
BrainIn: A Data-driven Software System for Neurorehabilitation of
People with Acquired Brain Injuries
Roman Mou
ˇ
cek
a
, Luk
´
a
ˇ
s Va
ˇ
reka
b
, Petr Br
˚
uha
c
, Pavel
ˇ
Snejdar
d
, Michal Hork
´
y
and Ivana Herejkov
´
a
New Technologies for the Information Society, Faculty of Applied Sciences, University of West Bohemia,
Univerzitn
´
ı 8, 306 14 Plze
ˇ
n, Czech Republic
Keywords:
Acquired Brain Injury, BrainIn, Computer-based Neurorehabilitation, Online Software System.
Abstract:
The current model of neurorehabilitation provides comprehensive care (neurologist, physiotherapist, occu-
pational therapist, psychologist, speech therapist) in the acute phase of acquired brain injuries during hos-
pitalization in some countries. However, follow-up care is insufficient or completely absent, especially for
disadvantaged people. Increasing the availability, effectiveness and efficiency of neurorehabilitation care is
beneficial both socially and economically. The BrainIn project aims to improve the quality, effectiveness, and
efficiency of neurorehabilitation procedures in both the acute phase and long-term home rehabilitation phase.
Moreover, its goal is to facilitate and accelerate the return of the affected people to their families, social, and
working life. The BrainIn project is freely available as a web application (https://brainin.kiv.zcu.cz/). It is
adapted to the needs of therapists and patients who have experienced acquired brain injuries.
1 INTRODUCTION
This paper deals with the neurorehabilitation of peo-
ple suffering from acquired brain injuries (ABIs) and
opportunities to improve its availability, effectiveness
and efficiency. First, it presents an overview of stud-
ies, approaches, questions and results achieved in the
ABI neurorehabilitation and then introduces an online
data-driven software system BrainIn that provides
ABI people, their families and therapists with vari-
ous neurorehabilitation tasks. Moreover, the BrainIn
system enables the personalization of neurorehabilita-
tion tasks, facilitates remote cooperation among ABI
people, their families and therapists and collects be-
havioural data that can help to improve neurorehabil-
itation procedures.
The term acquired brain injury (ABI) refers to any
brain injury that occurs after birth, i.e. is not hered-
itary, congenital, degenerative, or induced by birth
trauma. Medical disciplines use various classifica-
tions for ABIs, including traumatic brain injury (TBI)
and non-traumatic injuries such as infection, disease,
a
https://orcid.org/0000-0002-4665-8946
b
https://orcid.org/0000-0002-5998-3676
c
https://orcid.org/0000-0003-4031-8243
d
https://orcid.org/0000-0002-2800-3030
stroke, brain tumour, lack of oxygen, a blow to the
head, poisoning, and alcohol/drug abuse. ABI results
in a change to the brain’s neuronal activity, which can
lead to changes in the physical and sensory abilities,
behaviour and personality, metabolic activity, atten-
tion, memory, communication abilities, thinking and
learning or can cause other medical troubles such as
epilepsy.
It is generally difficult to predict the long-term
effects and consequences of ABI. These are differ-
ent for each individual and range from mild to se-
vere. People usually suffer from increased mental
and physical fatigue and decreased general abilities
to plan and solve problems and process information.
These changes require a period of adjustment, both
physically and emotionally, and affect the individu-
als suffering from ABI and their families, friends, and
caregivers.
There is general agreement that the neurorehabil-
itation care of people with ABI is very demanding. It
involves an overall systematic and interdependent co-
operation of experts such as neurologists, physiother-
apists, occupational therapists, psychologists, speech
therapists, and above all, ABI people themselves and
their family members. The big questions (to which
we have only very limited answers) are how to target
and organize neurorehabilitation care to make it effec-
126
Mou
ˇ
cek, R., Va
ˇ
reka, L., Br˚uha, P., Šnejdar, P., Horký, M. and Herejková, I.
BrainIn: A Data-driven Software System for Neurorehabilitation of People with Acquired Brain Injuries.
DOI: 10.5220/0011086100003188
In Proceedings of the 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2022), pages 126-133
ISBN: 978-989-758-566-1; ISSN: 2184-4984
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

tive and efficient for all involved individuals in their
daily routines, how to provide reasonable (sufficient
and non-annoying) feedback among all involved peo-
ple and implement innovative procedures improving
a long-term therapy.
