Simulations of a Computational Model for a Virtual Medical Assistant
Aryana Collins Jackson
1 a
, Marl
`
ene Gilles
1 b
, Eimear Wall
2
, Elisabetta Bevacqua
1 c
,
Pierre De Loor
1
and Ronan Querrec
1
1
ENIB, Lab-STICC UMR 6285 CNRS, Brest, France
2
Health Service Executive, Ireland
Keywords:
Intelligent Agents, Embodied Conversational Agents, Human-computer Interaction, Situational Leadership,
Medicine, Simulation.
Abstract:
We propose a virtual medical assistant to guide both novice and expert caregivers through a procedure with-
out the direct help of medical professionals. Our medical assistant uses situational leadership to handle all
interaction with a caregiver, which works by identifying the readiness level of the caregiver in order to match
them with an appropriate style of communication. The agent system (1) obtains caregiver behavior during the
procedure, (2) calculates a readiness level of the caregiver using that behavior, and (3) generates appropriate
agent behavior to progress the procedure and maintain a positive interaction with the caregiver.
1 INTRODUCTION
Due to advancements in virtual agents and
telemedicine, caregiving in various capacities
can now be done at a distance. For example, virtual
agents can perform health assessments (Montenegro
et al., 2019) and act as liaisons with medical staff
(Bickmore et al., 2015). In these examples, the agent
interacts directly with the patient. However, there are
cases in which an agent should interact only with a
caregiver. When a medical procedure is necessary
and there are no trained medical staff nearby, the
individual present must assume a caregiving role, and
they will need guidance on preserving the patient’s
health. During these situations, a permanent virtual
medical assistant could be useful (Nakhal, 2017).
The assistant will communicate with the caregiver
and will also communicate to a team of medical ex-
perts standing by on a different site monitoring the
procedure. Because of the possible latency and dis-
ruptions in communication between the remote site
and the site where the experts are, the virtual assistant
must be capable of guiding the caregivers through the
entire procedure without relying on the help of the
medical experts.
A huge part of organizing a successful procedure
is maintaining a positive interaction with the caregiver
a
https://orcid.org/0000-0002-4385-5258
b
https://orcid.org/0000-0003-1806-1672
c
https://orcid.org/0000-0002-7117-3748
while maintaining the health of the patient (Hjort-
dahl et al., 2009; Henrickson et al., 2013; Yule et al.,
2008; Flin et al., 2010). Both the caregiver and the
agent must work towards a common goal: the com-
pleted procedure that preserves the health of the pa-
tient. To foster this positive working alliance be-
tween agent and caregiver, situational leadership is
employed (Hersey et al., 1988). In situational leader-
ship, a leader adapts their behavior to the follower ac-
cording to their experience level and expertise. Situa-
tional leadership involves four readiness levels which
directly correspond to four leadership styles. The
readiness levels involve varying degrees of ability,
which refers to a person’s competence when complet-
ing tasks, and willingness, which refers to their con-
fidence and interest in completing those tasks. In this
scenario, the virtual agent assumes the role of leader,
and the caregiver assumes the role of follower. Situa-
tional leadership is covered in more depth in section 2.
