
Susceptibility to HIV and Strategies to Prevent AIDS
Zirui Li
a
High School Attached to Northwest Normal University,China
Keywords: HIV, AIDS, Immunodeficiency, Virus, Treatment, COVID-19.
Abstract: HIV (Human Immunodeficiency Virus) is an infectious disease that can progress to AIDS (Acquired
lmmunodeficiency Syndrome), causing deaths. Despite all the advances in understanding the molecular
mechanism of virus entry, replication, propagation and transmission, there is not a complete cure for this
disease. Although the disease can be controlled by antiretroviral therapy, the treatment is not available for
many people, causing a disparity in the care of the population who are infected. Furthermore, as HIV is mainly
transmitted by contact with infected body fluid, such as during sexual intercourse and sharing contaminated
needles, some vulnerable groups in the population are more susceptible to becoming infected. This article
provides an overview of HIV and AIDS by reviewing the current references from an epidemiological
perspective, in addition to discussing treatments available. Moreover, susceptible groups who are vulnerable
to HIV, such as people living in Sub-Saharan Africa, sexual workers, and drug abusers are discussed, and
some solutions are suggested. Finally, a connection between the COVID-19 pandemic and lessons which can
be learned for the HIV diagnosis and treatments is established. In conclusion, HIV and AIDS still remain a
threat to global health, and measures should be taken to not only to study the disease better, but also to find
permanent treatments such as vaccines, despite challenges.
1
INTRODUCTION
HIV (Human Immunodeficiency Virus) is an
infectious disease caused by retroviruses, which can
develop into AIDS (Acquired Immunodeficiency
Syndrome) if it remains untreated. HIV can be
transmitted through sexual contact, using
contaminated and shared needles, passed from
mother to child during pregnancy and childbirth, and
via contaminated blood transfusion (Cdc.gov. 2021).
Many infected patients do not show any symptoms
during the first few months of infection, and
therefore, can transmit the virus. Some people may
have flu-like symptoms, including fever, headache,
and sore throat during the early phases of the
infection, when the viral load is at its highest
(aidsmap.com. 2021). As the disease develops, the
immune system succumbs, and symptoms become
more pronounced, including swollen lymph nodes,
diarrhea, fever and rapid weight loss (HIV.gov. 2021).
HIV weakens the body's ability to fight other
infections, and people who do not receive treatment
are more susceptible to other diseases, such as
a
https://orcid.org/0000-0002-1231-2736
cholera, bacterial infections, cryptococcal meningitis
and some cancers (Who.int. 2021). In the battle
against AIDS, the best tactic for the treatment of HIV
is antiretroviral therapy (ART). Approximately 25
unique antiretroviral drugs are already used for the
treatment of adults. But there has not been a definitive
cure for HIV yet. The treatment objectives are to
minimize and sustain the viral load, to obtain immune
function reconstruction and maintain immune
function, to improve the quality of life, and to reduce
morbidity and mortality associated with HIV.
2
EPIDEMIOLOGY OF HIV
After initial uncertainties in the early 1980s
surrounding the emergence of a new disease, it soon
became apparent that an epidemic and then a
pandemic was underway. Since then, 38 million
people have acquired HIV, including 36.2 million
adults and 1.8 million children under 15 years old. It
is estimated that the number of people living with
HIV has increased by 1.9 million recently, but the
Li, Z.
Susceptibility to HIV and Strategies to Prevent AIDS.
DOI: 10.5220/0011233100003438
In Proceedings of the 1st International Conference on Health Big Data and Intelligent Healthcare (ICHIH 2022), pages 115-123
ISBN: 978-989-758-596-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
115
incidence rate is still 23% lower than in 2010.
Approximately 81% of people are tested for HIV
each year, so the figures are an underestimation, and
the actual number of infections is much higher than
the number recorded. Among people who are now
known to have been infected with HIV, by the end of
the 2019, 36.2 million people living with HIV (67%)
had access to antiretroviral drugs, and nearly 12.6
million people are still waiting for treatment
(HIV.gov. 2021), demonstrating a huge gap between
diagnosis and treatment.
