
Needs, Requirements, and Technology Acceptance using Telemedical
Consultations in Acute Medical Situations in Nursing Homes
Julia Offermann
1,* a
, Wiktoria Wilkowska
1b
, Anne Kathrin Schaar
1c
,
Jörg Christian Brokmann
2d
and Martina Ziefle
1e
(on behalf of the Optimal@NRW-Research Group)
1
Human-Computer Interaction Center, RWTH Aachen University, Campus-Boulevard 57, 52074 Aachen, Germany
2
Emergency Department, University Hospital RWTH Aachen, Pauwelsstraße 30, 52074 Aachen, Germany
Keywords: Telemedicine, Telemedical Consultations, Technology Acceptance, Nursing Homes, Geriatric Patients,
Qualitative Research, Interview Study.
Abstract: A lack of (medical) personnel and high proportions of older people in need of care pose enormous challenges
for care institutions, often resulting in hospitalizations of nursing home residents (geriatric patients).
Frequently, these hospitalizations are not medically necessary and cause a deterioration of health. The usage
of telemedical consultations in nursing homes represents one approach that aims at the reduction of
unnecessary hospitalizations of geriatric patients and at supporting care personnel in acute and medically
uncertain situations. For a successful implementation of these telemedical consultations, especially the
patients’ as well as the care personnel’s perspectives and acceptance are essential. This paper presents first
qualitative results from a social communication science perspective within the Optimal@NRW project. Based
on an interview study with residents and care personnel of different nursing homes (N=28) first attitudes,
perceived advantages, and concerns as well as requirements regarding the usage of telemedical consultations
are identified. These results provide the basis for further quantifications and comparisons of acceptance
parameters of using telemedical consultations in nursing homes in general and across the entire duration of
the project in specific.
1 INTRODUCTION
Studies have shown that 20% of nursing home
residents are hospitalised once a year. 40% of these
hospitalisations turn out to be unnecessary or
premature (Jakobs et al., 2018; Sundmacher et al.,
2015). Apart from the stressful emotional component,
hospital admissions can even cause harm to this
vulnerable group of patients. When a resident of a
nursing facility is taken to an emergency room for an
acute medical situation that could have been treated
by the general practitioner (GP), he or she joins the
ranks of other patients whose reasons for visiting the
emergency room are often more urgent and critical.
*
Corresponding Author
a
https://orcid.org/0000-0003-1870-2775
b
https://orcid.org/0000-0002-7163-3492
c
https://orcid.org/0000-0002-8643-6213
d
https://orcid.org/0000-0002-1745-6130
e
https://orcid.org/0000-0002-6105-4729
Long waiting times in an unfamiliar environment are
the consequences, which often trigger delirium,
especially in patients with dementia. It is not
uncommon for nursing home residents to spend
weeks recovering from the strain after a short stay in
an emergency room. In cases with e.g., occurring
delirium it is even likely that a higher level of
dependency persists due to the underlying condition
of frailty (Theou et al., 2018).
The main causes of these so called “ambulatory-
care sensitive conditions” (ACSC) are not finally
elucidated, but in many cases suboptimal outpatient
medical care of nursing home residents seems to be
responsible. This effect can be observed especially
Offermann, J., Wilkowska, W., Schaar, A., Brokmann, J. and Ziefle, M.
Needs, Requirements, and Technology Acceptance using Telemedical Consultations in Acute Medical Situations in Nursing Homes.
DOI: 10.5220/0011058100003188
In Proceedings of the 8th Inter national Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2022), pages 105-116
ISBN: 978-989-758-566-1; ISSN: 2184-4984
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
105

outside the regular consultation hours of the GPs
combined with an increasing workload of the nursing
staff in the facilities (e.g., low number of care
providers during night shifts).
Optimal@NRW project offers a low-threshold
opportunity by implementing telemedical acute care
for nursing home residents around the clock. For this
purpose, 25 participating senior care facilities are
equipped with the technology for telemedical
consultations as well as an early warning system. The
aim is to prevent nursing home residents from
unnecessary hospital admissions. The early warning
system is intended to preventively counteract a
potential deterioration of a health condition by regular
non-invasive measurement of vital parameters.
Likewise, the faster establishment of a doctor's
contact provides support for the nursing staff in acute
medical situations in the care facility.
In addition to the technical implementation of
telemedical infrastructure itself, the aim is to link the
components with the nursing home documentation
system via interfaces. With that approach, every
physician who is not familiar with the patient can also
access relevant preliminary medical information and
in turn document on the acute setting and therapy in a
way that is visible to co-therapists.
Further, the physicians in private practice and the
emergency service of the Association of Statutory
Health Insurance Physicians can optionally
participate in the beneficial telemedical infrastructure
to improve intersectoral medical care for nursing
home residents. It needs to be emphasized that
telemedicine is not intended to be a substitute for
personal doctor-patient interaction, but rather a
supplement to standard medical care - especially in
situations in which hospital admissions are the only
option left. Additionally, positive economic side
effects can be assumed by a reduction in ambulance
transports and hospitalizations.
2 BACKGROUND
In this section, the theoretical and empirical
background is presented, starting with a current state
on telemedical applications as well as insights
regarding empirical technology acceptance research.
Based on that, the underlying research project is
introduced, followed by the specific research aims
and research questions of the present study, focusing
on a social communication science perspective.
2.1 Telemedical Applications
Applying innovative digital applications has the
potential to address the main challenges in the
healthcare sector due to demographic change, i.e.,
high percentages of highly aged people with long-
term care needs at the same time shortages of medical
personnel and lack of financial resources (Wootton,
Craig & Patterson, 2017; Cook, Augusto & Jakkula,
2009). In more detail, the ubiquitous presence of the
Internet in combination with modern sensor-based
and ambient technologies enable the development
and design of innovative monitoring concepts for the
private environments, nursing facilities and hospitals.
