
Personalized Nutritional Guidance System to Prevent Malnutrition in
Pluripathological Older Patients
Jordi Torres
1
, Garazi Artola
1,2,3
, Nekane Larburu
1,2
, Amaia Agirre
4
, Elixabete Narbaiza
4
,
Idoia Berges
3
and Ainhoa Lizaso
1
1
Vicomtech Foundation, Basque Research and Technology Alliance (BRTA), Mikeletegi 57,
20009 Donostia-San Sebastián, Spain
2
Biodonostia Health Research Institute, (Bioengineering Area), eHealth Group, 20014 San Sebastián, Spain
3
Computer Languages and Systems Department, Faculty of Informatics, University of the Basque Country UPV/EHU,
20018 Donostia-San Sebastián, Spain
4
Grupo Ausolan, 20500, Arrasate, Spain
Keywords: Decision Support System, Nutritional Recommendation, Malnutrition, Comorbidity, Ageing.
Abstract: Malnutrition is a frequent problem in the elderly population, who usually is affected by one or more
pathologies. The health status of these patients can get worsened if malnutrition is left untreated. Nutritional
guidelines have been developed to fulfil the nutritional needs derived from certain pathologies, but still are
not easy to use. Digital tools can help implement and use these guidelines in real clinical scenarios. Current
solutions are designed around a single pathology or specific scenario, but the pluripathologic scenario presents
a challenge when it comes to provide nutritional support. In this paper, we present an adaptative tool that
provides personalized nutritional recommendations for pluripathological patients in an efficient way, and can
be extended to include other pathologies.
1 INTRODUCTION
Nutrition is often focused on healthy habits to prevent
obesity, diabetes and other diseases. However,
advanced age brings with it a series of physiological
(e.g., swallowing problems or inability to prepare the
meals) and psychological (e.g., social isolation)
changes that predispose people to inappropriate
eating habits and/or imbalances between nutrient
intake and the needs of the individual for an optimal
physical status that leads in malnutrition (Agarwal,
Miller, Yaxley, & Isenring, 2013). In addition,
pathological problems (e.g., several medications) that
accompany aging are considered one of the main
reasons negatively affecting the motivation to eat and
thus being possible causes of malnutrition within
elderly population. It is triggered by loss,
dependency, loneliness, and chronic illness, and
potentially impacts on higher morbidity and
mortality. Without intervention, it presents a
downwards trajectory leading to poor health and
decreased quality of life. That is why it is essential to
consider new multidisciplinary approaches and the
use of nutritional formulas to solve disease-related
malnutrition, as it is a health problem of high
prevalence and high costs for public health.
Nutritional guidelines have been developed to
cope with the needs related with specific pathologies
(NHLBI, 1998; Kushi, et al., 2012; Joint WHO/FAO
Expert Consultation on Diet, Nutrition and the
Prevention of Chronic Diseases, 2003). However, this
type of traditional nutrition evaluations not only
require the use of numerous tables and lists to provide
sufficient nutritional recommendations for each
patient, but are also very time-consuming due to
cross-referencing and calculations (Kuo, et al., 2018).
In this context, digital tools can help to develop more
competitive and personalized nutritional
recommender systems.
Different approaches have been recently carried
out with the objective of offering this type of decision
support systems both to patients (direct end-users) or
to health professionals or caregivers. For instance,
this recent study (Taweel, et al., 2016) presents the
design of a system that enables homecare
management in the context of self-feeding and
malnutrition prevention through balanced nutritional
338
Torres, J., Artola, G., Larburu, N., Agirre, A., Narbaiza, E., Berges, I. and Lizaso, A.
Personalized Nutritional Guidance System to Prevent Malnutrition in Pluripathological Older Patients.
