
The CoroPrevention-SDM Approach: A Technology-supported Shared
Decision Making Approach for a Comprehensive Secondary Prevention
Program for Cardiac Patients
Cindel Bonneux
1
, Deeman Yousif Mahmood
1
, Martijn Scherrenberg
2
, Maarten Falter
2
,
Gustavo Rovelo Ruiz
3
, Hanne Kindermans
4
, Dominique Hansen
5
, Reijo Laaksonen
6
, Paul Dendale
2
and Karin Coninx
1
1
Faculty of Sciences, HCI and eHealth, UHasselt, Diepenbeek, Belgium
2
Faculty of Medicine and Life Sciences, UHasselt, Diepenbeek, Belgium
3
Faculty of Sciences, EDM, UHasselt, Diepenbeek, Belgium
4
Faculty of Medicine and Life Sciences, Healthcare and Ethics, UHasselt, Diepenbeek, Belgium
5
Faculty of Rehabilitation Sciences, REVAL/BIOMED, UHasselt, Diepenbeek, Belgium
6
Finnish Cardiovascular Research Center Tampere, University of Tampere, Tampere, Finland
cindel.bonneux, deeman.mahmood, martijn.scherrenberg, maarten.falter, gustavo.roveloruiz, hanne.kindermans,
Keywords:
Shared Decision Making, Holistic Approach, Secondary Prevention, Cardiovascular Diseases, Behaviour
Change, eHealth.
Abstract:
After a cardiac event, secondary prevention is recommended to foster recovery and reduce the risk of recurrent
events. European guidelines and EAPC position statements on prevention of cardiovascular diseases recom-
mend a holistic approach that actively engages patients by using shared decision making (SDM). It has been
demonstrated that telerehabilitation can be a feasible and effective add-on or alternative compared to conven-
tional in-hospital secondary prevention. However, till date, there is no eHealth solution that offers a holistic
approach for secondary prevention that includes SDM. In this paper, we present the CoroPrevention-SDM
approach, a technology-supported shared decision making approach for a comprehensive secondary preven-
tion program for cardiac patients. The CoroPrevention Tool Suite consists of three applications that support
patients and caregivers in following this approach: 1) a caregiver dashboard that includes decision support sys-
tems and supports SDM, 2) a patient mobile application that supports patients in making behaviour changes
in their daily life, and 3) an extended ePRO application that collects patient reported outcomes and patient
preferences. In a formative usability study, we assessed patients’ and caregivers’ opinion about our approach.
The study indicated that both are willing to use our proposed approach to collaboratively set behavioural goals
during SDM encounters.
1 INTRODUCTION
Cardiovascular diseases are world’s leading cause
of death, accounting for an estimated 17.9 million
deaths globally in 2019 (World Health Organization,
2021). After a cardiac incident, patients typically en-
rol in cardiac rehabilitation as a secondary prevention
to foster recovery and reduce their risk of recurrent
events (Ambrosetti et al., 2021). In this paper, we fo-
cus on two interrelated needs for a guideline-based
secondary prevention program, namely its holistic
perspective and integration of shared decision mak-
ing. Furthermore, we elaborate on our technology-
supported shared decision making approach in the
CoroPrevention project, a large-scale H2020 funded
project on secondary prevention for high-risk pa-
tients. In this section, we consider the state of the art
for the two identified needs and raise ideas to move
beyond the currently implemented clinical practices.
1.1 The Need for a Holistic Approach
1.1.1 State of the Art
European guidelines and EAPC position statements
(Ambrosetti et al., 2021; Visseren et al., 2021) rec-
Bonneux, C., Mahmood, D., Scherrenberg, M., Falter, M., Rovelo Ruiz, G., Kindermans, H., Hansen, D., Laaksonen, R., Dendale, P. and Coninx, K.
The CoroPrevention-SDM Approach: A Technology-supported Shared Decision Making Approach for a Comprehensive Secondary Prevention Program for Cardiac Patients.
DOI: 10.5220/0011042300003188
In Proceedings of the 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2022), pages 59-69
ISBN: 978-989-758-566-1; ISSN: 2184-4984
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
59

ommend that a comprehensive, secondary prevention
program includes the following key components: pa-
rameter monitoring, education, medication, physical
activity, nutrition, smoking cessation, and stress man-
agement. For each of these key components, eHealth
solutions have been developed and are even com-
mercially available. Numerous apps are available in
smartphone’s app stores that enable users to set med-
ication reminders, measure their health parameters,
track their physical activity, record their nutrition in-
take, perform stress relief exercises, or offer smok-
ing cessation support. However, the main disadvan-
tages of these applications are twofold: 1) most of
these applications are not tailored to the risk profile
of a cardiac patient, and 2) to follow a comprehen-
sive, secondary prevention program, the patient has to
use several different applications. Using multiple ap-
plications can result in a higher cognitive burden and
interference of (or even conflicting) advice offered by
different applications.
In scientific literature, numerous studies were
published that evaluated eHealth interventions for
secondary prevention of cardiovascular diseases (Jin
et al., 2019; Brørs et al., 2019). A review performed
by Brørs et al. (Brørs et al., 2019) concluded that the
majority of studies included two or three secondary
prevention components, of which education was em-
ployed in 21 out of the 24 included studies. To the
best of our knowledge, there is no eHealth solution
that fully supports a comprehensive, secondary pre-
vention program, including all key components as de-
fined by Ambrosetti et al. (Ambrosetti et al., 2021)
and that was subject to extensive evaluation on medi-
cal effectiveness and user experience.
