
Research on Drug Therapy of Atherosclerosis
Yu Cao
1,*,† a
and Xiangrui Chen
2,† b
1
Southland Christian Schools CA, U.S.A.
2
Chengdu Foreign Languages School the International Department, Chengdu, Sichuan, China
†
These authors contributed equally
Keywords: Atherosclerosis, PCSK-9 Inhibitors, Marine Omega-3 Fatty Acids, Statin, Bio-Nanomedicines, Berberine.
Abstract: Atherosclerosis is a chronic inflammatory disease in which atherosclerotic plaque accumulated on the walls
of blood vessels and causes narrowing of the arteries. Atherosclerosis usually is asymptomatic in its early
stages, and may causes coronary artery disease, stroke, peripheral artery disease and renal failure in severe
cases. In general, the symptoms associated with atherosclerosis do not appear until after middle age. Most
elderly people who over 65-years-old have atherosclerosis of varying degrees, atherosclerosis is the leading
cause of death and disability in developed countries. The atherosclerotic process is very complex, to
participate in the cells and tissues, including epithelial cells, smooth muscle, monocytes, macrophage,
platelets, lipoprotein, growth hormone, cholesterol, fat and cytokines, etc. Based on these participated
mediators, cells and tissues, scientist developed many drugs to relief atherosclerosis. Prevention of
atherosclerosis generally includes a healthy diet, exercise, quitting smoking, and maintaining a healthy
weight. The drugs include Statins, aspirin, berberine and antiplatelet drugs. In addition to drugs, percutaneous
coronary intervention, coronary bypass surgery can also be used to treat atherosclerosis. Recently, scientists
focused on the “Bio-Nano” which provide more efficient approach to treat atherosclerosis. The advantages of
Nanomedicines are obvious and show its effective function in the clinically experiments, Nanomedicine
possess targeted positing systems and enter capillaries and flow freely in the blood circulation system. The
Nanomedicine with high future expectation worth showing to more people who suffer atherosclerosis. The
review article introduces several distinctive drugs which relief atherosclerosis based on the disease’s
pathogenesis, including their functions, detailed mechanism, how to play its function in human body.
1 INTRODUCTION
According to the global survey, one people has a
stroke among 12 people in China, there are about 2.7
million new cerebrovascular diseases every year, and
trend is increasing year by year, especially in rural
areas (Deright, Jorgensen, & Cabral, 2015). In the
United States, one person has a stroke among forty
people, the ischemic stroke accounts for 87%. The
recurrence rate of ischemic stroke is high, previous
report of Western stroke registries showed that the
cumulative recurrence rate within 5 years after stroke
was 17%-30%. (Carpenter, Ford, & Lee, 2010).
Although ischemic stroke has many etiologies or risk
factors, atherosclerosis is the main pathogenic factor,
especially in people over 5o years of age (Sanne,
Zinkstok, Ludo, & Beenen, et al. 2014).
a
https://orcid.org/0000-0003-0479-5544
b
https://orcid.org/0000-0003-0855-6727
Atherosclerosis, driven by the chronic inflammation
of the arteries caused by early endothelial dysfunction
and monocyte recruitment leading to the platelet
aggregation, gradually the plaque was formed with
the accumulation of cholesterol, lipid, or other blood
substance on the blood vessel wall, is the primary
cause of heart disease and stroke (Greenstein, Sun,
Calderon, Kim, Berman. 2000). In fact,
Atherosclerosis took place in people since adolescent
because of the transportation of oxygen and other
material to the rest of body make the arteries thicken
and harder, Healthy arteries are flexible and elastic
(Schreiber, Greenstein, Kim, Calderon, Berman,
1998), but over time, the walls in your arteries can
harden, a condition commonly called hardening of the
arteries. In westernized societies, it is the underlying
cause of about 50% of all deaths (Kim, Kang, Kwon,
440
Cao, Y. and Chen, X.
Research on Drug Therapy of Atherosclerosis.
DOI: 10.5220/0011214500003443
In Proceedings of the 4th International Conference on Biomedical Engineering and Bioinformatics (ICBEB 2022), pages 440-447
ISBN: 978-989-758-595-1
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

2005). To eliminates the patient’s conditions,
researcher developed several efficient drugs to relief
the Atherosclerosis, including statins, which lower
bad cholesterol as low-density lipoproteins, several
drugs such as PCSK-9 inhibition and Marine Omega-
3 Fatty Acids that promoting the cleanness of
cholesterol and the protection for fragile fibrous cap,
antiplatelet drug, and vasodilation drug, which all
researched and developed by the pathogenesis of the
atherosclerosis. These drugs matured during the long
period of applying and studying, But the bio-
Nanomedicine was still in the researching stage and
had profound meaning for atherosclerosis, with high
future expectations. Nowadays, many scientists,
especially Chung Hang Jonathan Choi research
interests include “Bio-Nano '' interactions, and bio-
nanomaterials, drug delivery (Davis, Mark,
Zuckerman, Jonathan, & E, 2010). The Bio-Nano
medicine provided a new perspective for scientists to
study the atherosclerosis, which was a more effective
approaches to help patients relieve. One more
important thing was that atherosclerosis was not a
disease that only affected human’s heart, it also had
subsequent impact on other organs, such as brain,
kidney, liver. Therefore, the information about
medicine that treated atherosclerosis was vital and
necessary for many people who had atherosclerosis or
not. The purpose of the review article was to
summarize different types of medicine and advanced
techniques around the world (Mulder, Jaffer, Fayad,
& Nahrendorf, 2014), because many European
countries, the amount of people who suffer
atherosclerosis increased by a dramatic rate. People
could get more advanced information about these
medicine from the article and know the basic
knowledge about the atherosclerosis, and how to
prevent the formation of atherosclerosis.
