
An Analysis on the Relationship between Obesity and COVID-19
Mortality
Xinyue Liu
Schulich School of Medicine & Dentistry, Western University, London, Ontario, Canada, N6A 3K7
Keywords: COVID-19/SARS-Cov-2, Covid-19 Mortality, Obesity, ER Stress, Immune Response, Lung Compliance.
Abstract: Since 2020, obesity and coronavirus disease 2019 (COVID-19) have become two of the most globally
challenged health and medical conditions, and the proportion of obese population and numbers of deaths for
COVID-19 continue to grow. Obesity has been claimed as a possible risk factor of COVID-19 infection and
mortality by the World Health Organization (WHO) and the World Obesity Federation. However, the
mechanisms about why obesity worsens COVID-19 symptoms have not been extensively and thoroughly
studied. So, literature research was performed in this study to propose the reason for declaring obesity as a
risk factor of severe COVID-19 and COVID-19 mortality. In conclusion, obesity induces endoplasmic
reticulum (ER) stress and vitamin D deficiency, which causes localized inflammation and impedes the
immune responses to SARS-CoV-2 infections. As ER stress state prolongs, unfolded protein response (UPR)
and apoptosis may be induced, which give rise to injury of tissues and organs. Although the obese population
has increased lung surfactants to balance their increased chest wall restraints, SARS-Cov-2 infections strongly
impair lung surfactants and enhance mechanical compression. These elements decrease lung compliance in
obese COVID-19 patients; thus, the patients experience difficulties of breathing. Therefore, the susceptibility
to the COVID-19 mortality increases. Further research is still needed to test these theoretical ideas and to
explore more on relationships between obesity and COVID-19.
1 INTRODUCTION
SARS-CoV-2, a new strain of coronavirus caused
COVID-19, has killed over 4 million deaths since the
beginning of 2020. Researches on SARS-CoV-2 and
COVID-19 are being carried out urgently in many
laboratories. It has been discovered that obesity
seems to be one of the risk factors for COVID-19
mortality (Cuschieri, and Grech 2020). A meta-
analysis based on over three million cases has shown
a significant increase in the COVID-19 mortality rate
of the obese population (Wang, Xu, Wang, Hou,
Feng, and Yang 2021). However, there is very little
research studying why obese COVID-19 patients are
more susceptible to death. Therefore, this study will
discuss the relationship between obesity and COVID-
19 mortality. Furthermore, brief descriptions of each
potential cause will be outlined respectively. It is
acknowledged that these three factors are not the only
factors that push obesity as a risk factor of COVID-
19 mortality, but this study will pay attention to the
theoretical analysis of how these three factors become
the main factors resulting in death in obese people.
For further research, experiments are needed to
confirm the proposed mechanisms and some potential
physical activity interventions that could be taken to
decrease COVID-19 mortality in the obese
population.
Previous researches have shown that both obesity
and virus infections induce ER stress in cells
(Banerjee, Czinn, Reiter, and Blanchard 2020, Zhou,
and Liu 2010). ER usually serves as a protein
modifying and secretory site. However, under ER
stress, unfolded and misfolded proteins are
accumulated in ER, which exceed the normal protein
concentration of 100 mg/ml and impede the functions
of ER (Wu, and Kaufman 2006). The ER stress will
activate unfolded protein response (UPR) to rapidly
decrease protein translation rate and initiate ER-
associated degradation (ERAD). Therefore, unfolded
and misfolded proteins are eliminated and the
survival rates of the cells are increased (Sureda,
Alizadeh, Nabavi, Berindan-Neagoe, Cismaru,
Jeandet, Łos, Clementi, Nabavi, and Ghavami 2020).
However, if the condition of ER stress prolongs and
the effort of survival fails, apoptosis will be activated
Liu, X.
An Analysis on the Relationship between Obesity and COVID-19 Mortality.