Previously when situational leadership has been
studied, it has been implemented (Sims et al., 2009;
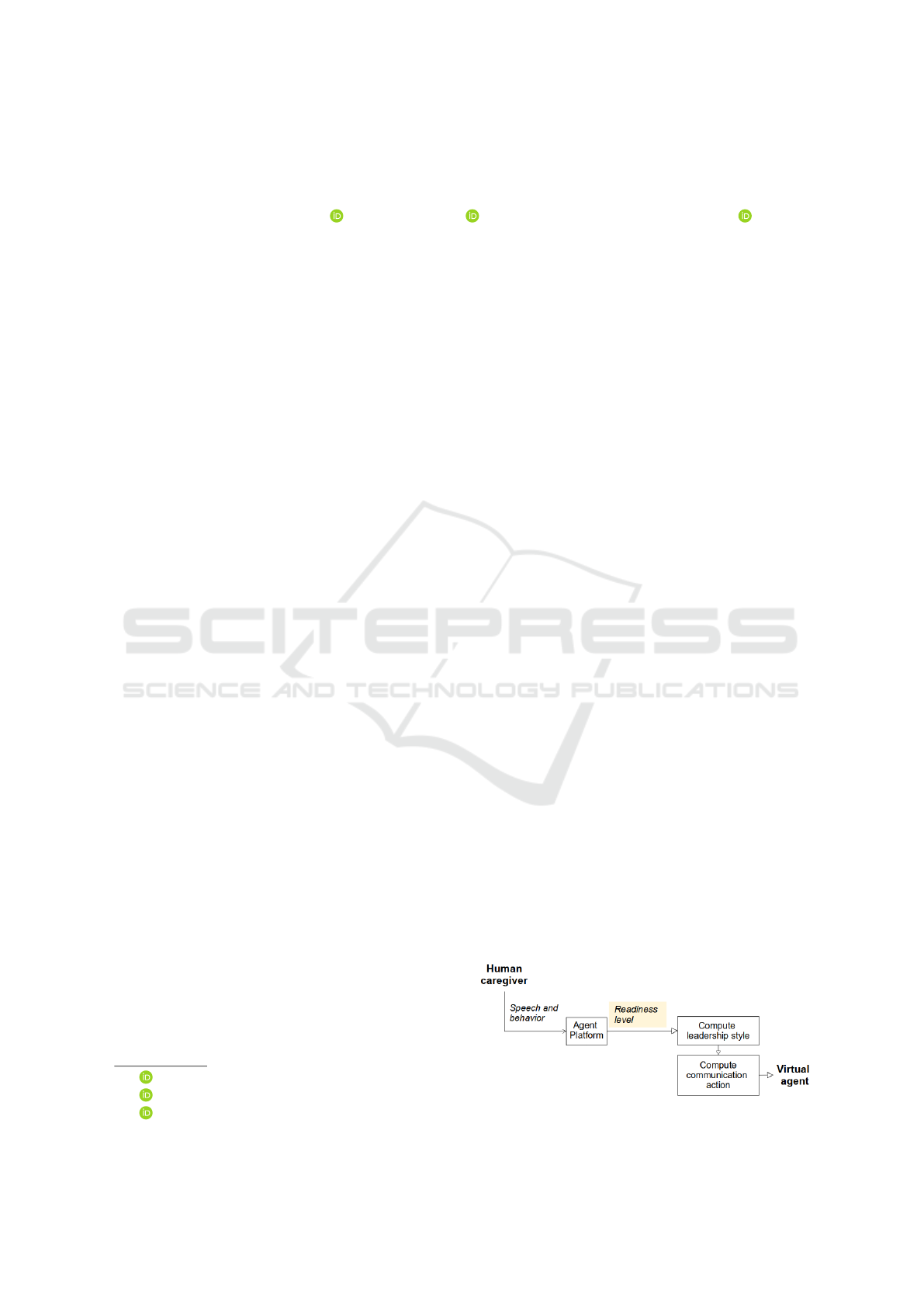
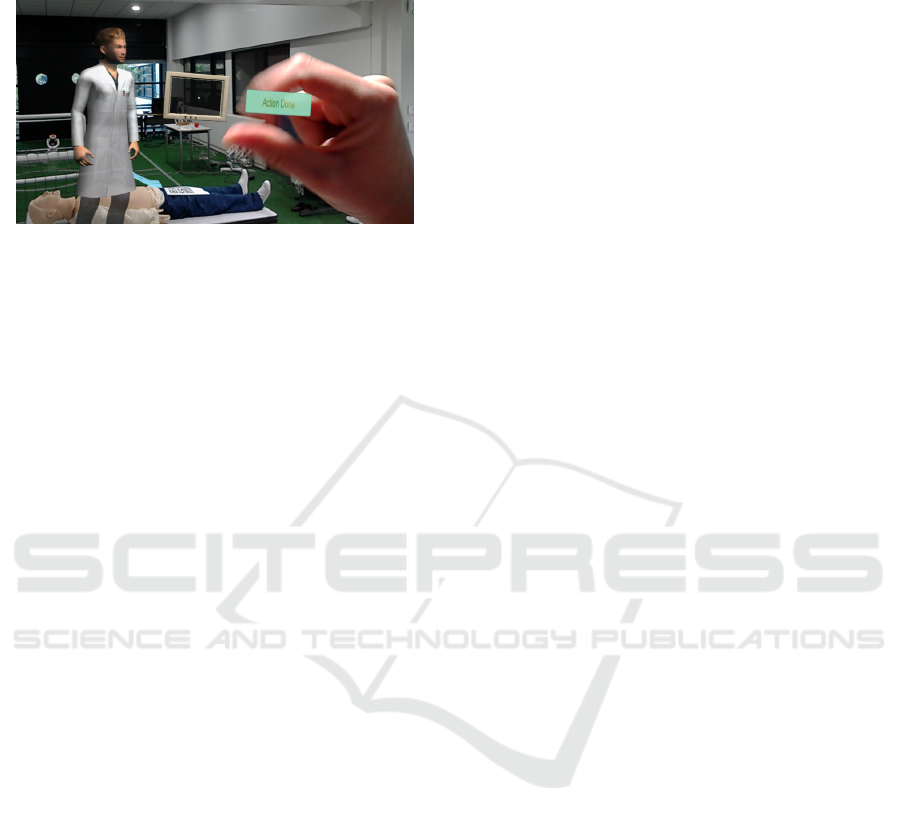
Figure 1: A basic representation of the agent framework.
94
Jackson, A., Gilles, M., Wall, E., Bevacqua, E., De Loor, P. and Querrec, R.
Simulations of a Computational Model for a Virtual Medical Assistant.
DOI: 10.5220/0010910700003116
In Proceedings of the 14th International Conference on Agents and Artificial Intelligence (ICAART 2022) - Volume 1, pages 94-105
ISBN: 978-989-758-547-0; ISSN: 2184-433X
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

Hersey et al., 1988; Lourdeaux et al., 2019) or simu-
lated for intended use in human-human relationships
(Bosse et al., 2017; Bernard, 2020). Virtual leaders
have used different methods of guiding humans and of
choosing behavior that is personalized to the individ-
ual humans. However, our work is the first to present
both a computational model of situational leadership
and an agent framework in which a virtual agent leads
humans (see Figure 1 for a basic representation of the
agent framework and Figure 6 for a detailed view).
We contribute an implementation of situational lead-
ership in which we (1) quantify the factors that deter-
mine readiness level, (2) create an algorithm for cal-
culating readiness level based on these criteria, and
(3) create a virtual agent system that uses readiness
level and human behavior to create personalized be-
havior.
While our work is conducted with the context of a
medical procedure in mind, the model itself is flexible
enough to be applicable to any situation in which a
human being must be led through a series of steps by
a virtual assistant.
In this paper, we detail what situational leadership
is and how it works, we discuss the current state of
the art regarding virtual leaders, we detail our com-
putational model of situational leadership, we explain
how our model is implemented using Mascaret, and
we discuss our conclusions and future work.
2 SITUATIONAL LEADERSHIP
As discussed in the introduction, situational leader-
ship encompasses four follower readiness levels and
four leadership styles. The four readiness levels (de-
noted with an R and a number) are listed below
(Hersey et al., 1988):
1. R1: Low ability, low willingness;
2. R2: Low to some ability, high willingness;
3. R3: High ability, variable willingness;
4. R4: High ability, high willingness.
Readiness levels R1 and R2 need the leader’s help
while readiness levels R3 and R4 should be able to
complete tasks without the leader’s help.
When a leader employs situational leadership,
they perform both task and relationship behavior to
guide the follower. Task behavior corresponds to a
follower’s competence (Bedford and Gehlert, 2013).