DOI: 10.5220/0011113700003188
In Proceedings of the 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2022), pages 338-343
ISBN: 978-989-758-566-1; ISSN: 2184-4984
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
intake. The design employs a service-based system
that incorporates several services including
monitoring of activities, nutritional reasoning for
assessing feeding habits, and diet recommendation
for food planning. In another study (Kuo, et al.,
2018), a clinical nutritional information system was
implemented to help hospital dietitians perform their
daily work more effectively in terms of time
management and paper work. The system mainly
targets in-patients who require cancer-nutrition
counselling.
As far as we can find in the state of the art, some
studies focus their work in supporting patients that
suffer from a specific disease or health problem
(Paulsen, Varsi, & Andersen, 2021), while the others
use patients’ general information (e.g., demographic
or socioeconomic data) without considering any
clinical data (Leipold, et al., 2018). Nevertheless, the
clinical information or health status of an older adult
is a variable that is essential to be considered for
obtaining a reliable nutritional recommendation. In
this sense, approaches that support not only single
pathologies but different combinations of
comorbidity cases are needed.
In addition, the use of technologies that pursue
knowledge sharing and interoperability is more and
more important in this kind of DSSs. That is why
recent approaches integrate semantic web
technologies into their systems (Espín, Hurtado, &
Noguera, 2016), allowing the inference of new
knowledge that could not be extracted from
traditional nutritional databases.
In this paper, the implementation of a solution that
offers personalized nutritional recommendations
taking into account not only the personal information
(e.g., malnutrition risk, gender) but also the
comorbidity profile of an elderly patient is presented.
This solution provides health professionals and
caregivers with a nutritional decision support system
that considers not only the different nutritional needs,
but also the whole environment of an elderly patient,
such as socio-demographic factors (e.g., sex, age...),
psychosocial factors (e.g., psychosocial disorders),
and morbidity factors (diseases).
2 METHODOLOGY
In this study we present the following approach to
develop a personalized nutritional guidance system,
which consists in three different modules: (i)
nutritional recommendations for each patient profile,
(ii) nutritional rule flow to generate the personalized
recommendations and (iii) nutritional ontology for
standardize the nutritional knowledge across the
platform.
2.1 Nutritional Recommendations
Nutritional guidelines were developed along with
experienced nutritionists on the domain. These
recommendations were generated for a set of possible
profiles considering i) the age and sex of the user, ii)
the malnutrition risk, iii) the need for texture adapted
meals, and iv) the intake level.
The structure of the recommendation provided by
our solution is divided as follows:
• Diet: Daily intake of several nutrients such as
carbohydrates, fats, cholesterol, proteins, fiber,
liquids, or salt; and daily caloric and protein
distribution.
• Fortification: Complement meals that help
reach the daily caloric and protein intake
values. These caloric and protein enrichments
are given by means of natural foods. If natural
fortification is not possible, it is carried out
artificially, through protein and/or caloric
modules.
• Food and liquid adaptation: Mainly texture
adaptations in order to ease the swallowing
process (i.e., solid food grinding). If these
adaptations entail low energy and nutritional
intake, Enteral Nutrition is recommended. In
case the patient's intestinal tract is not
functional, Parenteral Nutrition is prescribed.
• Supplementation: Recommendation of specific
oral nutritional supplements such as
hypercaloric and hyperprotein formulas.
• Enteral nutrition: Recommendations for
patients in need of enteral nutrition.
• Follow-up: Re-evaluation of the nutritional
status. For instance, the continuation,
reduction, or withdrawal of the
supplementation can be considered in this area.
