
Be Aware! Indications for Intercultural Awareness for Digital Health
Innovations and Innovation Capability
Lena Otto
a
, Linda Kosmol
b
, Tim Scheplitz
c
and Hannes Schlieter
d
Research Group Digital Health, Technische Universität Dresden, Dresden, Germany
Keywords: Digital Health Innovation, Dimension of National Culture, Interview Study.
Abstract: Cultural influences on single Digital Health Innovation (DHI) processes or on a society’s capability to
promote DHI development and implementation remain difficult to describe and to manage on different levels
of responsibility. Using Hofstede’s Dimensions of National Culture, we investigated the influence of each
dimension on DHI to support awareness and to derive valuable indications for both practice and research. An
expert study with 23 participants representing 13 different European countries explored the influence of a
nation’s characteristic on how the DHI domain is supported or slowed down. The results describe indications
for all six dimensions of Hofstede, but “Uncertainty Avoidance” and “Indulgence” are highlighted as the
interviewees could assess their influence on DHI confidently. Combined with cultural aspects that do not rely
on nationalities, our contribution can improve scientific and practice-oriented initiatives especially in context
of international collaborations or of DHI for multi-national usage scenarios.
1 INTRODUCTION
Digital health changes the way healthcare is delivered
by introducing “tools and services that use
information and communication technologies to
improve prevention, diagnosis, treatment,
monitoring, and management of health-related issues
and to monitor and manage lifestyle-habits that
impact health” (European Commision, 2020).
Various terms, topics or artefacts shall be
differentiated but all have the same aim: to improve
access to and quality of care and make healthcare
more efficient (European Commision, 2020).
Even though expectations regarding digital health
are high, studies show that various countries are not
equally ready or capable of implementing digital
health into their national health systems (Thiel et al.,
2019). Hence, the question is to whether there is a
common characteristic inherent in these countries
responsible for the different levels of readiness or
capability. Prior studies have investigated a variety of
barriers and enablers, i.e., influential factors to Digital
Health Innovation (DHI) processes and found that
a
https://orcid.org/0000-0003-3814-4088
b
https://orcid.org/0000-0003-0413-5968
c
https://orcid.org/0000-0003-0070-4561
d
https://orcid.org/0000-0002-6513-9017
culture is one of these (Kowatsch et al., 2019; Yusif
et al., 2017). National culture also has a big influence
on innovation capability, which in turn can increase
the competitiveness of a country (Prim et al., 2017).
Based on these findings, the question arises to what
extent DHI processes are influenced by culture.
Culture can be defined in many ways, but
Hofstede’s definition by using 6 dimensions to
describe a national culture is perhaps the most
popular one and commonly used (Hofstede et al.,
2010; Srite and Karahanna, 2006). The framework of
Hofstede has been applied by many researchers to
investigate a variety of domains. In particular, it has
been studied how culture influences the degree of
innovation of countries (Moonen, 2017; Prim et al.,
2017), the innovative strength of businesses (Gallego-
Álvarez and Pucheta-Martínez, 2021) or the
technology acceptance of a nation (Srite and
Karahanna, 2006).
The influence of culture in the domain of
healthcare has been partially investigated, e.g., by
integrating the cultural dimensions of Hofstede into
the Technology Acceptance Model or the Unified
Theory of Acceptance and Use of Technology to
Otto, L., Kosmol, L., Scheplitz, T. and Schlieter, H.
Be Aware! Indications for Intercultural Awareness for Digital Health Innovations and Innovation Capability.
DOI: 10.5220/0011009900003123
In Proceedings of the 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2022) - Volume 5: HEALTHINF, pages 801-811
ISBN: 978-989-758-552-4; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
801

explain eHealth or telemedicine adoption and use
(Hoque and Bao, 2015; Nwabueze et al., 2009).
Nevertheless, these studies investigate cultural
influence in the healthcare systems primarily from the
patient or technology user perspective rather than
from a systemic view of innovation in healthcare.
Braithwaite et al. applied cluster analysis to
investigate the cultural influence on the performance
of health systems in certain OECD countries and
conclude that cultural characteristics play an
important role on this performance (Braithwaite et al.,
2020). However, they focus on the performance of
health systems in general and not on DHI capability.
Hence, we want to understand how and to what
extent culture affects DHI processes and,
consequently, a society’s capability to promote DHI.
This supports learning about differences between the
state of DHI and provide new research questions that
may result in further evidence in best practices. Our
understanding of the term “DHI” is thereby process-
oriented, as cultural aspects influence the way of how
an innovative digital health artifact is designed,
developed and implemented. We see five scenarios
within the context of scaling DHI projects which are
affected by cultural differences and, thus, may benefit
from our investigation:
Management of DHI projects for international
usage contexts
Management of DHI projects with
cross-boarder collaborations
Interpretation and adaption of best practices
from different countries
Design and management of international DHI
spaces and programs
Supporting the National policy making in
developing and managing the legal framework
for DHI implementation
Therefore, our research lies at the intersection of
three topics: (digital) health, (digital) innovation, and
culture. Conclusively, the following research
question arises: How do a country’s characteristics of
national culture influence DHI processes regarding
and the related structure in DHI environments?
To analyze this influence, we conducted a
qualitative analysis. We held interviews with 23
experts from 13 European countries to get deeper
insights into their health system’s structure and
innovation processes. This explorative approach was
deemed feasible as the influence of culture on the
structure and innovation capability of healthcare
1
https://www.hofstede-insights.com/product/culture-
compass/
systems is not yet a well-investigated topic. We
provide descriptive findings in this paper and enrich
the knowledge base around healthcare systems and
their structure with a focus on cultural factors and
DHI. This lays the groundwork for further studies
investigating that topic in detail, which can derive
recommendations for best practices on how to handle
especially internationalization in digital health.
2 FUNDAMENTALS
2.1 Dimensions of National Culture
Culture can be defined in many ways, either based on
shared values or problem solving, or by using other
all-encompassing definitions (Straub et al., 2002).
Hofstede’s definition is “arguably the most
predominantly used” (Srite and Karahanna, 2006).