With eHealth as a central element within the work
of the World Health Organization (WHO), the value
of information and communication technologies
(ICT) for healthcare applications and their
socioeconomic benefits in healthcare are highly
acknowledged in the last years (Al-Shorbaji, 2013).
In line with this, the design and development of
eHealth and telemedical applications has been
immensely expedited. Regarding telemedicine,
applications addressing doctor-patient
communication and also applications for
communication between medical professionals –
such as tele-intensive care (Amkreutz, et al. 2020) or
tele-emergency care (Felzen et al., 2019; Czaplik et
al., 2014) – are focused. Supporting development and
research, diverse telemedicine and eHealth
approaches are funded as national and international
research projects. One international example is the
EU-project PAAL (Privacy-Aware and Acceptable
Lifelogging services for older and frail people)
aiming for a development of diverse video-, sensor-,
and speech-based systems that support older and frail
people in their everyday lives (Flórez-Revuelta et al.,
2018). Another example is the project AIDA, which
focuses on medical care of residents in nursing
homes, aiming for preparing nursing homes for the
usage of telemedicine to ensure adequate care for
elderly people (Ohligs et al., 2020).
Although the purposes of such research projects
are promising, it is still difficult to transfer the project
phases into the standard care of the national health
insurance funds. Beyond the primarily financial
difficulties, the acceptance of all involved
stakeholders (i.e., caregivers, patients, physicians)
poses an important prerequisite for the successful and
sustainable rollout of usable concepts.
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
106

2.2 Acceptance and Technology
Perception
In line with the increasing development of innovative
digital applications, the efforts in technology
acceptance research have rapidly grown in the last
decades. Initially – focusing on a differentiation
between acceptance subjects, objects, and contexts
(Kollmann, 1998) – technology acceptance research
based on successful and established acceptance
models like TAM (Davis, 1989) and further model
developments such as UTAUT (Venkatesh et al.,
2003). These models focused on the adoption of ICT
in working contexts and identified in particular two
factors, the perceived ease of use and perceived
usefulness, as good predictors for the behavioral
intention to use a specific technology or application.
To date, these models have been applied numerous
times and are frequently adapted to different contexts
(for an overview see Rahimi et al., 2018).
Beyond these models, acceptance research in
early project or technology development phases is
often challenged by the fact that it relates to areas that
have not been researched before, requiring that the
status quo must first be identified. In such phases –
when interaction with technical applications has not
yet started and only theoretical deliberations were
made – adequate explorative methodological
approaches are needed (especially in sensitive
contexts, such as nursing home environments).
Qualitative and scenario-based approaches are one
suitable measure to gain insights into the respective
stakeholders’ associations, mental models, perceived
(dis)advantages, needs, wishes, and the requirements
of using a specific application in a specific context.
2.3 The Context of the Study:
Optimal@NRW
Although telemedicine is a promising approach to
tackle the described challenges in the healthcare
sector, there are no solutions so far that have been
rolled out large-scale.
Continuing the efforts of the AIDA project
(Ohligs et al., 2020), the implementation and
standardization of telemedical processes, the proof of
medical evidence, cost coverage by the health
insurance companies as well as the acceptance of the
involved stakeholders are needed to enable a
sustainable and widespread use of telemedical care in
nursing homes. This is exactly the aim of the project
Optimal@NRW, representing a new intersectoral
approach that focuses on a provision of acute care and
support for geriatric patients based on the integration
of telemedical consultation systems in 25 nursing
homes and outpatient care within the region of
Aachen in Germany. In particular, the project aims
for the avoidance and reduction of inadequate
hospital admissions in ambulatory care-sensitive
hospital cases (Sundmacher et al., 2015) and
improved medical care in nursing homes. For this
purpose, a central emergency number acts as a virtual
hub for the care of geriatric patients and the idea is
that – in case of medical problems or acute situations
– the participating nursing homes firstly contact the
doctor's call center (116 117). The call center then
executes an initial medical assessment and decides
about urgency and following treatment. If the GP is
not available or if the call from the nursing home is
received outside the GP's opening hours, the
physicians of the resident health service are contacted
in order to provide a visit. If timely contact cannot be
guaranteed neither by the GP nor the resident health
service, teleconsultation by the tele-physicians can be
carried out at any time.
Besides medical research and evaluation of the
efficacy of the implemented structure and processes,
the project investigates user-related acceptance,
perceptions, requirements, and wishes of the relevant
stakeholders – in particular, the residents of nursing
homes and care personnel. Since in nursing homes
especially the actions of the care personnel determine
whether new structures and process are used in the
everyday life, it is precisely the perspective of this
group that must be considered, analyzed, and
understood throughout the entire project. Only this
way, central barriers, concerns, and requirements can
be timely identified enabling technical or medical
adaptions of the telemedical infrastructure and
processes.
The current study presents first results from an
initial qualitative interview study, identifying the
wishes, needs, concerns, and requirements of the two
most relevant user groups – geriatric patients and care
personnel – prior to the real usage of the telemedical
consultations.
2.4 Research Aim and Questions
From the perspective of social communication
science, the first aims of the project and, in particular,
of the present study refer to the understanding and
identification of acceptance-relevant parameters of
the telemedical consultations in nursing homes. In
more detail, the specific underlying research
questions were the following:
Needs, Requirements, and Technology Acceptance using Telemedical Consultations in Acute Medical Situations in Nursing Homes
107

RQ1: How do geriatric patients and care
personnel perceive telemedical consultations in
emergency situations in nursing homes in
general?
RQ2: Which benefits do geriatric patients and
care personnel perceive related to telemedical
consultations in emergency situations in nursing
homes?
RQ3: Which barriers and concerns do geriatric
patients and care personnel perceive related to
telemedical consultations in emergency
situations in nursing homes?
