in 14- to 19-year-old males within 4 days
of receiving the second dose of the Pfizer-BioNTech
COVID-19 vaccine with no evidence of acute SARS-
CoV-2 infection. (MARSHALL, FERGUSON,
LEWIS 2021) These individuals developed chest pain
within 4 days after the second shot of the vaccine, and
developed fever before and after the onset. Further
studies need to be conducted to determine causation.
6.2 Moderna COVID-19 Vaccine
(mRNA-1273)
mRNA-1273 is a vaccine developed by the company
Moderna that uses mRNA that is translated into the
SARS-CoV-2 Spike protein to elicit an immune
response.
On November 18th 2020, Moderna published
their vaccine Phase 3 clinical study. 24,907 (82.1%)
participants who were considered to be at
occupational risk for acquiring the SARS-CoV-2
infection, of whom around 25% were healthcare
workers. This preliminary analysis was performed 14
days after the second vaccination and included 95
confirmed COVID-19 cases among the participants,
90 of which belonged to the group receiving placebo
and 5 cases belonged to the group receiving the
vaccine, resulting in a calculated efficacy of the
candidate vaccine of 94.5%. Furthermore, of the 11
cases that were considered severe, none were in the
vaccinated group, which indicates that mRNA-1273
may also prevent severe COVID-19.
As for the safety of mRNA-1273, mainly mild to
moderate events have been reported. The most
frequent severe adverse effects were soreness at the
injection site after the first dose (2.7%), and myalgia
(8.9%), arthralgia (5.2%), fatigue (9.7%). Overall,
these effects were described as short-lived. (Moderna
2020)
7 SUBUNIT VACCINES
7.1 ZF2001
ZF2001 is a protein subunit COVID-19 vaccine
developed by Anhui Zhifei Longcom. It uses a
traditional alum-based adjuvant with a long safety
profile.
50 participants in phase 1 trial, 900 participants in
phase 2 trial, randomly assigned to receive two doses
of placebo, 25 μg vaccine, or 50 μg vaccine, or three
doses of placebo, 25 μg vaccine, or 50 μg vaccine.
(YANG, LI, DAI 2021)
In the three doses of 25 μg vaccine group, the
most common local adverse reactions included pain
at the injection site (12%), swelling (14%), induration
(9%), redness (16%) and itching (19%). The most
common systemic adverse reactions in this group
included fever (8%), cough (1%), headache (2%) and
fatigue (0%). In general, most volunteers had no
adverse reactions or only minor adverse reactions. In
terms of humoral immunity, the seroconversion rates
of serum antibodies were 69% after the first injection,
and reached 100% 30 days after the second injection.
Notably, neutralizing antibodies were detected in
97% of the 25ug group. 14 days after the third
injection, neutralizing antibody titers of the 25ug
group exceeded those in the serum level of the
recovered patients. In terms of cellular immunity (T
cell response), the researchers performed an ELISpot
test on the peripheral blood of volunteers and
determined that both the 25μg group or the 50μg
group could induce moderate Th1 (IFN-γ and IL-2)
and Th2 (IL-4 and IL-5) responses after vaccination.
The data from Phase I/II suggest that ZF2001
offers a safe profile and strong immunogenicity.
Therefore, it was finally decided to use a three-dose
of 25ug (30 days between each injection) in the phase
3 clinical trial.
7.2 CIGB-66
CIGB-66 is a protein subunit COVID-19 vaccine
developed by the Center for Genetic Engineering and
Biotechnology in Cuba.
Efficacy, Safety and Immune Reactions Associated with COVID-19 Vaccines
319

On June 22,2021, official Cuban government
sources reported that the results of an initial study
involving 48,290 participants administered vaccines
in 3 doses, with a 2 weeks space. Result showed that
CIGB-66 had a 92.28% efficacy rate at preventing
symptomatic COVID-19. the analysis was based on
153 infection cases, including 11 in the vaccination
group and 142 in the placebo group.
8 VACCINE INGREDIENTS
WITH POTENTIAL ALLERGIC
SIDE EFFECTS
In the vaccines described above, some ingredients
have been known to cause allergic reactions. Below,
we discuss the known side effects associated with
each.