3 DISCUSSION MECHANISMS
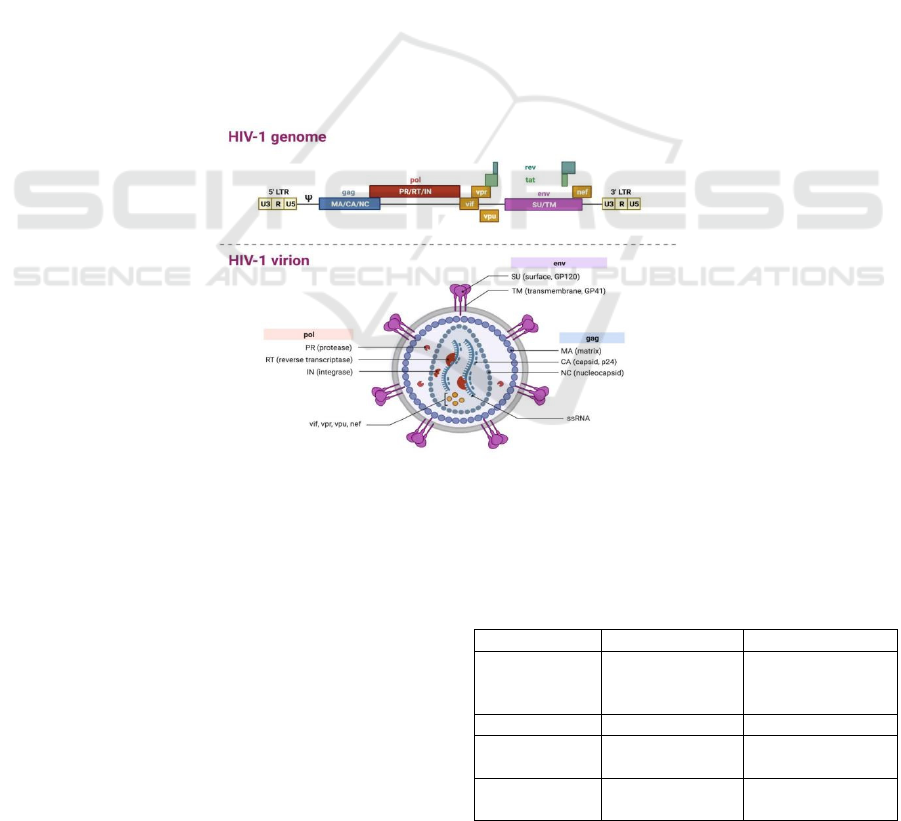
3.1 Virus Structure
Studying the susceptibility to HIV and strategies to
prevent AIDS, such as developing antiretroviral
drugs and vaccines, requires an understanding of the
HIV structure, which is discussed below. HIV
particles are spherical and 90-130 nanometers in
diameter (Wikipedia. 2021). The core of the virus is
hollow conical and consists of two identical single-
stranded RNA chains, reverse transcriptases and
proteins (Figure1). Outside the core is the viral shell,
which is three-dimensional symmetry of 20
polyhedromes and contains nuclear shell proteins.
The outermost layer is the envelope, where
glycoproteins have puncture-like structures, and
these are the main binding site of HIV and host cell
receptors. HIV is a retrovirus, with RNA containing
the gag, env and pol genes, as well as six regulatory
genes (tat, vif, vpr, vpx (vpu), nef, rev) (Online
Biology Notes. 2021). The core protein of the gag
gene encodes the virus; the enzymes (retroviruses,
integrated enzymes and proteases), which are
required for replication of the pol gene to encode
virus envelope protein, which is the main antigen for
HIV immunological diagnosis (Wikipedia. 2021).
Regulatory genes encode aid proteins and regulate
viral protein synthesis and replication.
Figure 1. An overview of HIV-1 virus genome (top) and its structure (bottom). The figure was generated using Biorender.
There are two main types of HIV present: HIV-1
and HIV-2. Both are transmitted through the same
routes, but HIV-2 has a lower chance of transmission
than HIV-1 because the immune system responds
better to HIV-2 and responds (Nyamweya, Hegedus,
Jaye, Rowland-Jones, Flanagan, Macallan 2013).
While there are still many essential differences
between HIV-1 and HIV-2, an extended comparison
is beyond the scope of this paper, and an overall
comparison of HIV-1 and HIV-2 is shown in table 1.
Table 1. A comparison of HIV-1 and HIV-2, including their
prevalence, origin, transmission and disease course.
HIV-1 HIV-2
Prevalence Global
West Africa,
Mozambique and
An
g
ola
Origin Chimpanzees Sooty mangabeys
MTCT
Relatively
common
Relatively rare
Heterosexual
sprea
d
Higher Lower
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
116
Genetic
Diversit
y
More Less
Time to AIDS
Less than 10
years
More than 20
years
3.2 HIV Transmission
Studying the transmission of HIV is essential for
tackling susceptibility and preventing disease
progression. HIV can be transmitted through body
fluids during sexual relations with people living with
HIV (anal or vaginal sex), through the sharing of
infected needles, syringes or other drug injection
equipment, and from mother to fetus during
pregnancy and birth.
3.2.1 Sexual Contact
People can contact HIV from their sexual partners
during sexual intercourse without using protection
measures, such as condoms or other medicines that
can prevent or control HIV. Anal sex is the greatest
risk factor for transmitting HIV, especially in men
who have sex with other men, due to the thin lining
of the rectum, which facilitates the HIV virus entry
into the body (Cdc.gov. 2021). Most women contract
HIV from vaginal sex because HIV can enter the
body through the mucous membranes that line on the
vaginal and cervix (Cdc.gov. 2021). Men also can get
HIV from this process because of contact with
contaminated vaginal secretion and blood that carry
the HIV, which enters the body through the opening
penis, which is not circumcised (Cdc.gov. 2021). Oral
sex can also cause transmission if both sexual
partners have small cuts in the mouth and one of them
has HIV. However, HIV transmitted from female to
female is rare (Cdc.gov. 2021).