RQ4: Which requirements are relevant for
geriatric patients and care personnel related to
telemedical consultations in emergency
situations in nursing homes?
The qualitative approach as a first step was
necessary to enable subsequent quantifications and
weightings of the identified acceptance parameters.
Beyond that, the investigation in the initial phase of
the project provides a baseline for the comparisons of
acceptance and the identification of impacting
parameters in later project phases.
3 EMPIRICAL APPROACH
This section presents the methodological approach of
the conducted study, starting with a description of the
empirical concept as well as the procedure and
specific contents of the interview study, followed by
an overview of the participants’ characteristics.
3.1 Empirical Concept
The entire project including the individual studies of
the different project partners was reviewed and
approved by the Ethics Committee at the RWTH
Aachen Faculty of Medicine.
Overall, the project can be divided in three
different phases: pre-implementation,
implementation, and post-implementation. During
the implementation phase of the project, an
evaluation of the medical and economic efficacy of
the implemented structure and processes will be
carried out in a cluster-randomized study, which
means that the telemedical infrastructure will be
implemented stepwise in four different clusters
containing each 6-7 nursing homes.
The pre- and post-implementation phases enable
the identification of relevant parameters, processes,
and structures directly at the beginning of the project,
and offer the opportunity to compare perceptions and
acceptance of the telemedical infrastructure regarding
the whole project period.
In each of the three phases, technology acceptance
and perception are investigated, using multi-faceted
empirical approaches consisting of qualitative
interview and quantitative survey studies. In addition,
the implementation phase enables to evaluate
interactions with the telemedical infrastructure in the
participating nursing homes, thus in real and not in
scenario-based or laboratory settings.
This study presents the results of an interview
study with geriatric patients and care personnel from
different nursing homes within the pre-
implementation phase. Hence, the identification of
opinions, attitudes, requirements, and wishes is
focused prior to first interactions with the telemedical
infrastructure. These results represent the basis for
subsequent quantitative investigations.
3.2 Interview Study
At the beginning of the interviews, participants were
shortly informed about the overall project and the
content of the study. Further, they gave their informed
consent to participate in the interview and to agree
with audio recordings of the interview.
In a first step, the participants were asked to share
some personal information, such as their age and
gender. Beyond that, the participating geriatric
patients were questioned about their health situation
as well as for their experiences and feelings
connected to the living in the nursing home. In
parallel, the care personnel answered questions
related to their professional experience in caring for
geriatric patients in general and specifically related to
the current professional everyday life in their nursing
homes.
As a thematic transition, both groups of
participants were then asked for their experiences
with emergency situations in nursing homes, focusing
on real past situations, existing processes, and
potential difficulties.
Afterwards, the concept of telemedical
consultations in nursing homes was introduced to the
participants using a short descriptive scenario
(translated version):
“In the Optimal@NRW project, telemedical
technology is being introduced and tested in
various nursing homes in the region of Aachen.
Once introduced, it will be possible for the on-site
care personnel to request support in emergency
situations via the central emergency number
(116117) of the Association of Statutory Health
Insurance Physicians. The trained staff at the
center will decide whether the specific case is
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
108
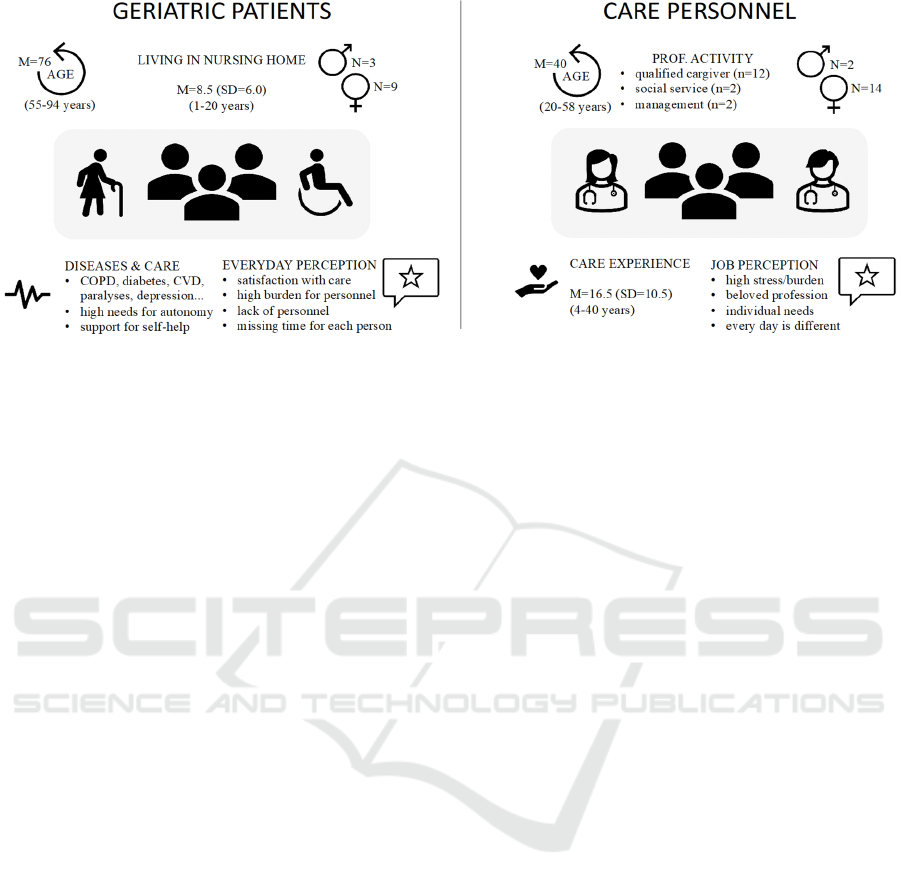
Figure 1: Characteristics of the participants.