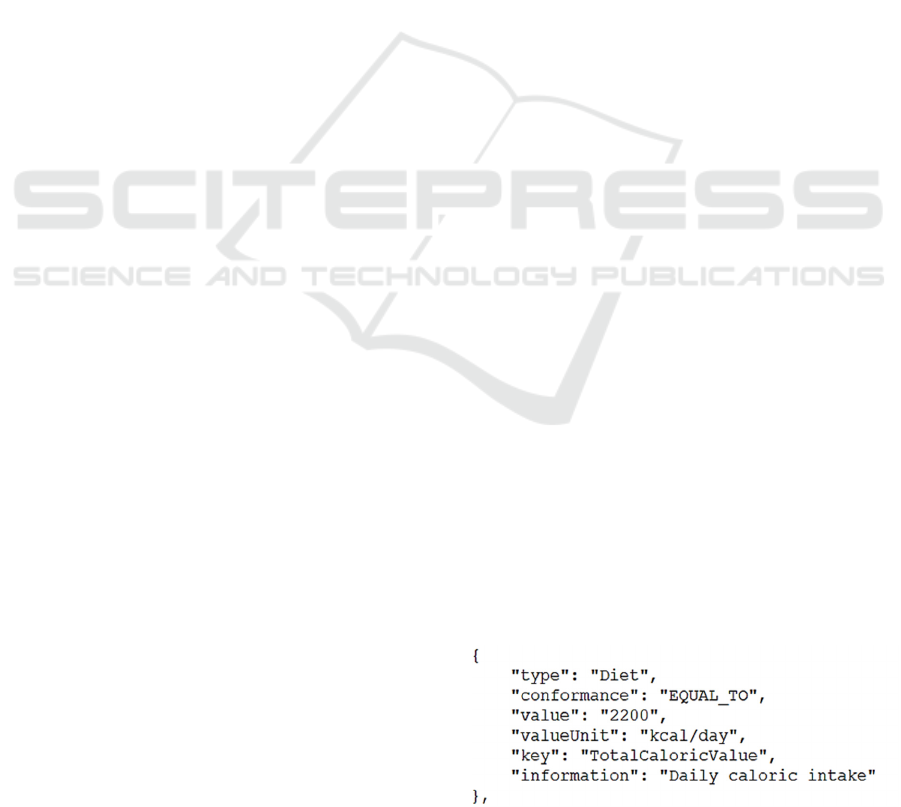
Each of these areas is formed by different
attributes. For instance, the Diet area is divided into
different recommendations, each one containing the
specific information about a different nutrient (see
Figure 1).
Figure 1: Example of a diet recommendation.
Personalized Nutritional Guidance System to Prevent Malnutrition in Pluripathological Older Patients
339
The presented structure is the core of the
nutritional recommendations. For each pathology and
user profile included in our platform, the first step
was to develop a complete set of recommendations
for the single pathology case. In the following step,
the combination of pathologies was tackled, taking
the single pathology case plans as the basis. In these
pluripathological cases, the nutrition plans were
generated by i) the combination of single pathology
nutrition plans (i.e., nutritional needs from pathology
1 and supplement intake from pathology 2, ii) the
generation of specific plans for each combination of
pathologies, and iii) the re-use of the nutrition plans
generated for the monopathological case if no
adaptation needs to be done for a specific
pluripathological case.
These recommendations are represented in a more
visual form to the users in a web application described
in Section 3. In Section 2.2 a detailed explanation on
how the generated nutritional recommendations were
introduced in a rule flow process is presented, for
both single and pluripathological cases.
2.2 Nutritional Rule Flow
The business logic of the presented platform consists
of a business process combined with a rule engine that
evaluates the patients’ data and generates the
personalized recommendation in return. The logic
implemented in this process consists, overall, on a
series of nodes that direct the process execution to the
set of nutrition recommendations that belong to the
pathology or combination of pathologies of the
evaluated patient. The specific recommendation is
generated based on the input data, as the rule engine
evaluates it and returns the nutritional
recommendation triggered by the patients’ data.
Our work is based on the previous work carried
out in (Torres, Artola, & Naiara, 2020) where a
platform for the development of domain independent
rule based clinical decision support systems (CDSS)
is described. From that starting point, jBPM processes
were included in the developed rule engine (Drools).
The BPMN Eclipse plugin was used to design and
implement the flows, and to link them with the
generated rules.