8.1 Beta-propiolactone
Beta-propiolactone (BPL) has been used for several
decades in different vaccines, such as the ones for
rabies. In 1987, a study by MC Anderson and
colleagues saw an association between urticarial
reactions and the rabies vaccine. (ANDERSON,
BAER, FRAZIER 1987) By looking at IgE and IgG
antibodies, researchers saw that besides developing
IgG against the subvirion, immunized individuals
also developed IgE and IgG to the BPL-Human serum
albumin used as adjuvant in the vaccine, which seems
to be the component that caused the strongest
reaction. Immunized subjects without urticaria had no
detectable IgE. The authors hypothesized that the
allergic reactions are mostly due to IgE antibodies,
since no fever, arthritis, lymphadenopathy or
nephritis were part of the symptoms. For the double
inactivated vaccine, beta-propiolactone, and human
serum albumin, most subjects with a urticarial
response to the booster had IgE. In contrast,
undetectable IgE in immunized subjects without
urticaria. A research article from 1987 also mentioned
urticaria as a common reaction to a rabies vaccine,
which also contained beta propiolactone. Studies
have shown that these responses are not caused by the
rabies virus antigens themselves, they are mostly
caused by the PBL-HSA complex. Notably, this
rabies vaccine response was very similar to that after
penicillin, suggesting an association with IgE
antibodies to penicillin metabolites that are haptens.
Apart from urticarial reactions, no adverse effects
have been associated with the use of beta-
propiolactone as an adjuvant, and therefore it seems
to be a safe ingredient in vaccine formulations.
8.2 Hydroxypropyl-β-cyclodextrin
Hydroxypropyl-β-cyclodextrin (HP-β-CD) is a cyclic
oligosaccharide of the cyclodextrin family that has
been used safely as an excipient for pharmaceutical
agents for decades. It is widely used to improve the
solubility of different compounds and it has been as a
excipient in pharmaceutical agents for several
decades. HP-β-CD as a vaccine adjuvant has shown
to induce IgG responses, but no IgE responses were
detected. Subcutaneous injection of solutions
containing HP-beta-CD is known to induce type I
interferon release and responses in Th2 cells, leading
to higher Ag-specific IgG titers, such as IgG1 and
IgG2c. However, no systemic proinflammatory
cytokine responses were detected. For this reason,
and for its high adjuvant activity, HP-β-CD is still
considered a safe adjuvant in vaccine formulations
with the main adverse event being diarrhea and there
have been no adverse events on kidney function.
(GOULD, SCOTT 2005)
8.3 Alum-based
Potassium alum, commonly named simply alum, is an
adjuvant with the formula KAl(SO
4
)
2
. Alum is well-
tolerated in a vast majority of cases and does not
usually induce clinically visible inflammatory
reactions in vaccinated subjects. It is known,
however, to cause nodules at the site of injection.
These nodules contain a large quantity of fibrin,
histone and host DNA and uric acid. It is
hypothesized that this release of intracellular
molecules may cause them to be recognized as
damage-associated molecular patterns (DAMPs).
(DESMET 2014) This release can trigger a
noninfectious inflammatory response by binding to a
pattern-recognition receptor. Aluminum-adjuvant-
containing vaccines are typically given over
relatively long intervals over a relatively short period
of time. Aluminum adjuvants immunotherapy should
take into consideration.
Aluminum salts are not currently used in
immunotherapy in the United States; however, they
are used in Europe as an immune stimulant. Some
researchers state that aluminum salts are mostly
irrelevant in immunotherapy. (TERHUNE, DETH
2014) Aluminum salts in allergy vaccines are known
to contribute to increased allergen-specific IgE, at
least in the 6 months following vaccine
administration. (JUTEL AKDIS 2011) In a 1972
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
320

study, young healthy men experimentally immunized
with ryegrass pollen allergens and alum allergens
developed type I cutaneous hypersensitivity, specific
histamine-releasing, and passively transferable of IgE
antibodies. (MARSH, LICHTENSTEIN, NORMAN
1972)
8.4 Lipid Nanoparticles (LNPs)
The Pfizer-BioNTech vaccine includes 4 different
LNPs: cholesterol, ALC-0159 (2-[(polyethylene
glycol)2000]-N,N-ditetradecylacetamide),1,2-
distearoyl-sn-glycero-3-phosphocholine (DSPC) and
ALC-0315 [(4-hydroxybutyl)azanediyl)bis(hexane-
6,1-diyl)bis(2- hexyldecanoate)]. Cholesterol and
DSPC are also ingredients of the Moderna vaccine
and have been used in different pharmaceutical agents
such as Doxil. ALC-0315 is an aminolipid that helps
with mRNA compaction and is involved in its cellular
delivery and cytoplasmic release, which is thought to
happen by endosomal destabilization. The Moderna
vaccine also contains an ionizable aminolipid, the
formulation of which is not disclosed, but its thought
to be heptadecan-9-yl8-((2-hydroxyethyl)(6-oxo-6-
(undecyloxy)hexyl)amino)octanoate. ALC-0159 is
present in the Pfizer-BioNTech vaccine at levels <2
mol % and it helps with nanoparticle stabilization by
a steric mechanism through its (polyethylene glycol)
PEG moiety. The Moderna vaccine has a similar
compound named 1,2-dimyristoyl-rac-glycero-3-
methoxyPEG2000, which is also a PEGylated lipid.