According to Hofstede, “culture is the collective
programming of the mind that distinguishes the
members of one group or category of people from
others” (Hofstede, 2011). Various patterns and
dimensions exist to describe the facets of culture
(Straub et al., 2002), with Hofstede’s dimensions of
national culture being most frequently used.
Hofstede describes national culture by using six
dimensions (Hofstede et al., 2010): Power Distance,
Uncertainty Avoidance, Individualism vs.
Collectivism, Masculinity vs. Femininity, Long-
Term vs. Short-Term Orientation, and Indulgence vs.
Restraint. These dimensions depict how a society’s
culture affects the value and behavior of its members.
They are briefly described in Table 1. Based on these
dimensions and through multiple cross-national and
replication studies, Hofstede and other colleagues
have generated a dataset that contains the value scores
for the cultural dimensions for 111 countries and
regions around the world. As this data set is provided
on Hofstede’s website, it is eagerly used for further
research, despite criticism and discussion (Gaspay et
al., 2009). In the following, the Hofstede dimensions
are briefly described as per the Culture Compass, and
as communicated to our study participants. The
Culture Compass
1
is a questionnaire to assess an
individual's scores regarding the cultural dimensions.
2.2 Prior Research
Some previous studies already identified an influence
of Hofstede’s cultural dimensions on the degree of
Scale-IT-up 2022 - Workshop on Scaling-Up Health-IT
802
innovation in certain countries, that we like to
investigate further within the domain of DHI. For
instance, Prim et al. analyzed the influence of cultural
dimensions on the degree of innovation in general
(Prim et al., 2017). They found a negative relation for
PDI and a positive one for IDV.
Other authors investigating the role of Hofstede’s
cultural dimensions on (IT) adoption and innovation
also concluded that a high PDI has a negative (Halkos
and Tzeremes, 2013; Thatcher et al., 2003) and a high
IDV a positive effect on the degree of innovation
(Moonen, 2017; Yaveroglu and Donthu, 2002).
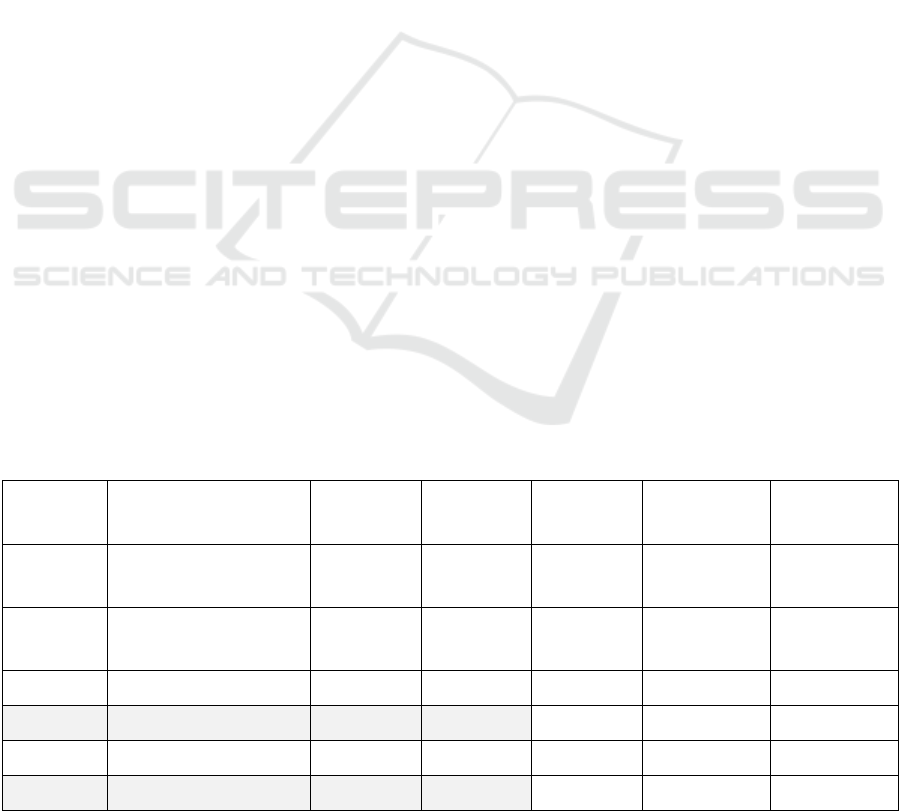
Table 1: Dimensions of national cultures (Hofstede et al.,
2010).
PDI A high value of Power Distance indicates a high
acceptance of power being distributed unequally
within a society; hierarchy is needed rather than
just being a convenience.
Societies with a low
score in the PDI dimension put emphasis on the
importance of equal rights, as opposed to the
importance of privileges of the more powerful
one.
UAI A high value of Uncertainty Avoidance
indicates a need for predictability and structure,
often in the form of written and unwritten rules.
Societies scoring low in the UAI dimension
consider uncertainty as normal and each day is
taken as it comes.
IDV In societies with a high score in the
Individualism dimension, there is a strong sense
of "I", meaning that one’s personal identity is
distinct from others’. In collectivist societies
(low score in IDV), there is a strong sense of
"we", illustrating a mutual practical and
psychological dependency between the person
and the in-group.
MAS In societies with a high score in the Masculinity
dimension, people tend to focus on personal
achievement, material success and the
importance of status. In feminine societies (low
scores), people are more concerned with quality
of life, taking care of those less fortunate,
ensuring leisure time, and finding consensus.
LTO Societies with a high score in the Long-term
Orientation dimension, focus on perseverance
and thrift. Short-term oriented societies (low
scores) emphasize respect for traditions and
fulfilling social obligations.
IVR Societies with a high score in Indulgence
dimension reflect a positive attitude and the view
that one can act as one pleases. In contrast, in
restraint societies (low score) gratification of
needs is regulated by strict social norms and
leisure is less important.
Also, the dimensions of MAS and UAI were
already found by other authors to be negatively
related to the degree of innovation (Halkos and
Tzeremes, 2013; Prim et al., 2017), while Moonen
sees this negative connection only during the
initiation phase of innovations, while a higher level of
masculinity can be positively influencing when
implementing innovations. Halkos and Tzerenes
underline that the environment of innovations is often
uncertain which is especially contradictory in
countries with a high score of UAI (Halkos and
Tzeremes, 2013). Moonen and Prim et al. showing
that planning and optimism can be very supportive
not only for innovations in general but also for DHIs
and postulate a positive influence of LTO and IVR
(Moonen, 2017; Prim et al., 2017).