The paper itself is organized as follows. The
State of the Art section provides a short overview
of available resources: mainly review papers and
computer-based neurorehabilitation papers are pro-
vided. The third section introduces the core concepts
of the BrainIn software system. Then the fourth sec-
tion describes the system implementation. The fifth
section gives an overview of groups of neurorehabili-
tation tasks available in the BrainIn system. The sixth
section provides a study on using the system by a
long-term ABI patient. The last section comes with
concluding remarks.
2 STATE OF THE ART
Although we might assume that the questions of ef-
fectiveness and efficiency of the neurorehabilitation
interventions should have already been resolved, this
is not the case. This section provides a state-of-the-art
overview of ABI rehabilitation, focusing mainly on its
effectiveness and efficiency. Since hundreds of stud-
ies were carried out and published to aim at different
ABI rehabilitation approaches, usually review papers
with their results and conclusions are presented.
The efficacy of acquired brain injury rehabilita-
tion is investigated in the systematic review given
in (Cullen et al., 2007) to provide guidance for clini-
cal practice. The authors conclude that most interven-
tions have only been supported by limited evidence,
although positive outcomes are documented. These
include, e.g. moderate evidence that inpatient rehabil-
itation results in a successful return to work or that di-
rect patient involvement in neurorehabilitation goals
results in significant improvements in reaching and
maintaining those goals. The authors conclude that
there is a need for studies of improved methodologi-
cal quality into ABI rehabilitation.
(Turner-Stokes and Wade, 2015) present a sys-
tematic review of 19 studies involving 3480 peo-
ple of working age. They claim that systematic re-
views demonstrate that multi-disciplinary rehabilita-
tion is effective in the stroke population, in which
older adults predominate. However, the evidence for
the effectiveness of rehabilitation following ABI in
younger adults has not been established. They con-
clude that different interventions and combinations of
interventions are required to meet the needs of pa-
tients with different problems.
Efficacy of neurofeedback interventions for cog-
nitive rehabilitation following brain injury is system-
atically reviewed in (Ali et al., 2020) concluding that
’given the limited quantity and quality of the available
research, there appears to be insufficient evidence to
comment on the efficacy of neurofeedback therapies
within an ABI rehabilitation context’ and providing
recommendations for future research.
A scoping review (Stolwyk et al., 2021) exam-
ines the literature related to economic evaluations of
neuropsychological rehabilitation in individuals with
ABI. There were included studies published between
1995 and 2019 with a study population of adults aged
18 years or more with any ABI aetiology. The au-
thors state (among other conclusions) that most stud-
ies have documented cost savings from providing var-
ious models of multi-disciplinary inpatient or outpa-
tient rehabilitation. On the other hand, these benefits
were estimated without a control group. Only a few
eligible studies included a cost-effectiveness analysis
that yielded mixed evidence for interventions consid-
ered cost-effective for ABI.
A systematic review of the use of computer-
ized cognitive rehabilitation of attention and execu-
tive function in ABI provided in (Bogdanova et al.,
2016) concludes that preliminary evidence suggests
improvements in cognitive functions following com-
puterized rehabilitation for ABI populations. How-
ever, it is also stated that further studies are needed
to address issues such as small sample sizes or inade-
quate control groups.
A systematic review of outcomes of computerized
cognitive training (CCT) in adults with ABI using
the International Classification of Functioning, Dis-
ability and Health (ICF) is given in (Sigmundsdottir
et al., 2016). One of the conclusions is that there is
much research examining the efficacy of CCT, but rel-
atively few Level 1 (randomized controlled trials with
a PEDro-P score ≥ 6/10) studies and evidence is lim-
ited mainly to body function outcomes.
Computer-based cognitive interventions in ABI
are systematically reviewed in (Fern
´
andez L
´
opez and
Antol
´
ı, 2020). The authors conclude that such inter-
ventions might be beneficial for ABI people to im-
prove their visual and verbal working memory, al-
though no effect was found in other cognitive do-
mains.
The efficacy of ICT-Based neurocognitive rehabil-
itation programs for ABI was systematically reviewed
in (Geraldo et al., 2018). Most of the thirty-one stud-
ies use a pre-post methodological design, with few
performing assessment moments during intervention
or follow-up. Attention, memory, and executive func-
tions were the variables mainly considered by these
BrainIn: A Data-driven Software System for Neurorehabilitation of People with Acquired Brain Injuries
127

studies to assess neurocognitive rehabilitation pro-
grams efficacy. The studies present a considerable
heterogeneity of the instruments and methods used,
even for the same assessment purpose; a lack of con-
sensus regarding assessment protocol is well visible.