DOI: 10.5220/0011244900003438
In Proceedings of the 1st International Conference on Health Big Data and Intelligent Healthcare (ICHIH 2022), pages 215-220
ISBN: 978-989-758-596-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
215
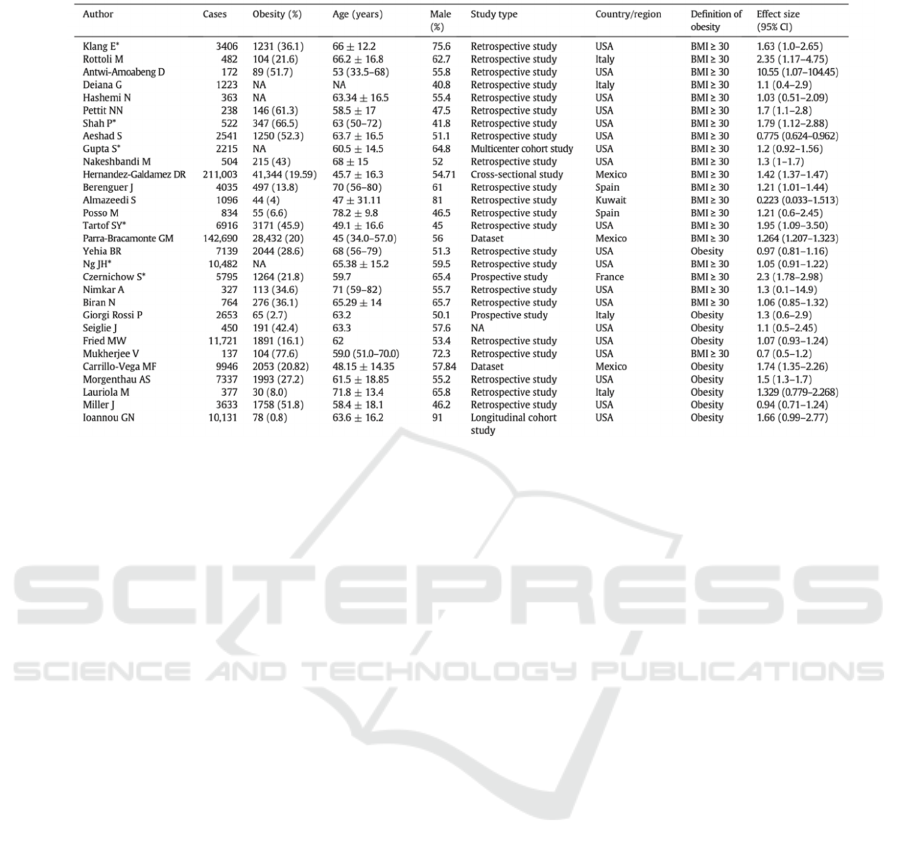
Table 1. General information of included studies (Wang, Xu, Wang, Hou, Feng, and Yang 2021)
to respond to irreversible ER stress (Sureda,
Alizadeh, Nabavi, Berindan-Neagoe, Cismaru,
Jeandet, Łos, Clementi, Nabavi, and Ghavami 2020).
The immune response is essential for defending
against viral infections. Nevertheless, the previous
study has shown that obesity will chronically
attenuate immune response by impeding the synthesis
of vitamin D, which is required for the functions of
the immune system (Banerjee, Czinn, Reiter, and
Blanchard 2020). Additionally, obesity causes a
decrease in lung compliance by lipid accumulation,
increasing chest wall compression, and relative
surfactant deficiency (Inselman, Chander, and Spitzer
2004). The decreased lung compliance requires more
forces during lung inflation and deflation. All these
factors contribute to COVID-mortality.
2 OBESITY, COVID-19, AND ER
STRESS
ER stress and its following mechanisms contribute to
COVID-19 mortality in the obese population by
causing organ damage. Both obesity and SARS-CoV-
2 infections cause ER stress, activating the UPR, and
triggering adaptive programs. The accumulation of
misfolded and unfolded proteins is detected by an
ER-specific chaperone called binding immunoglobin
protein (BiP, 78kDa), which then activates the three
ER stress sensors: protein kinase-like ER kinase
(PERK), the inositol-requiring ER-to-nucleus signal
kinase 1 (IRE1), and activating transcription factor 6
(ATF6) (Zhou, and Liu 2010). These three routes will
contribute to solving the problem of ER stress by
increasing ER folding efficiency, degrading unfolded
and misfolded protein by ubiquitin-proteasome
pathway or autophagy-dependent pathway, and
producing apoptotic signals if necessary (Zhou, and
Liu 2010).