3.2.2 Transmission Via Blood
The risk of HIV infection from blood transfusions is
very rare worldwide (Avert. 2021). Nowadays, all
blood products (organs and tissues) are tested for the
presence of infections such as HIV. Blood transfusing
is the direct route of transmission (Avert. 2021).
Other factors that may cause direct contact in the
blood are tattoos or body piercings. However, sharing
needles, syringes, or other injection equipment also
puts people at risk for getting HIV. HIV particles can
survive on the syringes for nearly 42 days, depending
on storage temperature and other surrounding factors
(Abdala, Reyes, Carney, Heimer 2000), causing
infection through blood exchange. The use of
contaminated needles in hospitals is extremely rare,
and used needles are treated safely in hospitals
(Avert. 2021). HIV infection via contaminated
needles is a direct route among drug users (Cdc.gov.
2021). Therefore, the Government should increase
drug control, especially intravenous drugs, while
vigorously screening drug users within its jurisdiction
and testing them for HIV. Many of these addicts are
pregnant women, and the vast majority of their
infants become drug addicted to drug and are born
with HIV from birth.
3.2.3 MTCT (Mother to Child
Transmission)
MTCT, as a vertical propagation way of transmission,
is the most common way that children get HIV, which
occurs during pregnancy or breastfeeding. Without
any intervention, transmission rates range from 15%
to 45%
(https://www.who.int/hiv/topics/mtct/about/en.
2021). MTCT is relatively rare with HIV-2. During
pregnancy, the HIV hidden in blood can enter into the
baby’s body through the placenta and umbilical cord.
In addition, it is worth noting that infection can lead
to damage to other organs (cardiovascular, nervous,
bone and other tissues) in adults (Hazra, Siberry, &
Mofenson 2010).
3.3 Immune Response to HIV
At the beginning of HIV infection, the virus first
attacks the mucous membrane tissue of the cell and
then spreads to the lymphatic system (eclipse phase)
(Avert. 2021). About three weeks later, the genetic
material for HIV can be detected, and the virus begins
to proliferate and reach its peak (Avert. 2021). At this
acute phase, the spread of the virus can also be
partially controlled by the action of the adaptive
immune response. Patients show some flu-like
symptoms during the acute phase, which can last
about nine weeks, after which viral load reach the set
point, a stable level (Avert. 2021). Damage to CD4 T
cells caused by HIV viruses can lead to
immunodeficiency and chronic inflammation. After
up to nine years from the onset of infection, HIV
develops into AIDS, a period known as the latent
infection (Figure3). CD4 T cells in a normal adult
body are typically between 500 cells and 1500 cells
per μl (aidsmap.com. 2021); however, the number
frequency of CD4 T cells decreases after HIV
infection as the CD4+ T cell number declines to <350
cells per μl, opportunistic infections and cancers can
develop (Figure2).
Susceptibility to HIV and Strategies to Prevent AIDS
117
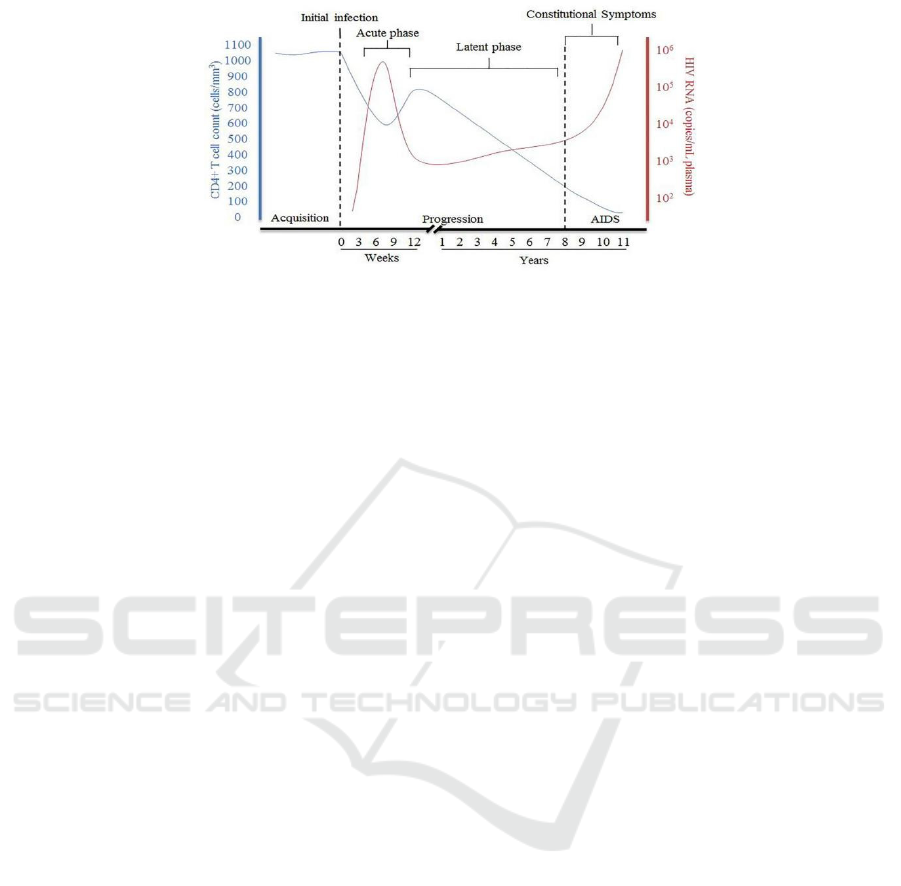
Figure 2. A graph demonstrating changes in the CD4+ T cell count and HIV viral load during the disease progression from
HIV to AIDS. The figure is adopted from (
An, Ping, and Cheryl A Winkler. 2010).