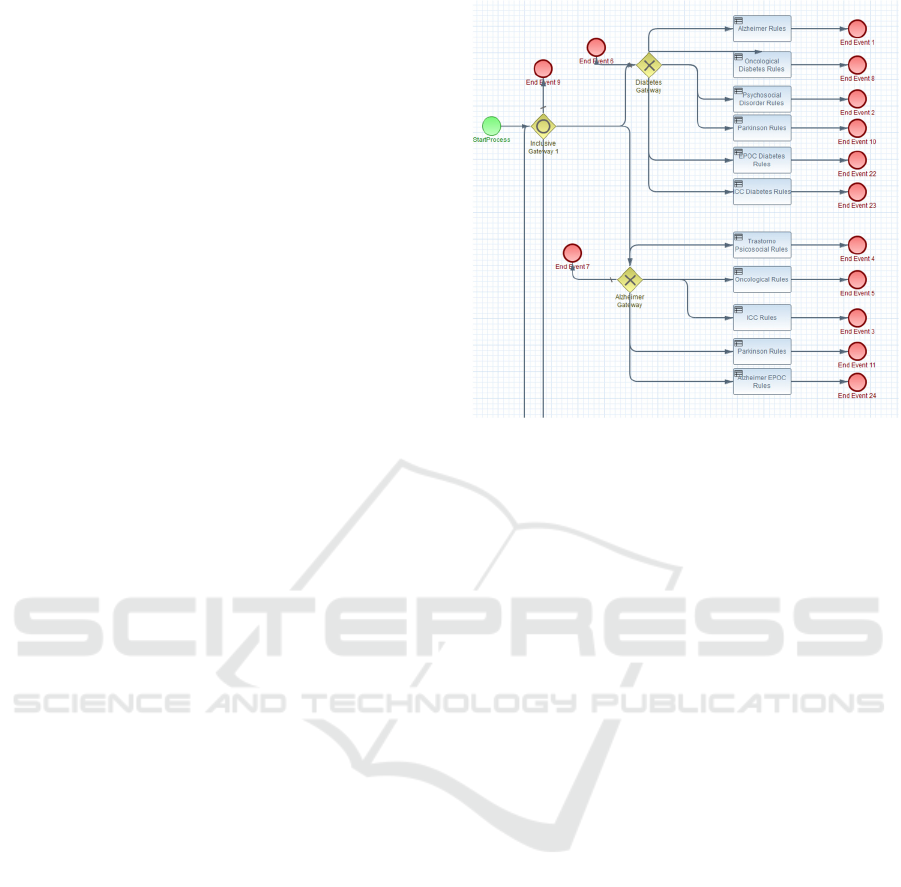
Three flows were configured, one for patients
with one pathology, and the rest for pluripathological
patients suffering from 2 or 3 of the included
pathologies. The general structure of the flows is the
same, an entry node, a set of decisional gateways and
business rule tasks, and the end nodes for each
possible pathological pathway (see Figure 2).
Figure 2: jBPMN process for the combination of 2
pathologies. Example of the combinations with Diabetes
and Alzheimer.
The path followed to reach an end node is what
we have called pathological pathway, theoretically,
for each pathology and its combinations, a
pathological pathway would need to be defined along
with its defined set of rules, but our solution reduced
the final amount of sets of rules needed by making
use of the execution of specific rule flow groups in
more than one pathway. The cases where the
nutritional recommendations coincide were grouped
under the same rule group attribute, reducing the total
amount of nutrition plans and rules that were needed
and avoiding duplicates.
2.3 Ontology
An ontology was developed for the nutrition
recommendations formalization process. The
variables formalized were differentiated between the
variables related with the patient and the ones related
with the nutritional recommendation. The ontology
was generated using Protégé, and it can be easily
updated with new pathologies apart from the ones
specified in Section 3.