It has been observed that many tissues like
adipose tissues, the liver, and the pancreas undergo
ER stress because the homeostasis is not balanced in
obese patients (Zhou, and Liu 2010). The
inflammatory responses can be augmented by
reducing adiponectin gene expression; however,
adiponectin plays an important role in autophagy-
mediated degradation (Zhou, and Liu 2010). The
decrease in adiponectin is observed in both of obese
and COVID-19 patients. COVID-19 patients with a
higher body mass index (BMI, 32.8 ± 9.5) have a
lower survival rate (75%) than non-COVID-19
patients (BMI, 30.2 ± 5.4; survival rate, 82%). Also,
nearly 4 times lower adiponectin level was
discovered in COVID-19 patients with respiratory
failure compared to non-COVID-19 respiratory
failure (Kearns, Ahern, Patrie, Horton, Harris, and
Kadl 2021). The decreased adiponectin level results
in the ineffectiveness of degrading misfolded and
unfolded proteins and a prolonged the chronic
inflammatory condition, which is harmful to the
human body and causes many other systematic
problems.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
216
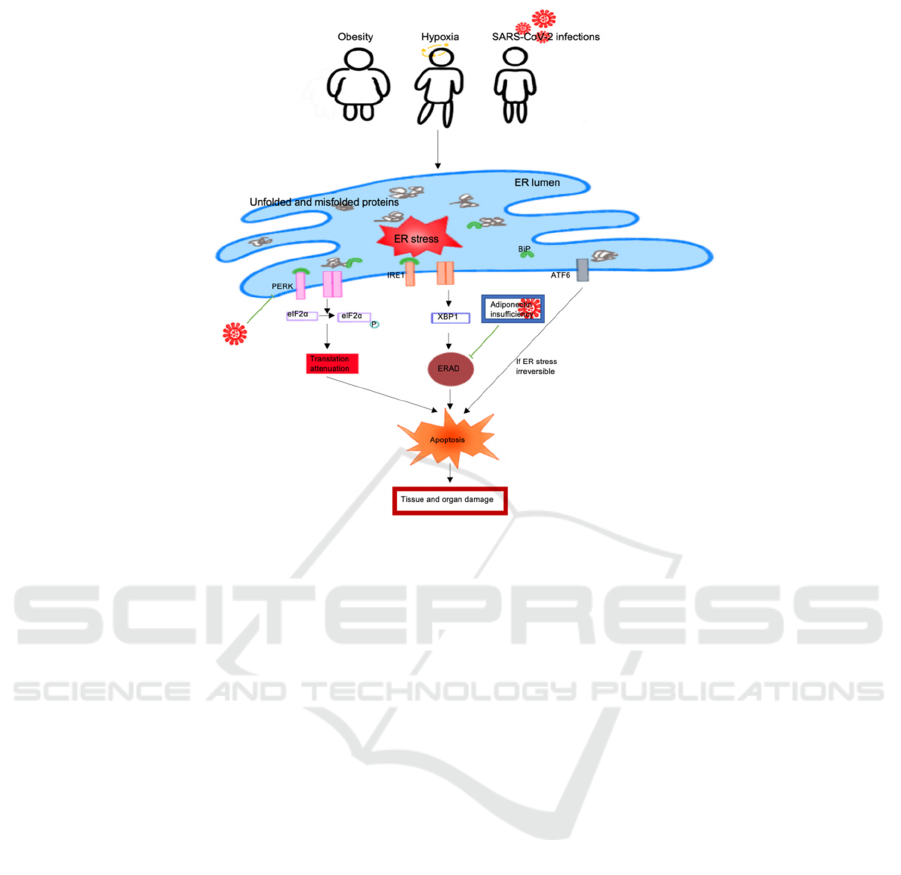
Figure 1. Schematic representation of how obesity increases COVID-19 mortality by activating ER stress and apoptosis.
SARS-CoV-2 causes inhibition of translational attenuation and adiponectin transcription, leading to prolonged ER stress and
tissue and organ damage.