3.4 Diagnosis and Clinical Behaviors
Early HIV testing is significant, and if a patient is
HIV-positive, treatment options should be discussed
with the doctor as soon as possible, as well as
decreasing high-risk behaviors to decrease the virus
spread. The most important approach is to prevent
transmission to others during this period and
prioritizing the treatment. Many medical facilities
also offer anonymous and free counseling, including
asking patients about symptoms, psychological state,
medical history, and allergens. There are four main
HIV tests including, ELISA test, home test, saliva test
and viral load test (Parker, Botchan, and Berger
2021).
ELISA (enzyme-linked immunosorbent assay).
This test can be used to detect HIV infection. If an
ELISA test is positive, the Western blot test (blood
test) is usually administered to confirm the diagnosis.
ELISA is very sensitive to chronic HIV infection, but
because antibodies do not produce immediately after
infection, and the infected person may test negative
within weeks to months of infection. Even if the
person's test results turn negative in this window, the
infected person may have a high level of the virus and
is at risk of spreading the infection.
Home test: AIDS test paper is a new generation of
test reagents developed using colloidal gold
immunotomography technology to detect HIV-1/2
endemic antibodies in whole blood, serum or plasma
specimens. Test time is six weeks (42 days), and with
short operating time (generally 15-20 minutes to
observe the results), and without the need for
additional equipment, as well as a high accuracy rate
of 97% to 99%, this method is very fast, and efficient.
However, additional testing confirmation tests may
be required (Bhiva.org. 2021).
Saliva test, a piece of cotton in the test box is used
to collect saliva, which is sent to the laboratory to test,
and test results are usually available within three
days. Further blood tests are required if tested
positive. This test is only checking for antibodies, not
the actual disease (HowStuffWorks, Health,
Medicine and Treatment 2021).
Viral Load test measures the number of HIV
viruses detected in the body. Three techniques for
detecting HIV viral load: reverse transcription and
polymerase chain reaction (RT PCR), branched DNA
(bdna), and nucleic acid sequence based
amplification analysis (Nasba) (Tests 2021).
As mentioned previously, there are three stages
between the development of HIV and AIDS. Within
the acute infection phase, most infected people have
flu-like symptoms such as cough, fever, red rash,
muscle soreness and sore throat. Some people have
no symptoms during the early stage of HIV. If an
individual feels infected with HIV or recently
exposed to HIV, they need to do the HIV test
immediately. In the latent phase, viruses continue to
increase or mutate. Infected people may not feel
uncomfortable or have any symptoms at this stage.
Insisting on treatment at this stage can be effective in
suppressing the disease, but if not treated, it will
develop into the next stage of AIDS in about a decade
(Hivinfo.nih.gov. 2021). When the disease develops
into AIDS, the immune system is already very weak.
Symptoms can also be more severe than before. For
example, rapid weight loss , pneumonia, memory
loss, depression and other neurologic disorders
(Bhiva.org. 2021). At this stage, it is likely that a
small cold will threaten the patient's life. So, HIV
should be detected early and early treatment should
initiate to avoid AIDS.
4 TREATMENT & PREVENTION
As mentioned previously, a latent period occurs
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
118

before the development of HIV into AIDS, and such
progression be hindered by drug treatments. To this
day, there is no complete cure for HIV; however, six
families of antiretroviral drugs are used for
treatments: Non-nucleoside reverse transcriptase
inhibitors, nucleoside reverse transcriptase inhibitors,
protease inhibitors, fusion inhibitors, CCR5 receptor
antagonists and integrase inhibitors (Table 2 shows
below and Figure 3) (HIV.gov. 2021). Antiretroviral
drugs are often used in combination to prevent drug
resistance and multiple viruses from mutating in the
body in a timely manner (Hivinfo.nih.gov. 2021).
These drugs have many side effects, so many patients
cannot adhere long-term to their treatment, which is
also an important factor for the high prevalence of
HIV disease progression to AIDS. Only patients who
respond positively to the condition will cooperate
with their doctors. Maintaining a positive attitude is
also one of the important treatments for diseases.