2.3 Initial Indications of Influence
To gain insights into the status of DHI capability in
different countries and whether or how this is linked
to Hofstede's cultural dimensions, we related the
country-specific scores of the Hofstede dimensions
(values from 2015) to the country-specific values of
the Digital Health Index (DH Index, values from
2018) by the Bertelsmann foundation (Thiel et al.,
2019). We examined whether and to what extent the
values correlate with the Hofstede values. Hofstede
scores were available and originally marked as valid
for all 17 countries ranked within DH Index. Table 2
presents the results of our analysis. The only
significant correlation with the DH Index is regarding
MAS. We interpreted this correlation only as first
indication for our further research activities.
Table 2: Correlation analysis - dimensions of national
culture and DH Index; significance highlighted in grey.
Dimension Correlation & Si
g
nificance
PDI Corr: -0,40;
p
-value: 0,103
IDV Corr: -0,05;
p
-value: 0,841
MAS Corr: -0,48;
p
-value: < 0,05
UAI Corr: -0,37;
p
-value: 0,140
LTO Corr: -0,27;
p
-value: 0,295
IVR Corr: 0,19;
p
-value: 0,468
Although the amount of research on the influence
of Hofstede’s dimensions of national culture on DHI
processes and capability is scarce, there are previous
studies that identified and described their influence on
innovation capability in general. Prim et al. found a
negative relation for PDI and a positive one for IDV
(Prim et al., 2017). Other authors investigating the
role of Hofstede’s cultural dimensions on (IT)
Be Aware! Indications for Intercultural Awareness for Digital Health Innovations and Innovation Capability
803

adoption and innovation also concluded that a high
PDI has a negative (Halkos and Tzeremes, 2013;
Thatcher et al., 2003) and a high IDV a positive effect
on the degree of innovation (Moonen, 2017;
Yaveroglu and Donthu, 2002).
Also, the dimensions of MAS and UAI were
already found by other authors to be negatively
related to the degree of innovation (Halkos and
Tzeremes, 2013; Prim et al., 2017), while Moonen
sees this negative connection only during the
initiation phase of innovations and a positive relation
when implementing innovations (Moonen, 2017).
Also, a positive influence of LTO and IVR have
been stated in general as planning and optimism is
highlighted as very supportive for innovation projects
(Moonen, 2017; Prim et al., 2017).
3 METHODS
Drawing on the initial, quantitative indications, we
approached the study of the relationship between
dimensions of national culture and DHI in an
explorative, qualitative way. We followed this
approach with expert interviews, as literature on the
influence of culture on digital health innovation
processes and on healthcare system’s digital health
capability is scarce. The aim was to get a diverse
picture on European countries, which rank different
in the culture dimensions, to investigate the
relationship between culture and DHI.
3.1 Study Design
The expert interviews followed a semi-structured
interview guide supplemented with additional
questions for clarification, examples, and deeper
insights. The interview guide included three parts.
The 1st part involved organizational matters, e.g.,
consent to recording of the interview and questions
about the interviewee, such as working experience
and current position in the healthcare system.
In the 2nd part, the interviewees were asked about
the structure and innovation processes of their
country's healthcare system and their understanding
of how digital innovation is introduced. Questions
related to these two topics were, e.g. “Who are the
main actors driving DHIs in your country?”, “What
strengths of the people/the healthcare system enable
DHIs?”, or “Do DHI ecosystems exist?”.
2
Scores available via https://geerthofstede.com/research-
and-vsm/dimension-data-matrix/
The 3rd part focused on the central part: cultural
influence on the healthcare system. The interviewees
were asked about characteristic traits, strengths and
trust into the government that may influence the
healthcare system and how innovation takes place in
that domain. Afterwards, the Hofstede values for each
country as well as the individual Culture Compass
results served as a basis to investigate how the
dimensions may influence the country's health system
structure and digital health innovation capability. The
country scores of each cultural dimension were
categorized as being very low, low, average, high, or
very high, compared to the distribution of all
Hofstede country scores. Each interviewee was given
this categorization and a description of what it means
according to Hofstede. Afterwards, they could
subjectively assess if they feel this is true for their
country and if it has an impact on how the healthcare
system is structured or how DHI processes happen.
Also, all experts were asked if best practices from
healthcare systems in other countries are only
imported from countries that are similar or if the
healthcare system’s structure of the other country is
not relevant for adopting best practices. The aim of
that was to analyze if structural or cultural similarity
makes it easier to learn from each other.
3.2 Participant Selection
To obtain a diverse picture of European countries, we
looked for participants with national backgrounds
that scored both minimal and maximal for each of the
six cultural dimensions
2
. For each dimension, two
countries were selected that are among the five
highest or the five lowest scoring countries in this
dimension. In selecting, countries with more than one
extreme value among the culture dimensions were
prioritized. For example, Denmark has one of the
lowest scores in PDI, MAS, UAI, and LTO, and one
of the highest scores in IVR. Similarly, the scores of
Romania are among the highest for PDI and among
the lowest for IDV and IVR. Another aspect for
country selection was the diversity between
geographic parts of Europe. We aimed to include at
least two countries per part of Europe.
Interviewees in each country were contacted via
two big European networks focusing on DHIs and/or
digital health ecosystems as they were expected to be
experts for their country’s health systems. Those
networks are the European Innovation Partnership on
Active and Healthy Ageing (EIP on AHA) and the
Scale-IT-up 2022 - Workshop on Scaling-Up Health-IT
804
European Connected Health Alliance (ECHAlliance).
In both networks, key stakeholders were contacted via
mail to recommend suitable interview partners in each
of the selected countries. The goal was to interview two
experts per country, which is why the interviewees
were also asked to suggest further experts in their
country with a position different from their own one.
To analyze the answers given by each interviewee in
the right context, all participants were given access to
the Culture Compass survey with an individual code.
The results mirror the background of each interviewee
more specifically than the general country scores.