In a recent study, researchers have discussed how
coronavirus causes ER stress and interrupts the UPR
(Banerjee, Czinn, Reiter, and Blanchard 2020). In the
cases of COVID-19, hypoxia, another factor causing
ER stress, has been observed (Sureda, Alizadeh,
Nabavi, Berindan-Neagoe, Cismaru, Jeandet, Łos,
Clementi, Nabavi, and Ghavami 2020). The levels of
reactive oxygen species and Ca
2+
are disrupted in the
infected cells (Banerjee, Czinn, Reiter, and Blanchard
2020). These disturbances are activated by ER stress
and lead to signal transductions and activations of the
UPR. However, the researchers also suggested that
coronavirus can interrupt the host UPR by interacting
with the host’s UPR pathways (Banerjee, Czinn,
Reiter, and Blanchard 2020). The route of PERK,
which has antiviral activities, could be disrupted by
the virus via constant eukaryotic translation initiation
factor 2 alpha (eIF2α) phosphorylation. This
phosphorylation also blocks the translation of the X-
box binding protein 1 (XBP1) transcriptional factor,
which can attenuate the ERAD quality control
mechanism and lead to prolonged ER stress and
inflammation state. Apoptosis is activated by the
UPR and inflammatory signals are increased
dramatically if obese patients are invaded by SARS-
CoV-2. Obesity accelerates this process as the
apoptosis continues in inflammatory tissues and
damages organs (Sureda, Alizadeh, Nabavi,
Berindan-Neagoe, Cismaru, Jeandet, Łos, Clementi,
Nabavi, and Ghavami 2020). As a one of the leading
causes of death, organ damages have been observed
in many deaths of obese COVID-19 patients.
3 OBESITY, COVID-19, AND
IMMUNE RESPONSE
Obesity gives rise to the hindrance and attenuation of
immune response to SARS-CoV-2, which increases
the risk of COVID-19 mortality. If obese patients stay
in chronic inflammation for a long time, the
inflammation will spread from local to systematic
inflammation and from adipose cells to mass cells
such as pulmonary epithelial and endothelial cells
(Cuschieri, and Grech 2020). The inflammation in the
airway increases the susceptibility to be infected by
SARS-CoV-2 and have airway diseases. Besides,
systematic inflammation can disrupt blood flow, thus
inducing hypoxia and impairing immune cell
functions and responses (Cuschieri, and Grech 2020).
The chronic and systematic inflammation condition
also delays immune responses, which gives SARS-
An Analysis on the Relationship between Obesity and COVID-19 Mortality
217
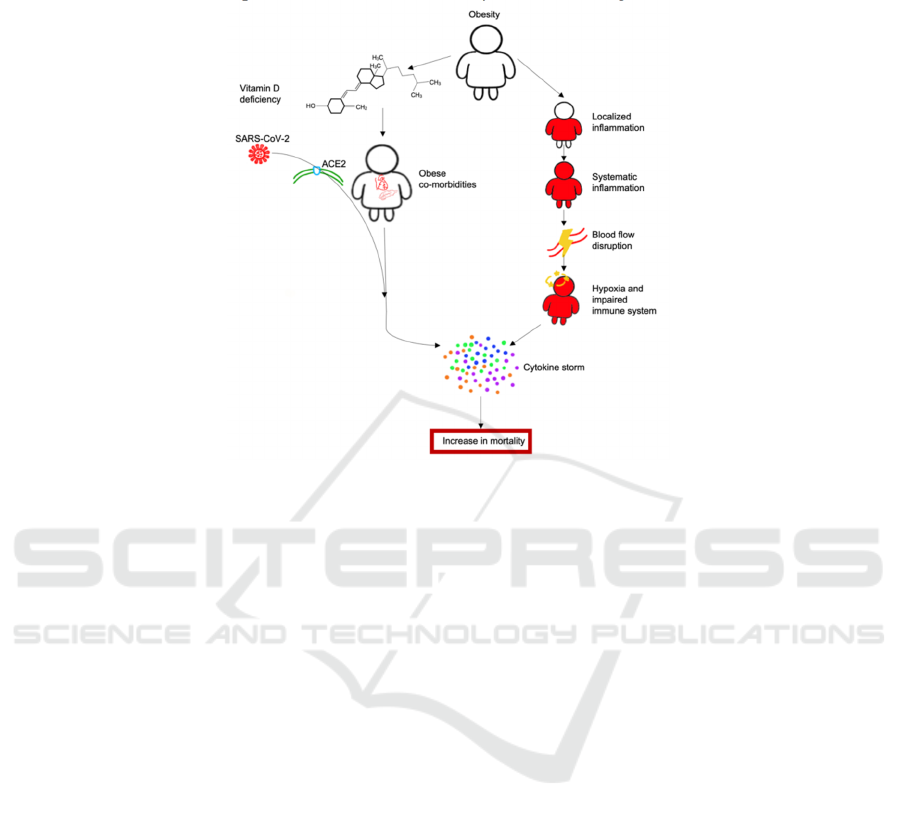
CoV-2 viruses more time to replicate and spread.