A systematic review in (Resch et al., 2018) exam-
ines studies investigating cognitive rehabilitation in-
terventions for children with ABI, also focusing on
identifying effective (computerized) drill-based exer-
cises. Authors conclude (preliminarily, due to small
sizes and heterogeneity of included studies) that avail-
able evidence suggests that multi-component rehabil-
itation, including drill-based training, is most promis-
ing and can lead to improvements in children’s cogni-
tive and psychosocial functioning ABI.
A clinical review dealing with neurorehabilita-
tion of traumatic brain injuries (TBIs) is presented
in (Oberholzer and M
¨
uri, 2019). The authors point
out specific characteristics of TBI individuals com-
pared to individuals with ABIs. They address ques-
tions on timing and existing evidence for various re-
habilitation programmes and their impact on the out-
comes in TBI rehabilitation. They also state that
there are currently no international guidelines regard-
ing treatment in the early rehabilitation phase for pa-
tients with severe TBI and that only a few studies
have investigated the effect of integrating rehabilita-
tion into acute TBI care.
A literature review of immersive virtual reality in
TBI rehabilitation is provided in (Aida et al., 2018)
concluding that ”while the current literature gener-
ally offers support for the use of VR in TBI recov-
ery, there is a paucity of strong evidence to support its
widespread use”.
A qualitative study aimed to explore the needs of
individuals with TBIs and their loved ones (Lefebvre
and Levert, 2012) point out that health care profes-
sionals should adopt a personalized approach to re-
spond to needs related to the evolution of informa-
tion, support, and relationships among them, individ-
uals with TBIs and their loved ones.
A systematic review (Coxe et al., 2020) deal-
ing with telebehavioral interventions for family care-
givers of individuals with TBI concludes that care-
givers generally express positive outcomes related to
telebehavioral interventions, but low diversity of sam-
ples prevents generalizing these outcomes.
A critical review of the literature (Fetta et al.,
2017) dealing with the efficacy of computer-based
cognitive rehabilitation interventions on cognitive
performance after mild TBI and ABI concludes that
computer-based interventions seem promising when
improving working memory in individuals with ABI.
However, there is no evidence that currently available
interventions are specific to mild TBI.
To summarize the state-of-the-art section, we can
argue that many studies describe ABI/TBI rehabilita-
tion’s success. On the other hand, only a small part
of the studies was carried out so that the success of
the rehabilitation, or rather the rehabilitation proce-
dures used, was proven. This can also be stated in the
case of computer-based rehabilitation. All in all, the
evidence that targeted rehabilitation procedures lead
to significantly better results than any rehabilitation,
even if based on everyday human activities, is not
convincing.
Finally, we can modestly state that various stim-
uli that motivate ABI people to be active and improve
their abilities and skills have a rehabilitative character.
Then, a computer-based system providing tasks tar-
geted to improve various skills and abilities can help
ABI people, their families, and therapists in the long
term.
3 BrainIn SYSTEM
BrainIn is an online software system (web applica-
tion) for the neurorehabilitation of patients with ABI.
It is designed for patients in institutional and home
care, their families, and therapists and enables the
computerized definition, execution, and basic evalua-
tion of personalized neurorehabilitation tasks of vary-
ing degrees of difficulty for each patient. The ther-
apist defines the sets of personalized neurorehabilita-
tion tasks, and the patient then performs them with the
help of the therapist, the family, or completely alone.
The main advantage of the BrainIn system is the pos-
sibility of personalization of the tasks by the therapist,
the creation of exercises of different difficulty lev-
els, the organization of activities in packages, and the
readiness of the system for partially automated evalu-
ation of the patient’s results and the subsequent use of
machine learning methods to make recommendations
for personalized therapies.
The BrainIn system is based on task templates
with input variables for adjusting each task for an in-
dividual patient. These input variables must be set
before execution. Their setting occurs in the task that
runs the program. These tasks are easily editable, and
it is easy to create a similar version (for example, with
a different number of rounds, other pictures, ques-
tions, etc.). The exercise for each patient typically
forms a package consisting of multiple tasks.
We have introduced the terms template, task, and
package.
• A template is both the program itself and a web
form defining input and output variables. Input
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
128

Figure 1: Vocabulary task. The patient is asked to select the caption corresponding to the picture shown with a mouse click.
It is possible to use help (e.g., ’50:50’ to hide two wrong options) by clicking on the question mark button.
variables define parameters of the task typically
used for modifying the difficulty level and person-
alization. For example, the therapist can select fa-
miliar images for each patient (e.g., towns in their
neighbourhood), the number of hints, or highlight
some letters related to the task. The output param-
eters describe the performance and recordings of
each task execution. For example, the success rate
of the answers, the number of hints used, or event
recordings, such as a history of mouse clicks. Ex-
amples of input and output parameters are in Ta-
ble 1. The code is shared for all tasks created by
the same template.