1.1.2 Looking Beyond the State of the Art
When working on risk factor reduction to prevent re-
current cardiovascular events, the main parameters to
control are blood pressure, weight, cholesterol, and
glucose levels. For each of these parameters, a tar-
get value can be defined (in line with the European
guidelines and EAPC position statements (Ambrosetti
et al., 2021; Visseren et al., 2021)) and an outcome
goal can be set (i.e. respectively lowering blood pres-
sure, healthy weight, lowering cholesterol, and dia-
betes management). To improve a parameter value
and achieve the associated outcome goal, different
strategies can be followed. For example, a healthy
weight can be achieved by increasing physical ac-
tivity, eating healthier, or a combination of both. It
is important that patients understand how they can
work on an outcome goal. Setting the goal of los-
ing weight until your body mass index (BMI) is below
25 is too abstract for a patient. In the context of be-
haviour change, people need to set actionable goals
that are directly linked to behaviours over which they
have direct control (Medynskiy et al., 2011). There-
fore, we suggest that in a rehabilitation program the
outcome goals for secondary prevention should be
linked to behavioural goals. The following five be-
havioural goals should be considered when aiming at
a healthy lifestyle to prevent recurrent cardiac events:
medication adherence, start moving, healthy nutri-
tion, smoke-free living, and stress relief. For each
of these behavioural goals, specific, short-term goals
should be set (Medynskiy et al., 2011). After defin-
ing the behavioural goals for the upcoming period, it
is equally important that follow-up is done and that
feedback is provided on the progress towards the be-
havioural goals (Scobbie et al., 2011). Therefore, it
is essential that patients can monitor their parame-
ters and caregivers can remotely follow up on these
reported values.
1.2 The Need for Shared Decision
Making
1.2.1 State of the Art
From a clinical point of view, patients should reduce
their cardiovascular disease (CVD) risk as soon as
possible, as much as possible. This would require
optimizing all outcome goals at the same time, and
thus working on multiple behavioural goals simulta-
neously. After a cardiac incident, some patients want
to drastically change their life and are eager to work
on multiple or even all behavioural goals at the same
time. However, this is not advised, since some be-
haviour changes oppose each other (e.g. smoking ces-
sation and losing weight) which results in disillusion-
ment for the patient. Furthermore, working on mul-
tiple behaviour changes simultaneously is not feasi-
ble for everyone. For those patients for whom a dras-
tic approach is not feasible, a more gradual approach
in which they target one behaviour change at a time
works better. In such cases, it has to be decided which
behavioural goal is targeted first. There is evidence
that some factors (which can be linked to behaviour
changes) have a bigger effect on CVD risk than oth-
ers (SCORE2 working group and ESC Cardiovascular
risk collaboration, 2021; SCORE2-OP working group
and ESC Cardiovascular risk collaboration, 2021).
However, if the patient is not willing or able to work
on the behaviour change, it will be almost impossi-
ble to achieve the desired effects. Moreover, there are
patients for whom it will be difficult or even impos-
sible to tackle a certain risk factor. E.g., for a person
with severe rheumatism, it will be very challenging to
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
60

achieve the exercise targets and it is better to focus on
reducing the other CVD risk factors.
For this type of situations, where there is no clear
best choice and the decision has to be made by bal-
ancing the pros and cons of different options (i.e. the
behaviour changes), it is recommended to use shared
decision making (Wennberg et al., 2003). More-
over, shared decision making is at the core of patient-
centered care and the European Society of Cardiology
also acknowledges that patient engagement (in clini-
cal decision making) is needed to improve cardiovas-
cular care (Graham et al., 2017; Institute of Medicine,
2001). Shared decision making (SDM) combines
the patient’s preferences, values, goals, and context
with the clinical evidence and caregivers’ expertise
to make an informed decision (Kon, 2010; Stiggel-
bout et al., 2012), i.e. in this case which behavioural
goal(s) the patient will work on first. When making
this decision, the risk reduction of the different be-
haviour changes should be balanced with the patient’s
motivation to work on these behaviour changes. We
propose to use a digital decision aid or SDM tool in
a shared decision making encounter with the patient,
to support a dialogue about the balancing exercise be-
tween the patient’s motivation for behaviour change
and necessary health risk reduction. Decision aids
are tools that support patients and caregivers in SDM
by making the decision explicit, offering information
about the available options (and their advantages and
disadvantages), and assisting in clarifying congruence
between personal preferences/values and the decision
at hand (Stacey et al., 2017).
To actively participate in shared decision making
and become the manager of their own disease, pa-
tients need to understand their condition and their own
preferences (Joseph-Williams et al., 2014). There-
fore, education is an essential component when con-
sidering shared decision making in the context of sec-
ondary prevention. This education can be delivered
by caregivers during the encounters using a SDM tool,
but also patients can learn on their own using digital
resources such as articles, videos, and infographics
(Sankaran et al., 2018).
1.2.2 Looking Beyond the State of the Art
Recently, Bonneux et al. (Bonneux et al., 2019) pro-
posed three levels of decision-making in cardiac reha-
bilitation (CR):
Level 1 The CR program: the key components to in-
clude and when they get the patient’s focus
Level 2 The key components of the CR program: the
details of the included components
Level 3 The actions for the key components: the de-
tails of what the patient can do to implement
the lifestyle changes in daily life
Cardiac rehabilitation can be considered as a tool
for secondary prevention of cardiovascular disease
(Mampuya, 2012). Therefore, we believe that these
three decision-making levels can be utilized in the
context of secondary prevention of CVD as well. Fur-
thermore, Bonneux et al. (Bonneux et al., 2019) made
a categorization of different tools that can support
patients and caregivers at different points in time in
following a SDM approach for these three levels of
decision-making.
Inspired by patients’ and caregivers’ need for
a holistic approach and shared decision making in
the context of secondary prevention of cardiovas-
cular diseases, we developed the CoroPrevention-
SDM approach. In Section 2, we describe patients’
and caregivers’ requirements for tools supporting
SDM for a comprehensive secondary prevention pro-
gram. In Section 3 and Section 4, we present our
CoroPrevention-SDM approach and highlight how
the digital support that was realised in CoroPreven-
tion fulfills patients’ and caregivers’ needs.
2 PATIENTS’ AND CAREGIVERS’
REQUIREMENTS FOR
SHARED DECISION MAKING
TOOLS
To support patients and caregivers in shared deci-
sion making for the behavioural goals of a secondary
prevention program, the approach of Bonneux et al.
(Bonneux et al., 2019) can be adapted. Whereas guid-
ance of the patient is necessary throughout the sec-
ondary prevention program, shared decision making
is often facilitated in a discrete way, in a number of
(physical) shared decision making encounters. When
looking at a single SDM encounter, we can define
three points in time where digital tools can support
caregivers and patients in shared decision making:
1. Preceding to the SDM encounter
2. During the SDM encounter
3. After the SDM encounter
For these three moments in time, we describe in the
next sections the goals and needs for both patients and
caregivers regarding support for shared decision mak-
ing.