These PEGylated lipids are thought to be the
causative agents in the few cases, anaphylaxis was
observed in individuals to whom the vaccines were
administered. Complement activation was initially
thought to be the cause of allergic reactions to
pegylated nanodrugs. (MOGHIMI 2018) Although
complement activation, was initially proposed as a
possible reaction to vaccines, it does not seem to be
the actual case, since anaphylaxis is very rare in both
Pfizer-BioNTech and Moderna vaccines. (GANSON,
POVSIC, SULLENGER 2016) In cases of
anaphylactic reactions to the PEGylated
nanomedicines, the mechanisms are still unknown.
Although most people have high levels of anti-PEG
IgG, adverse allergic reactions are not expected. This
may be due to differences in the properties of anti-
PEG antibodies, and individual differences in
susceptibility to antibody-triggered responses cannot
be ruled out. Still, the molecular basis of these
responses in humans remains unknown.
In responding individuals, hypersensitivity
reactions to LNP-based vaccines may be related to the
pre-existing pre-existence of presumed anti-PEG IgE,
in addition, the likely intradermal titers of anti-PEG
IgG are expected to be extremely low to explain the
hypersensitivity of vaccine recipients’ reaction.
(ZHOU, STONE, JAKUBOVIC 2021) Given the
widespread presence of PEG in cosmetics and daily
hygiene products, these products appear to be
frequently used by people who have displayed
allergic reactions to mRNA vaccines. It is reasonable
since that other IgEs that cross-react with a
heterogeneous set of allergenic determinants also
recognize LNP and LNP aggregates, trace
lipid/mRNA impurities. In addition, different
epitopes on vesicles and PEG-lipid micelles that may
coexist can also be recognized.
In summary, PEG 2000, which is used in the
Pfizer-BioNTech and Moderna vaccines to stabilize
lipid nanoparticles, is the only compound in these
vaccines reported to cause anaphylaxis.
8.5 Polysorbate80
Polysorbate 80 is another compound similar to PEG
2000 that is present in many food and drugs, as well
as the Oxford/AstraZeneca vaccine. Polysorbate 80
has is considered a potential trigger to anaphylactoid
reacts and it is thought to cross-react with PEG.
Polysorbate 80 is used as an excipient in many drugs
and some vaccines. It can also use as a food additive.
Polysorbate 80 is widely tolerated. However, it has
been thought to potentiate anaphylactic reactions.
(COORS, SEYBOLD, MERK 2005) The use of high
molecular weight PEGs in a large variety of
medications, cosmetic and cleaning products which
may lead to sensitization in a more susceptible
individuals.(STONE, LIU, RELLING 2019)
9 CONCLUSIONS
In this paper we reviewed the different types of
vaccines, their ingredients and the reactions
associated with them. With the fast spread of the
COVID-19 pandemic and the appearance of different
newly-developed vaccines against SARS-CoV-2,
many concerns were raised regarding the efficacy and
safety of these vaccines, particularly about the mRNA
ones based on newer technologies.
Although the ingredients in the vaccines herein
analyzed seem safe for most, care should still be
taken, and possible alternatives be sought. Virus-
inactivators such as beta-propiolactone seems to
cause allergic reactions in only a few subjects.