Drugs are also very expensive, which is an important
reason for patients’ non-compliance.
Table 2. A summary of some of current antiretroviral drugs used for the treatment of HIV. The information in this table was
derived mainly from (Hivinfo.nih.gov. 2021), (Drugs 2021).
Inhibitors Mechanism of action Drug name Side effect
Non-
nucleoside
reverse
transcriptase
inhibitors
Directly inhibit the HIV-1 reverse
transcriptase by binding in a
reversible and non-competitive
manner to the enzyme
Efavirenz
Associated with
rashes including
Stevens-Johnson
syndrome
pPasma cholesterol
concentrations
Nevirapine
Occasionally with
fatal hepatitis
Protease
inhibitors
These inhibit HIV enzyme required
to produce mature infectious viral
particles by cleaving structural
proteins and enzymes from their
precursors.
Atazanavir
Cough, insomnia, depression, numbness of
hands and feet, etc.
Darunavir
Fatigue, anorexia, nausea, jaundice, darker
urine color
Indinavir
Multi-dream, urine pain, blood urine,
crystalline urine
Fusion
inhibitors
Inhibits HIV from fusing to the host
cell
Enfuvirtide
Insomnia, anxiety, peripheral neuropathy,
fatigue
CCR5
receptor
antagonists
Block the CCR5 receptor on the
outside of CD4 cells.
Maraviroc
Cough, stomach pain, or tiredness may
occur. Lightheadedness or dizziness
Integrase
inhibitors
Integrase inhibitor and is indicated in
combination with other antiretroviral
drugs for HIV infection resistant to
first-line ART.
Raltegravir
Trouble sleeping insomnia, headache,
dizziness, nausea, tiredness
Nucleoside
reverse
transcriptase
inhibitors
These inhibit the RNA-dependent
DNA polymerase (reverse
transcriptase) which HIV uses to
convert viral RNA into DNA before
its incorporation into the cell
genome.
Zidovudine
As the disease progresses, adverse
reactions increase
Abacavi
r
increased cardiovascular ris
k
Didanosine
Hair loss, allergic reactions, weakness,
pain, chills and fever
Stavudine Anemia, white blood cell deficiency
Susceptibility to HIV and Strategies to Prevent AIDS
119

Figure 3. An overview of antiretroviral therapy approaches used to tackle entry and propagation of HIV. The figure was
generated using Biorender.
Avoiding early HIV infection is the most effective
way to reduce the incidence of AIDS. The early
stages of avoiding infection require a holistic
approach from society and the government. The
following are some suggestions for preventive
measures for both individuals and government.
Personal:
1. Drug use should be strictly prohibited and
syringes are not shared with others.
2. Blood transfusion should be prohibited without
authorization, should be used under the guidance of a
doctor.
3. Personal items such as toothbrushes, razors,
shavers, etc. should not be shared.
4. Condom use as one of the most effective
preventive
measures in sexual life for the prevention
of diseases and AIDS should be encouraged.
5. Direct contact with the blood, semen and milk
of AIDS patients be avoided.
National and international recommendations are
as follows:
Awareness of HIV among the public should be
raised by organizing regular community events,
national awareness campaigns, TV and social media
advertisements, etc.
HIV education should be incorporated into school
and national education curriculum.
Discrimination and stigma against HIV should be
removed by raising awareness.
HIV drug prices should be subsidized and if
possible, free and anonymous HIV testing should be
available.
New needles should be supplied to drug abusers.
Condoms and other preventative measures should
become available in public places such as colleges,
universities, leisure areas, etc.
More funding should be invested on HIV
research.
4.1 Vaccines in the Future
Vaccines have traditionally been the most effective
means of preventing or even eradicating infectious
diseases. Vaccines are safe and cost-effective in
preventing various diseases, disabilities and death.
Similar to smallpox and polio vaccines, preventive
HIV vaccines can help save millions of lives.
Vaccines are synthesized using inactivated and
detoxified microorganisms, injecting treated bacteria,
viruses and toxins into the body to induce an immune
response to help the body fight infection more
effectively (HIV.gov. 2021). But so far, there has been
no vaccine that can completely cure HIV. The biggest
obstacle to the development of HIV vaccines is the
variety of genetic material of the virus. HIV not only
replicates quickly, but also tends to have a high error
rate, during which mutations can form a new type of
HIV virus; new HIV strains will also be re-integrated
in human-to-human transmission (Verywell Health.
2021). As conventional vaccines can only prevent a
limited number of strains, developing a single
vaccine that eradicates more than 60 dominant strains
and multiple recombinant strains worldwide becomes
even more challenging (Verywell Health. 2021).
Developing a safe, efficient, and affordable vaccine
to prevent HIV infection in uninfected people and end
the global spread of HIV is the highest priority of HIV
researchers. Recent research has shown that use
cytomegalovirus (CMV) as a vaccine vector can
protect against multiple infectious diseases including
simian immunodeficiency virus in rhesus macaques
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
120

(Barry, Peter A et al. 2020). This technology is
expected to be used in HIV in humans.