1.1 Atherosclerosis
Atherosclerosis is known as Arteriosclerotic Vascular
Disease (ASVD) which is considered an
inflammatory disease of the artery, which can thicken
and harden the arterial wall, and gradually lose
elasticity and narrow lumen in the artery. Injury to
endothelial cells in the artery provokes a series of
inflammatory responses (Nilsson, 2019). The
endothelial cells start to produce cell surface adhesion
molecules like VCAM-1, which can cause monocytes
and T-lymphocytes to adhere to the endothelial cells,
and let endothelial cells move downstream through
squeezing. The endothelial cells also change shape,
and elasticity, which increase the permeability to
fluid, lipids and leukocytes, especially the LDL
(Kang, Martinez, HJ Müller, & E Angléscano. 1997).
When these factors migrate into the intima,
monocytes differentiate into macrophages, which
begin to take up LDL. Macrophages retain the lipid
they take up, and as they become more lipid-laden,
they are referred to as foam cells. Finally, foam cells
will undergo apoptosis and die, but the lipid will
accumulate in the intima (Munro, 1988). That’s why
the fatty streak forms in the artery wall beneath the
endothelium. Over time, the fatty streak can evolve
into atherosclerotic plaques, or they can remain stable
or even regress. Slowly growing plaques expand
gradually due to accumulation of lipid in foam cells
and migration and proliferation of smooth muscle
cells, these slowly growing plaques are matured and
called fibrin caps, which are not prone to rupture. But
other plaque grows more rapidly as a result of more
rapid lipid ruptures, it can trigger an acute thrombosis
by activating platelets and the clotting cascade
(
Cunningham, Gotlieb, 2005).
In detail, atherosclerosis can be divided into three
diseases, including arteriosclerosis of small arteries,
arteriosclerosis in the middle layer and
atherosclerosis. The atherosclerosis appears with the
growth of age, and its rule usually occurs in the
adolescent periods and aggravates and comes on in
the middle and old age. and atherosclerosis is usually
asymptomatic in its early stages, but when it becomes
serious, may cause coronary artery disease, stroke,
peripheral artery disease and renal failure in several
cases (Kutikhin, Brusina, & Yuzhalin, 2013). The
pathogenesis of atherosclerosis is complex and has
not been fully elucidated, the main risk factors are
included hypertension, hyperlipidemia, smoking,
diabetes and genetic factors, the treatment plan for
various risk factors consist of appropriate physical
activity, intervention of lifestyle and food, as well as
drug and surgical treatment. Among them, the drug
therapy is the most effective and quick treatment for
atherosclerosis.
2 DRUG TYPES
Currently there are three kinds of medications that
have been put into use in order to treat atherosclerosis,
which are antiplatelet drugs, anticoagulants, and
cholesterol-lowering drugs.
Research on Drug Therapy of Atherosclerosis
441

2.1 Antiplatelet Drugs
Firstly are the antiplatelet drugs, medicines used to
reduce the aggregation of platelets in the blood
therefore preventing the formation of blood clots.
After the vascular endothelial injury, collagen is
exposed, and stationary platelets, platelet membrane
glycoprotein (GPlb), and von Willebrand factor (vWF)
is influenced, then blood platelets are activated and
show adhesive property. With the effect of platelet
activator, such as ADP, TXA 2, 5-HT and Adr,
platelet membrane receptors GPIIb/IIIa bind to
fibrinogen to form early thrombosis. During the
adhesion, a series of reactions take place, including
the metabolism of arachidonic acid (AA), with
production of TXA2. As the platelets absorb fibrin
network, the blood clot gradually develop into strong
platelet-fibrin mesh.
Aspirin, as one familiar name for a large number
of people, is considered as the most commonly used
oral antiplatelet drug. It works by irreversibly
inhibiting the cyclooxygenase enzyme (COX)
activity in the prostaglandin synthesis pathway
(PGH2). This prostaglandin is a precursor of
thromboxane A2 (TXA2) and PGI2. (Warner,
Nylander, & Whatling, 2011) Also being an epoxide
inhibitor, the inhibition on COX-1 is reversible using
Indobufen. As mentioned, TXA2, a synthetase, is
produced during the activation of platelets, which can
be controlled by a kind of thromboxane synthase
inhibitor called Ozagrel. Another medicine, tirofiban,
works by reversibly combining with platelet receptor
GPIIb/IIIa, preventing receptors and fibrinogen
coming together, therefore resisting platelet
aggregation. Tirofiban is very effective and highly
selective. In antithrombotic therapy, sometimes a
combination of drugs is required as different drugs
taking effects at different stages may be more
efficient.