Besides, the severe medical issue called cytokine
storm occurs and causes fatal problems in the human
body (Hammock, Wang, Gilligan, and Panigrahy
2020). The quick multiplication of the virus and
cytokine storm augments the therapeutic difficulties.
Figure 2. Schematic representation of how obesity increases COVID-19 mortality by the combination of vitamin D deficiency
and delayed immune responses. This combination gives more possibility of cytokine storm occurrence and increases in
COVID-19 mortality.
It has been reported that vitamin D deficiency was
shown in most of the obese patients. This deficiency
may be caused by co-morbidities of obesity like liver
steatosis and hyperparathyroidism (Cuschieri, and
Grech 2020). Vitamin D takes an important role in the
“modulation of both the innate and the adaptive
immune responses” (Cuschieri, and Grech 2020).
Therefore, if the vitamin D is deficient, the immune
responses cannot be efficient, the susceptibility of the
spread of SARS-CoV-2 in the body is increased, and
cytokine storm are induced. Obese patients themself
have delayed immune responses additionally with
vitamin D deficiency further worsens the symptoms
of COVID-19.
It is commonly known that obese patients have
various co-morbidities such as type 2 diabetes
mellitus, hypertension, respiratory muscle function
impairment, and cardiovascular diseases. These co-
morbidities are linked with cell dysfunctions,
impaired immune system, and increased risk of
COVID-19 mortality. SARS-CoV-2 can easily enter
pancreatic and myocardial cells through angiotensin-
converting enzyme 2 (ACE2) receptors, which are
commonly found in many cell types and “responsible
for anti-inflammatory responses” (Cuschieri, and
Grech 2020). The disruption of ACE2 signaling
pathways results in acute metabolic dysfunctions like
hyperglycemia and acute cell injury. For this reason,
COVID-19 patients with obesity and its co-
morbidities have a 2 to 3 times higher rate of being in
intensive care unit (Cuschieri, and Grech 2020) and
thus an augmented risk of mortality.
4 OBESITY, COVID-19, AND
LUNG COMPLIANCE
Decreased lung compliance in obese patients by
increased chest wall compression and surfactant
deficiency conduce to augmented COVID-19
mortality. It has often been seen that obese patients
have faster and shallower breaths. This symptom is
due to the stiff chest wall caused by mechanical
compression, accumulated lipid around the
diaphragm and in the abdomen, and increased work
of respiratory muscles (Cuschieri, and Grech 2020,
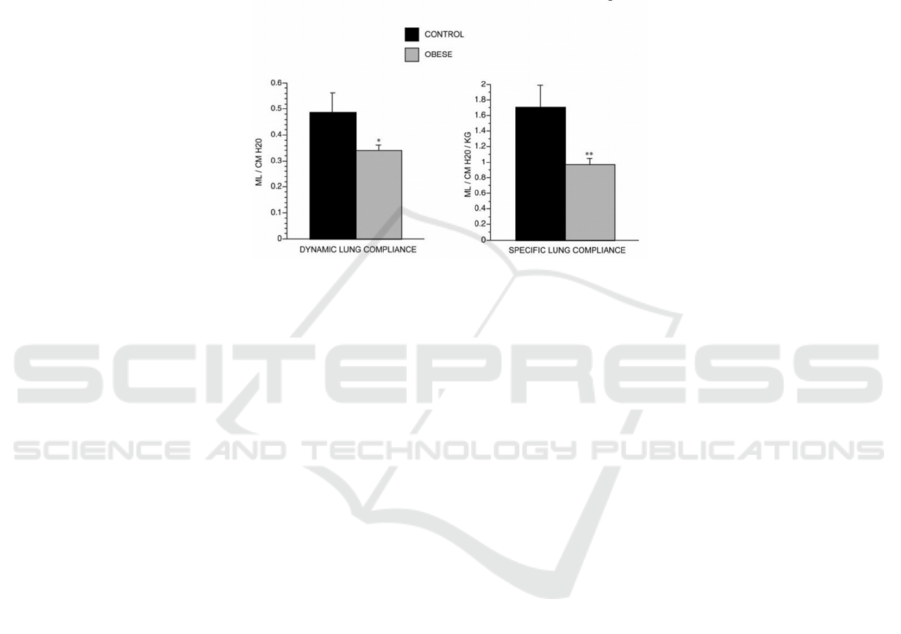
Inselman, Chander, and Spitzer 2004) A 33%
increase of respiratory rates (RR) and 29% and 44%
decreases of dynamic and specific lung compliance
were observed in obese rat models with a 31%
increase in weights (Inselman, Chander, and Spitzer
2004). The respiratory muscles try to adapt and
compromise the decreased lung compliance and “the
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