Relationship behavior refers to how the leader fosters
and maintains a positive working alliance with the fol-
lower and corresponds to a follower’s willingness, or
confidence (Bedford and Gehlert, 2013). The lead-
ership styles that correspond to these readiness levels
are (Hersey et al., 1988):
1. Directing: high task, low relationship behavior;
2. Coaching: high task, high relationship behavior;
3. Supporting: low task, high relationship behavior;
4. Delegating: low task, low relationship behavior.
Note that low relationship behavior is required for
followers with low ability and low willingness be-
cause the person may not be interested in being en-
couraged. For followers with high ability and low to
some willingness, the agent motivates the person be-
cause they have the skills necessary to complete the
procedure successfully.
Follower behavior that can indicate a particular
readiness level includes both prior experience and
knowledge and non-anatomical behavior such as the
number of questions asked, the amount of hesitation
after receiving tasks, etc. (Collins Jackson et al.,
2019; Bosse et al., 2017; Hersey et al., 1988):
Situational leadership is an effective method of
managing followers because it accounts for follow-
ers with both high and low ability and willingness.
This model has been proven effective in an educa-
tional environment in which medical instructors im-
plemented leadership styles in their classes and with
individual students (Sims et al., 2009), work environ-
ments in which managers adopted leadership styles
with their direct reports (Hersey et al., 1988), and in
a clinical medical supervision context (Bedford and
Gehlert, 2013). Situational leadership has also been
implemented in a virtual environment to help train
medical staff (Lourdeaux et al., 2019).
There is very limited work on computational mod-
els using situational leadership, and existing work in-
volves human-human interaction only (Bosse et al.,
2017; Bernard, 2020). Rarely are agents in positions
of leadership in human-agent interaction. Our work
models the work on situational leadership and also
provides a new method in which agents and humans
can interact by allowing an agent to lead a human.
Our model permits an agent to maintain a positive in-
teraction with a follower and interact with the human
in a way that is most beneficial for them in addition to
maintaining the health of the patient.
In the following section, we discuss previous work
on virtual agent leaders.
3 VIRTUAL LEADERS
This work involves a virtual agent acting as a med-
ical assistant who leads a caregiver through a medi-
cal procedure. Within the medical domain, there has
Simulations of a Computational Model for a Virtual Medical Assistant
95

been a lot of work regarding human-human relation-
ships in the emergency room. The person leading a
medical procedure holds an important role in that they
manage both the procedure tasks, the health of the pa-
tient, and the interaction with the caregiver(s). Thus
having the trust of the caregivers and being compe-
tent at their work are two of the most important qual-
ities a leader can have (Hjortdahl et al., 2009). Addi-
tional qualities that a medical leader should embody
include communication, negotiation, autonomy, cre-
ativity, and appreciation of the caregivers (Araszewski
et al., 2014). Many of these qualities are therefore in-
cluded in medical professional behavior taxonomies
(Henrickson et al., 2013; Yule et al., 2008; Flin et al.,
2010).
In terms of virtual agents in medicine, there are a
variety of examples of virtual agents created for use
specifically in medical situations: agents which act
as liaisons between patients and physicians using pre-
scripted speech (Bickmore et al., 2015), agents which
are meant to connect emotionally with patients for
mental health benefits (Yang and Fu, 2016), agents
which act as companions for the elderly (Montenegro
et al., 2019), and agents which conduct psychiatric in-
terviews (Philip et al., 2020). In each of these exam-
ples, user engagement with the agent was dependent
on whether they trusted the agent.
The concept of developing trust is inherent in all
types of human-computer interactions, regardless of
domain, as it is a prerequisite to a positive interaction
(Hoegen et al., 2019; Kulms and Kopp, 2016; Lee
et al., 2021). Additionally, trust leads to greater ef-
ficiency when the human is completing tasks (Kulms
and Kopp, 2016). Situational leadership was devel-
oped knowing that followers’ trust of their leader is
hugely important to successful interactions, and that
trust can be built and maintained when leaders interact
in an appropriate manner to followers (Hersey et al.,
1988). Thus employing situational leadership itself is
a method of building and maintaining trust between a
human and an agent.