2.2 Anticoagulants
Anticoagulants play an important role in restricting
clot formation at the injured site. Anticoagulants
mainly focus on thrombin, an important enzyme that
causes the final path of coagulation process, and
coagulation factor X, known as the intersection of
endogenous and exogenous coagulation systems.
They can be divided into thrombin direct (bivalirudin,
argatroban) and indirect (heparin) inhibitors, vitamin
K antagonists and factor Xa inhibitors (rivaroxaban,
apixaban). Direct thrombin inhibitors can inhibit both
fibrin-binding thrombin and free thrombin, while
indirect thrombin inhibitors can only work on free
thrombin. Xa factor, a kind of vitamin K - dependent
serine protease, is the speed-limiting factor in the
formation of thrombin. The inhibitors have a strong
inhibitory effect on both Xa factors and
prothrombinase complex. As the role of factor Xa
infers, the inhibition on factor Xa is thought to be
more effective than the effect of thrombin inhibitors.
(Viladrich, E Daudén Tello, Solano-López, FJ López
Longo, Samso, & P Sánchez Martínez, et al. 2016)
2.3 Cholesterol-lowering Drugs
There are also cholesterol-lowering medicines, which
are used to lower lipid level in the blood, particularly
the low density lipid (LDL) cholesterol. Statins is one
of the cholesterol-lowering medicines , including
simvastatin, atorvastatin, and pravastatin. Bile acid
sequestrants—colesevelam, cholestyramine and
colestipol—and nicotinic acid are other types of
medicine that may be used to reduce cholesterol
levels.
Among those, the statins are the first choice of
lipid-lowering drugs. HMG-CoA reductase is a rate-
limiting enzyme in the cholesterol synthase system.
By inhibiting it, statins can reduce cholesterol
synthesis, reduce cholesterol concentration in plasma
and tissue cells, promote the activity of
concentration-dependent LDL receptors, and
accelerate the catabolism of LDL. It can also reduce
the synthesis of very low density lipoprotein, which
is VLDL, and convert VLDL into LDL reduction.
Therefore, it is proven that statins can significantly
decrease TC and LDL levels, reducing TC levels by
30%-40% and LDL-C levels by 35%-45%.
3 PROVE TO CLEAR
SUBSTANCE
3.1 PCSK9 Inhibitor
Proprotein convertase subtilisin/kexin type-9 (PCSK-
9) is a key player in plasma cholesterol metabolism
that can bind to LDL-R at the liver and stimulates the
absorption and degradation of these receptors,
eventually lowering the receptors levels (Cameron,
Ranheim, Kulseth, Leren, & Berge, 2008). PCSK-9 is
a 72-kd protease, expressed highly in the liver with
three recognizable domains, an N-terminal pro
domain, a catalytic domain, and a carboxyl-terminal
domain of unknown function, and these can bind to
the LDL receptor on the surface of cells, when the
nuclear environment reach the acidic level, the
ICBEB 2022 - The International Conference on Biomedical Engineering and Bioinformatics
442
affinity of PCSK-9 for the LDL receptor increases by
nearly 150-fold, and PCSK-9 binds to the epidermal
growth factor (EPG) repeat A of the LDL receptor,
which known as a crucial for recycling of the LDL
receptor from endosome to the cell surface (Mabus,
Palmer, Prouty, Hornby, & Wade, 2010). Overall,
PCSK-9 disrupts the route of the LDL receptor,
making it miss the way to reach the cell surface.
So, the drug called PCSK-9 inhibitors can play its
function through inhibition of PCSK-9, the
degradation of LDL-R is prevented thereby
improving the absorption by the liver of LDL
cholesterol particles, which consequently leads to
lower LDL cholesterol plasma concentration (Norata,
Garlaschelli, Grigore, Raselli, Tramontana, &
Meneghetti, et al. 2010). For now, the PCSK-9
therapy is suitable in a wide range of patients
provided that they express LDL-R.