4.2 Susceptible People to HIV Infection
Groups
4.2.1 People Living in Sub-Saharan
Africa
Large generalized epidemics of HIV-1 is a potential
cause of mass mortality and morbidity in sub-Saharan
Africa (UNAIDS 2017). The World Health
Organization reported that almost 70% of the
population in sub-Saharan Africa live with HIV
(Gleason 2012). In addition, approximately 92% of
women and 90% of children living with HIV in the
sub-Saharan area (Ilo.org. 2021). As the availability
of antiretroviral therapy and male medical
circumcision has increased, the rate of new infections
has been reduced (Grabowski, et al. 2017). Despite
such progress, HIV still remains a major problem in
the sub-Saharan Africa region. Some natives still
keep eating uncooked meat, like chimpanzees (most
prevalent strains HIV-1 Group M originated from
these), causing exposure to primate blood (Avert.
2021). Chaotic sexual behavior is also one of the
main ways of transmission. A person with HIV may
have many sexual partners, and in the chronic phase,
the carrier of HIV may not notice, causing the virus
to spread. But in practice, far more people actually
have HIV than are recorded because many people
may fear discrimination or isolation, so they would
deliberately hide their illness or refuse to take HIV
tests. Some people even do not know about HIV and
how it spreads. Racial discrimination still exists in
many Sub-Saharan areas, and many black people fear
that white hospitals misdiagnose them, and many
white doctors do not want to visit and treat a black
man. This can lead to a crisis of confidence in the
local health care system, which reduces medical
efficiency. The class disparity is also one of the
reasons why the health care system of some African
countries is struggling under pressure. Many poor
people with HIV do not receive formal treatment, and
more and better medical resources are in the hands of
those with money and power. Poor people deserve
good housing and equal access to education, factors
that directly or indirectly increase the risk of HIV
infection. The best way to reduce the incidence of
HIV is to spread HIV knowledge across the board so
that everyone knows and understands the disease.
The second is to implement compulsory education
and formulate policies to make education compulsory
are free for all school-age children, similar to the
strategy adopted in China. Furthermore, the
availability of scholarships and bursaries as financial
incentives for school children can prompt their
parents to allow children to attend school. Finally,
there is the fight against the industry, which will be
mentioned in the next section.
4.2.2 Sex Workers
Sex workers are more likely than other groups to be
infected with HIV because of various reasons, such
as agreeing to high-risk sexual behaviors because of
financial incentives (Cdc.gov. 2021). While HIV
prevention programs are feasible for most people,
there are many barriers and discrimination for sex
workers, making them more than thirteen times more
likely to be infected with HIV than the general
population (Avert. 2021). Many sex workers are
discriminated and marginalized, often receive unfair
treatment, such as lack of access to HIV testing or
treatment, which can delay their treatments if they are
infected with HIV (Cdc.gov. 2021). They also have to
have sexual intercourse with various people, but in
some cases, they cannot convince their clients to use
preventative measures, which can make them prone
to infection. Furthermore, sex workers can be young
and lack sufficient knowledge about HIV; for
example, a study in Ukraine found that 20% of female
sex workers were aged between 10 and 19 (Silverman
2011).
5 CORRELATION WITH OTHER
DISEASE
The COVID-19 pandemic has affected almost
everyone’s lives since its spread in 2019. The
negative consequences of COVID-19 have been more
on some people compared to others. COVID-19 has
caused a huge challenge for people living with HIV
as well. Restrictions on travel and cargo transfer have
caused it more difficult to obtain drugs and treatments
available (BMC Public Health. 2021). Therefore,
while there have been some positive effects of the
COVID-19 pandemic on HIV due to a decrease in the
number of HIV cases due to restrictions on people
meeting each other and observing social distancing,
the availability of drugs has become a challenge too.
However, while there has been a global decrease in
HIV cases, some groups in populations still remain
prone to the disease, poverty, sexual exploitation,
food insecurity and drug abuse.
Beyond the disparity in catching the disease,
people with HIV are more susceptible to being
Susceptibility to HIV and Strategies to Prevent AIDS
121

infected with COVID-19 and facing severe
consequences due to a compromised immune system
(Cdc.gov. 2021). But at the same time, governments,
organizations and healthcare systems can learn many
lessons from the COVID-19 pandemic to fight HIV.
In this global fight against the epidemic, various
governments quickly responded to the public health
crisis and imposed strict measures to prevent the
spread of the disease. Additionally, public health
campaigns increased the public’s awareness about
COVID-19, helping to reduce disease transmission.