3.3 Interview Conduction
The interviews were conducted in February and
March 2021 in the form of online video conferences,
which mainly lasted around an hour of time. In total,
23 persons (11 women, 12 men) were interviewed.
The goal of two interviews per country was reached
in ten countries: Belgium (one interview for the
Dutch-speaking Flemish, one for the French-speaking
Walloon part), Croatia, Denmark, Estonia, Finland,
Germany, Greece, Italy, Portugal and the United
Kingdom (one interview for Northern Ireland, one for
Scotland). For Norway, Romania, and Slovakia only
one expert was willing to participate in our study.
Alongside with the interviews, publicly available
data on the healthcare system was used to obtain
additional insights. All interviewees, except for one,
had at least five years of experience in the healthcare
sector. All of the interviewees had a health-related
background, seventeen additionally had an IT-related
background, and nine of the seventeen had an
innovation background on top. Also, the
organizational background of all 23 interviewees was
quite diverse, ranging from employees of
governmental authorities, network organizations or
universities to healthcare providers and consultants.
3.4 Interview Analysis
All responses were analyzed across all interviews
according to the specific questions. We checked for
relationships between the cultural scores and
responses, e.g., if the existence of digital health
ecosystems or the trust in government are dependent
on certain cultural characteristics. Additionally, the
perceived influence of each cultural dimension on the
innovation structure or capability were analyzed
across all interviews to receive an overall statement
per dimension.
4 RESULTS
Below, we lay out what impact the Hofstede
dimensions had on innovation in the national
healthcare system as perceived by the interviewees.
Table 3 summarizes whether a relationship was seen
and interpreted as being positive or negative.
Especially for the PDI and IDV dimension, a
beneficial or detrimental influence on DHI of a high
or low score might depend on the phase of the
innovation, e.g., initiation or implementation. This
distinction arises primarily from the main actors in
the two phases: while start-ups, companies or
researchers are more likely to be the driving force
during the creative initiation phase, implementation
in the health sector requires governmental authorities
(e.g. for a national roll out of DHIs).
Table 3: Correlation perceived by the interviewees regarding Hofstede’s dimensions of national culture and DHI capability.
Stated positive or negative relationships highlighted in grey for further discussion.
Dimension Overall Positive Negative Part-part No correlation I don’t know
PDI
Depends on the step in
the innovation process
4 8 4 2 5
IDV
Depends on the step in
the innovation process
4 6 2 1 10
MAS Weak negative 2 6 0 1 14
UAI Negative 0 13 1 0 9
LTO Weak positive 7 2 0 3 11
IVR Positive 13 1 0 1 8
Be Aware! Indications for Intercultural Awareness for Digital Health Innovations and Innovation Capability
805

In the following, the results per dimension with
the feedback and thoughts of the experts are presented
more in detail. We rearranged the order of
presentation to: first, discuss MAS as this is the only
dimension that correlates directly with DH Index
;
second, focus on UAI and IVR as these dimensions
were commonly assessed influential by the experts;
and last, complete the overview of interview results
with selected impressions of the remaining
dimensions PDI, IDV and LTO.
4.1 Masculinity (MAS)
The dimension MAS was associated with caring,
status, position, quality of life, and well-being. To
counteract the problem of this dimension being often
linked to gender roles (Gaspay et al., 2009), we have
only paraphrased this dimension in the interview, but
not mentioned it by name. The majority of the
interviewees, 14 out of 23, did not know how to
interpret MAS in the context of DHI. The
interviewees remarked that the healthcare system is
generally oriented toward the common welfare in
terms of structure and goals, thus inherently feminine
and caring for people. Looking at the individual
actors in the healthcare domain, e.g., doctors or
politicians, a high MAS was considered rather
obstructive, especially for the implementation of
DHIs, since the pursuit of status of the individual may
be in opposition to the idea of the common good.
4.2 Uncertainty Avoidance (UAI)
The dimensions UAI and LTO were difficult to
delineate, but we try to focus on each dimension
separately. UAI was associated with system structure,
regulation, risk taking, predictability, and in the
health context strongly with evidence. The
interviewees identified an almost exclusive negative
relation between UAI and DHI capability. Reasons
for that are that a high UAI slows down innovation
due to falsely assumed security (GER), and that a
“need for stability may disrupt innovation” (SLK)
because “in order to accept innovation you need to
accept uncertainty” (ITA). Other feedback was also
related to the individual context in each country, e.g.,
that in Denmark, due to a good social security system,
risks can be taken, people are not afraid of risks and
thus can drive innovation (DEN).
Over all interviews, the experts expressed that
UAI itself may hinder innovation as it leads to people
not taking risks and not focusing on change.
However, they also expressed that security is nice to
have on the personal level. Some healthcare
specificities also affect this dimension, as the
healthcare sector immanently requires certainty in
terms of evidence-based medicine and is strongly
structured and highly regulated. By highly regulating
it, the healthcare sector tries to give security and
stability. However, this should not go too far, as an
Estonian interviewee mentioned: “Healthcare is
moving to […] a more regulated field […], but on the
other hand you can’t go too far with the rules because
every person is an individual and there are so many
variables when you make treatment or diagnostic
decisions that you can’t describe all rules”.
All in all, there seems to be a negative relation
between UAI and the DHI capability.
4.3 Indulgence (IVR)
IVR was associated with how optimistic people in
each country are and how far they are open for new
things/innovations and are not afraid to fail in the area
of innovation. This was considered for the initiation
and implementation phase alike. The IVR dimension
was not very much commented on but more than half
of all interviewees (n=13) saw a positive connection
between IVR and innovation.
The statements of the interviewees fully support
the quantitative results, namely that there is a strong
positive relation between IVR and innovation in
healthcare, i.e., the higher a country’s IVR the higher
its degree of innovation in digital healthcare
4.4 Statements on Other Dimensions
4.4.1 Power Distance (PDI)
PDI was particularly associated by the interviewees
with hierarchies, communication opportunities and
information flows with stakeholders of DHIs, and
national or regional governmental regulations in
general. Regarding the effect of PDI, eight
interviewees indicated that PDI and innovation are
negatively correlated as it was associated with few
opportunities for entrepreneurs as well as limited
participation and communication flows. On the other
hand, four interviewees felt that strong hierarchies are
helpful for DHIs, as they can drive and support
innovation from the top.