3.2 Marine Omega-3 Fatty Acids
Marine Omega-3 Fatty Acids are nutrients people get
from food or supplements that help build and
maintain a healthy body. They’re key to the structure
of every cell wall people have, also an energy source
and help keep heart, lungs, blood vessels and immune
system working the way they should. Based on the
function of Marine Omega-3 Fatty Acids, researcher
found the potentially possibility to relief
Atherosclerosis (Calder, 2012). Marine Omega-3
Fatty Acids can make the fibrous cap or plaque
become more stable, the patients who ingest Marine
Omega-3 Fatty Acids in a long time, the plaque from
patients are more likely to be type IV, which possess
well-formed necrotic core with an overlapping thick
fibrous cap, IV plaque can be considered a good
fibrous cap (Kühnast, van der Hoorn, JoséVan,
Havekes, Liau, & Jukema, et al. 2012). Marine
Omega-3 Fatty Acid also lowers the level of these
immune cells surrounding the plaque. Rupture of
plaque is an extremely acute occurrence that exposes
the plaque contents to the high prothrombotic
environment of the vessel lumen, which can lead to
myocardial infarction, stroke or another vascular
event. Also, inflammatory cells, including
macrophages, T cells, mast cells, are typically
abundant at such locations within thin and tender
fibrous cap that easier to rupture, and these cells can
produce a range of medicator and enzymes that can
thin and weaken the fibrous cap making the plaque
vulnerable and unstable (Eschen, Christensen, Toft,
& Schmidt, 2005). So essentially Atherosclerosis is
an inflammatory event called plaque that can rupture
and lead to a series of dangerous consequences.
Marine Omega-3 Fatty Acids can stabilize
atherosclerotic plaque by decreasing infiltration of
inflammation and immune cells, like
monocyte/macrophages and lymphocytes, into the
plaques or by decreasing the activity of these cells
once in the plaque to lower the possibility of rupture
of plaque. There are two crucial ones- EPA and DHA
which are primarily found in certain fish, ALA
(Alpha-Linolenic Acid), another Omega-3 Fatty
Acids, is found in plant sources such as nuts and seeds
(Calder, 2012). EPA and DHA give rise to resolving
which are anti-inflammatory and inflammation
resolving, and also affect production of peptide
mediators of inflammation.
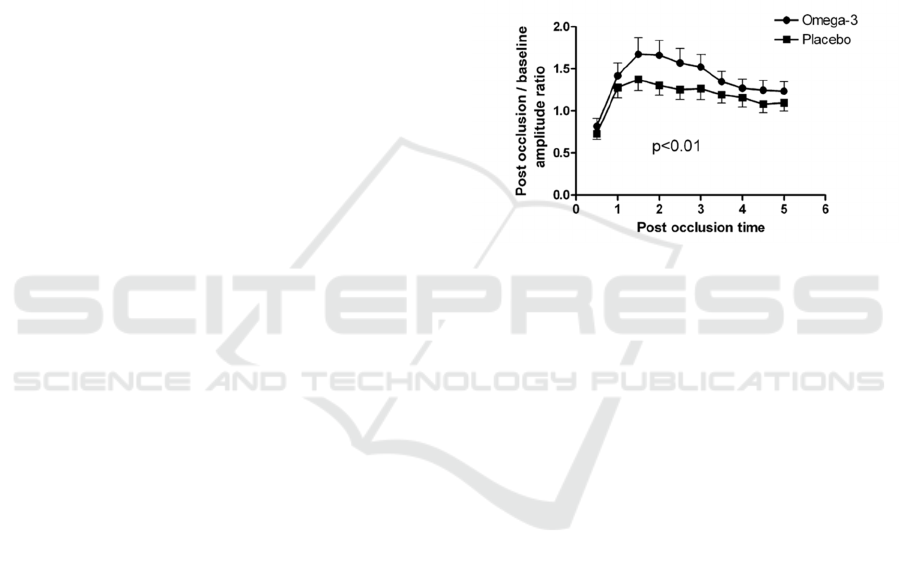
Figure 1: Vasodilatory response to reactive hyperemia after
omega-3 or placebo treatment. Pair-wise compared curves
using global fitting are shown (p = 0.01). Data points
represent mean ± SD. (Dangardt, Osika, Chen, & et al.
2010).
4 NEWTYPE DRUGS
4.1 Target Medications
Several nanomedicines are exemplified by the US
Food and Drug Administration’s approval for various
conditions. The main idea about nanomedicine is
about targeting specific substances in the blood, like
nonspecific targeting, specific targeting of the
vasculature, etc. Nanoparticle-facilitated therapeutics
can potentially be applied to target the liver and
change lipid levels systemically, or they can directly
inject the high density of lipoprotein nanoparticles to
enhance the transport of cholesterol in plaque to the
liver for excretion. And nanomedicine can deplete the
recruitment of monocytes or decrease plaque
inflammation and neovascularization (Tian, Lu,
Feng, & Melancon, 2018). Nanomedicine is a new
type and still developing medication.
Nanomedicine’s delivery systems can solubilize
drugs, improve drug half-life, improve drug
distribution in vivo and reduce toxic and side effects.