218
increased mechanical and metabolic requirements for
chest wall expansion” (Inselman, Chander, and
Spitzer 2004, Mahadev, Salome, Berend, and King,
2013). However, the respiratory muscles adaptions
are not enough to compromise the increased
mechanical compression. Adding to the problem, the
stiffness of respiratory muscles is increased and
consequently further narrows the airway by 42.6 ±
8.6% (Inselman, Chander, and Spitzer 2004)
(Inselman, Chander, and Spitzer 2004, Mahadev,
Salome, Berend, and King 2013). The narrower
airway is fatal for COVID-19 patients as they have
acute respiratory distress syndrome (ARDS), which
can further decrease blood oxygen levels and
deteriorate the symptoms of hypoxia. The reduced
chest wall compliance can increase dead space during
breathing and increase ventilation heterogeneity,
which may result in more severe pulmonary
dysfunctions. Besides, the continued airway
inflammation and airway narrowing are associated
with surfactant dysfunction (Mahadev, Salome,
Berend, and King 2013).
Figure 3. Dynamic and specific compliance in control and obese rats at age 8 weeks. Values are means ± SE. *p < 0.05; ** p
< 0.001. Both dynamic and specific lung compliance are reduced in obese rats (n = 16) when compared with control rats (n
= 14) (Inselman, Chander, and Spitzer 2004).
To compromise increased chest wall
compressions, a slight increase in lung surfactant
levels of large aggregates (14%) and small aggregates
(35%) has been observed in obese rat models
(Inselman, Chander, and Spitzer 2004). However,
these changes can result in a deficiency of lung
surfactants and impairment of lung functions. As
COVID-19 may result in lung injury, the surfactant
can progressively aggregate and lead to “a loss of
overall surface activity in the lung” (Inselman,
Chander, and Spitzer 2004) and lung instability
(Schousboe, Wiese, Heiring, Verder, Poorisrisak,
Verder, and Nielsen 2020)]. The lung surfactant
deficiency can be fatal because it increases the
difficulty of breathing in obese COVID-19 patients
and further augments COVID-19 severity. It has been
monitored that if COVID-19 patients’ lung
compliances further decrease to 42 ± 3 mL/cmH2O
and the breaths become shallower, it is likely to cause
hyperinflation that gives rise to more severe diseases
and deaths (Roesthuis, van den Berg, and van der
Hoeven 2020).
5 CONCLUSIONS
This study has discussed the relationship between
obesity and COVID-19 mortality and proposed three
possible mechanisms of how obesity deteriorate the
symptoms of COVID-19 symptoms. Obese
individuals are more susceptible to death from
COVID-19 because of ER stress-mediated apoptoses,
defective immune responses, and decreased lung
compliances. These three factors accelerate the
process and severity of COVID-19. Obesity causes
prolonged inflammation and ER stress. These two
conditions expedite the action of driving degradation
machinery UPR to activate apoptotic mechanisms.