The CoroPrevention-SDM Approach: A Technology-supported Shared Decision Making Approach for a Comprehensive Secondary
Prevention Program for Cardiac Patients
61

Figure 1: The patient’s goals and needs preceding to, during, and after the SDM encounter.
2.1 The Patient’s Perspective
From the patient’s perspective, the aim is to increase
self-management of the disease and therefore become
an active participant in the SDM process. This leads
to a process that balances patient and caregiver de-
cisions regarding the rehabilitation approach. The pa-
tient’s goals and needs that can be supported by digital
tools are depicted in Figure 1. Preceding to a SDM
encounter, digital tools can support patients in be-
coming informed about what will happen during the
encounter. In this regard, patients should think about
their preference to be involved in the decision-making
process e.g. do they want to take the decision, make a
shared decision, or leave the decision to the caregiver.
Furthermore, digital tools can support patients in re-
flecting on their current status, gaining insight into
their progress over the last months and into the next
possible steps. Referring back to the above mentioned
two aims for the patient, information and reflection,
we activate and empower the patient to become ac-
tive participants in the SDM consultation. During the
SDM encounter, digital tools can support patients in
improving their understanding, reflecting on past be-
haviour, stating their preferences, and understanding
what actions should be taken. The desired result is
that the patient can make an informed decision to-
gether with the caregiver during the SDM consulta-
tion and is motivated to work on the agreed behaviour
changes. After the SDM encounter, mobile eHealth
applications can support patients in making the agreed
behaviour changes at home. These applications can
provide patients guidance in how to achieve the be-
havioural goals and how to bring the decisions that
were made during the encounter into practice in their
daily life. There will be moments when the patient
has a setback. At those moments, the tools can sup-
port the patient to feel comfortable while getting back
on track. However, it is important to note that the
tools cannot replace the support of the caregiver but
are rather facilitating the caregiver in this role. In the
next section, we discuss how tools can support care-
givers in achieving their goals.
2.2 The Caregiver’s Perspective
From the caregiver’s perspective, the aim is to make
guideline-based recommendations for the patient’s
treatment, to support the patient in making behaviour
changes, and to follow up on the patient’s progress for
a healthy lifestyle. Similarly as patients, caregivers
have different goals and needs that can be supported
by digital tools at different points in time (Figure 2).
Preceding to the SDM encounter, caregivers can use
digital tools to prepare themselves for the upcoming
appointment, so they can make (together with the pa-
tient) well-informed decisions during the encounter.
Digital tools can support caregivers in reviewing the
patient’s evolution since last consultation and pending
goals. In addition, decision support systems can sup-
port caregivers in preparing for prescribing guideline-
based care to their patients. During the SDM en-
counter, a digital tool can support the caregiver in
discussing the outcome goals that are needed from
a clinical point of view (i.e. transferring knowledge
to the patient) and collaboratively setting behavioural
goals that are in line with the clinical evidence and
the patient’s preferences (i.e. facilitating collaborative
discussion and motivating the patient). The desired
result is that the patient can make an informed deci-
sion together with the caregiver during the SDM con-
sultation and that the patient is motivated to make the
agreed behaviour changes. Between SDM encoun-
ters, caregivers want to follow up on their patients’
progress. However, there is only limited time avail-
able for this follow-up. Therefore, digital tools, such
as dashboard visualizations and alerts, can support
caregivers in following up on the patient’s progress.
Digital tools can alert the caregiver when the patient
deviates from the agreed goals and action plans, so the
caregiver can contact the patient or take this into ac-
count during the next SDM encounter. At those mo-
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
62
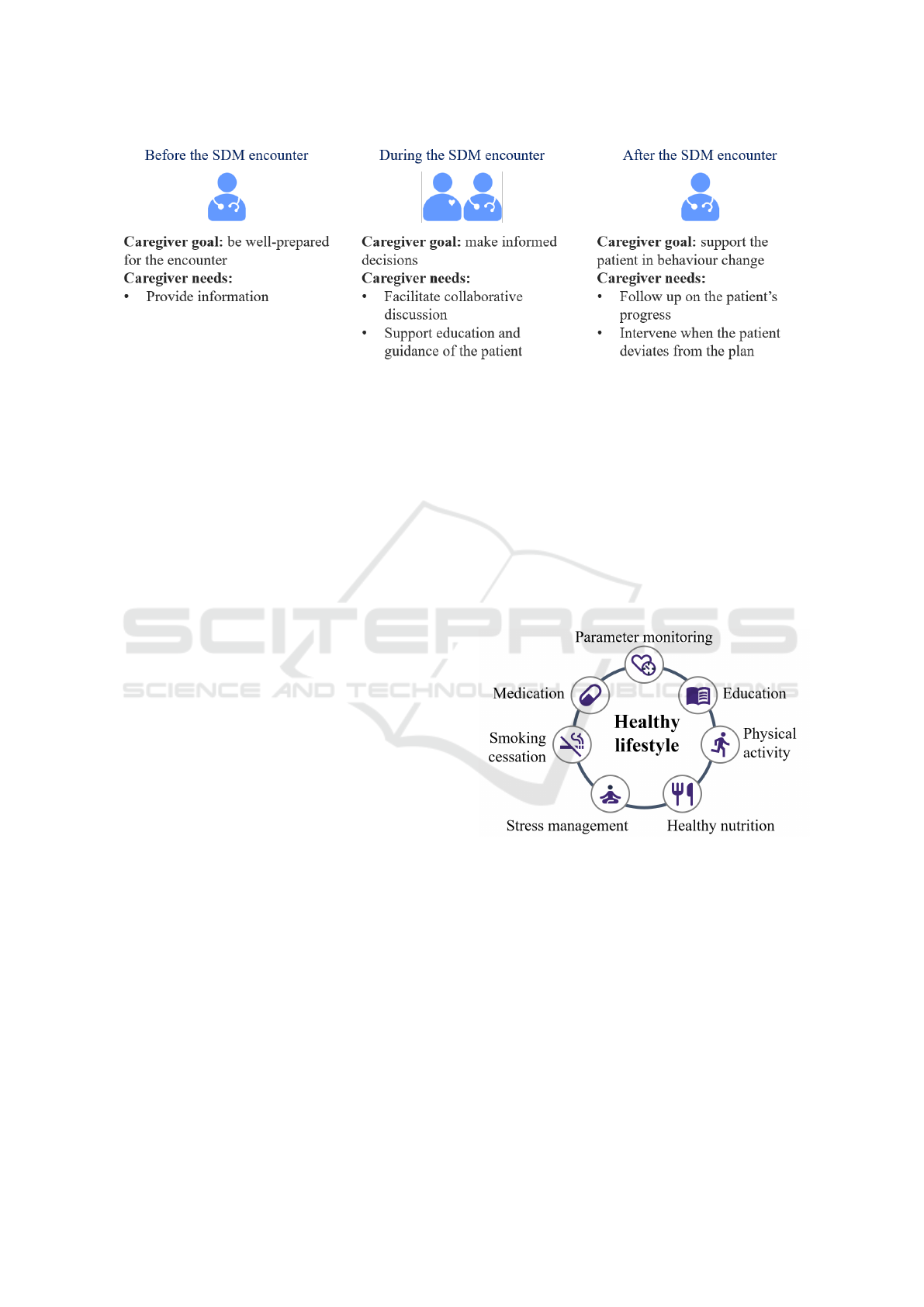
Figure 2: The caregiver’s goals and needs preceding to, during, and after the SDM encounter.