Research on Drug Therapy of Atherosclerosis
443

Bio-Nanomaterials is considered as a new strategy to
curing Atherosclerosis and the application of the
strategy to promote the specific delivery of
therapeutic molecules to atherosclerotic plaques is
under active investigation. A classic example is the
doxorubicin-containing liposome, the first Bio-
Nanomedicine approved by the United States Food
and Drug Administration for treating cancer in 1995
(Maranh, Tavares, AF Padoveze, Valduga, Oliveira,
& Rodrigues, 2006). Because Bio-Nanomedicine
contains partially or completely of biomolecules,
such as lipids, sugars and nucleic acid and proteins,
which is easier to control or develop the methods to
change the dimensional structure or the number of
biomolecules. An efficient approach to apply bio-
nanomedicine is to let the drug be injected into a lipid
which acts as a vector, and the drug-encapsulated
lipid could target the atherosclerotic plaques. In 2016,
Scientists (Kim, Rutka, & Chan, 2010) loaded
carmustine, a lipophilic chemotherapeutic, into lipid
NPs for targeting atherosclerosis plaques. They set a
series of experiments which inject the bio-
Nanomedicine into the atherosclerotic New Zealand
rabbits, and the drug-encapsulated NPs can reduce the
plaque size. But the method still was in the
experiment stage. Actually, all Bio-Nanomedicine
was applied based on the pathogenesis of
Atherosclerosis. The migration and death of
monocyte and macrophage can destroy local tissue of
architecture by secreting proteases and inflicting
oxidative stress on the vessel wall. And some
enzymes would digest the fibrous cap, thereby
initiating plaque rupture. So, the macrophage was
readily ingested nanomaterial and could be the prime
of target for novel therapeutics. Lobato et al.
(Lobatto, Fayad, Silvera, Vucic, Calcagno, & Mani,
et al. 2010) develop the methods of using bio-
nanomedicine to inhibit plaque macrophage
inflammation directly, they observed marked and
persistent plaque inflammation inhibition using a
liposomal nanoparticle containing glucocorticoids in
the atherosclerotic mouse.
One new study of Bio-Nanomedicine is using a
“camouflage” to inhibit the atherosclerotic plaque.
Because when strangers enter into the bloodstream in
a human's body, the immune system would start to
attack the drug and make it fail (Yamawaki, & Iwai,
2006). The methods used the methods that cover the
drug with the common cell membrane that the
immune system recognized and familied, and then
inject it into blood, the immune system still would
attack the drug but less than without the
“camouflage”. The Biomimetics nanometer therapy
(Rienzo, Jacchetti, F Cardarelli, Bizzarri, F Beltram,
& Cecchini, 2013) in the study is to read cell
membrane packages on the surface of nanodrugs,
implementation of nanodrugs “camouflage”, which
can effectively reduce the possibility that the body
system removes the nanodrugs, so that nanodrugs can
make long-term-nanodrug efficiency in the blood
circulation, thereby promoting nanodrugs targeting to
the pathological changes of atherosclerosis.
4.2 Berberine as an Antiatherosclerosis
Drug
Scientists have been also working on new type drugs
for higher effectiveness as atherosclerosis is still a
serious disease today. One of the existing drugs that
mainly works on digestive system has been found to
behave as a lipid-lowering drug. Berberine, which a
lot of studies have been done on, has antibacterial
effect on hemolytic streptococcus, Staphylococcus
aureus, Neisseria gonorrhoeae and Shigella dysentery,
etc., and can enhance leukocytophagocytosis. It has
varying degrees of inhibitory effect on tuberculosis
bacillus and yersinia pestis, and also has inhibitory
effect on amoeba in rats. With the strong support of
the National Natural Science Foundation of China,
the research team led by Dr. Jiang Jiandong, director
of the Institute of Medical Biotechnology of the
Chinese Academy of Medical Sciences, has made
breakthroughs in gene sequence, cell, animal
experiments and clinical treatment. The
pharmacodynamics, pharmacodynamics and
molecular mechanism of berberine in reducing blood
cholesterol and triglyceride were systematically
studied. They found that berberine lowers blood
lipids at the post-transcriptional level by acting on
mRNA (messenger RNA) that stabilizes LDL
receptors in the 3'UTR region, a mechanism
completely different from that of statins currently
used to reduce blood lipids. This provides a new
molecular target for finding new hypolipidemic drugs
in theory. Clinical studies have shown that oral
berberine (1 gram per day for 3 months) can reduce
cholesterol, low density lipoprotein and triglyceride
by 20% ~ 35% in patients with hyperlipidemia, which
has been further confirmed by hyperlipidemia golden
hamster model animal experiments. Dr. Jing Wei
from Nanjing First Hospital and Dr. Jingwen Liu
from Veterans Hospital paralto, California, USA,
both indicated that berberine may be a substitute for
statins, and is expected to be used in combination
with statins in the treatment of cardiovascular
diseases.
ICBEB 2022 - The International Conference on Biomedical Engineering and Bioinformatics
444
4.2.1 BBR Protect the Cardiac Muscles by
Raising the Concentration of Protein
Kinase of Ischemic Myocardia
The activated adenosine 5’-monophosphate-activated
protein kinase (AMPK), as the key particles in the
regulation of biological energy metabolism, can
restrain the consuming of adenosine triphosphate
(ATP). On the other hand, it can stimulate cells to
produce more ATP, therefore prolonging ATP supply
time within the cells, which plays a protective effect
to ischemic cardiac muscle cells.