suitable for teleconsultation or whether another
step must be taken. If the requirements for a
teleconsultation are met, a wheeled stand
equipped with a camera, monitor, microphone
and specific medical technology equipment (for
measuring blood pressure, oxygen saturation,
pulse, and temperature), is pushed into the
patient's room. Then, a specialist is available in a
time period of maximum 10 minutes. The
physician can communicate live with the patient
and the care personnel and view the electronic
patient file. Once the patient's medical history has
been taken, the telemedicine specialist decides on
the next course of action. If necessary, he or she
can, for example, order the deployment of a
specially trained mobile nurse to the nursing
home, who can then carry out interventions on
site, such as changing a catheter. Actions such as
these can prevent a resident from being rushed to
hospital, instead of being able to remain in their
familiar environment. At the same time, long
waiting times for the difficult-to-reach general
practitioners or specialists should be avoided.”
Subsequent to this information, the participants were
asked to describe their first impressions focusing on
the question if they can imagine using (or agree with)
telemedical consultations in emergency situations.
In a next step, the participants were asked to think
about and describe potential advantages they
associate with the usage of telemedical consultations
in nursing homes. In line with this, the participants
should also anticipate potential concerns or barriers
regarding the usage of telemedical consultations in
emergency situations.
In a last step, the participating patients and care
personnel were asked which specific wishes, needs,
and requirements are considered important and
should be addressed when the telemedical
consultations are implemented in their nursing home.
At the end of the interview, the participants had
the opportunity to comment and give feedback on the
topic or the interview itself, or to ask specific
questions about the project.
Following the interviews, the recorded audio files
were transcribed literally, and were analyzed by
means of qualitative content analysis (Mayring,
2014). For data analysis, a deductive system of
categories was derived based on the literature-driven
interview guide, and iteratively supplemented with
inductive categories after analyzing the data material.
The authors coded the quotations independently and
only indisputable quotations were included in the
categories.
3.3 Participants
Overall, N = 28 participants took part in the interview
study (for details, see Figure 1). Among the
participants, 16 persons belonged to the care
personnel and 11 persons were the residents of
nursing homes, whereas one interviewed person was
an accompanying family member. The participants
belonging to the care personnel were on average 40.4
years old, while most of them were female (n=14).
Most of the care personnel reported a long-term
professional experience in care (> 10 years), while
only five participants indicated 4-5 years of
professional care experience. The caregivers
expressed satisfaction with their profession and doing
their job with conviction. However, they also
described high burdens in their everyday professional
activities due to time restrictions and a lack of
personnel. Further, they pronounced the individual
Needs, Requirements, and Technology Acceptance using Telemedical Consultations in Acute Medical Situations in Nursing Homes
109
needs of their patients/residents and that no two days
are alike within their professional everyday life.
Since all residents of the participating nursing
homes suffered of at least one chronic disease (see
Figure 1), we call this group of participants “geriatric
patients” in this study. The geriatric patients were on
average 76.2 years old, whereas the youngest person
was 55 and the oldest 94 years old. Nine participants
were female (75%). On average, the participants
lived comparably long in the nursing homes (M=8.5
years; SD = 6.0), while only one person lived there
only for one year. All participants suffered from
chronic diseases, such as diabetes, paralyses, chronic
obstructive pulmonary disease (COPD), or
cardiovascular diseases (CVD).
All of them described that they were supported in
their everyday life aiming at a support for self-help
and assistance in being as independent and
autonomous as possible. Regarding living in their
nursing home, the participants were on average
satisfied with care and the respective care personnel.
However, they described the high workload of the
caregivers, the lack of personnel, and resulting
missing times for the individual person (in particular,
for social contact, conversations, etc.).
Focusing on experiences with emergency
situations, both groups described that such situations
occur on a regular basis and that waiting times for
physicians on call are mostly too long. Circumstances
like that frequently lead to hospital admissions and
result in burdens and frequent health deteriorations
for the patients. Participants in both groups
emphasized that something must fundamentally
change in terms of healthcare supply and processes.
4 RESULTS
In the following, the key insights of the interview
study are presented guided by the previously
introduced research questions.
4.1 General Insights (RQ1)
The general perception of the concept of telemedical
consultations in emergency situations was well-
reviewed in both groups.
Among the care personnel, all participants
expressed and expected the telemedical consultations
to be a useful and beneficial approach. All of them
indicated a willingness to use telemedical
consultations and confirmed the implementation of
the telemedical care infrastructure within their
nursing home to be highly appreciated. One
participant added a sceptical comment regarding the
accessibility and the interaction with telemedical
physicians (see RQ3).
Considering the perspectives of the geriatric
patients, all of them showed a positive attitude
towards using telemedical consultations in
emergency or medically uncertain situations. Despite
the positive attitude, two of the respondents were also
sceptical about the implementation in everyday life
and possible technical problems (see RQ3).
Nonetheless, all participants could easily imagine
the usage of telemedicine in their nursing home, and
immediately began weighing possible benefits
against potential concerns.
4.2 Perceived Benefits (RQ2)
Overall, the participants mentioned 21 aspects
referring to potential benefits and motives to use
telemedical consultations in nursing homes. From
these, 13 benefits were mentioned and discussed by
at least two of the participants. These perceived
benefits were divided into three categories and are
shown in Table 1: general benefits, patient-related
benefits, and personnel-related benefits.
Table 1: Identified perceived benefits and their categories.
Patient Faster help in an emergency
Shorter waiting times for medical treatment
Avoidance of hospital admission or stay
Avoidance of transport to the hospital
Avoidance of stress and deterioration of health
Personnel Reducing the workload of caregivers
Quick decisions at the nursing homes
Increase of safety for caregivers through
medical decisions
Flexibility in time and place
General Higher sense of security
Improved sense of care
Improved docto
r
-patient communication
Use of innovative technologies in care
Within the category general benefits, the
participants (in particular, the care personnel)
mentioned that using telemedical consultations would
give them a higher sense of security as fast advice of
medical experts is enabled.