The ontology was used as the basis from which to
formalize the diets generated by the nutritionist into
business rules. Due to the vast number of
recommendations that were entered into the system,
the use of an ontology reduces the risk of human
errors in the formalization process.
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
340
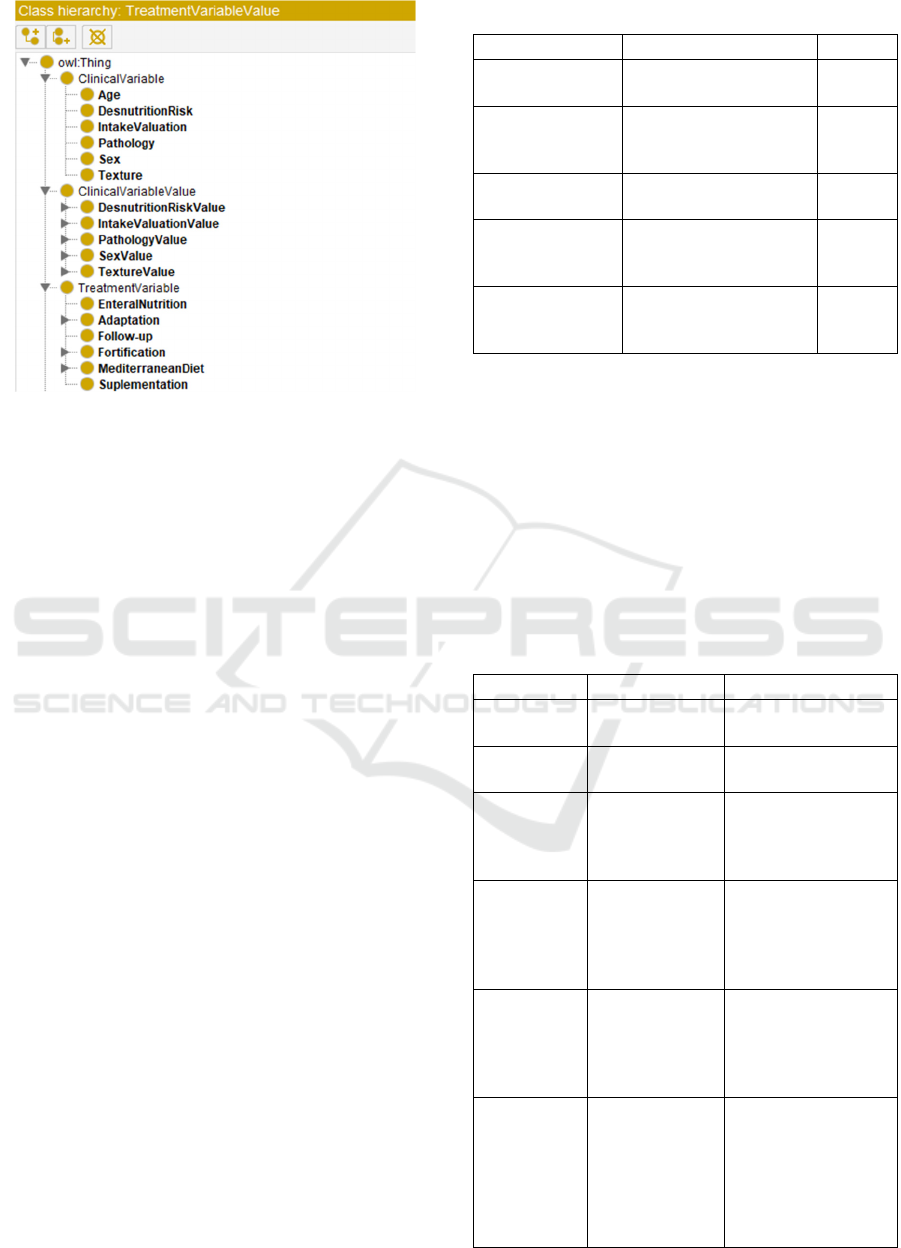
Figure 3: Structure of the ontology used to formalize the
nutrition recommendations.