Another four interviewees differentiated between
the impact of PDI on innovation initiation and
innovation implementation. A low PDI was perceived
as beneficial in the initiation phase, but for
implementation a higher PDI was considered more
advantageous. A lower PDI is perceived better for
Scale-IT-up 2022 - Workshop on Scaling-Up Health-IT
806

initiation and creativity regarding DHIs as “[low PDI
results in] flat hierarchies that give people the ability
to think, you encourage them and that helps [DHI]”
(BEL-Flanders) and “you get feedback and support”
(DEN). A “[high PDI] makes it harder to innovate,
harder to implement a solution because success is
affected by your position in the hierarchy” (CRO).
This is also reflected by some respondents who
indicated that the country’s innovation processes are
either bottom-up or bottom-up in combination with a
top-down approach, but not exclusively top-down.
In terms of DHI implementation, a higher PDI
was considered better since it may speed up decision-
making and implementation processes due to less
discussions, "it is just decided, we will do it this way"
(GER). Moreover, in the healthcare domain “no
innovations were successful that have not been given
blessing by higher level decision-makers” (CRO)
implying the need for governmental support.
Additionally, some interviewees concluded that
an average value, something in between strong and
flat hierarchies, is the worst for DHI initiation and
implementation, as it neither fosters innovation
through consensus nor enforcement.
Further, we observed that countries with existing
or developing DHI ecosystems tend to have a lower
or average PDI value which may suggest that the
value of networks is more likely to be recognized in
countries with a low PDI.
4.4.2 Individuality (IDV)
The dimension IDV was associated with creativity,
entrepreneurship, forerunners/leaders, teamwork,
collaboration, and group dependency vs. a focus on
an individual. As with PDI, in different phases of DHI
different IDV traits were considered necessary by the
majority of the interviewees. A higher IDV was
perceived to be better for initiating DHIs as
“innovation needs to be started by strong individuals”
(CRO) and a high IDV was linked to innovative
forerunners, albeit "[too high IDV] might prevent
working in a team and this is crucial for innovation
[implementation]” (BEL-Flanders). Hence, a lower
IDV was regarded as helpful for implementation, i.e.
the rollout of DHIs, because forerunners with ideas
will have to work in groups or be supported by groups
to reach broader mass, acceptance, and consensus and
actually implement DHIs (DEN). The need for groups
or network thinking also became clear as many of the
interviewees' countries increasingly rely on or have
defined the emergence of ecosystems in the
healthcare sector as a goal. 17 of the 23 experts
reported that they either have several ecosystems
mainly on the regional level or one central one
already in place or are currently working on it.
4.4.3 Long-term Orientation (LTO)
The dimension LTO was often associated by the
interviewees with legislation (periods), regulation
and predictability. Many interviewees expressed the
political uncertainty regarding rules as related DH
strategies are highly dependent on the governance
periods (BEL-Flanders, CRO, EST). This was also
expressed as a sector-specific aspect as healthcare is
highly influenced by the government, regarding the
regulation but in some countries also regarding
financing and research funding. Another aspect
related to the dependence on legislation periods is
political will, which needs to be present to bring DHI
forward (“You need political will to make this all
happen” (FIN) and "[it is] not a question of regulation
but political will" (POR)).
Even though eleven interviewees were uncertain
regarding a possible relation, seven saw a positive
relation, two a negative one and three saw no relation
at all. Reasons for seeing a positive relation were that
it would be better for the healthcare sector and DHIs
if regulations and agendas would last longer than one
legislation period as this would increase the
plannability for all stakeholders, which in turn
supports the innovation capability. Even though the
administration in some countries works on long-term
strategies or visions, this is in some countries still
subject to change when a new minister comes in
(BEL-Flanders). A similar observation was made in
Greece: A stronger focus more on the long-term is
needed and ”we [Greeks] have strategies, but in
practice actions are guided by where the money is”.
In other countries, such as Estonia, “strategies are not
changing with the governments”. From some experts,
a negative relation was seen as in that people may
stick to the status quo when LTO is high, which in
turn hinders innovation (GER).
Based on the qualitative results, we cannot fully
confirm but like to call a tendency towards a positive
relation between LTO and the DHI capability.
4.5 System Comparisons
In planning the interview, we expected to see an
influence between cultural characteristics and best
practices from other countries that are adapted and
implemented. Our expectation was that countries
rather look into countries with a similar system and,
even if not directly intended, with comparable
cultural dimension scores to get inspiration or adapt
Be Aware! Indications for Intercultural Awareness for Digital Health Innovations and Innovation Capability
807

best practices. However, the qualitative results could
not support this view. Only in some countries, the
focus is on similar structures but not necessarily on
the country-level. In Slovakia, for example, Scotland
is taken as an example as they are similar in size of
population and structure of the system. Another
example is Belgium where Netherland and France are
looked at as they both have a Bismarck system and
are closely related to Belgium. Also, Switzerland is
looked at as it also has different cultures within one
country like Belgium. In general, the experts stated
that – no matter how similar or diverse a country’s
structure or healthcare system is compared to others
– each best practice from another country needs to be
“translated” to the specific national conditions. The
focus is on “pick and change” (BEL-Flanders), which
is mostly done on a small-scale level (e.g. region or
municipality rather than country level) as pointed out,
e.g., by experts from Estonia, Germany, United
Kingdom and Italy.
5 DISCUSSION
Based on the qualitative results, we have found
valuable indications about how Hofstede’s
dimensions of national culture influence DHI
processes and/or DHI capability of societies. We
could therefore confirm the importance of cultural
factors for the area of DHIs and support the thesis that
“an understanding of culture is important to the study
of information technologies (IT) in that culture at
various levels, including national, […] can influence
the successful implementation and use of information
technology” (Leidner and Kayworth, 2006).
Regarding the main usage scenarios of intercultural
awareness stated in the introduction, we provide in
the following practical and scientific implications.
5.1 Implications for Research
With our study we contribute to the knowledge base
regarding the influence of national culture focused on
DHI processes and capability. Our indications lay the
groundwork for further studies especially for
hypothesis building that can help beneficial
investigations for increasing the DHI capability in
healthcare systems worldwide.