“It simply gives you more safety and a better
feeling.” (Personnel, female, 24)
Further, they expected an improved sense of care
as well as an improved doctor-patient-
communication.
“Maybe it will make residents feel better about
the care they receive – here in the nursing home,
but also in conversations with physicians.”
(Personnel, female, 34)
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
110
Finally, it was also expressed that the use of
innovative technologies in care is beneficial in order
“to move away from old and conventional
conditions more and more” (Personnel, female,
50 years).
The second category included perceived
personnel-related benefits. Here, the geriatric
patients expressed the expectation that the usage of
telemedical consultations would contribute to
reducing the workload of caregivers and enable
flexibility in time and place.
“It would be easier and reduce efforts for the care
personnel because it would be faster and they
would be more flexible.” (Patient, female, 84)
From the perspective of care personnel, the
benefit of quick decisions at the nursing homes was
of major importance and connected with the
expectation that a fast contact to medical experts
would lead to an increase of safety for caregivers
though medical decisions.
“In the future, it may bring relief in care because
responsibility can be handed over; when a doctor
deals with it directly (without waiting time), the
doctor takes responsibility and the decision.”
(Personnel, female, 50)
“And I think it's also a good thing for the
professionals who are at the bedside in this case,
because they are of course often confronted with
uncertainties, they have to make decisions, and
not having to stand there all alone helps, I think,
a lot to overcome these uncertainties.”
(Personnel, female, 25)
The third category referred to patient-related
benefits. Here, both groups of the participants
expected that the use of telemedical consultations
enables faster help in emergencies and shorter
waiting times for medical treatment.
“Decisions are made here on site and, above all,
help can be provided quickly.” (Patient, male, 84)
“If a telemedical consultation would be
guaranteed within 10 minutes, this would be so
great and so much faster than calling a doctor
and he had to come here first. Usually, we have
been waiting many times longer.” (Personnel,
male, 33)
“It would be great to have no, or little, waiting
time here on site.” (Personnel, female, 40)
In addition, more than half of the participants
mentioned the reduction and avoidance of hospital
admissions or stays as well as avoidance of transport
to the hospital as relevant motives to use telemedicine
in nursing homes.
“Sometimes they lie in the emergency room for 6
hours and then come back again – this could be
avoided, and the residents could be spared the
whole procedure (i.e., transport, stay). Especially
for residents with dementia, or other cognitive
impairments, staying in the facility is certainly
always best.” (Personnel, female, 26)
In line with this, also the avoidance of stress and
deterioration of health was mentioned by both care
personnel and geriatric patients, expecting that
reduced or avoided hospitalizations contribute to the
wellbeing of residents in nursing homes.
“Of course, I think that would save a lot of stress
and health deterioration for our residents.”
(Personnel, female, 58)
4.3 Perceived Barriers (RQ3)
Concerning perceived barriers of using telemedical
consultations in nursing homes, the participants
mentioned 15 different aspects, while 14 of them
were discussed by at least two participants. Table 2
presents these 14 potential barriers and concerns,
which were classified into four categories:
communicative concerns, technological concerns,
handling concerns, as well as data management and
privacy concerns.
Table 2: Identified perceived barriers and their categories.
Communicative
concerns
Impersonal/Indirect Contac
t
Distance to physicians providing
treatmen
t
Inconvenient communication of
complaints
Lack of understanding of physicians due
to the distance
Technological
concerns
Immature, possibly deterren
t
technology
Physicians not easy to understan
d
Physicians not easy to recognize
Technical failures (e.g., WLAN)
Technical errors (e.g., pixelated display)
Handling
concerns
Errors in operation (e.g., physicians, care
personnel)
Lack of availability of trained personnel
Overstraining of care personnel
Data & Privacy
Concerns
Insecure data transmission
Invasion of privacy
Starting with communicative concerns, the
concern of impersonal or indirect contact and thereby
a feared distance to the physicians providing
treatment was mentioned by participants of both
groups.
Needs, Requirements, and Technology Acceptance using Telemedical Consultations in Acute Medical Situations in Nursing Homes
111

“The physician has no or only a difficult personal
insight due to the distance.” (Personnel, male, 33)
“It is just not face-to-face communication. Due to
the distance, there is already the danger that the
personality of the patient is not perceived in its
entirety.” (Personnel, female, 50)
“I am concerned that the doctor may not
understand me as well (as usual), because he is
less close.” (Patient, female, 82)
Further, some of the participating geriatric
patients were afraid that due to the distance health
complaints could be communicated inconveniently by
using telemedical consultations.
“I doubt whether I can describe it exactly how I
feel, what I have and that it doesn't come across
right if I say, for example, 'it's pressing there'.”
(Patient, female, 82)
In line with this, both groups of participants
expressed the concern of a lack of understanding of
the physicians due to the distance to the patients.
The second barrier category referred to
technological concerns. Here, some participants of
the care personnel feared that the technology may
have an immature, deterrent effect on the patients –
especially regarding patients suffering from dementia
or other comparable cognitive impairments.
“For cognitively impaired residents in particular,
the new equipment and also the conversation with
the doctor via a monitor could have an initially
deterrent effect.” (Personnel, female, 20)
Furthermore, some of the geriatric patients (and
the accompanying relative) expressed concerns that
the physicians are not easy to understand and not
easy to recognize within the telemedical
consultations.
In line with this, the greatest concerns related to
specific technical problems were expressed
especially by the participating care personnel, but
also occasionally by the geriatric patients. In more
detail, technical failures (e.g., WLAN interruptions)
based on the infrastructure in the nursing homes and
technical errors (e.g., pixelated display) related to
data transmission and the Internet connection were
discussed.