Because our work involves an agent leading a hu-
man, we examined previous work in which agents
exist in pedagogical scenarios. We again found that
trust was important to student-tutor relationships and
was a product of a supporting environment (Castel-
lano et al., 2013; Saerbeck et al., 2010). These rela-
tionships are most successful when the agent adapts
to the learner by responding based on his or her previ-
ous experience and level of knowledge (Pecune et al.,
2010; Taoum et al., 2018; Cisneros et al., 2019; Quer-
rec et al., 2018).
As mentioned in the introduction, few computa-
tional models on situational leadership have been de-
veloped (Bosse et al., 2017; Bernard, 2020). While
these models have involved human-human interaction
only, they have provided a foundation for computing
readiness level and therefore determining leadership
style from various behavioral parameters. One model
is based entirely on follower behavior and allows the
leader to adapt their leadership style by monitoring
a follower’s advancement through the different readi-
ness levels (Bosse et al., 2017). This work in particu-
lar formed the backbone of our own research.
In the following section, we outline our own com-
putational model of situational leadership when a vir-
tual agent is a medical leader.
4 A COMPUTATIONAL MODEL
OF SITUATIONAL
LEADERSHIP
Readiness level is determined by examining follower
behavior. Other research has analyzed behavior such
as facial actions and head movements (Dermouche
and Pelachaud, 2019). However, we do not uti-
lize a human activity monitor in this project. While
these kinds of non-verbal behaviors are certainly use-
ful, we chose to prioritize the caregiver’s ability to
move around the environment without worrying about
whether their faces were reliably detected. Instead,
we focus on human behavior that can be monitored
and input from a keyboard.
In this section, we discuss the parameters used in
our model, we detail the follower behavior that are
used, we discuss why we chose certain parameter val-
ues, we thoroughly explain how the model works, and
we explain how our model can be used to adhere to
guidelines set by the existing work on situational lead-
ership.
4.1 Model Parameters
Our model uses several parameters and various care-
giver behaviors to determine readiness level. From
now on, we refer to individual behaviors as behavior
criteria or simply criteria.
Two of the parameters needed in this algorithm,
persistence and valence, are adapted from an exist-
ing model (Bosse et al., 2017), but the others are
our own contributions. The parameters explained be-
low are used in equations 1 and 2 (detailed in sec-
tion 4.4) to calculate a performance value which de-
scribes how high the follower’s performance is in re-
gards to each criterion. These values change depend-
ing on the procedure. Before explaining how that cal-
ICAART 2022 - 14th International Conference on Agents and Artificial Intelligence
96

Table 1: The behavior criteria used for computing readiness level and each of their parameters. The persistence values change
depending on whether the follower has low or high ability and willingness.
Criterion Name Domain Persistence:
high
Persistence:
low
Weight Performance
threshold
1 Error: action in task ability 0.7 0.85 0.05 0
2 Error: action outside task ability 0.1 0.85 0.25 1
3 Wrong resource chosen ability 0.7 0.85 0.15 0.75
4 No resource chosen ability 0.2 0.85 0.25 1
5 Action duration too short ability 0.1 0.85 0.06 0
6 Action duration too long ability 0.1 0.85 0.07 1
7 Question for help ability 0.4 0.85 0.17 1
8 Hesitation willingness 0.9 0.9 0.5 0.5
9 Question for reassurance willingness 0.9 0.9 0.5 0
culation works, we explain what each parameter is:
Extent refers to the extent to which the follower
exhibits the criterion and is described by either 0 or 1
where 0 indicates that the follower does not embody
that criterion at all, and 1 indicates that the follower
embodies that criterion to the fullest extent possible.
Domain refers to whether the criterion is an indi-
cator of ability or willingness; criteria can either exist
in the ability domain or the willingness domain.
Persistence describes how much the behavior dur-
ing a previous task influences the current readiness
level with a float on the interval [0, 1]. A value of 0
indicates low persistence while a value of 1 indicates
high persistence. The lower the persistence value, the
faster the performance value will rise or fall when the
extent to which the follower exhibits that criterion is
high or low respectively (Bosse et al., 2017).