• A task is a web form that sets the input variables
defined in the template, the setting of which is
necessary to run the template program.
• The package is a set of tasks. Our concept is a
web form that creates a list of tasks.
The BrainIn users can be assigned a total of five roles
that modify their capabilities and behaviour in the sys-
tem:
• Super-Administrator manages the rights for
other roles and provides application environment
settings.
• Administrator takes care of the operation of the
application. He/she creates new tasks, manages
users, assigns patients to therapists, etc.
• Therapist assigns patients and gives them neu-
rorehabilitation tasks.
• Super-Therapist creates custom tasks that other
therapists can use.
• Patient role is assigned to each user after regis-
tration. The patient performs tasks assigned to
him/her and can evaluate them.
4 BrainIn WEB APPLICATION
BrainIn is built on the ASP.NET MVC framework
using the Microsoft SQL Server database. Each
neurorehabilitation task is implemented in the game
framework Unity 3D, providing developers with rapid
exercise development and huge graphic variability.
All exercise templates are based on a minimal tem-
plate with basic functionality. It guarantees the same
user interface (such as the menu, icons, buttons)
through all exercise templates.
There is a landing page for non-registered users
with basic information about the project. It allows
users to try out sample tasks. For registered users,
functionality is different for each role in the system.
There is a dashboard control panel with statistics,
graphs, and shortcut buttons for quick and easy access