Although it has proved to be a very effective viral
inactivator, perhaps some non-immunological
Efficacy, Safety and Immune Reactions Associated with COVID-19 Vaccines
321

alternatives such as radiation, formalin, or heat
inactivation could be considered to inactivate the
virus during the vaccine development stage. Several
vaccines inactivated using these methods have shown
great success in prevention. However, if a virulent
strain is used to produce the virus stock, inadequate
inactivation with formaldehyde can lead to several
issues. A number of children immunized with an
inactivated poliovirus vaccine preparation containing
inadequately inactivated Mahoney poliovirus
developed paralytic poliomyelitis. Furthermore, in
the 1960s, a formalin-inactivated RSV vaccine made
children sicker when they were exposed to natural
infections, resulting in several deaths. Likewise, an
inactivated measles vaccine was connected with an
unusual rash after exposure to the wild-type virus, a
reaction known as "atypical" measles. This brings us
back to the vaccines that do not use inactivated forms
of the virus, such as mRNA vaccines, where such
issues are not expected to occur. Despite very few
adverse reactions to beta-propiolactone, different
alternatives can be explored, mainly to reduce public
fear of vaccines and thus increase the number of
people getting vaccinated.
Concerning possible alternatives to alum, HP-
beta-CD seems to be a strong candidate, as it doesn’t
appear to elicit any IgE response. (GOULD, SCOTT
2005)
Alternatives to PEG as the main agent to different
allergic responses have also been proposed. While
compounds with a similar formulation are expected to
still cause allergic responses, neutral stabilizers such
as polyvinylpyrrolidone and its derivatives are a
possible alternative. It is often administered to large
numbers of individuals as a plasma expander to many
individuals with no reports of severe reactions
(BURNETT 2017).
Another factor to consider in COVID-19
vaccines, are potential changes in gene expression
arising from the Spike protein S, which is present in
some whole-protein vaccines or is the final
translational product of mRNA vaccines, which have
been recently described. (Evans 2021) These data are,
however, very preliminary.
Excluding pregnant women and adolescents, the
safety and effectiveness of these groups are unknown.
Other vaccines lack these two groups in the most
important phase III clinical trials. Clinical trials can
be supplemented in the future. It is mainly carried out
among healthy young men in the Middle East, while
the number of the elderly, women, and patients with
chronic diseases is limited.
As for efficacy, current vaccines seem to offer
protection against new variants, such as the high-
spreading Delta, and as such, their formulations are
most likely remaining unaltered for a while.
(GOV.UK 2021) In the trial of Heterologous
ChAdOx1 nCoV-19 and BNT162b2 prime-boost
vaccination elicits potent neutralizing antibody
responses and T cell reactivity, a total of 26
volunteers aged 25-46 years (median age 30.5 years)
received a dose of Oxford vaccine and then a dose of
Pfizer vaccine 8 weeks later. The variants selected
here are B.1.1.7 (Alpha, first discovered in the UK),
B.1.351 (Beta, first discovered in South Africa) and
B.1.617 (Delta, first discovered in India). (GROSS,
ZANONI, SEIDEL 2021) Studies have shown that
these variants are effectively neutralized by the sera
of all vaccinators.
It is important to note, that despite adverse effects
that are rare, COVID-19 vaccines are still considered
to be much safer than exposure to the virus, that even
for healthy people, might cause death or a variety of
lingering cardiac and neurologic symptoms
(NIKHRA 2021).
REFERENCES
AL KAABI N, ZHANG Y, XIA S., (2021). Effect of 2
Inactivated SARS-CoV-2 Vaccines on Symptomatic
COVID-19 Infection in Adults: A Randomized Clinical
Trial. J/OL. JAMA.
ANDERSON M C, BAER H, FRAZIER D J., (1987). The
Role of Specific IgE and Beta-Propiolactone in
Reactions Resulting from Booster Doses of Human
Diploid Cell Rabies Vaccine. J. The Journal of Allergy
and Clinical Immunology.
B. Sanders, M. Koldijk, and H. Schuitemaker., (2014).
Inactivated Viral Vaccines. J. Vaccine Analysis:
Strategies, Principles, and Control, pp. 45–80.
Bharat Biotech., (2021). COVAXIN - India’s First
Indigenous Covid-19 Vaccine | Bharat Biotech.
https://www.bharatbiotech.com/covaxin.html.
BUCCI E M, BERKHOF J, GILLIBERT A., (2021). Data
Discrepancies and Substandard Reporting of Interim
Data of Sputnik V Phase 3 Trial. J. The Lancet,
397(10288): 1881–1883.
BURNETT C L., (2017). PVP (Polyvinylpyrrolidone). J.
International Journal of Toxicology, 36(5_suppl2):
50S-51S.
CDC., (2021). Local Reactions, Systemic Reactions,
Adverse Events, and Serious Adverse Events: Janssen
COVID-19 Vaccine (J&J) |
CDC.https://www.cdc.gov/vaccines/covid-19/info-by-
product/janssen/reactogenicity.html.