Furthermore, a global effort resulted in the
production of effective vaccines against SARS-CoV-
2 in an unprecedented time. The rapid development
of vaccines in this fight is also one of the most
important reasons for controlling the disease, and
government funding and researchers' efforts have
allowed the COVID-19 vaccine to be quickly
designed, synthesized, manufactured and be
approved by regulatory agencies. Additionally, the
development and availability of user-friendly
COVID-19 diagnosis kits have enabled rapid and
effective diagnosis to identify infected patients and
prevent further transmission of the disease. While
HIV is a complex disease, many lessons can be
learned from an infectious disease such as COVID-
19 to improve our public health strategies. For
example, a global effort supported by increased
funding and attention is required to find possible
vaccines. Moreover, the development of user-
friendly and accessible diagnosis kits can identify
infected patients to prevent HIV transmission.
Finally, effective public health campaigns can
remove the stigma of HIV and raise awareness of the
disease.
6 CONCLUSIONS
HIV is a major public health concern, which can
cause the development of AIDS and finally death if it
remains untreated. In comparison, the incident rate
has decreased in developed countries over the past
three decades, many developing countries, especially
those in the Sub-Sahara region struggle with the
disease. Even in developed countries, certain groups
within the population, such as those with lower
socioeconomic status, sexual workers, and drug
abusers are more prone to HIV than others. This
demonstrates a social disparity resulting in public
health inequality. Despite all advances in the
understanding of HIV over the past few decades,
more research is required to find better treatment with
fewer side effects in addition to global efforts to
develop vaccines against HIV. The COVID-19
pandemic can provide a fresh perspective in public
health strategies for combatting HIV and AIDS, and
many lessons can be learned at personal, national and
international levels.
REFERENCES
2021. [online] Available at:
<https://www.who.int/hiv/topics/mtct/about/en>
Abdala N, Reyes R, Carney JM, Heimer R. Survival of
HIV-1 in syringes: effects of temperature during
storageexternal icon. Subst Use
Misuse 2000;35(10):1369–83
aidsmap.com. 2021. Viral load. [online] Available at:
<https://www.aidsmap.com/about-hiv/viral-load>
aidsmap.com. 2021. CD4 cell counts. [online] Available at:
<https://www.aidsmap.com/about-hiv/cd4-cell-
counts>
Avert. 2021. Sex workers, HIV and AIDS. [online]
Available at:
<https://www.avert.org/professionals/hiv-social-
issues/key-affected-populations/sex-workers>
Avert. 2021. Blood transfusions & transplants and HIV.
[online] Available at: <https://www.avert.org/hiv-
transmission-prevention/blood-transfusions-
transplants>
Avert. 2021. Blood transfusions & transplants and HIV.
[online] Available at: <https://www.avert.org/hiv-
transmission-prevention/blood-transfusions-
transplants>
Avert. 2021. Origin of HIV & AIDS. [online] Available at:
<https://www.avert.org/professionals/history-hiv-
aids/origin>
Avert. 2021. Symptoms and stages of HIV infection.
[online] Available at: <https://www.avert.org/about-
hiv-aids/symptoms-stages>
Barry, Peter A et al. “Cytomegalovirus-vectored vaccines
for HIV and other pathogens.” AIDS (London,
England) vol. 34,3 (2020): 335-349.
doi:10.1097/QAD.0000000000002396
Bhiva.org. 2021. [online] Available at:
<http://www.bhiva.org/documents/Guidelines/Treatm
ent/2015/2015-treatment-guidelines>
Bhiva.org. 2021. [online] Available at:
<http://www.bhiva.org/documents/Guidelines/Treatm
ent/2015/2015-treatment-guidelines>
BMC Public Health. 2021. Consequences of COVID-19
crisis for persons with HIV: the impact of social
determinants of health - BMC Public Health. [online]
Available at:
<https://bmcpublichealth.biomedcentral.com/articles/1
0.1186/s12889-021-10296-9]>
Cdc.gov. 2021. COVID-19 and HIV | HIV Basics |
HIV/AIDS | CDC. [online] Available at:
<https://www.cdc.gov/hiv/basics/covid-19.html>
ICHIH 2022 - International Conference on Health Big Data and Intelligent Healthcare
122

Cdc.gov. 2021. HIV Transmission | HIV Basics |
HIV/AIDS | CDC. [online] Available at:
<https://www.cdc.gov/hiv/basics/transmission.html>
Cdc.gov. 2021. HIV Transmission | HIV Basics |
HIV/AIDS | CDC. [online] Available at:
<https://www.cdc.gov/hiv/basics/transmission.html>
Cdc.gov. 2021. Facts about HIV Stigma | HIV Basics |
HIV/AIDS | CDC. [online] Available at:
<https://www.cdc.gov/hiv/basics/hiv-
stigma/index.html>
Cdc.gov. 2021. HIV and Substance Use | HIV
Transmission | HIV Basics | HIV/AIDS | CDC. [online]
Available at: <https://www.cdc.gov/hiv/basics/hiv-
transmission/substance-use.html>
Cdc.gov. 2021. Sex Workers | HIV by Group | HIV/AIDS |
CDC. [online] Available at:
<https://www.cdc.gov/hiv/group/sexworkers.html>
Drugs, H., 2021. Efavirenz: MedlinePlus Drug
Information. [online] Medlineplus.gov. Available at:
<https://medlineplus.gov/druginfo/meds/a699004.html
>
Gleason K. HIV research in Sub-Saharan Africa: research
roundup. The Journalist’s Resource 2012. Available
at: https://journalistsresource.org/economics/hiv-aids-
sub-saharan-africa-research-roundup/
Grabowski, M. K. et al. HIV prevention efforts and
incidence of HIV in Uganda. N. Engl. J. Med. 377,
2154–2166 (2017).