to essential features. An example of the dashboard
with results is shown in Figure 2.
The BrainIn system is available at https://brainin.
kiv.zcu.cz/. Users’ recommended requirements are
64bit OS, Mozilla Firefox or Google Chrome web
browsers, and a touch screen for fine motor tasks.
BrainIn: A Data-driven Software System for Neurorehabilitation of People with Acquired Brain Injuries
129
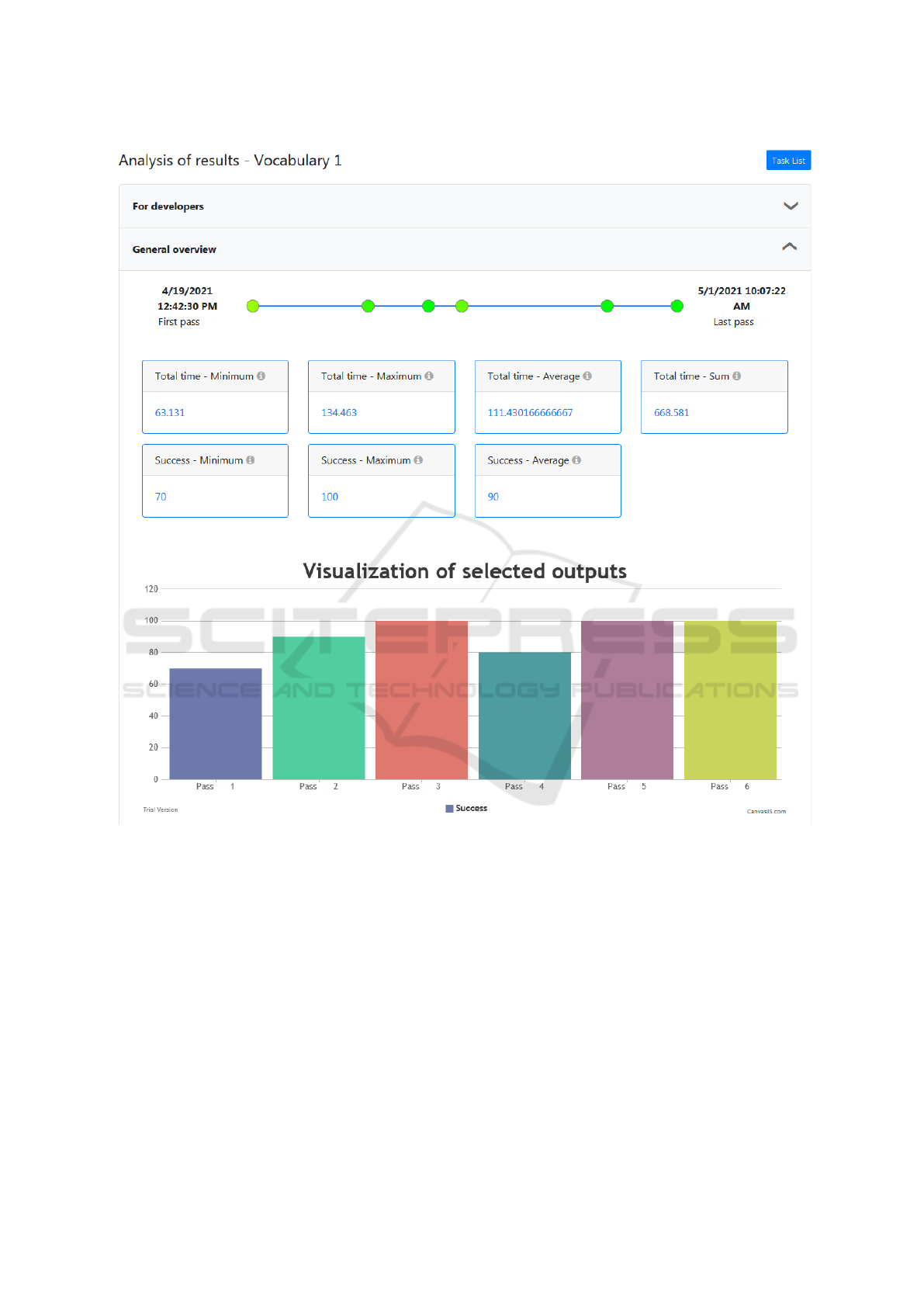
Figure 2: Visualization of results from the Vocabulary task.
4.1 Data Collection and Annotation
The BrainIn system collects anonymized data from
the neurorehabilitation process. The aim of the data
collection is:
• to provide continuous neurorehabilitation results
(i.e., output parameters of tasks) to therapists to
personalize therapy,
• to allow export of multiple datasets in JSON for-
mat for statistical analysis.
All patients sign the informed consent about anony-
mous data collection and further processing using a
web form. We process the following personal data in
the system: name and surname, e-mail address, user-
name, and password.
For statistical processing during system valida-
tion and development, we collect and process addi-
tional data in Google Forms: Patient ID, gender, age,
neurorehabilitation start date, duration of the BrainIn
neurorehabilitation in weeks, assigned tasks, patient
education, dominant hand, initial patient condition,
the patient’s final condition, the reason for ending
therapy, and the patient’s behavioural data.
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
130
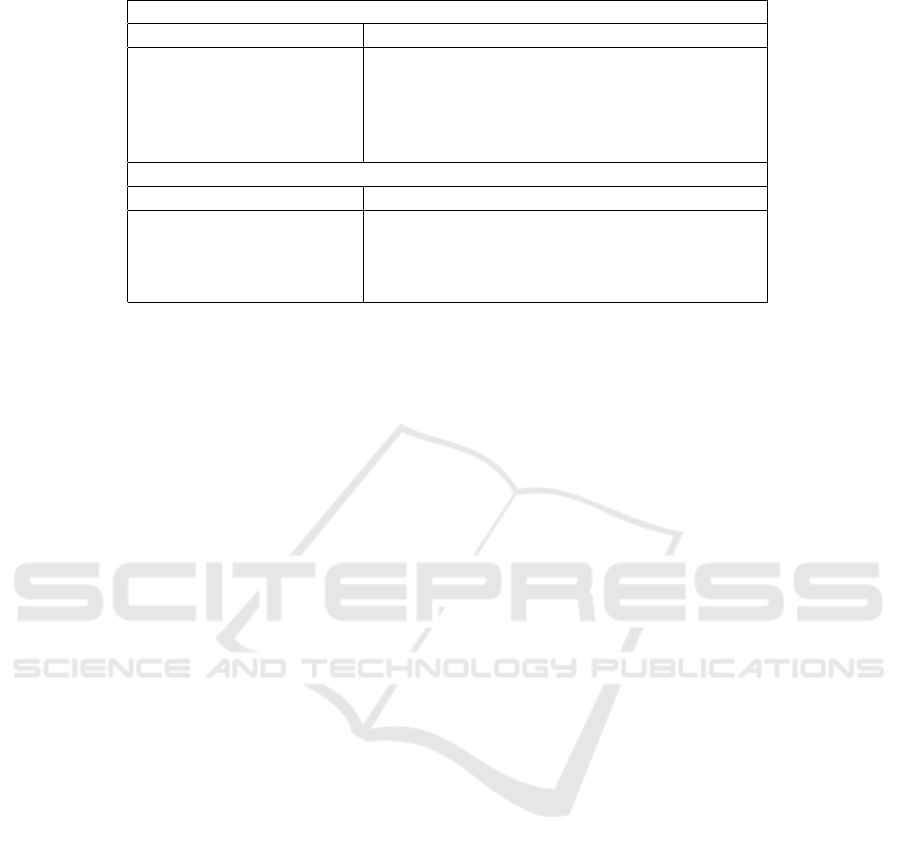
Table 1: Examples of Default input and output parameters from the Vocabulary template.