COORS E A, SEYBOLD H, MERK H F., (2005).
Polysorbate 80 in Medical Products and
Nonimmunologic Anaphylactoid Reactions. J. Annals
of Allergy, Asthma & Immunology: Official
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
322

Publication of the American College of Allergy,
Asthma, & Immunology, 95(6): 593–599.
DESMET C J., (2014). Chapter 12 - Adjuvants Targeting
the DNA Sensing Pathways – Alum Based Adjuvants.
In: ISHII K J, TANG C K. (Eds.), Biological DNA
Sensor. Academic Press, Amsterdam. pp. 271-312.
EUROPEAN MEDICINES AGENCY., (2021). Vaxzevria
EMEA-H-A-5(3)-
1507.https://www.ema.europa.eu/en/documents/referr
al/use-vaxzevria-prevent-covid-19-article-53-
procedure-assessment-report_en.pdf.
FDA., (2021). FDA and CDC Lift Recommended Pause on
Johnson & Johnson (Janssen) COVID-19 Vaccine Use
Following Thorough Safety
Review.https://www.fda.gov/news-events/press-
announcements/fda-and-cdc-lift-recommended-pause-
johnson-johnson-janssen-covid-19-vaccine-use-
following-thorough. EUROPEAN MEDICINES
AGENCY. (2021) COVID-19 Vaccine Janssen:
Guillain-Barré syndrome listed as a very rare side
effect. https://www.ema.europa.eu/en/news/covid-19-
vaccine-janssen-guillain-barre-syndrome-listed-very-
rare-side-effect.
GANSON N J, POVSIC T J, SULLENGER B A., (2016).
Pre-existing anti–polyethylene glycol antibody linked
to first-exposure allergic reactions to pegnivacogin, a
PEGylated RNA aptamer. J. The Journal of allergy and
clinical immunology, 137(5): 1610-1613.e7.
GOULD S, SCOTT R C., (2005). 2-Hydroxypropyl-Beta-
Cyclodextrin (HP-Beta-CD): A Toxicology Review. J.
Food and Chemical Toxicology: An International
Journal Published for the British Industrial Biological
Research Association, 43(10): 1451–1459.
GOULD S, SCOTT R C., (2005). 2-Hydroxypropyl-β-
Cyclodextrin (HP-β-CD): A Toxicology Review. J.
Food and Chemical Toxicology, 43(10): 1451–1459.
GOV.UK (2021) Confirmed cases of COVID-19 variants
identified in UK.
https://www.gov.uk/government/news/confirmed-
cases-of-covid-19-variants-identified-in-uk.
GROSS R, ZANONI M, SEIDEL A., (2021). Heterologous
ChAdOx1 NCoV-19 and BNT162b2 Prime-Boost
Vaccination Elicits Potent Neutralizing Antibody
Responses and T Cell Reactivity. J. MedRxiv.
JACKSON N A C, KESTER K E, CASIMIRO D., (2020).
The Promise of MRNA Vaccines: A Biotech and
Industrial Perspective. J. Npj Vaccines, 5(1): 1–6.
JUTEL M, AKDIS C A., (2011). Immunological
Mechanisms of Allergen-Specific Immunotherapy. J.
Allergy, 66(6): 725–732.
LIVINGSTON E H, MALANI P N, CREECH C B., (2021).
The Johnson & Johnson Vaccine for COVID-19. J/OL.
JAMA.
LOGUNOV D Y, DOLZHIKOVA I V,
SHCHEBLYAKOV D V., (2021). Safety and Efficacy
of an RAd26 and RAd5 Vector-Based Heterologous
Prime-Boost COVID-19 Vaccine: An Interim Analysis
of a Randomised Controlled Phase 3 Trial in Russia. J.
The Lancet, 397(10275): 671–681.
MARSH D G, LICHTENSTEIN L M, NORMAN P S.,
(1972). Induction of IgE-Mediated Immediate
Hypersensitivity to Group I Rye Grass Pollen Allergen
and Allergoids in Non-Allergic Man. J. Immunology,
22(6): 1013–1028.
MARSHALL M, FERGUSON I D, LEWIS P., (2021).
Symptomatic Acute Myocarditis in Seven Adolescents
Following Pfizer-BioNTech COVID-19 Vaccination.
J/OL. Pediatrics.