Weight refers to the importance of the criterion
within the ability and willingness domains when de-
termining readiness level and is described by a float
on the interval [0, 1].
Performance threshold refers to the lowest perfor-
mance value possible of that criterion before the fol-
lower could be considered to have low ability or low
willingness.
4.2 Follower Behavior Criteria
In previous research, the extent to which a follower
exhibits thirty-three different behaviors determines
readiness level (Bosse et al., 2017). That model is
based on an interaction between a student and a su-
pervisor, and thus many of these behaviors were either
irrelevant to a medical scenario (such as feeling over-
obligated and lacking self-esteem) or were impossible
to compute within a virtual environment (such as de-
fensive behavior and discomfort in body language).
Additionally, these thirty-three behaviors are catego-
rized by readiness level, indicating that each behavior
is indicative of only one readiness level. While our
work is based on this research, in order to adapt it to
the context of a medical procedure led by a virtual
agent, some changes had to be made.
Using that existing list of behaviors (Bosse et al.,
2017), we created our own list of behavior criteria
(see Table 1). Instead of grouping them by readiness
level, we group them by whether they are indicators of
ability or willingness. Because all four readiness lev-
els can be described as having ability and willingness
that is high, low, or somewhere in between, follow-
ers of any style can embody each of the behaviors to
varying extents. The list of criteria are explained be-
low. Note that in the procedure, there are both tasks
and actions. A task is a complete step, while an action
is a sub-step of a task. Thus each task may involve
multiple actions. A resource is a tool that can be used
to perform an action. Each action has an appropriate
duration that it is expected to take. All of this infor-
mation exists within Mascaret, our agent framework,
which is explained further in section 6.
1. Error: action in task: The follower has chosen to
do an action out of order;
2. Error: action outside task: The follower has cho-
sen to do an action that does not exist in the cur-
rent task;
3. Wrong resource chosen: The follower has taken
the wrong resource for the action;
4. No resource chosen: The follower has neglected
to take a resource when one is required or tries to
take a resource when none is required;
5. Action duration too short: The action duration is
less than 0.9 times the expected action duration
(as devised by our medical professional);
6. Action duration too long: The action duration is
more than 1.1 times the expected action duration
(as devised by our medical professional);
7. Question for help: The follower has asked a ques-
tion because they do not know how to proceed;
8. Hesitation: The follower has hesitated for more
than five seconds before beginning an action;
Simulations of a Computational Model for a Virtual Medical Assistant
97

9. Question for reassurance: Also referred to as a
clarifying question; the follower has asked a ques-
tion to ensure what they are doing is correct.
4.3 Expert-defined Parameter Values
The values for the parameters in Table 1 were devised
by consulting with the medical doctor on our team.
The procedure that these values were created for is the
diagnosis of abdominal pain, and with these values,
we assume that the case is not urgent.
Because our context is rather specific, it was im-
portant to create our model with the guidance of our
team’s medical professional. Therefore, all of these
values are very procedure specific. The values for per-
sistence, weight, and performance threshold would
change depending on the procedure.
For a non-urgent diagnosis of abdominal pain, the
most important ability criteria are Error: action out-
side task and No resource chosen because they indi-
cate that the follower does not understand the current
task and how to reach the end goal. Each are given
the highest weight of 0.25. If the follower is consid-
ered to be high-ability, these two errors change their
performance values considerably with low persistence
values of 0.1 and 0.2 respectively.
Question for help is the next most important cri-
terion in the ability domain because it indicates that
the follower does not know how to proceed without
the agent’s help. This criterion is given a moderate
persistence of 0.4 when the follower is considered to
have high-ability because while questions for help are
indicative of more novice behavior, the follower’s his-
tory should be more important than it is for Error:
action outside task and No resource chosen.
Unlike the previous three criteria, there is room for
human error in Wrong resource chosen where a fol-
lower may accidentally reach for the wrong resource,
hence the higher persistence value of 0.7.
Error: action in task, Action duration too short,
and Action duration too long have the lowest weights.