Along with SARS-CoV-2 infections, acute organ
damage will be induced in the obese population. Also,
obese people have dysfunctional immune systems
due to vitamin D deficiency, cytokine storms, and
disrupted ACE2 signal pathways. These hindered
immune responses increase therapeutic difficulties.
Lastly, obesity results in a decreased lung compliance
and lung volume by increasing chest wall
compression and lung surfactant dysfunction.
COVID-19 patients may have lung injury which
accelerates the aggregation of lung surfactants,
leading to lung instability and dysfunctions, and then
An Analysis on the Relationship between Obesity and COVID-19 Mortality
219

contributing to COVID-19 mortality. These factors
should be noticed when treating obese COVID-19
patients. Obesity, a chronic and metabolic disease,
should be put more attention on because it not only
causes a wide range of co-morbidities but may be
fatal especially when people are invaded by viruses.
This study may have important implications
regarding to the development of valuable approaches
to reduce COVID-19 mortality in the obese
population. Future studies and experiments are
needed to test whether these three reasons primarily
cause increased COVID-19 mortality in the obese
population. Also, efficient treatments and
interventions can be considered based on these three
factors.
ACKNOWLEDGMENTS
The author is grateful to Dr. Shibin Cheng (Brown
University) and Xinyue Qiu (Yale University) for
their instructions and support. The author
acknowledges for creating figures using Sketchbook
application and Microsoft PowerPoint software.
REFERENCES
Banerjee, A., Czinn, S. J., Reiter, R.J., and Blanchard, T. G.
(2020). Crosstalk between endoplasmic reticulum
stress and anti-viral activities: A novel therapeutic
target for COVID-19. Life Sciences, 255, 117842.
Cuschieri, S., and Grech, S. (2020). Obesity population at
risk of COVID-19 complications. Global Health,
Epidemiology and Genomics, 5.
Hammock, B. D., Wang, W., Gilligan, M. M., and
Panigrahy, D. (2020). Eicosanoids: The Overlooked
Storm in Coronavirus Disease 2019 (COVID-19)? The
American Journal of Pathology, 190(9), 1782–1788.
Inselman, L. S., Chander, A., and Spitzer, A. R. (2004).
Diminished Lung Compliance and Elevated Surfactant
Lipids and Proteins in Nutritionally Obese Young
Rats. Lung, 182(2), 101–117.
Kearns, S. M., Ahern, K. W., Patrie, J. T., Horton, W. B.,
Harris, T. E., and Kadl, A. (2021). Reduced adiponectin
levels in patients with COVID‐19 acute respiratory
failure: A case‐control study. Physiological
Reports, 9(7).
Mahadev, S., Salome, C. M., Berend, N., and King, G. G.
(2013). The effect of low lung volume on airway
function in obesity. Respiratory Physiology &
Neurobiology. 188(2), 192–199.
Roesthuis, L., van den Berg, M., and van der Hoeven, H.
(2020). Advanced respiratory monitoring in COVID-19
patients: use less PEEP! Critical Care, 24(1), 230–230.
Schousboe, P., Wiese, L., Heiring, C., Verder, H.,
Poorisrisak, P., Verder, P., and Nielsen, H. B. (2020).
Assessment of pulmonary surfactant in COVID-19
patients. Critical Care, 24(1), 552–552.
Sureda, A., Alizadeh, J., Nabavi, S. F., Berindan-Neagoe,
I., Cismaru, C. A., Jeandet, P., Łos, M. J., Clementi, E.,
Nabavi, S. M., and Ghavami, S. (2020). Endoplasmic
reticulum as a potential therapeutic target for covid-19
infection management? European Journal of
Pharmacology, 882, 173288.
Wang, Y., Xu, J., Wang, Y., Hou, H., Feng, H., and Yang,
H. (2021). An updated meta-analysis on the
relationship between obesity and COVID-19
mortality. Metabolism, 122, 154820.
Wu, J., and Kaufman, R. J. (2006). From acute ER stress to
physiological roles of the Unfolded Protein
Response. Cell Death & Differentiation, 13(3), 374–
384.
Zhou, L., and Liu, F. (2010). Autophagy: Roles in obesity-
induced ER stress and adiponectin downregulation in
adipocytes. Autophagy, 6 (8), 1196–1197.
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
220