Hazra, R., Siberry, G. K. & Mofenson, L. M. Growing up
with HIV: children, adolescents, and young adults with
perinatally acquired HIV infection. Annu. Rev. Med.
61, 169–185 (2010).
HIV.gov. 2021. Global Statistics. [online] Available at:
<https://www.hiv.gov/hiv-basics/overview/data-and-
trends/global-statistics>
HIV.gov. 2021. Symptoms of HIV. [online] Available at:
<https://www.hiv.gov/hiv-basics/overview/about-hiv-
and-aids/symptoms-of-hiv>
HIV.gov. 2021. HIV Vaccines. [online] Available at:
<https://www.hiv.gov/hiv-basics/hiv-
prevention/potential-future-options/hiv-vaccines>
HIV.gov. 2021. Symptoms of HIV. [online] Available at:
<https://www.hiv.gov/hiv-basics/overview/about-hiv-
and-aids/symptoms-of-hiv>
Hivinfo.nih.gov. 2021. FDA-Approved HIV Medicines |
NIH. [online] Available at:
<https://hivinfo.nih.gov/understanding-hiv/fact-
sheets/fda-approved-hiv-medicines>
Hivinfo.nih.gov. 2021. The Stages of HIV Infection | NIH.
[online] Available at:
<https://hivinfo.nih.gov/understanding-hiv/fact-
sheets/stages-hiv-infection>
HowStuffWorks, Health, Medicine and Treatment,
2021. How Does an Oral HIV Test Work?. [online]
HowStuffWorks. Available at:
<https://health.howstuffworks.com/medicine/tests-
treatment/oral-hiv-test>
Ilo.org. 2021. HIV/AIDS in Africa (Africa). [online]
Available at: <https://www.ilo.org/africa/areas-of-
work/hiv-aids/lang--en/index.htm>
Nyamweya S, Hegedus A, Jaye A, Rowland-Jones S,
Flanagan KL, Macallan DC. Comparing HIV-1 and
HIV-2 infection: Lessons for viral
immunopathogenesis. Rev Med Virol. 2013
Jul;23(4):221-40. doi: 10.1002/rmv.1739. Epub 2013
Feb 26. PMID: 23444290.
Online Biology Notes. 2021. Structure, genome and
proteins of HIV - Online Biology Notes. [online]
Available at:
<https://www.onlinebiologynotes.com/structure-
genome-proteins-hiv/>
Parker, M., Botchan, M. and Berger, J., 2021. Mechanisms
and regulation of DNA replication initiation in
eukaryotes.
Silverman JG. Adolescent female sex workers: invisibility,
violence and HIV. Arch Dis Child. 2011
May;96(5):478-81. doi: 10.1136/adc.2009.178715.
Epub 2011 Feb 28. PMID: 21357241.
Tests, M., 2021. HIV Viral Load: MedlinePlus Medical
Test. [online] Medlineplus.gov. Available at:
<https://medlineplus.gov/lab-tests/hiv-viral-load>
This picture adopt from An, Ping, and Cheryl A Winkler.
“Host genes associated with HIV/AIDS: advances in
gene discovery.” Trends in genetics : TIGvol. 26,3
(2010): 119-31. doi:10.1016/j.tig.2010.01.002
ucsfhealth.org. 2021. HIV Diagnosis. [online] Available at:
<https://www.ucsfhealth.org/conditions/hiv/diagnosis
>
UNAIDS. UNAIDS Data 2017, Document JC2910E.
http://www.unaids.org/
en/resources/documents/2017/2017_data_book (2017).
Verywell Health. 2021. Why Is It So Hard to Make an HIV
Vaccine?. [online] Available at:
<https://www.verywellhealth.com/hiv-vaccine-
development-4057071>
Verywell Health. 2021. Why Is It So Hard to Make an HIV
Vaccine?. [online] Available at:
<https://www.verywellhealth.com/hiv-vaccine-
development-4057071>
Who.int. 2021. HIV/AIDS. [online] Available at:
<https://www.who.int/health-topics/hiv-
aids#tab=tab_2>
Wikipedia. 2021. HIV - Simple English Wikipedia, the free
encyclopedia. [online] Available at:
<https://simple.wikipedia.org/wiki/HIV>
Wikipedia. 2021. HIV - Simple English Wikipedia, the free
encyclopedia. [online] Available at:
https://simple.wikipedia.org/wiki/HIV
Susceptibility to HIV and Strategies to Prevent AIDS
123