ments in time, the support of the caregiver can help
the patient getting back on track in case of difficul-
ties.
As can be seen in Figure 1 and Figure 2, the goals
and needs of the different stakeholders in the SDM
process are not complementary, but in essence are the
same goals from different (patient and caregiver) per-
spectives. When looking at the goals and needs of
both stakeholders, we can conclude that these can be
satisfied by a selection of the tools proposed in the
categorization of Bonneux et al. (Bonneux et al.,
2019). In the next section, we introduce a possible
timeline for a single SDM encounter and present ac-
companying tools to satisfy the needs of the different
stakeholders (patients and caregivers) in the context
of secondary prevention of cardiovascular diseases.
3 TIMELINE FOR A SHARED
DECISION MAKING
ENCOUNTER
In this paper, we present the CoroPrevention-SDM
approach, a technology-supported shared decision
making approach for a comprehensive secondary pre-
vention program for cardiac patients. As recom-
mended by guidelines and EAPC position statements
(Ambrosetti et al., 2021; Graham et al., 2017; Vis-
seren et al., 2021), the CoroPrevention secondary pre-
vention program implements a holistic approach that
targets the risk factors for cardiovascular diseases and
incorporates shared decision making. To satisfy all
requirements that were stated above (i.e. offering a
holistic approach for secondary prevention, support-
ing shared decision making, and satisfying all patient
and caregiver needs identified in Section 2), we de-
signed and developed the CoroPrevention Tool Suite.
The CoroPrevention Tool Suite takes a holistic ap-
proach for secondary prevention by offering the fol-
lowing 7 modules, when it reaches the full target im-
plementation: parameter monitoring, education, med-
ication, physical activity, healthy nutrition, smoking
cessation, and stress management (Figure 3). The
modules in the Tool Suite are gradually elaborated
further during the project. Most of these modules
can directly be linked to the behavioural goals, i.e.
medication adherence, start moving, healthy nutri-
tion, smoke-free living, and stress relief. The two re-
maining modules, education and parameter monitor-
ing, are essential to support the shared decision mak-
ing process and remote follow-up by the caregiver.
Figure 3: The seven modules of the CoroPrevention Tool
Suite to implement a comprehensive secondary prevention
program for cardiac patients.
The CoroPrevention Tool Suite is composed of
three digital tools that support patients and caregivers
in shared decision making for the secondary preven-
tion program (Figure 4). The first tool is an extended
ePRO application. In the context of the CoroPre-
vention Tool Suite, Electronic Patient-reported Out-
comes (ePRO) are questionnaires for patients to indi-
cate how they are feeling and what they prefer. Pa-
tients use the extended ePRO application on a tablet
in the waiting room (prior to the SDM encounter) to
inform themselves about the SDM process, report on
their current status, and state their preferences. A
The CoroPrevention-SDM Approach: A Technology-supported Shared Decision Making Approach for a Comprehensive Secondary
Prevention Program for Cardiac Patients
63

Figure 4: The timeline and accompanying tools to be used during a single encounter to support shared decision making for a
comprehensive secondary prevention program.
caregiver dashboard with integrated clinical decision
support systems and shared decision making support
is the second tool of the CoroPrevention Tool Suite.
This dashboard is used by caregivers to prepare for
the encounter and to follow up on their patients be-
tween encounters. Furthermore, the caregiver dash-
board can be used during a consultation on a shared
display to encourage collaboration and spark discus-
sion with the patient. The third tool is a smartphone
application that patients use at home to follow up
on their behaviour change process and receive sup-
port for decision-making in daily life. Figure 4 pro-
vides an overview of the usage of the different tools of
the CoroPrevention Tool Suite for a single SDM en-
counter. The tools are categorized according to the
three moments in time that were identified before:
preceding to the SDM encounter, during the SDM en-
counter, and after the SDM encounter.
4 SHARED DECISION MAKING
IN THE COROPREVENTION
TOOL SUITE
In this section, we describe the CoroPrevention Tool
Suite according to the timeline for a single encounter,
i.e. preceding to the SDM encounter, during the SDM
encounter, and after the SDM encounter.
4.1 Preparation of the SDM Encounter
Given the short time available for live encounters
(with an average of just about 10 minutes per pa-
tient (Elmore et al., 2016)), it is important that both
patients and caregivers are well prepared for the en-
counter. To preserve more time during the encounter
for shared decision making, patients can already pro-
vide a status update about their risk factors and related
behavioural goals in the extended ePRO application
preceding to the encounter. In shared decision mak-
ing, it is crucial that the patient’s preferences are taken
into account. These preferences can range from very
high-level e.g. which goals would the patient like to
work on, to very specific e.g. which sports activities
does the patient like to perform. Patients might be
unsure to state their preferences in front of their care-
givers, because they are overwhelmed and did not ex-
pect that their caregivers would ask them about their
preferences. Therefore, the patient’s preferences are
collected before the SDM encounter in the extended
ePRO application. These preferences are depicted on
the shared display during the SDM encounter, which
can encourage patients to talk about their preferences.