Calcium ions are vital to the human body, because
they participate in the clotting process, muscle
contractions, neurotransmitter synthesis and release,
hormone synthesis and secretion, plus they are the
important elements in bone formation. When BBR
reduces the number of alpha-adrenergic receptors on
the membranes of the cardiac muscles, calcium influx
is inhibited, and cell apoptosis is blocked in order to
protect myocardial cells. (Cheng-Yi, H. U., & Zhi-
Xian, M. O)
4.2.2 Trials of Patients with Related
Diseases
According to a series of trials involving 874 patients
who had type 2 diabetes, hyperlipidemia,
hypercholesterolemia and related diseases. Ten
experiments were single-center experiments, and one
study was multi-center experiments. Patients with
type 2 diabetes were included in four studies. One
study recruited hyperlipidemia patients with type 2
diabetes. And there was a study of patients with
impaired glucose tolerance and hyperlipidemia.
Patients with hyperlipidemia were included in two
other studies. And another two studies included
patients with hypercholesterolemia. Besides, one of
the research projects included recruited patients with
polycystic ovary syndrome and insulin resistance.
Six studies randomly assigned participants to take
berberine under lifestyle changes and without
changes, and placebo with or without intervention.
According to experiment description, two trials
showed combined effects of berberine and oral
hypoglycemic agent with a controlled hypoglycemic
agent. Two others compared the combination action
of berberine and simvastatin with a simvastatin
control. One trial compared a combined intervention
of berberine and cyproterone acetate with placebo
plus cyproterone acetate. Two berberine preparations
were used in the inclusion trials, berberine chloride
tablets (used in 10 trials) and berberine chloride
liposome capsules (used in only 1 trial). Different
doses of berberine were used in these trials. The
intake of berberine is generally between 0.5-1.5 g per
day. Daily intake of berberine is divided into two or
three doses. The dose of berberine did not change
during the 8 trial periods. Three trials reduced the
dose of berberine when gastrointestinal discomfort
occurred during the study period.
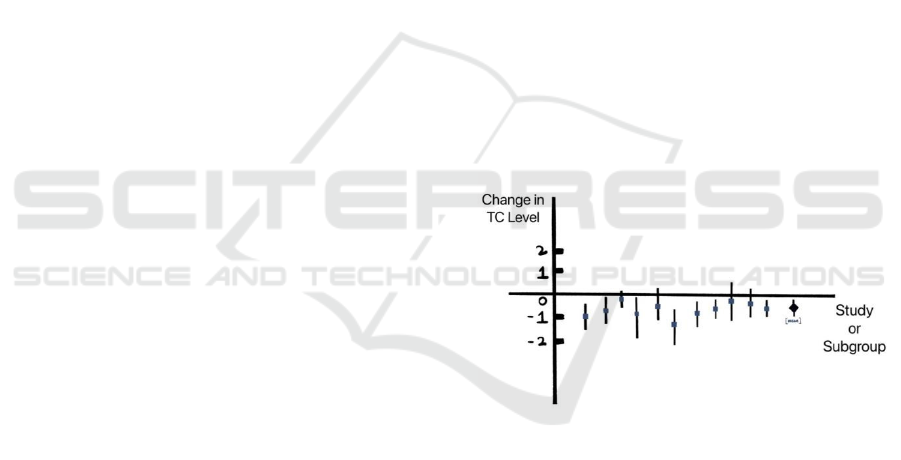
A comprehensive estimate of the effect of
treatment on lipid concentration is summarized in
Figure 3. There was significant statistical
heterogeneity in blood TC and TG results among
different studies (P <0.10). The results showed that
there was significant difference between the
berberine treatment group and the control group.
Berberine was significantly better than the control
group in improving blood TC (P < 0.00001;Md-0.61
easier/L;95% CI-0.83 ~ 0.39) and TG (P
<0.00001;Md-0.50 mmol/L: 95% CI-0.69 ~
0.31).There were no statistically significant
differences in LDL-C and HDL-C among tests (P >
0.10).Compared with the control group, the level of
LDL-C was significantly increased in patients taking
berberine (P <0.00001; Md-0.65 easier/L; 95% CI -
0.76 -- 0.54) and HDL-C (P =0.001;MD 0.05 easier/L;
95% CI 0.02 to 0.09).( Dong, H., Zhao, Y., Zhao, L.,
& Lu, F.. (2013)
Figure 2: Meta-analyse of the effects of berberine on total
cholesterol levels.
5 CONCLUSIONS
In conclusion, atherosclerosis is a chronic vascular
disease that usually occurs in the aorta and muscular
arteries, such as the coronary, cerebral, renal, and
carotid arteries (Stary, Blankenhorn, Chandler,
Glagov, Insull, & Richardson, et al. 1992). These
disease with high death rate were caused by
atherosclerosis, so the medication for reliving
atherosclerosis was more vital. Clinically, there are
many drugs used for the pathogenesis of
atherosclerosis, such as dyslipidemia and
hypertension, and their action pathways and targets
Research on Drug Therapy of Atherosclerosis
445

are different. Based on the dyslipidemia, which was a
basic pathogenesis of atherosclerosis, scientists
developed the drug called PCSK-9 inhibitor, which
inhibits the PCSK-9 that prevents the LDL receptor
bind with cholesterol. And statin was the most
common drug that was used in relieving
atherosclerosis, statin could lower cholesterol level,
its working process to block a specific substance that
participated in process making cholesterol. Drugs,
like statin, PCSK-9 inhibitor, antiplatelet medication,
were tested and already used for a long time (Taleb,
Witztum, & Tsimikas, 2011). They possessed high
stability and took advantage in the drug market. In
addition, different drugs can be used in combination
according to different mechanisms of action to
achieve better efficacy. Nowadays, some kinds of
bio-nanomedicine are undergoing development. They
achieve progress in the experimental stage, which
motivates people to study further and persist.