Input parameters
Parameter Description
Number of rounds Number of repetitive parts of the task
Number of options Number of multiple choice fields (one correct)
Shuffle Whether to show options in random order
Help How many times help can be used during a task
Showing the right solution Whether to display the correct solution
Output parameters
Parameter Description
Total time Total run time of the task in seconds
Round time Run time of each round in task in seconds
Success Percentage success of the task
Help used If the help was used in the round
5 NEUROREHABILITATION
TASKS
5.1 Categorization of Tasks
The BrainIn system contains samples of publicly ac-
cessible neurorehabilitation tasks. Now the system
has six task categories (examples of tasks are given
in parentheses):
• Speech functions (Text Completion 1, Word Se-
ries, Vocabulary, Anagrams, Charade, Characters
search, Interview)
• Memory (Ascending Numbers)
• Logical thinking (Lamps, Pyramid, Orion)
• Concentration (Lettuce Harvest, Test Tubes, Ad-
dition and Subtraction)
• Spatial orientation (Grid)
• Light motor skills (Finish the Half Example,
Painting with Hands, Joining Points, Connecting
Pairs)
5.2 Speech Therapy Use Case
Patients with speech disorders, such as aphasia, need
speech therapy in addition to classical rehabilitation.
This rehabilitation should always be targeted and
should reliably lead to speech adjustment. If the pa-
tient is hospitalized, they receive this care daily in
the hospital. After their release, the patients have to
train at home according to the instructions of a clini-
cal speech therapist and a regular speech therapist.
The BrainIn system offers daily targeted speech
therapy tasks – tailor-made brain training. These are
mainly exercises focused on naming and syntax disor-
ders, disorders of language emotion, memory, atten-
tion, reading, analysis, word synthesis, and exercises
in text and field of view.
The tasks Vocabulary and Word series allow the
patients to strengthen lexical semantics, vocabulary,
and equipment of concepts. Skills such as reading,
text orientation, perception of phrases, and under-
standing of meanings are supported by the task Text
completion. The Anagrams and Word Charade tasks
help the patients to analyze and synthesize letters (or
sounds), syllables, and words and thus facilitate writ-
ing. The Ascending Numbers task strengthens visual
memory and trains arranging consecutive elements.
All tasks require attention and concentration; they
can be considered cognitive tasks. The speech tasks
are ranked from the lowest difficulty (level 1) to the
average difficulty (level 5).
As an example, the task Vocabulary (see Fig. 1)
is provided. The patient is asked to select the caption
corresponding to the picture shown. Similarly to other
tasks, there are yellow control buttons on the right of
the screen. The therapist can give the patient systemic
help in text form or by hiding 50% of the options. The
question mark button is used for this option. The pa-
tient can turn on/off all audio stimuli of the task using
the speaker button. The vocabulary contains over 400
words, which fall into 16 categories (food, fruit, veg-
etables, personal things, colours, profession, musical
instruments, animals, cities, flowers, trees, transport
facilities, buildings, furniture, home appliances, and
home accessory).