Moderna., (2020). Moderna’s COVID-19 Vaccine
Candidate Meets Its Primary Efficacy Endpoint in the
First Interim Analysis of the Phase 3 COVE Study.
https://investors.modernatx.com/news-releases/news-
release-details/modernas-covid-19-vaccine-candidate-
meets-its-primary-efficacy/.
MOGHIMI S M., (2018). Nanomedicine Safety in
Preclinical and Clinical Development: Focus on
Idiosyncratic Injection/Infusion Reactions. J. Drug
Discovery Today, 23(5): 1034–1042.
Nicholas J. Evans., (2021). R3097 - "Lung Time No See":
SARS-Cov-2 Spike Protein Changes Genetic
Expression in Human Primary Bronchial Epithelial
Cells After
Recovery.https://www.eventscribe.net/2021/EB2021/i
ndex.asp?presTarget=1640424.
NIH., (2019). Vaccine Types | NIH: National Institute of
Allergy and Infectious Diseases.
https://www.niaid.nih.gov/research/vaccine-types.
NIKHRA V., (2021). Living with ‘Long COVID-19’: The
long-term complications and sequelae. J. International
Journal of Clinical Virology, 5(1): 011-021.
PALACIOS R, BATISTA A P, ALBUQUERQUE C S N.,
(2021). Efficacy and Safety of a COVID-19 Inactivated
Vaccine in Healthcare Professionals in Brazil.
https://papers.ssrn.com/abstract=3822780.
PARDI N, HOGAN M J, PORTER F W., (2018). MRNA
Vaccines — a New Era in Vaccinology. J. Nature
Reviews Drug Discovery, 17(4): 261–279.
Pfizer., (2020). Pfizer and BioNTech Conclude Phase 3
Study of COVID-19 Vaccine Candidate, Meeting All
Primary Efficacy
Endpoints.https://www.pfizer.com/news/press-
release/press-release-detail/pfizer-and-biontech-
conclude-phase-3-study-covid-19-vaccine.
SADOFF J, GRAY G, VANDEBOSCH A., (2021). Safety
and Efficacy of Single-Dose Ad26.COV2.S Vaccine
against Covid-19. J. New England Journal of Medicine,
384:2187-2201.
SCHULTZ N H, SØRVOLL I H, MICHELSEN A E.,
(2021). Thrombosis and Thrombocytopenia after
ChAdOx1 nCoV-19 Vaccination. J. New England
Journal of Medicine, 384:2124-2130.
STONE C A, LIU Y, RELLING M V., (2019). Immediate
Hypersensitivity to Polyethylene Glycols and
Polysorbates: More Common Than We Have
Recognized. J. The journal of allergy and clinical
immunology. In practice, 7(5): 1533-1540.e8.
TATSIS N, ERTL H C J., (2004). Adenoviruses as Vaccine
Vectors. J. Molecular Therapy, 10(4): 616–629.
Efficacy, Safety and Immune Reactions Associated with COVID-19 Vaccines
323

TERHUNE T D, DETH R C. (2014) A Role for Impaired
Regulatory T Cell Function in Adverse Responses to
Aluminum Adjuvant-Containing Vaccines in
Genetically Susceptible Individuals. J. Vaccine, 32(40):
5149–5155.
Vaccine Tracker., (2021). Vaccines – COVID19 Vaccine
Tracker.
https://covid19.trackvaccines.org/vaccines/approved/.
VOYSEY M, CLEMENS S A C, MADHI S A., (2021).
Safety and Efficacy of the ChAdOx1 NCoV-19
Vaccine (AZD1222) against SARS-CoV-2: An Interim
Analysis of Four Randomised Controlled Trials in
Brazil, South Africa, and the UK. J. The Lancet,
397(10269): 99–111.
YANG S, LI Y, DAI L., (2021). Safety and
Immunogenicity of a Recombinant Tandem-Repeat
Dimeric RBD-Based Protein Subunit Vaccine
(ZF2001) against COVID-19 in Adults: Two
Randomised, Double-Blind, Placebo-Controlled, Phase
1 and 2 Trials. J. The Lancet. Infectious Diseases,
21(8): 1107-1119.
ZHOU Z-H, STONE C A, JAKUBOVIC B., (2021). Anti-
PEG IgE In Anaphylaxis Associated with Polyethylene
Glycol. J. The journal of allergy and clinical
immunology. In practice, 9(4): 1731-1733.e3.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
324