"But if you have got a data connection that doesn't
work before, which is pixelated, that you don't see
the person properly like on TV, if it's raining,
you've got the pixels. It could happen. And then
you think, you're lying there, you want to tell him
something, you can't see him properly and you
think, does this have to be now? Why is that not
possible and he should help me?“ (Relative of a
patient, female, 57)
A third category contained perceived barriers related
to handling concerns. Both groups thought about
errors in the operation of the telemedical
consultations – both on the side of the physicians and
on the side of the responsible care personnel.
“I'm concerned that it won't work properly or
much more that there won't be a person around to
operate it properly.” (Patient, female, 82)
A majority of the participating care personnel
expressed concerns about a lack of availability of
trained personnel, because they have previously
experienced that new systems can often only be
operated by one or a few trained colleagues, who are
not always available on site.
In line with this, some participants also feared –
especially at the beginning – an overstraining of the
care personnel regarding the processes in interaction
with the new technologies.
“And I think, depending on which caregiver
colleague you have, it could be an overload.
Because they're not used to it, it has to settle in
[...]. They're nervous then thinking ‘am I doing
something wrong’?”(Personnel, female, 58)
“Okay, so where do I start this, where do I stop?
Which button do I press now? But all beginnings
are hard and you just don't know. I think you're in
an excited situation anyway, is now the right
moment for me to use telemedicine? That's
another thing, that's new and then putting
everything on and communicating with the
doctor.” (Personnel, female, 34)
The last barrier category related to data and privacy
concerns. Here, a potential insecure data
transmission and an invasion of privacy was
mentioned. However, it was striking that these well-
known barriers in the context of other health-related
technologies (e.g., Peek et al., 2014) were only
sporadically mentioned by our study participants.
4.4 Needs and Requirements (RQ4)
Considering the results regarding specific needs and
requirements, the participants mentioned overall 25
different aspects: 11 of them were discussed by single
participants, while the remaining 14 aspects were
discussed by several participants and were
subsequently classified in four categories:
introduction and training, trust-related conditions,
technology-related conditions, as well as interaction
with physicians (see Table 3).
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
112
The first category contained requirements related
to the introduction and training regarding the
telemedical infrastructure and processes. Here,
almost all care personnel participants desired a
detailed technical introduction as well as regular
technical trainings on how to use the telemedical
consultations and how to behave in such situations
correctly. Further, some of these participants also
desired a refreshment of specific medical trainings in
this context.
“So in any case, a good introduction to the
equipment must take place and not only once, but
also repeatedly. That you are first of all well
accompanied. That would be important."
(Personnel, female, 34)
A second category referred to trust-related
requirements. Here, participants of both groups
mentioned that the availability of trained staff is a
prerequisite for trust. In line with this, trust in the
technology as well as trust in the respective tele-
physicians were also discussed to be relevant
conditions. Beyond that, the requirement of ensuring
data privacy and system security were also
occasionally mentioned.
“There must be trained personnel and the
technology must be operated 100%, of course
everything must also fit technically.” (Relative of
a patient, female, 57)
Concerning technology-related requirements it
was mentioned that in particular the technical
infrastructure has to be created and ensured. The
majority of these comments referred to the often poor
WLAN connection in the nursing homes. Further,
technical support and maintenance were mentioned
to be essential parameters not only in the beginning
but also continuously during the use of the
telemedical consultations. As a last technology-
related aspect, care personnel but also some of the
geriatric patients mentioned the appearance and
design of the wheeled stand to be an important factor:
As new technologies can have a deterrent effect, in
particular to patients suffering from dementia,
unobtrusive and well-known designs should be
focused.
Finally, the category interaction with physicians
included aspects referring to the indirect contact.
Based on previous experiences with physicians on
call, the geriatric patients mentioned the necessity
that the tele-physicians must have enough time for the
consultations and empathy for the residents’
situations. Some care personnel participants specified
this requirement and added that the tele-physicians
should bring along patience for the residents and
their needs. Beyond that, the care personnel
participants highlighted that an understanding of the
tele-physicians for age-typical clinical pictures is
essential.
“Above all, it needs empathetic physicians who
have time and act in the will and support of the
residents.” (Patient, female, 87)
“The physicians must have time for residents
within the consultations, they must be skilled with
geriatric-psychiatric residents and they have to
take both, residents and their needs as well as the
caregivers, seriously.” (Personnel, female, 55)
Table 3: Identified need/requirements and their categories.
Introduction
and training
Detailed technical introduction for staff
Regular technical training for staff
Refreshment of specific medical trainings
for staff (e.g., medical parameters)
Trust Availability of trained staff
Trust in tele-physicians
Ensure data privacy/system security
Trust in the technology
Technology Creation of technical requirements/
infrastructure (e.g., reliable WLAN).
Appearance/design of technology
Technical support and maintenance
Interaction
with
physicians
Tele-physicians must have enough time for
consultations
Understanding of tele-physicians for age-
typical clinical pictures
Empathy of the tele-physicians for the
situation of the residents
Patience of tele-physicians for residents and
needs
5 DISCUSSION
In this qualitative study, we aimed at the uncovering
of acceptance-relevant aspects for the use of
telemedical consultations in acute medical situations
in nursing homes, thoroughly studying two essential
user groups: the residents of nursing homes and the
care personnel. The results enable us to better
understand the perceived benefits and barriers of such
complex, yet highly useful, technology which has the
potential to significantly relieve the processes and
ease consultations with specialized medical
professionals in the long run. This approach can
therefore positively complement the healthcare
system and significantly support the situation in
Germany’s currently troubled institutional care.