Our findings do not provide final evidence on
whether or how a single dimension of national culture
influence DHI processes or capability. Regarding our
observations and argumentation above, we’d rather
like to highlight MAS, UAI and IVR as dimensions
for further research. MAS and UAI are two
dimensions that seem to have a negative influence on
the degree of innovation in general and also in the
digital health area. IVR was seen as having a positive
influence not only on innovations in general but also
on the innovation capability in digital healthcare, i.e.,
the more optimistic the people in a country and
healthcare system, the easier new innovations are
initiated and implemented. In contrast to our
approach, further investigations should more focus
these dimensions to foster evidence on their influence
and interdependencies. We therefore recommend to
precise hypotheses or research questions by content
but extent the number of participants or interviewees
for a proof our indications.
Based on further large-scale studies including
other countries worldwide, best practices could be
identified between certain countries belonging to one
cultural cluster as it has been done by Braithwaite et
al. for the performance of health systems (Braithwaite
et al., 2020). Our study only laid the groundwork into
this direction by identifying correlations, which are
partially different for certain phases in the innovation
process. A deeper analysis of the various phases of
the DHI process could reveal finer granular results.
Based on this, precise recommendations could be
derived in how far each of the phases can be
supported best depending on in which country the
innovation takes place.
Another finding of our study was that best
practices from other countries are rather found and
implemented on a regional, not on a national level.
This is also underlined by initiatives such as EIP on
AHA, where certain regions across Europe are
connected to share their experiences and knowledge.
The structures of national healthcare systems may be
too diverse on a national but more similar on a
regional level. This could also be further investigated
in future studies if there are sub-cultures within
several countries which are more similar at this
regional than on the national level and can therefore
be considered when getting new impulses for
improving the healthcare system and its innovation
capability regarding digital health.
5.2 Implications for Practice
When starting the study, our hypothesis was that DHI
ecosystems can support the successful long-term
implementation of digital health innovations and thus
a society’s DHI capability but that the existence of
such ecosystems is dependent – among others – on
cultural aspects. With our study, we could generally
confirm our assumption and found indications for a
detailed and differentiated view on those cultural
Scale-IT-up 2022 - Workshop on Scaling-Up Health-IT
808

aspects. Our investigation highlights thereby
Hofstede’s dimensions MAS, UAI and IVR but does
not reject the other dimensions. Rather, we argue that
MAS, UAI and IVR might be a suitable starting point
for increasing cultural awareness activities and
discussions. In harmony to our motivation, we would
like to promote the use of our indications in practice
for: I) Analysis of multi- or international usage
contexts of upcoming DHI projects to adjust
requirements of DHI artefacts or innovation process
models; II) Management purposes of international
collaboration for DHI projects to improve internal
project organization; III) Interpretation and adaption
of “best practice” and “lesson learned” description or
case study research; and IV) Design and conduction
of international DHI initiatives and programs that
seek to support DHI knowledge exchange or to build
international data or innovation spaces.
While technological progress will continue
dynamically, established structures of health systems
(e.g., its segmentation, regulation and administration)
are rough to change simultaneously due to their
linkage to national culture. International intended
DHI projects or programs should not underestimate
the task of bridging such gaps. In Slovakia, for
example, the innovation-driving health insurance
company is private, which leads to implemented DHI
but also lacks in accessibility to society (only for
ensured people). A similar case could be found in
Germany, where pilots are financed by various health
insurance agencies and only people insured by the
respective agency are then able to use them. In
Croatia, old-fashioned laws affecting DHIs can be
interpreted flexible, which supports DHIs, while the
peer pressure from other countries further boosts the
initiation and implementation of DHIs. The system in
the United Kingdom, in turn, supports DHIs by its
segmentation. As a national health system exists for
each member state, networking is easy as each system
is autonomous and relatively small, so that the actors
involved know each other what enables collaboration.
Differences in the presented dimensions of
national culture may have led to structural country-
specific aspects that were also noted by the
interviewees. For example, the Greek interviewees
also highlighted financing is a crucial element.
Greece relies heavily on EU funding and may hence
have less “in-house” structures to support DHIs than
other countries. Also, dimensions of national culture
may be influenced the development of digital
infrastructures (EST), the level of education and
innovation mentality (NOR) or principles of equity
and equality (FIN) that do now positively influence
ongoing and upcoming DHI progress. On the
contrary, the Romanian interviewee expressed a
general mentality to settle with things and to lower
consequently the desire to pursue the new which can
also hinder innovations in general. Additionally, one
German expert expressed that Germans trust in
regulations and are only seldomly pragmatic, which
can negatively influence the speed of innovations.
Those longitudinal dependencies of cultural aspects
leading to structures and phenomena and again
leading to positive or negative DHI influence factors
are scientifically investigated as “path dependencies”
(Arthur, 2021) and should also be more considered in
practice-oriented discussions of international DHI
projects or programs.
Two additional thoughts mentioned by a Belgium
and a Romanian expert should complete this practical
implication section. First, the case of Belgium
showed that culture and (innovation processes in) the
healthcare system can differ vastly even within one
country. Even though the Flemish and the Walloon
system together with Brussels form Belgium, there
are different cultures and (healthcare) systems in
place in each region. Thus, our implications regarding
“international cultural awareness” could also be
valuable for intranational DHI projects or programs
under specific circumstances.
Second, the Romanian interviewee expressed that
culture does not seem to play a major role for the
innovation capability in the healthcare system of
Romania. Rather, missing leaders and money are the
most important problems that need to be solved to
focus more strongly on DHIs. “Even if you had all
this mentality and all these other aspects [positively
influencing cultural factors], if you don’t have the
money to buy an aspirin, […] you can dream a lot but
it is pretty much impossible to do the innovation.”
Thus, our presented implications might be very
helpful but should be reflected with the inclusion of
other, directly noticeable issues.
5.3 Limitations
Our study is limited in three areas, the usage of
Hofstede’s dimensions of national culture, the
conducted qualitative analyses and the influence
further cultural perspectives beyond nationalities.