For patients that might then still be reluctant to talk
about them, the caregiver can take into account the
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
64
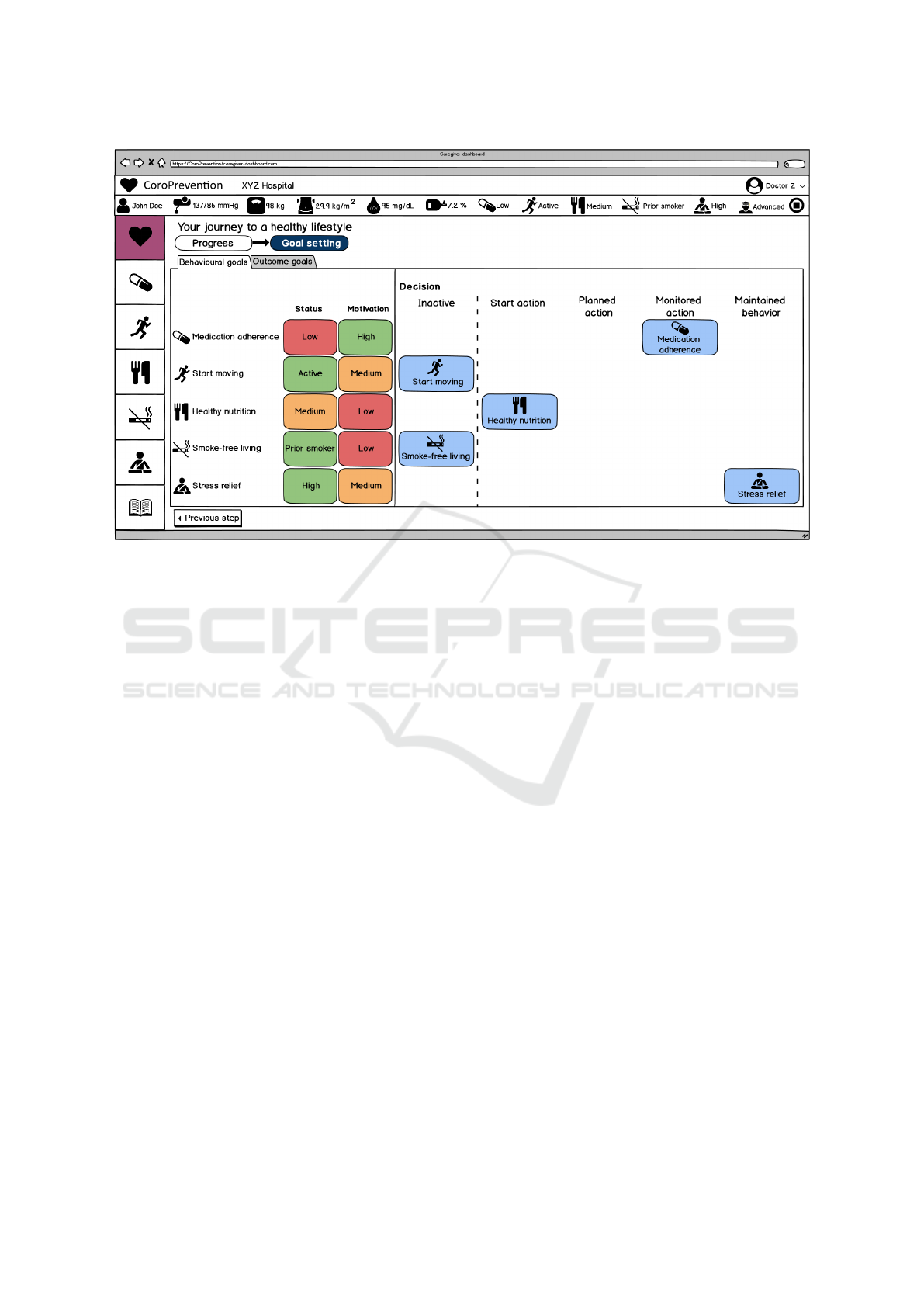
Figure 5: Goal setting of behavioural goals in the caregiver dashboard. The patient and caregiver discuss the patient’s status
and motivation for the behavioural goals and decide upon the patient’s behavioural goals for the upcoming period.
preferences that were collected by the system. Col-
lecting this information before the SDM encounter
does not only lead to more time for decision-making
during the encounter, but also provides patients a clear
moment to reflect on their status, behaviour, and pref-
erences. Furthermore, a video offered in the extended
ePRO application before the first SDM encounter al-
ready provides the patient some information about
shared decision making in general and familiarizes
him/her with the process that will follow.
Next to patients, caregivers also need to be well-
prepared for a SDM encounter. If desired, caregivers
can prepare themselves for the encounter by checking
the patient’s performance in the last months and pend-
ing goals in the caregiver dashboard. Furthermore,
clinical decision support systems (CDSS) can support
caregivers in prescribing guideline-based care to their
patients. In the CoroPrevention caregiver dashboard,
we incorporated the EXPERT tool (Hansen et al.,
2017a; Hansen et al., 2017b) for guideline-based ex-
ercise prescription and a decision support system for
medication prescription. A detailed description of
these systems is beyond the scope of this SDM arti-
cle. Using DSS systems during encounters with pa-
tients can be cumbersome and might affect the pa-
tient’s perception of the caregiver’s credibility and au-
thority. Also, using a clinical decision support system
before the SDM encounter leaves more time during
the SDM encounter to discuss the decisions that were
made with input of the CDSS, set goals, and decide
upon the actions that the patient should take to achieve
these goals.
4.2 Shared Decision Making
Consultation
During the SDM encounter, the dashboard acts as a
SDM tool that supports the shared decision making
conversation between the caregiver and the patient.