Needs, Requirements, and Technology Acceptance using Telemedical Consultations in Acute Medical Situations in Nursing Homes
113

5.1 Key Insights of the Study
Results reveal that the important stakeholders are
open-minded and have generally positive attitudes
towards using telemedical infrastructure. Confirming
previous research (e.g., Peek et al., 2014; Offermann-
van Heek et al., 2019), these attitudes are associated
with the perception of technology-related perceived
benefits and barriers of using the telemedical
infrastructure. In line with previous research (e.g.,
Jaschinski & Allouch, 2015; Offermann-van Heek &
Ziefle, 2018) the perceptions of benefits and barriers
or concerns possessed different priorities and differed
in their depth of detail depending on the two relevant
user groups under study.
In more detail, this study identified concrete
perceived benefits (divided in general, personnel- and
patient-related aspects) of using telemedical
consultation in acute situations in nursing homes. For
instance, the participating residents of nursing homes
expressed rather generic benefits regarding a
potential reduction of the workload and thus a relief
for the everyday life of the care personnel. In contrast,
the participating care personnel described the
perceived benefits of using telemedical consultations
very precisely in terms of quick decisions at the
nursing homes and an increase of safety for them as
caregivers through medical decisions enabled by the
fast contact to medical experts.
On the other hand, the study also identified that
both investigated user groups were concerned about
possible drawbacks that the technology could bring
along. Concrete barriers and concerns were
determined referring to communicative, technology-,
handling- as well as privacy- and data security-related
issues. Among these issues, a major hurdle is posed
to technical requirements and competence in handling
the technology. Not only is the widest possible
expansion of Internet access perceived as vital, but
also an uninterrupted support from technically
competent and well-trained personnel is highly
required. Other concerns refer to possible
communication issues due to the distance to
physicians providing treatment.
Along with the anticipated benefits and barriers of
using telemedical tools, we also gained insights into
the requirements for, and conditions of, the use from
the involved study groups. These requirements
referred to the main topics introduction and training,
technology, interaction with physicians, and trust.
With regard to the latter and in line with previous
research on trust in medical technologies (Montague
et al., 2009; Wilkowska & Ziefle, 2018), needs and
requirements had different priorities depending on
both investigated user groups. To build trust in the
completely novel ways of communication concerning
the sensible topics of health and assistance of frail
persons in nursing home environments, participants
especially required a proper technical training for,
and an accessible technical support from a technically
competent staff; correspondingly, an appropriate
technological infrastructure is necessary in such
facilities. Empathy, patience, and particular
sensitivity for the situation of the nursing home
residents on the part of treating physicians is all the
more vital here – compared to direct interactions in a
doctor-patient situation – and an important
requirement for a successful usage of telemedical
consultations.
5.2 Future Research Agenda
As far as potential stakeholders solely envision the
use of the technology, instead of the real interaction
with the telemedical tools/infrastructure, we have to
expect that the attitudes greatly differ from the actual
use (Ajzen & Fishbein, 1980). A purposeful and
trouble-free use of the telemedical consultations also
requires the perspective of the attending physicians
and can uncover additional issues, which need to be
appropriately addressed. Based on the insights
identified from the first scenario-based qualitative
study that focused on the essential user groups, i.e.,
residents and care personnel, and their attitudes
towards using telemedicine in acute medical
situations in nursing homes, concrete strategies for
further steps of the user-centered investigations
within the Optimal@NRW project can be derived:
1) Fulfilling a holistic user-centered consideration
and in addition to already applied scenario-based
analyses, a major focus must be put on investigations
of acceptance and evaluations of “real” interactions
with telemedical systems. The analysis and
evaluation of direct interactions within telemedical
consultations enables to identify appearing problems,
the users’ unaltered reactions, and relevant process
flows. Up to now, the initially applied scenario-based
approaches of the present study supported the
understanding and enabled an identification of mental
models, opinions, and perceptions regarding care in
nursing homes, existing process flows, and general
attitudes before telemedicine was integrated in the
nursing homes.
2) As the results of this study revealed differences
between the respective user groups, the opinions and
evaluations of all relevant stakeholders (in particular
residents and care personnel) have to be investigated
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
114

and considered in all phases of the project
(before/during/after implementation).
3) For a successful realization of acceptance
research within the project, qualitative and
quantitative methodological approaches have to be
combined. Thereby, interviews have been conducted
in particular at the beginning of the project to identify
wishes, attitudes, and needs of the involved
stakeholders. Further, qualitative approaches will be
applied to enable the involvement of older and frail
participants who are not able to take part in
quantitative surveys. Only on the basis of, and in
addition to, these qualitative analyses a holistic
quantification of the results using (online) surveys is
usefully realizable. Thereby, a combined usage of
qualitative and quantitative approaches enables the
inclusion of different stakeholders and their specific
characteristics.
4) As a last aspect, combining comparative and
summative acceptance analyses along the project
enables to identify changing acceptance parameters
over time (pre- / during / post-implementation).
Further, the empirical approach enables to identify
influencing characteristics of the stakeholders (e.g.,
age, gender, experience), which may also vary over
the different project phases.
Following this research agenda and considering a
social communication science perspective, the user-
centered investigations will contribute to a better
understanding of needs, requirements, and
technology acceptance patterns of partly vulnerable
stakeholders (in particular residents of nursing homes
and their caregivers). Only this way, an appropriate
medical, technical, or organizational adaption of
telemedical processes and infrastructure to the needs
of the respective user groups can be realized.
ACKNOWLEDGEMENTS
The authors thank all participants – residents and care
personnel of the different nursing homes – for their
patience and openness to share opinions on a novel
technology approach in healthcare. Furthermore, the
authors want to thank Anna Rohowsky for research
assistance. Beyond that, the authors thank the
Optimal@NRW research group. This work was
funded by the German joint federal committee
„Innovationsfond“ (grant number: 01NVF19015).