Scientists indicated the bio-Nanomedicine with
“camouflage” might potentially become the most
expectable drug (Stenosis, 1995), which reduces the
rejection phenomenon. Within the potentiality of bio-
nanomedicine, it would become the mainstream of
atherosclerosis, it is more precise and readily but still
undergoes experiment clinically. In the future, Bio-
nanomedicine may would be the mainstream to cure
or treat some diseases, which could provide more
efficient treatment for patients and more precise to
target its pathological position. Scientists might
should pay more attention on the accuracy of target
with the bio-nanomedicine and how to use magnetic
field to kill cancer cells.
REFERENCES
Carpenter, D. A., Ford, A. L., & Lee, J. M. . (2010). Patent
foramen ovale and stroke: should pfos be closed in
otherwise cryptogenic stroke. Current Atherosclerosis
Reports, 12(4), 251-258.
Cunningham, K. S., & Gotlieb, A. I.. (2005). Erratum: the
role of shear stress in the pathogenesis of
atherosclerosis. Laboratory Investigation.
Cameron, J., Ranheim, T., Kulseth, M. A. , Leren, T. P. , &
Berge, K. E. . (2008). Berberine decreases pcsk9
expression in hepg2 cells. Atherosclerosis, 201(2), 266-
273.
Calder, P. C. (2012). The role of marine omega‐3 (n‐3) fatty
acids in inflammatory processes, atherosclerosis and
plaque stability. Molecular Nutrition & Food Research,
56(7).
Calder, P. C. (2012). The role of marine omega‐3 (n‐3) fatty
acids in inflammatory processes, atherosclerosis and
plaque stability. Molecular Nutrition & Food Research,
56(7).
Cheng-Yi, H. U., & Zhi-Xian, M. O.. Research progress on
pharmacological actions and mechanism of berberine.
Chinese Journal of Experimental Traditional Medical
Formulae.
Deright, J., Jorgensen, R. S., & Cabral, M. J. . (2015).
Composite cardiovascular risk scores and
neuropsychological functioning: a meta-analytic
review. Annals of Behavioral Medicine, 49(3), 344-
357.
Davis, Mark, E., Zuckerman, Jonathan, & E., et al. (2010).
Evidence of rnai in humans from systemically
administered sirna via targeted nanoparticles. Nature,
464(7291), 1067-1070.
Dong, H., Zhao, Y., Zhao, L., & Lu, F.. (2013). The effects
of berberine on blood lipids: a systemic review and
meta-analysis of randomized controlled trials. Planta
Medica, 79(06), 437-446.
Dangardt, F., Osika, W., Chen, & Y., et al. (2010). Omega-
3 fatty acid supplementation improves vascular
function and reduces inflammation in obese
adolescents. ATHEROSCLEROSIS -AMSTERDAM-.
Eschen, O., Christensen, J. H., Toft, E. , & Schmidt, E. B. .
(2005). Soluble adhesion molecules and marine n-3
fatty acids in patients referred for coronary
angiography. Atherosclerosis, 180(2), 327-331.
Greenstein, S. M. , Sun, S. , Calderon, T. M. , Kim, D. Y. ,
& Berman, J. W. . (2000). Mycophenolate mofetil
treatment reduces atherosclerosis in the cholesterol-fed
rabbit. Journal of Surgical Research, 91(2), 123-129.
S Kühnast, van der Hoorn, José W.A., Van, d. H. A. M. ,
Havekes, L. M. , Liau, G. , & Jukema, J. W. , et al.
(2012). Aliskiren inhibits atherosclerosis development
and improves plaque stability in apoe*3leiden.cetp
transgenic mice with or without treatment with
atorvastatin. Journal of Hypertension, 30.
Kim, J. S., Kang, D. W. , & Kwon, S. U. . (2005).
Intracranial atherosclerosis: incidence, diagnosis and
treatment. Journal of Clinical Neurology, 1(1), 1-7.
Kang, C. , Martinez, C. , HJ Müller, & E Angléscano.
(1997). 2.p.121 binding of apo(a) isoforms to fibrin is
modified by their incorporation into an ldl lipoparticle.
Atherosclerosis, 134(1), 142-142.
Kutikhin, A. , Brusina, E. , & Yuzhalin, A. E. . (2013). A
Hypothesis of Virus-Driven Atherosclerosis. Springer
New York.