6 THERAPEUTIC PRACTICE
AND RESULTS
Since early 2021 the BrainIn system has been used in
hospitals and care homes in the Pilsen region. Four
BrainIn: A Data-driven Software System for Neurorehabilitation of People with Acquired Brain Injuries
131
0th Week 2nd Week 3rd Week 4th Week 5th Week 6th Week 7th Week 8th Week1st Week
Stroke
Start of
rehabilitation
with Brainin
Hospitalization
Practicing of exercises for fine
motor skills and name things
Start of
rehabilitation
Leaving the
hospital
9th Week
Vocabulary 1, 2
Vocabulary 3
Vocabulary 4
Text
completion 1
Vocabulary 5
Text
completion 2
Brainin motoric exercises
Text
completion 3
Vocabulary 5
Anagrams 1
Day 0 - Disabilities
- No ability to name things
- No ability to writing
- No ability to speaking
6 weeks rehabilitation
progress
- Ability to name things
- Ability to Writing
- Ability to Speaking
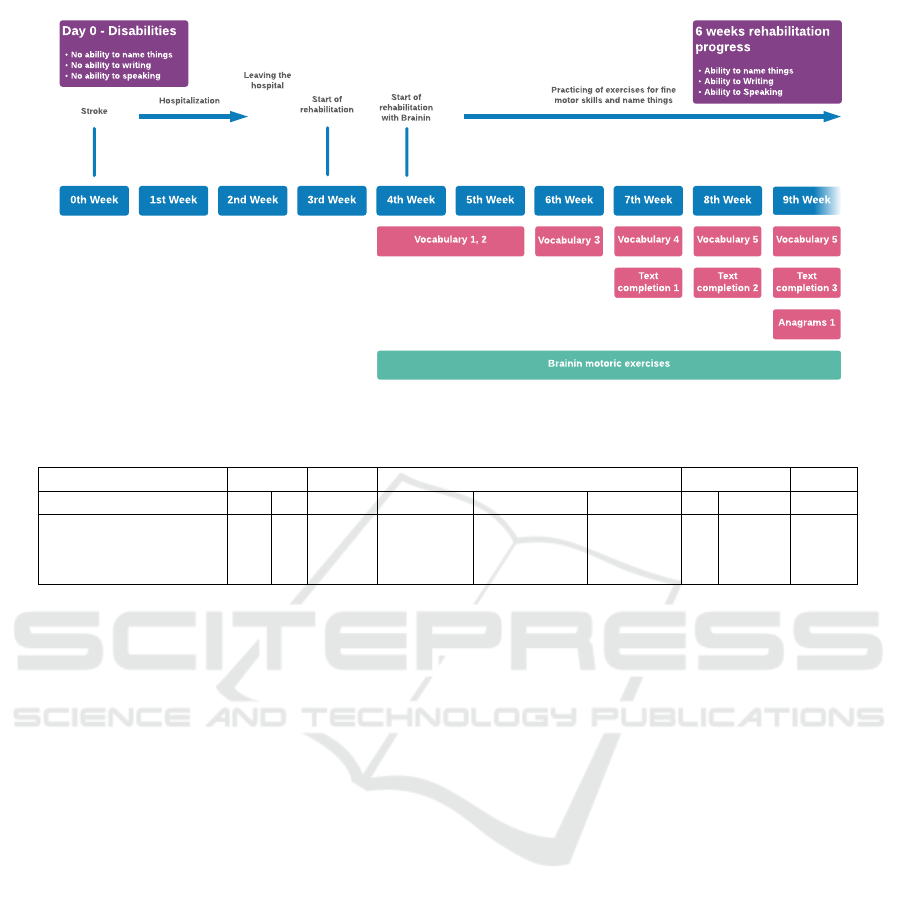
Figure 3: The timeline of patient progress when performing neurorehabilitation tasks with the BrainIn system.
Table 2: Basic patient data.
Institution Sex Age Education Laterality Total
M F - Primary Secondary Tertiary L R
University Hospital 3 3 37-64 0 4 2 0 6 6
Zb
˚
uch Centre 8 2 27-64 4 6 0 6 4 10
Total 11 5 0 4 10 2 6 10 16
patients (aged 37-49) have been actively perform-
ing logopedic tasks, and two patients (aged 49-64)
have been actively performing light motor tasks in
the University Hospital. In the centre of residen-
tial and field social services in Zb
˚
uch, ten patients
(aged 27-64) have been using the BrainIn system
for various tasks. While in this care home patients
are generally stable and significant improvements are
not expected; in the hospital, the patients’ improve-
ments are monitored using various screening meth-
ods (e.g., MAST, The Mississippi Aphasia Screening
Test (Nakase-Thompson et al., 2002) for logopedic
patients and BI for patients with cognitive problems).
The basic data about the patients is given in Table 2.
A woman, 48 years old, was hospitalized in March
2021 for a cerebral haemorrhage caused by a brain
tumour and underwent urgent surgery. Her initial
MAST score was 64/100. She could not write and
express what she wanted to say and name one-third
of the objects shown. She started to perform neu-
rorehabilitation with the BrainIn system consistently
and regularly about one month later. Simultaneously
but less frequently, she has been given traditional neu-
rorehabilitation tasks on paper. Her condition, includ-
ing speech, has gradually improved. Now (December
2021), she remembered 50/50 objects shown, some-
times with a delay. Moreover, her MAST score im-
proved to 83/100 (May 2021) and 88/100 (December
2021). Her progress when performing neurorehabili-
tation with the BrainIn system is depicted in Figure 3.
7 CONCLUSION
This paper presents a novel online system for person-
alized neurorehabilitation. BrainIn is based on a close
collaboration between therapists and patients and al-
lows a wide range of task parameter modifications.