They start by discussing the patient’s evolution in
the past period and his/her current status for the be-
havioural goals and related outcome goals. For the
outcome goals (e.g. lowering blood pressure, lower-
ing cholesterol, and healthy weight), shared decision
making is not possible in our approach, as these goals
are determined based on clinical guidelines and the
caregiver’s expertise. Moreover, cholesterol and hy-
pertension are more influenced by medication than
by lifestyle changes. Therefore, the caregiver will
strongly emphasize the importance of medication ad-
herence to reduce the patient’s CVD risk. Neverthe-
less, behaviour changes such as reducing salt intake,
exercising more, and eating healthier can be other
ways to work on these outcome goals. Therefore,
it is still important to discuss the patient’s outcome
goals during the encounters. Based on the patient’s
outcome goals and status, the behavioural goals (e.g.
increasing physical activity, eating healthier, and quit-
The CoroPrevention-SDM Approach: A Technology-supported Shared Decision Making Approach for a Comprehensive Secondary
Prevention Program for Cardiac Patients
65

ting smoking) that the patient should work on from
a clinical point of view can be determined and dis-
cussed (Figure 5). The patient’s motivation (that was
collected in the extended ePRO application) to work
on these behavioural goals is depicted to spark discus-
sion and encourage the patient to state his/her prefer-
ences. During the discussion, the patient and care-
giver agree upon a feasible behavioural goal for the
patient (i.e. decision-making level 1). After deciding
upon the behavioural goal, they discuss and record the
plans to achieve this goal (i.e. decision-making level
2 and possibly even decision-making level 3). If the
patient and caregiver agree to set multiple behavioural
goals, the process restarts to set the next behavioural
goal. During this process, the caregiver’s role is not
only to support the patient in decision-making, but
also to motivate the patient to work on the agreed be-
havioural goals. At the end of the SDM encounter,
a feasible set of behavioural goals has been agreed
upon and action plans have been recorded to support
the patient in achieving these goals. This informa-
tion is used to configure the mobile application that
belongs to the CoroPrevention Tool Suite on the pa-
tient’s smartphone, that will guide the patient until the
next SDM encounter.
4.3 Remote Follow-up
Between SDM encounters, at home, the mobile ap-
plication supports the patient in working on the be-
havioural goals and making smaller decisions in daily
life (i.e. decision-making level 3). In the mobile ap-
plication, patients receive support to make decisions
on a daily basis (e.g. which sports activities will I
perform today) and can follow up on their medication
intake. Furthermore, they can record their progress
(e.g. tracking sports activities) and follow up on their
journey towards a healthy lifestyle. Based on the pa-
tient’s progress, the mobile application makes recom-
mendations to increase/decrease the support for the
behavioural goals. However, patients can also decide
themselves to start or stop working on a behavioural
goal (patient autonomy) and as such, become the
manager of their own disease. When the patient ac-
tivates a new behavioural goal, the mobile application
supports the patient in setting feasible goals and con-
structing action plans. However, there will also be
moments when the patient has difficulties. At those
moments, the mobile application (and caregivers) will
be there to help the patient getting back on track. The
data that is collected in the patient mobile application
is used as input in the next SDM discussion.
Caregivers can follow up on their patients between
visits by receiving alerts about their patients’ progress
and behaviour, which can be consulted in the care-
giver dashboard. Given the busy schedules of care-
givers and the large number of patients that they have
to supervise, it should be avoided that caregivers re-
ceive too many alerts. Therefore, some alerts are han-
dled automatically by the CoroPrevention Tool Suite,
without requiring input of the caregiver (e.g. send-
ing tailored educational material to the patient to en-
courage the patient to take action). However, in some
cases (e.g. when the patient’s medication adherence is
very low), caregivers may want to intervene (e.g. call
the patient to assess barriers). The CoroPrevention
caregiver dashboard facilitates this decision to care-
givers by offering all information and triggering alerts
with regard to the status of a patient.
5 FORMATIVE EVALUATION OF
THE COROPREVENTION-SDM
APPROACH
To the best of our knowledge, the concept of set-
ting behavioural goals collaboratively during SDM
encounters has not yet been investigated in the past in
the context of secondary prevention of cardiovascular
diseases. We assessed patients’ and caregivers’ opin-
ion on our proposed shared decision making approach
for secondary prevention as part of a formative us-
ability study of the different applications of the Coro-
Prevention Tool Suite. The formative usability study
was approved by the Medical Ethical Committees of
Hasselt University and Jessa Hospital Hasselt. 10 car-
diac patients and 7 caregivers were asked about their
willingness to use the tools of our proposed SDM ap-
proach to set behavioural goals. After participants
were acquainted with the caregiver dashboard and/or
mobile application by performing an individual task-
based formative usability test regarding some of the
modules of the CoroPrevention Tool Suite, they filled
in a custom-made questionnaire consisting of sev-
eral Likert-scale questions. Caregivers were asked if
they were willing to use a caregiver dashboard during
their consultations with patients to discuss patients’
progress and set goals for a healthy lifestyle. Simi-
larly, patients were asked if they would be willing to
use a caregiver dashboard during a consultation with
a caregiver to discuss their progress and set goals for
a healthy lifestyle. Furthermore, patients were asked
if they would be willing to use a mobile application to
follow up at home on their journey towards a healthy
lifestyle.
The results of our survey are depicted in Figure 6.
All participants (both patients and caregivers) unani-
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
66

Figure 6: Patients’ and caregivers’ willingness to use the digital tools of the CoroPrevention Tool Suite.
mously agreed that they would be willing to use the
proposed tools supporting the CoroPrevention-SDM
approach. There were a few neutral responses. For
the patients that participated in the study, these neu-
tral responses might be due to the fact that the car-
diac patients that participated in the usability study
already completed cardiac rehabilitation quite a long
time ago. Therefore, using these tools might be less
relevant for them at this moment. As a minor limita-
tion, we should note that there is a possibility for bias
in favour of more motivated patients, due to the way
in which we recruited our participants, i.e. people that
already participated in cardiac rehabilitation and were
willing to participate in a formative usability test.
6 CONTRIBUTIONS AND
FUTURE DIRECTIONS
European guidelines and EAPC position statements
(Ambrosetti et al., 2021; Graham et al., 2017; Vis-
seren et al., 2021) recommend that secondary preven-
tion programs offer a holistic approach and incorpo-
rate shared decision making as a means to engage pa-
tients. We are not aware of any existing system that
offers this support at the time of writing this paper.
Current systems include only some of the key compo-
nents of secondary prevention and/or do not support
shared decision making. This prompted us to design
and develop a technology-supported shared decision
making approach for a comprehensive secondary pre-
vention program for cardiac patients.