The six cultural dimensions of Hofstede are not
the only concept that can be used for describing
cultures on a national level and are also subject of
criticism and discussion (Gaspay et al., 2008). Other
dimensions are, e.g., monochronism vs. poly-
chronism (Hall, 1976) or locus of control (Smith et
al., 1995). The former describes if there is a focus
rather on performing one or several activities in
Be Aware! Indications for Intercultural Awareness for Digital Health Innovations and Innovation Capability
809
parallel and the latter if one’s own life is seen as being
controlled external or internally (Leidner and
Kayworth, 2006). However, Hofstede’s dimensions
are often used and can easily be applied to one’s own
research as the country scores and the Culture
Compass are publicly available. As these dimensions
are widely used, they also enable a comparison
among studies conducted by different researchers.
Also, the qualitative study contains some
limitations. Although we had a number of
interviewees with different professional as well as
cultural backgrounds, the statements collected remain
a sample of experiences that may not be
representative in a certain country. We aimed to take
personal bias and the character traits of our
interviewees into account by applying the Culture
Compass and involving two persons per country, but
a differentiation between an individual experience
and group opinion/national culture remains difficult.
Also, our study focused exclusively on European
countries and is therefore limited to these countries.
Further large-scale studies are needed in future work
to confirm the results also for other countries.
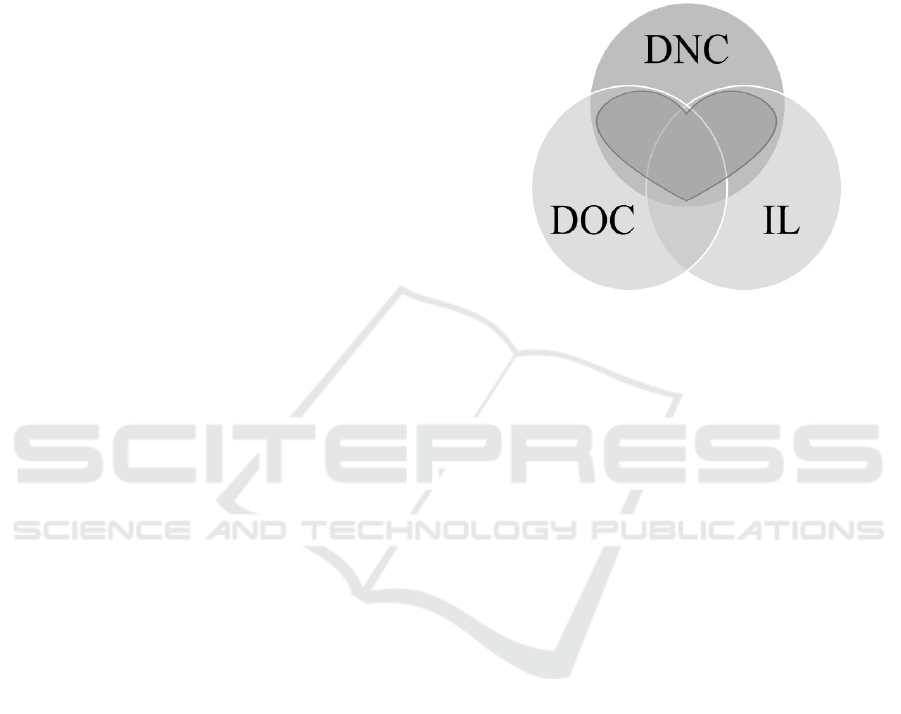
Our study focuses on differences between
national cultures. However, "cultural" factors
influencing the success of DHI processes and the DHI
capability of societies can also be stated from other
perspectives. Broaden the realm of cultural
influences, we see that the need of interdisciplinarity
and interorganizational collaboration in initiating,
conducting, and implementing digital health artifacts
cause further cultural influence factors. Thus, other
concepts next to the Dimensions of National Culture
(DNC) used in this paper should be added to ensure a
comprehensive understanding of intercultural
awareness. With the Dimensions of Organizational
Culture (DOC), Hofstede also offers an
organizational view and describes similarities and
differences between organizations by their values,
rituals, heroes, symbols and practices (Hofstede
Insights, 2020). Interdisciplinarity or
interprofessional collaboration might be addressed by
the concept of Institutional Logics (IL) that can be
used to describe the pluralism of values, logics and
behavior from medical, business, legal or
technological standpoints (Berente et al., 2019;
Hansen and Baroody, 2020; Thornton et al., 2012).
We therefor want to motivate both research and
practice of DHI to use our indications of international
cultural influence factors under consideration of these
overlaying concepts. Figure 1 illustrates the
interconnection of cultural perspectives by nations
(DNC), organizations (DOC) as well as disciplines
(IL) and highlights the “heart” of international
cultural awareness in relation to other cultural
influences. We suggest, that discussions about
culture-related phenomena in the digital health
domain should seek to clarify the spot within this
heart for each phenomenon as influences of DNC,
DOC and IL may occur simultaneously and
interdependently, but rarely equilibrated.
Figure 1: Overlaying concepts for intercultural awareness.
6 CONCLUSION
In our expert study, we discussed the influence of
Hofstede’s dimensions of national culture on DHI and
a DHI capability. Our findings provide indications on
how practice and research should be aware of each
dimension to promote DHI processes or DHI
capability. Due to our findings, Uncertainty
Avoidance seems to influence DHI projects
negatively while Indulgence have been interpreted as
a positive influence factor. Power Distance and
Individualism might influence DHI differently
depending on the development stage of a DHI. Long-
term Orientation was assessed as generally
supportive while rapidly changing circumstances
challenge this characteristic. Even though
Masculinity correlates negatively with the DH Index
of a previous Bertelsmann study, our findings could
not clarify this numeric indication conclusively.
International collaborations or DHI for multinational
usage contexts should primarily benefit of our
contribution under consideration its limitations.
ACKNOWLEDGEMENTS
This work is part of the EFRE-funded project
“Häusliche Gesundheitsstation”. We especially like
to thank our project partners, supporters and study
participants to ensure the presented research.
Scale-IT-up 2022 - Workshop on Scaling-Up Health-IT
810

REFERENCES
Arthur, W. B., 2021. Foundations of complexity
economics. Nat. Rev. Phys. 3, 136–145.
https://doi.org/10.1038/s42254-020-00273-3
Berente, N., Lyytinen, K., Yoo, Y., Maurer, C., 2019.