Kim, B. , Rutka, J. T. , & Chan, W. . (2010). Nanomedicine
— NEJM.
Kunde, S. S., & Wairkar, S. . (2021). Platelet membrane
camouflaged nanoparticles: biomimetic architecture for
targeted therapy. International Journal of
Pharmaceutics, 598, 120395.
Lobatto, M. E., Fayad, Z. A. , Silvera, S. , Vucic, E.,
Calcagno, C. , & Mani, V. , et al. (2010). Multimodal
clinical imaging to longitudinally assess a nanomedical
anti-inflammatory treatment in experimental
atherosclerosis. other, 7(6).
Mulder, W. J. M., Jaffer, F. A. , Fayad, Z. A. , &
Nahrendorf, M.. (2014). Imaging and nanomedicine in
inflammatory atherosclerosis. Science Translational
Medicine, 6(239), 239sr1.
ICBEB 2022 - The International Conference on Biomedical Engineering and Bioinformatics
446

Munro, J.. (1988). The pathogenesis of atherosclerosis:
atherogenesis and inflammation. Lab Invest, 58.
Maranh O, R. C. , Tavares, E. R. , AF Padoveze, Valduga,
C. J. , Oliveira, T. V. , & Rodrigues, D. G. . (2006). Wh-
w49:7 paclitaxel associated with a lipidic nanoemulsion
(lde) promotes atherosclerosis regression in the rabbit.
Atherosclerosis Supplements, 7(3), 466-466.
Mabus, J. R. , Palmer, J. M. , Prouty, S. M. , Hornby, P. J. ,
& Wade, P. R. . (2010). Methods of modulating
intestine epithelial functions. Janssen Pharmaceutica.
Norata, G. D. , Garlaschelli, K. , Grigore, L. , Raselli, S. ,
Tramontana, S. , & Meneghetti, F. , et al. (2010).
Effects of pcsk9 variants on common carotid artery
intima media thickness and relation to apoe alleles.
Atherosclerosis, 208(1), 177-182.
Nilsson, J. ,. . (2019). Cytokines and smooth muscle cells
in atherosclerosis.
Poston R . TREATMENT OF ATHEROSCLEROSIS: US,
WO2006032905 A1[P]. 2006.
Rienzo, C. D. , Jacchetti, E. , F Cardarelli, Bizzarri, R. , F
Beltram, & Cecchini, M. . (2013). Unveiling lox-1
receptor interplay with nanotopography:
mechanotransduction and atherosclerosis onset.
Scientific Reports, 3, 1141.
Sanne, M., Zinkstok, Ludo, F., & Beenen, et al. (2014).
Early deterioration after thrombolysis plus aspirin in
acute stroke. Stroke, 45(10).
Schreiber, T. C. , Greenstein, S. M. , Kim, D. Y. , Calderon,
T. M., & Berman, J. W.. (1998). Effect of
mycophenolate mofetil on atherosclerosis in a rabbit
model: initial histologic and immunohistochemical
analyses. Transplantation Proceedings, 30(4), 961-962.
Stary, H. C., Blankenhorn, D. H., Chandler, A. B., Glagov,
S., Insull, W., & Richardson, M. , et al. (1992). A
definition of the intima of human arteries and of its
atherosclerosis-prone regions. a report from the
committee on vascular lesions of the council on
arteriosclerosis, american heart association.
Circulation, 85(1), 391-405.
Stenosis, E.. (1995). Executive committee for the
asymptomatic carotid atherosclerosis study. jama.
Tian, L., Lu, L. , Feng, J. , & Melancon, M. P. . (2018).
Radiopaque nano and polymeric materials for
atherosclerosis imaging, embolization and other
catheterization procedures. Acta Pharmaceutica Sinica
B, 8(003), 360-370.
Taleb, A., Witztum, J. L., & Tsimikas, S.. (2011). Oxidized
phospholipids on apob-100-containing lipoproteins: a
biomarker predicting cardiovascular disease and
cardiovascular events. Biomarkers in Medicine, 5(5),
673-694.
Viladrich, I. M., E Daudén Tello, G Solano-López, FJ
López Longo, Samso, C. T., & P Sánchez Martínez, et
al. (2016). Consensus document on prevention and
treatment of tuberculosis in patients for biological
treatment. Archivos De Bronconeumologia, 52(1), 36-
45.
Warner, T. D., Nylander, S., & Whatling, C.. (2011). Anti-
platelet therapy: cyclo-oxygenase inhibition and the use
of aspirin with particular regard to dual anti-platelet
therapy. British Journal of Clinical Pharmacology,
72(4), 619-633.
Yamawaki, H., & Iwai, N. (2006). Mechanisms underlying
nano-sized air-pollution-mediated progression of
atherosclerosis. Circulation Journal, 70(1), 129-140.
Zhang, L., & Nichol, M. B. (2007). Ao1 medication
compliance to statin therapy and its impact on disease
outcomes in type 2 diabetes. Value in Health, 10(3),
A6-A6.
Research on Drug Therapy of Atherosclerosis
447