6.1 Summary of Contributions
The contributions of this paper are the following:
• Bringing together patients’ and caregivers’ needs
with the European guidelines and EAPC position
statements for secondary prevention in a holistic,
shared decision making approach for secondary
prevention of cardiovascular diseases;
• Incorporating the resulting needs in a Tool Suite
that supports patients and caregivers in following
a SDM approach for a comprehensive secondary
prevention program;
• Deriving initial insights on collaborative goal-
setting for behavioural goals based on a formative
usability study of our proposed approach and ac-
companying tools with patients and caregivers.
In Figure 1 and Figure 2, we provided an overview of
cardiac patients’ and their caregivers’ goals and asso-
ciated needs for tools supporting SDM for a compre-
hensive secondary prevention program. During the
design phase, this overview supported us in selecting
features that support the target users and ensuring that
the designed applications fit with end users’ needs.
We believe that the overview of goals and needs can
be generalized to any eHealth intervention supporting
shared decision making for a healthy lifestyle. There-
fore, we hope that our overview can be useful for
other researchers working in this field.
In this paper, we presented the CoroPrevention-
SDM approach and accompanying Tool Suite consist-
ing of three applications supporting a shared decision
making approach for a comprehensive cardiac sec-
ondary prevention program. We illustrated how these
tools align with the categorization of tools to support
shared decision making of Bonneux et al. (Bonneux
et al., 2019) and with our conceptual figures (Figure
1 and Figure 2). Furthermore, we gave a high-level
overview of the core features of the different tools of
the CoroPrevention Tool Suite. However, a detailed
overview of the features and design of the different
applications is out of scope for this paper.
Lastly, we evaluated our proposed
CoroPrevention-SDM approach in a question-
naire that was part of a formative usability study. Our
survey showed that both patients and caregivers are
interested in using our proposed CoroPrevention Tool
Suite to set behavioural goals during shared decision
The CoroPrevention-SDM Approach: A Technology-supported Shared Decision Making Approach for a Comprehensive Secondary
Prevention Program for Cardiac Patients
67

making encounters. This gives a first indication of
patients’ and caregivers’ willingness to use digital
tools for SDM, but a more thorough investigation
is needed to evaluate the impact of these tools on
patient outcomes, such as health parameters, but also
motivation and engagement in the decision-making
process.
6.2 Future Directions
In our formative usability tests using wireframes,
we collected preliminary insights on patients’ and
caregivers’ willingness to follow our proposed
CoroPrevention-SDM approach and evaluated the us-
ability of the different applications of the Coro-
Prevention Tool Suite. Currently, our proposed
CoroPrevention-SDM approach and supporting Tool
Suite are in development, and gradually extended
with additional modules. As a next step, we plan
to investigate if the tools of the CoroPrevention Tool
Suite support shared decision making. In a summa-
tive test with the application modules that will used in
the RCT, we will let patients and caregivers collabora-
tively set personalized goals during a SDM encounter.
Next, in the second half of 2022, a large-scale
randomized controlled trial (RCT) will start to eval-
uate our proposed technology-supported shared de-
cision making approach for a comprehensive sec-
ondary prevention program for cardiac patients (ref-
erence to https://clinicaltrials.gov/ anonymized for re-
view). In the RCT, 12000 coronary heart disease pa-
tients will be recruited across 6 European countries, of
which 2000 high-risk patients will be enrolled in the
nested RCT that evaluates the CoroPrevention-SDM
approach and accompanying Tool Suite. Over a pe-
riod of three years, patients and their supporting care-
givers will use the CoroPrevention Tool Suite to set
personalized goals for the patients and follow up on
their progress. Human-Computer Interaction related
outcomes will include the usability and user experi-
ence of the different tools, patients’ motivation for be-
haviour change, and the influence of the Tool Suite on
shared decision making.
7 CONCLUSIONS
In this paper, we identified varying needs and
requirements for a holistic approach for a sec-
ondary prevention program for cardiovascular dis-
eases. Based on these needs, we designed the
CoroPrevention-SDM approach and accompanying
Tool Suite. The CoroPrevention-SDM approach is
a technology-supported shared decision making ap-
proach for a comprehensive secondary prevention
program for cardiac patients. The CoroPrevention
Tool Suite consists of three applications supporting
our proposed approach: 1) an extended ePRO ap-
plication to collect patient’s status and preferences,
2) a caregiver dashboard with integrated clinical de-
cision support systems and shared decision making
support, and 3) a patient mobile application support-
ing behaviour change. A formative usability study of
the applications indicated that both patients and care-
givers are willing to use the designed applications and
follow the CoroPrevention-SDM approach. A more
thorough evaluation of our proposed approach and
supporting applications is planned for early 2022.
ACKNOWLEDGEMENTS
The research presented in this paper was supported
by grants from the Special Research Fund (BOF)
of Hasselt University (BOF18DOC26), and from
FWO (Fellowship 1SE1222N, and the FWO-ICA
project EXPERT network G0F4220N). The CoroPre-
vention project has received funding from the Euro-
pean Union’s Horizon 2020 research and innovation
programme under grant agreement No 848056.
REFERENCES
Ambrosetti, M., Abreu, A., Corr
`
a, U., Davos, C. H.,
Hansen, D., Frederix, I., Iliou, M. C., Pedretti, R. F.,
Schmid, J.-P., Vigorito, C., et al. (2021). Sec-
ondary prevention through comprehensive cardiovas-
cular rehabilitation: From knowledge to implementa-
tion. 2020 update. a position paper from the secondary
prevention and rehabilitation section of the european
association of preventive cardiology. European jour-
nal of preventive cardiology, 28(5):460–495.
Bonneux, C., Rovelo, G., Dendale, P., and Coninx, K.
(2019). A comprehensive approach to decision aids
supporting shared decision making in cardiac rehabil-
itation. In Proceedings of the 13th EAI International
Conference on Pervasive Computing Technologies for
Healthcare, pages 389–398. ACM.
Brørs, G., Pettersen, T. R., Hansen, T. B., Fridlund, B.,
Hølvold, L. B., Lund, H., and Norekv
˚
al, T. M. (2019).
Modes of e-health delivery in secondary prevention
programmes for patients with coronary artery disease:
a systematic review. BMC health services research,
19(1):1–24.