3 USE CASE
The presented solution was developed within the
NUTRIGEP project. In this project, a platform for the
management of elderly pluripathologic patients at
risk of suffering malnutrition was developed. The
main goals of the project are i) to determine the
prevalence of malnutrition in admitted patients, ii) to
analyse the possible relationship between different
risk factors and the nutritional status of patients
during admission, and iii) to correct each diagnosed
malnutritional state through the management and
personalization of diets and specific
recommendations of food and/or supplements. The
solution hereby presented corresponds with the third
goal in charge of providing the specific nutritional
recommendations that aim to improve the nutritional
state of the users.
The pathologies that were included in the
NUTRIGEP platform are representative of the ones
present among the elderly, chronic patients of the
Asunción Klinika (Tolosa, Spain), the hospital
involved in the project: diabetes, Alzheimer,
Parkinson, Chronic Obstructive Pulmonary Disease
(COPD), cardiac failure, cancer and psychosocial
disorders. For each of the included pathologies and its
combinations, a nutrition plan was developed (see
Section 2.1), and modelled into the rule flow process
(see Section 2.2). Combinations of pathologies were
limited to all possible combinations up to 3
pathologies in order to set the number of possible
diets.
Table 1: Summary of Nutrigep use case data.
Item Description Amount
Pathologies Pathologies considered
in Nutrigep
7
Possible
pathology
combinations
Total amount of
possible combinations
of pathologies
63
Nutrition plans Amount of generated
nutrition plans
21
Nutrition
recommendations
/plan
Amount of
recommendations per
nutrition plan
378
Total nutrition
recommendations
Total amount of
recommendations of the
Nutrigep platform
7938
The Nutrigep project is aimed at a specific
population, the elderly. Due to this, for the
development of the recommendations a minimum age
of 65 was considered. The other factors taken into
consideration to provide personalized nutrition
recommendations were the sex, risk of malnutrition,
need for food and liquid adaptation, the pathology(es)
of the patient and a valuation of the quantity of food
eaten normally by the user (see Table 2 for more
detail).
Table 2: Description of patient’s data used in the Nutrigep
project.
Variable Description Values
Age Age of the
patient
>65
Sex Sex of the
patient
Male/Female
Risk of
malnutrition
Qualitative
assessment of
risk of
malnutrition
High / medium / low
Pathology Pathology or
combination of
pathologies
Alzheimer / Diabetes
/ COPD / Cardiac
failure / Psychosocial
disorders / Cancer /
Parkinson
Intake
valuation
Qualitative
estimation of
the amount of
food consumed
by the patient
Appropriate /