REFERENCES
Ajzen I, Fishbein M., 1980. Understanding Attitudes and
Predicting Social Behavior, Englewood Cliffs, NJ:
Prentice-Hall.
Al-Shorbaji, N., 2013. The World Health Assembly
resolutions on eHealth: eHealth in support of universal
health coverage. Methods of Information in Medicine,
52(06), 463-466.
Amkreutz, J., Lenssen, R., Marx, G., Deisz, R., & Eisert,
A., 2020. Medication safety in a German telemedicine
centre: Implementation of a telepharmaceutical expert
consultation in addition to existing tele-intensive care
unit services. Journal of Telemedicine and Telecare,
26(1-2), 105-112.
Cook, D. J., Augusto, J. C., & Jakkula, V. R. (2009).
Ambient intelligence: Technologies, applications, and
opportunities. Pervasive and Mobile Computing, 5(4),
277-298.
Czaplik, M., Bergrath, S., Rossaint, R., Thelen, S.,
Brodziak, T., Valentin, B., Hirsch, F., Beckers, S.K., &
Brokmann, J. C., 2014. Employment of telemedicine in
emergency medicine. Methods of Information in
Medicine, 53(02), 99-107.
Davis, F. D., 1989. Perceived usefulness, perceived ease of
use, and user acceptance of information technology.
MIS Quarterly, 319-340.
Felzen, M., Beckers, S. K., Kork, F., Hirsch, F., Bergrath,
S., Sommer, A., Brokmann, J.C., Czaplik, M., &
Rossaint, R. (2019). Utilization, Safety, and Technical
Performance of a Telemedicine System for Prehospital
Emergency Care: Observational Study. Journal of
Medical Internet Research, 21(10), e14907.
Flórez-Revuelta, F., Mihailidis, A., Ziefle, M., Colonna, L.,
& Spinsante, S. (2018, September). Privacy-Aware and
Acceptable Lifelogging services for older and frail
people: The PAAL project. In 2018 IEEE 8th
International Conference on Consumer Electronics-
Berlin (ICCE-Berlin). IEEE, pp. 1-4.
Jacobs, K., Kuhlmey, A., Greß, S., Klauber, J., Schwinger,
A. (2018). Pflege-Report 2018: Qualität in der Pflege.
[Care Report 2018: Quality in Care]. Springer Nature.
Jaschinski, C., Allouch, S. B. (2015). An extended view on
benefits and barriers of ambient assisted living
solutions. Int. J. Adv. Life Sci, 7(2), 40-50.
Kollmann, T. (1998). Akzeptanz innovativer Nutzungsgüter
und Systeme: Konsequenzen für die Einführung von
Telekommunikations- und Multimediasystemen.
[Acceptance of innovative consumer goods and
systems: consequences for the introduction of
telecommunication and multimedia systems] Bd. 239.
Springer.
Mayring P. Qualitative content analysis: theoretical
foundation, basic procedures and software solution.
Klagenfurt, 2014. https://nbn-resolving.org/urn:nbn:
de:0168-ssoar-395173
Montague, E. N., Winchester III, W. W., & Kleiner, B. M.
(2010). Trust in medical technology by patients and
healthcare providers in obstetric work systems.
Behaviour & information technology, 29(5), 541-554.
Needs, Requirements, and Technology Acceptance using Telemedical Consultations in Acute Medical Situations in Nursing Homes
115

Offermann-van Heek, J., Wilkowska, W., Brauner, P., &
Ziefle, M. (2019). Guidelines for Integrating Social and
Ethical User Requirements in Lifelogging Technology
Development. In 4th International Conference on
Information and Communication Technologies for
Ageing Well and e-Health (ICT4AWE 2019, pp. 67-79.
Offermann-van Heek, J., & Ziefle, M., 2018. They Don’t
Care About Us! Care Personnel’s Perspectives on
Ambient Assisted Living Technology Usage: Scenario-
Based Survey Study. JMIR Rehabilitation and
AssistiveTechnologies, 5(2), e10424.
Ohligs, M., Stocklassa, S., Rossaint, R., Czaplik, M., &
Follmann, A. (2020). Employment of telemedicine in
nursing homes: clinical requirement analysis, system
development and first test results. Clinical
Interventions in Aging, 15, 1427.
Peek, S. T., Wouters, E. J., Van Hoof, J., Luijkx, K. G.,
Boeije, H. R., & Vrijhoef, H. J. (2014). Factors
influencing acceptance of technology for aging in
place: a systematic review. International journal of
medical informatics, 83(4), 235-248.
Rahimi, B., Nadri, H., Afshar, H. L., & Timpka, T. (2018).
A systematic review of the technology acceptance
model in health informatics. Applied Clinical
Informatics, 9(03), 604-634.
Sundmacher, L., Fischbach, D., Schuettig, W., Naumann,
C., Augustin, U., Faisst, C. (2015). Which
hospitalisations are ambulatory care-sensitive, to what
degree, and how could the rates be reduced? Results of
a group consensus study in Germany. Health policy,
119(11), 1415-1423.
Theou, O., Squires, E., Mallery, K., Lee, J. S., Fay, S.,
Goldstein, J., Armstrong, J.J., Rockwood, K. (2018).
What do we know about frailty in the acute care setting?
A scoping review. BMC geriatrics, 18(1), 1-20.
Venkatesh, V., Morris, M. G., Davis, G. B., & Davis, F. D.,
2003). User acceptance of information technology:
Toward a unified view. MIS Quarterly, 425-478.
Wilkowska, W., Ziefle, M. (2018). Understanding Trust in
Medical Technologies. In Proceedings of the 4th
International Conference on Information and
Communication Technologies for Ageing Well and e-
Health (ICT4AWE 2018), pp. 62-73.
Wootton, R., Craig, J., & Patterson, V. (2017). Introduction
to telemedicine. CRC Press.
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
116