Elmore, N., Burt, J., Abel, G., Maratos, F. A., Montague, J.,
Campbell, J., and Roland, M. (2016). Investigating the
relationship between consultation length and patient
experience: a cross-sectional study in primary care.
British Journal of General Practice, 66(653):e896–
e903.
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
68

Graham, I., Filippatos, G., Atar, D., Vardas, P. E., Pinto,
F. J., and Fitzsimons, D. (2017). Patient engagement.
Hansen, D., Coninx, K., and Dendale, P. (2017a). The eapc
expert tool. European Heart Journal, 38(30):2318–
2320.
Hansen, D., Dendale, P., Coninx, K., Vanhees, L., Piepoli,
M. F., Niebauer, J., Cornelissen, V., Pedretti, R.,
Geurts, E., Ruiz, G. R., Corr
`
a, U., Schmid, J. P.,
Greco, E., Davos, C. H., Edelmann, F., Abreu, A.,
Rauch, B., Ambrosetti, M., Braga, S. S., Barna, O.,
Beckers, P., Bussotti, M., Fagard, R., Faggiano, P.,
Garcia-Porrero, E., Kouidi, E., Lamotte, M., Ne-
unh
¨
auserer, D., Reibis, R., Spruit, M. A., Stettler, C.,
Takken, T., Tonoli, C., Vigorito, C., V
¨
oller, H., and
Doherty, P. (2017b). The European Association of
Preventive Cardiology Exercise Prescription in Every-
day Practice and Rehabilitative Training (EXPERT)
tool: A digital training and decision support system
for optimized exercise prescription in cardiovascular
disease. European Journal of Preventive Cardiology,
24(10):1017–1031.
Institute of Medicine (2001). Crossing the Quality Chasm:
A New Health System for the 21st Century. The Na-
tional Academies Press, Washington, DC.
Jin, K., Khonsari, S., Gallagher, R., Gallagher, P., Clark,
A. M., Freedman, B., Briffa, T., Bauman, A., Redfern,
J., and Neubeck, L. (2019). Telehealth interventions
for the secondary prevention of coronary heart dis-
ease: A systematic review and meta-analysis. Euro-
pean Journal of Cardiovascular Nursing, 18(4):260–
271.
Joseph-Williams, N., Elwyn, G., and Edwards, A. (2014).
Knowledge is not power for patients: a systematic re-
view and thematic synthesis of patient-reported barri-
ers and facilitators to shared decision making. Patient
education and counseling, 94(3):291–309.
Kon, A. A. (2010). The shared decision-making continuum.
Jama, 304(8):903–904.
Mampuya, W. M. (2012). Cardiac rehabilitation past,
present and future: an overview. Cardiovascular di-
agnosis and therapy, 2(1):38.
Medynskiy, Y., Yarosh, S., and Mynatt, E. (2011). Five
strategies for supporting healthy behavior change. In
CHI ’11 Extended Abstracts on Human Factors in
Computing Systems, CHI EA ’11, page 1333–1338,
New York, NY, USA. Association for Computing Ma-
chinery.
Sankaran, S., Bonneux, C., Dendale, P., and Coninx, K.
(2018). Bridging patients’ needs and caregivers’ per-
spectives to tailor information provisioning during
cardiac rehabilitation. In Proceedings of the 32nd In-
ternational BCS Human Computer Interaction Con-
ference 32, pages 1–11.
Scobbie, L., Dixon, D., and Wyke, S. (2011). Goal setting
and action planning in the rehabilitation setting: de-
velopment of a theoretically informed practice frame-
work. Clinical Rehabilitation, 25(5):468–482.
SCORE2-OP working group and ESC Cardiovascular risk
collaboration (2021). SCORE2-OP risk prediction
algorithms: estimating incident cardiovascular event
risk in older persons in four geographical risk regions.
European Heart Journal, 42(25):2455–2467.
SCORE2 working group and ESC Cardiovascular risk col-
laboration (2021). SCORE2 risk prediction algo-
rithms: new models to estimate 10-year risk of cardio-
vascular disease in Europe. European Heart Journal,
42(25):2439–2454.
Stacey, D., L
´
egar
´
e, F., Lewis, K., Barry, M. J., Bennett,
C. L., Eden, K. B., Holmes-Rovner, M., Llewellyn-
Thomas, H., Lyddiatt, A., Thomson, R., et al. (2017).
Decision aids for people facing health treatment or
screening decisions. Cochrane database of systematic
reviews, (4).
Stiggelbout, A. M., Van der Weijden, T., De Wit, M. P.,
Frosch, D., L
´
egar
´
e, F., Montori, V. M., Trevena, L.,
and Elwyn, G. (2012). Shared decision making: re-
ally putting patients at the centre of healthcare. BMJ,
344:28–31.
Visseren, F. L. J., Mach, F., Smulders, Y. M., Carballo, D.,
Koskinas, K. C., B
¨
ack, M., Benetos, A., Biffi, A.,
Boavida, J.-M., Capodanno, D., Cosyns, B., Craw-
ford, C., Davos, C. H., Desormais, I., Di Angelan-
tonio, E., Franco, O. H., Halvorsen, S., Hobbs, F.
D. R., Hollander, M., Jankowska, E. A., Michal, M.,
Sacco, S., Sattar, N., Tokgozoglu, L., Tonstad, S.,
Tsioufis, K. P., van Dis, I., van Gelder, I. C., Wan-
ner, C., Williams, B., and ESC Scientific Document
Group (2021). 2021 ESC Guidelines on cardiovascu-
lar disease prevention in clinical practice: Developed
by the Task Force for cardiovascular disease preven-
tion in clinical practice with representatives of the Eu-
ropean Society of Cardiology and 12 medical societies
With the special contribution of the European Asso-
ciation of Preventive Cardiology (EAPC). European
Heart Journal, 42(34):3227–3337.
Wennberg, J. E., Fisher, E. S., and Skinner, J. S. (2003). Ge-
ography and the debate over medicare reform. Health
Affairs, page W96.
World Health Organization (2021). Cardiovascular diseases
(cvds). Accessed on 18/11/2021.
The CoroPrevention-SDM Approach: A Technology-supported Shared Decision Making Approach for a Comprehensive Secondary
Prevention Program for Cardiac Patients
69