Moderate / Low
Texture Texture
adaptations
needed by the
patient
Normal / Soft /
Lightly thickened /
Little thick / Wet
chopped / Blended-
moderately thickened
/ Extremely thick
mash/pudding
Personalized Nutritional Guidance System to Prevent Malnutrition in Pluripathological Older Patients
341
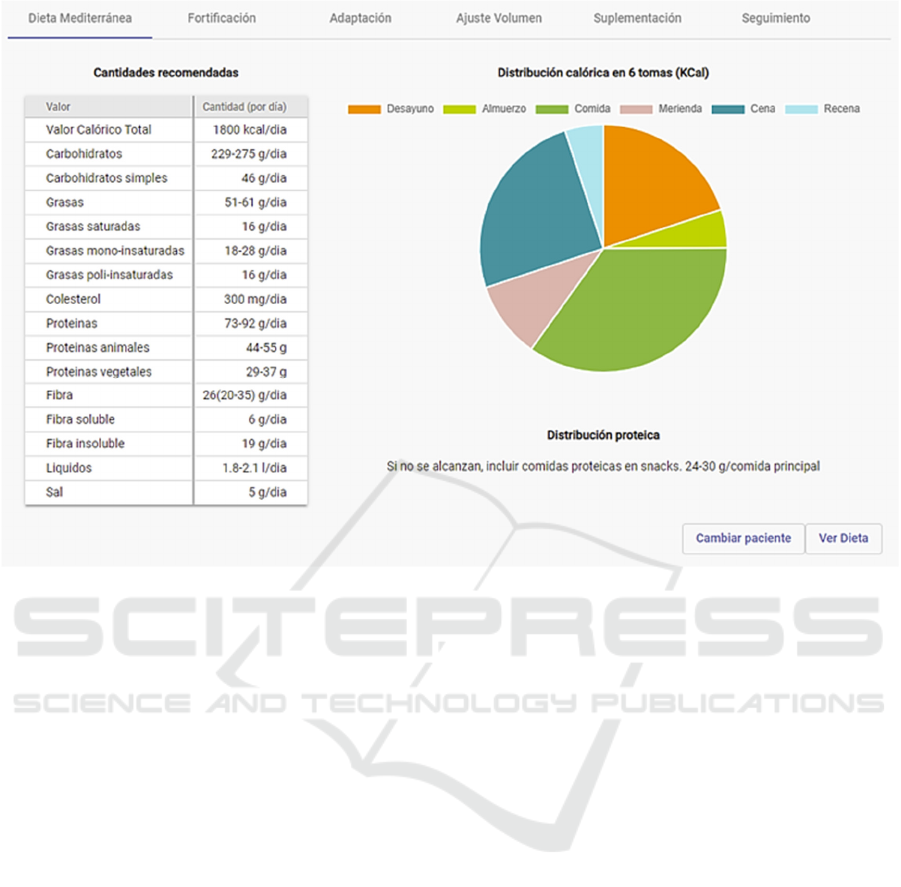
Figure 4: Example of the visualization of a nutritional recommendation in the Nutrigep web application for health
professionals.
The personalized nutritional recommendations
are visualized in a web application designed for
health professionals to aid them in the management
of their patients, where the developed
recommendation system was integrated. In this
platform, the clinicians can select the patient they
need to evaluate from the list of all the patients in the
database, and receive the personalized nutritional
recommendations given by our solution (Figure 4).
The clinical value of this recommender system
will be assessed in a clinical validation study that will
be carried out in Asuncion Klinika. This validation
will enrol twenty older patients suffering from one or
more of the pathologies included in the developed
system. The health professionals responsible for these
patients will access the web platform developed for
the Nutrigep project and enter the data of the patients
for the generation of personalized nutritional
recommendations. In the following three months, the
health status of the patients will be monitored and a
final evaluation will be done to assess the impact that
the nutritional guidance of Nutrigep can have on it.
4 CONCLUSIONS AND FUTURE
WORK
This paper presents a solution that can prevent
malnutrition in the geriatric environment,
contributing to the good nutritional management of
the elderly in order to improve their state of health.
It provides health professionals and caregivers
with a tool that offers personalized nutritional
recommendations for elderly pluripathologic patients
with risk of suffering from malnutrition. Not only the
personalized diet plans are generated for a specific
pathology and the patient’s malnutrition risk, but also
our solution generates specific diet plans for patients
that suffer from a combination of the diagnosed
pathologies, a typology of patients for which,
according to our research, current platforms cannot
properly offer nutritional recommendations.
Furthermore, the logic of the system can be easily
followed thanks to the visual representation of the
business processes that is being used. The system was
implemented in a real clinical scenario, where a
clinical study is going to be carried out. The clinical
study will show the impact of the developed platform
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
342

and the developed nutritional guidelines in the
patients’ health status.