Institutional logics and pluralistic responses to
enterprise system implementation: a qualitative meta-
analysis. MIS Q. 43, 873–902. https://doi.org/
10.25300/MISQ/2019/14214
Braithwaite, J., Tran, Y., Ellis, L.A., Westbrook, J., 2020.
Inside the black box of comparative national healthcare
performance in 35 OECD countries: Issues of culture,
systems performance and sustainability. PLOS ONE
15, e0239776. https://doi.org/10.1371/journal.pone.02
39776
European Commision, V., 2020. eHealth: Digital Health
and Care [WWW Document]. Public Health - Eur.
Comm. URL https://ec.europa.eu/health/ehealth/
home_en (accessed 11.9.21).
Gallego-Álvarez, I., Pucheta-Martínez, M.C., 2021.
Hofstede’s cultural dimensions and R&D intensity as
an innovation strategy: a view from different
institutional contexts. Eurasian Bus. Rev. 11, 191–220.
https://doi.org/10.1007/s40821-020-00168-4
Gaspay, A., Dardan, S., Legorreta, L., 2009. “Software of
the Mind”-A Review of Applications of Hofstede’s
Theory to IT Research. J. Inf. Technol. Theory Appl.
JITTA 9, 3.
Gaspay, A., Dardan, S., Legorreta, L., 2008. “Software of
the Mind” - A Review of Applications of Hofstede’s
Theory on IT Research. J. Inf. Technol. Theory Appl.
9, 1–37.
Halkos, G.E., Tzeremes, N.G., 2013. Modelling the effect
of national culture on countries’ innovation
performances: A conditional full frontier approach. Int.
Rev. Appl. Econ. 27, 656–678.
Hall, E.T., 1976. Beyond Culture. Anchor, Garden City,
CA.
Hansen, S., Baroody, A.J., 2020. Electronic Health Records
and the Logics of Care: Complementarity and Conflict
in the U.S. Healthcare System. Inf. Syst. Res. 31, 57–
75. https://doi.org/10.1287/isre.2019.0875
Hofstede, G., 2011. Dimensionalizing Cultures: The
Hofstede Model in Context. Online Read. Psychol.
Cult. 2. https://doi.org/10.9707/2307-0919.1014
Hofstede, G.H., Hofstede, G.J., Minkov, M., 2010. Cultures
and organizations: software of the mind: intercultural
cooperation and its importance for survival, 3rd ed. ed.
McGraw-Hill, New York.
Hofstede Insights, 2020. Whitepaper: Organisational
Culture: What You Need to Know.
Hoque, Md.R., Bao, Y., 2015. Cultural Influence on
Adoption and Use of e-Health: Evidence in
Bangladesh. Telemed. E-Health 21, 845–851.
https://doi.org/10.1089/tmj.2014.0128
Kowatsch, T., Otto, L., Harperink, S., Cotti, A., Schlieter,
H., 2019. A design and evaluation framework for digital
health interventions. It - Inf. Technol. 61, 253–263.
https://doi.org/10.1515/itit-2019-0019
Leidner, D.E., Kayworth, T., 2006. A Review of Culture in
Information Systems Research: Toward a Theory of
Information Technology Culture Conflict. MIS Q. 30,
357–399.
Moonen, P., 2017. The impact of culture on the innovative
strength of nations: A comprehensive review of the
theories of Hofstede, Schwartz, Boisot and Cameron
and Quinn. J. Organ. Change Manag. 30, 1149–1183.
https://doi.org/10.1108/JOCM-08-2017-0311
Nwabueze, S.N., Meso, P.N., Mbarika, V.W., Kifle, M.,
Okoli, C., Chustz, M., 2009. The Effects of Culture of
Adoption of Telemedicine in Medically Underserved
Communities, in: 2009 42nd Hawaii International
Conference on System Sciences. Presented at the 2009
42nd Hawaii International Conference on System
Sciences, pp. 1–10. https://doi.org/10.1109/
HICSS.2009.430
Prim, A.L., Filho, L.S., Zamur, G.A.C., Di Serio, L.C.,
2017. The relationship between national culture
dimensions and degree of innovation. Int. J. Innov.
Manag. 21, 1–22. http://dx.doi.org/10.1142/S1363919
61730001X
Smith, P., Trompenaars, F., Dugan, S., 1995. The Rotter
Locus of Control Scale in 43 Countries: A Test of
Cultural Relativity. Int. J. Psychol. 30, 377–400.
Srite, M., Karahanna, E., 2006. The Role of Espoused
National Cultural Values in Technology Acceptance.
MIS Q. 30, 679–704. https://doi.org/10.2307/25148745
Straub, D., Loch, K., Evaristo, R., Karahanna, E., Srite, M.,
2002. Toward a Theory-Based Measurement of
Culture. J. Glob. Inf. Manag. JGIM 10, 13–23.
https://doi.org/10.4018/jgim.2002010102
Thatcher, J.B., Srite, M., Stepina, L.P., Liu, Y., 2003.
Culture Overload and Personal Innovativeness with
Information Technology: Extending the Nomological
Net. J. Comput. Inf. Syst. 44, 74–81.
Thiel, R., Deimel, L., Schmidtmann, D., Piesche, K.,
Hüsing, T., Rennoch, J., Stroetmann, V., Stroetmann,
K., 2019. SmartHealthSystems: international
comparison of digital strategies. Gütersl. Bertelsmann-
Stift.
Thornton, P.H., Ocasio, W., Lounsbury, M., 2012. The
institutional logics perspective: A new approach to
culture, structure, and process. Oxford University Press
on Demand.
Yaveroglu, I.S., Donthu, N., 2002. Cultural Influences on
the Diffusion of New Products. J. Int. Consum. Mark.
14, 49–63.
Yusif, S., Hafeez-Baig, A., Soar, J., 2017. e-Health
readiness assessment factors and measuring tools: A
systematic review. Int. J. Med. Inf. 107, 56–64.
https://doi.org/10.1016/j.ijmedinf.2017.08.006
Be Aware! Indications for Intercultural Awareness for Digital Health Innovations and Innovation Capability
811