These modifications are individually selected for each
patient and are gradually adjusted during the neurore-
habilitation process. These adjustments mean that it is
difficult to evaluate the benefits of the BrainIn system
statistically. Instead, we presented a specific case of
the neurorehabilitation process. For future work, once
more anonymized data are collected, it is planned to
apply machine learning methods to help to personal-
ize the course of neurorehabilitation.
ACKNOWLEDGEMENTS
This work was supported by ERDF and the Min-
istry of Regional Development of the Czech Republic
within the project INTERREG V-A 191.
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
132

REFERENCES
Aida, J., Chau, B., and Dunn, J. (2018). Immersive virtual
reality in traumatic brain injury rehabilitation: A liter-
ature review. NeuroRehabilitation, 42(4):441–448.
Ali, J. I., Viczko, J., and Smart, C. M. (2020). Effi-
cacy of neurofeedback interventions for cognitive re-
habilitation following brain injury: Systematic re-
view and recommendations for future research. Jour-
nal of the International Neuropsychological Society,
26(1):31–46.
Bogdanova, Y., Yee, M. K., Ho, V. T., and Cicerone, K. D.
(2016). Computerized cognitive rehabilitation of at-
tention and executive function in acquired brain in-
jury: a systematic review. The Journal of head trauma
rehabilitation, 31(6):419.
Coxe, K. A., Liu, C., and Moore, M. (2020). Telebehavioral
interventions for family caregivers of individuals with
traumatic brain injury: a systematic review. Journal
of head trauma rehabilitation, 35(6):E535–E546.
Cullen, N., Chundamala, J., Bayley, M., and Group, J. J.
F. T. E. (2007). The efficacy of acquired brain injury
rehabilitation. Brain Injury, 21(2):113–132.
Fern
´
andez L
´
opez, R. and Antol
´
ı, A. (2020). Computer-
based cognitive interventions in acquired brain injury:
A systematic review and meta-analysis of randomized
controlled trials. PloS one, 15(7):e0235510.
Fetta, J., Starkweather, A., and Gill, J. M. (2017).
Computer-based cognitive rehabilitation interventions
for traumatic brain injury: a critical review of the lit-
erature. The Journal of neuroscience nursing: journal
of the American Association of Neuroscience Nurses,
49(4):235.
Geraldo, A., Dores, A. R., Coelho, B., Rami
˜
ao, E.,
Castro-Caldas, A., and Barbosa, F. (2018). Efficacy
of ict-based neurocognitive rehabilitation programs
for acquired brain injury. European Psychologist,
23(3):250–264.
Lefebvre, H. and Levert, M. J. (2012). The needs experi-
enced by individuals and their loved ones following
a traumatic brain injury. Journal of Trauma Nursing,
19(4):197–207.
Nakase-Thompson, R., Manning, E., Sherer, M., Yablon,
S., Vickery, C., Harris, C., and Dickson, S. (2002).
Bedside screen of language disturbance among acute
care admissions: Initial psychometrics of the missis-
sippi aphasia screening test. In Archives of Clinical
Neuropsychology, volume 17, pages 848–848.
Oberholzer, M. and M
¨
uri, R. M. (2019). Neurorehabilita-
tion of traumatic brain injury (tbi): A clinical review.
Medical Sciences, 7(3).
Resch, C., Rosema, S., Hurks, P., de Kloet, A., and van
Heugten, C. (2018). Searching for effective compo-
nents of cognitive rehabilitation for children and ado-
lescents with acquired brain injury: a systematic re-
view. Brain injury, 32(6):679–692.
Sigmundsdottir, L., Longley, W. A., and Tate, R. L. (2016).
Computerised cognitive training in acquired brain in-
jury: A systematic review of outcomes using the inter-
national classification of functioning (icf). Neuropsy-
chological rehabilitation, 26(5-6):673–741.
Stolwyk, R. J., Gooden, J. R., Kim, J., and Cadilhac, D. A.
(2021). What is known about the cost-effectiveness of
neuropsychological interventions for individuals with
acquired brain injury? a scoping review. Neuropsy-
chological rehabilitation, 31(2):316–344.
Turner-Stokes, L, P. A. N. A. D. P. and Wade, D. (2015).
Multi-disciplinary rehabilitation for acquired brain in-
jury in adults of working age. Cochrane Database of
Systematic Reviews, (12).
BrainIn: A Data-driven Software System for Neurorehabilitation of People with Acquired Brain Injuries
133