We have identified some future work to improve
the current platform. Firstly, in order to widen the
scope of potential users, other pathologies should also
be included. Furthermore, recommendations should
include other information related with the health
status, such as physical or wellbeing
recommendations, in order to provide not only diet
recommendations, but a more holistic set of
recommendations that could help improve the overall
wellbeing of the patients. Lastly, in order to make the
system easy to configure, a web authoring tool is
being developed where the user will be able to define
the different combinations of pathologies that are
supported by the platform. The diet plans will also be
generated using the same tool, as a result of this, the
scalability of the system will be increased as the
addition of new logic and new recommendations will
be supported from the same tool, reducing the work
needed to update the platform.
ACKNOWLEDGEMENTS
This study was supported by the grant ZL 2019/00647
NUTRIGEP from Eusko Jaurlaritza (Basque
Government) and the European Union under the
European Regional Development Fund (ERDF). The
funding sources had no involvement in the collection,
analysis and interpretation of data; in the writing of
the report; or in the decision to submit the article for
publication.
The study complies with the current laws of Spain
and Europe.
All authors declare that they have no competing
interests.
REFERENCES
Agarwal, E., Miller, M., Yaxley, A., & Isenring, E. (2013).
Malnutrition in the elderly: A narrative review.
Maturitas, 76, 296-302. doi:https://doi.org/10.1016/
j.maturitas.2013.07.013
Espín, V., Hurtado, M. V., & Noguera, M. (2016). Nutrition
for Elder Care: a nutritional semantic recommender
system for the elderly. Expert Systems, 201-210.
doi:10.1111/exsy.12143
Joint WHO/FAO Expert Consultation on Diet, Nutrition
and the Prevention of Chronic Diseases. (2003). Diet,
Nutrition And The Prevention Of Chronic Diseases.
Geneva: WHO technical report series.
Kuo, S.-E., Lai, H.-S., Hsu, J.-M., Yu, Y.-C., Zheng, D.-Z.,
& Hou, T.-W. (2018). A clinical nutritional information
system with personalized nutrition assessment.
Computer Methods and Programs in Biomedicine, 155,
209-216.
doi:https://doi.org/10.1016/j.cmpb.2017.10.029
Kushi, L. H., Doyle, C., McCullough, M., Rock, C. L.,
Demark-Wahnefried, W., Bandera, E. V., Guidelines,
T. A. (2012). American Cancer Society Guidelines on
Nutrition and Physical Activity for Cancer Prevention.
CA: A Cancer Journal for Clinicians, 30-67.
doi:10.3322/caac.20140
Leipold, N., Madenach, M., Schäfer, H., Lurz, M.,
Terzimehic, N., Groh, G., Krcmar, H. (2018). Nutrilize
a Personalized Nutrition Recommender System: an
Enable Study. HealthRecSys.
NHLBI, O. E. (1998). Clinical Guidelines on the
Identification, Evaluation, and Treatment of
Overweight and Obesity in Adults. Bethesda (MD):
National Heart, Lung, and Blood Institute. Retrieved
from https://www.ncbi.nlm.nih.gov/books/NBK2003/
Paulsen, M., Varsi, C., & Andersen, L. (2021). Process
evaluation of the implementation of a decision support
system to prevent and treat disease-related malnutrition
in a hospital setting. BMC Health Serv Res, 21, 281.
doi:https://doi.org/10.1186/s12913-021-06236-3
Taweel, A., Barakat, L., Miles, S., Cioara, T., Anghel, I.,
Tawil, A.-R. H., & Salomie, I. (2016). A service-based
system for malnutrition prevention and self-
management. Computer Standards & Interfaces, 225-
233. doi:https://doi.org/10.1016/j.csi.2016.03.005
Torres, J., Artola, G., & Naiara, M. (2020). A Domain-
Independent Semantically Validated Authoring Tool
for Formalizing Clinical Practice Guidelines. Studies in
Health Technology and Informatics, 517-521.
Personalized Nutritional Guidance System to Prevent Malnutrition in Pluripathological Older Patients
343