The most important thing is that the task has been
completed, and so errors out of order do not matter
so much as long as the task is being completed. Per-
sistence for this error is set quite high. Action com-
pletion duration times are not important unless there
is a life-threatening emergency. However, the persis-
tence is set low for the action duration errors as these
can co-occur with other criteria, such as Error: ac-
tion in/outside task and Question for help and there-
fore they should be taken quite seriously. Because of
their low weight, short or long action duration times
on their own do not generally affect the overall ability
performance unless they happen repeatedly through-
out the procedure.
Finally, Hesitation and Question for reassurance
are weighted equally in the willingness domain. Each
of these are equally indicative of a follower’s willing-
ness. Additionally, the persistence for both is set quite
high at 0.9 because a follower’s willingness should be
calculated from their history rather than from a single
task.
As shown in Table 1, there are two different val-
ues for persistence, one for followers are deemed to
have low ability or willingness and one for those who
are deemed to have high ability or willingness. These
values were devised in order to account for a novice
who does everything correctly versus an expert who
makes one or two mistakes. During a medical proce-
dure, even one small mistake can lead to serious con-
sequences. When a follower displays high-ability be-
havior, the mistakes they make should have more im-
pact on the performance value. The Persistence: high
values are used when a follower begins the proce-
dure with high ability or willingness. When the abil-
ity performance drops below the first ability threshold
of 0.8525, then the Persistence: low values are used
instead. Persistence: low values are also used for fol-
lowers who begin the procedure with low ability or
willingness.
Additionally, persistence changes based on the
difficulty of the current action so that a follower who
is only easily able to do easier actions and a follower
who is able to do harder actions are not considered to
be the same level. Each action in the procedure is as-
signed a value of 1 (most difficulty), 2 (medium diffi-
culty), and 3 (least difficulty). If the action is assigned
a 1, then the persistence value for that task decreases
by 0.05 to ensure that the persistence is never 1 or
0. If the action is assigned a 3, then the persistence
value for that task increases by 0.05. If the action is
assigned a 2, there is no change to persistence. This
ensures that more difficult tasks are weighted more
when the performance value is calculated.
4.4 The Model Explained
The first step to determining readiness level is to
calculate the performance value for each criterion.
The performance value is a float on the interval [0, 1]
where a value of 0 indicates low ability or willingness
and a value of 1 indicates high ability or willingness.
Equation 1 is used to calculate the performance
value v at time t for criterion c, where p represents the
persistence and e represents the extent (Bosse et al.,
2017).
v
c,t
= (p
c
∗ v
c,t−1
) + ((1 − p
c
) ∗ (1 −e
c,t
)) (1)
ICAART 2022 - 14th International Conference on Agents and Artificial Intelligence
98
Equation 1 requires the performance value at time
t − 1. At the very beginning of the procedure, default
performance values are used in place of v
c,t−1
. Val-
ues of 0 or 1 are established for each criterion which
correspond to the follower’s previous experience and
knowledge, called the follower profile. The follower
profile establishes which readiness level the individ-
ual has prior to beginning the procedure and is based
on previous procedures, external evaluations of the
follower, and self-evaluations. For a follower profile
indicating low or variable ability or willingness, the
default performance value is 0, and for a follower pro-
file indicating high ability or willingness, the default
performance value is 1.
For example, if a follower profile indicates that the
individual’s readiness level is style 3, then they have
high ability and variable willingness (see Figure 2).
The default performance values for all the criteria in
the ability domain are 1, and the default performance
values for the criteria in the willingness domain are 0.
Calculating the performance value v for Error: action
in task for a follower of style 3 who has made an error
at the very beginning of the procedure would look like
this: (0.1 ∗ 1)+ ((1 − 0.1) ∗ (1 − 1)) = 0.1.
The performance value v is then fed back into the
model in equation 1 the next time readiness level is
calculated.
The next step of determining readiness level is to
average all the performance values within each do-
main. Equation 2 is used where n refers to the num-
ber of criteria in the ability and willingness domains,
weight
c
refers to the weight that each criterion holds,
and v
c,t
refers to the performance value at time t of
each criterion as calculated by equation 1. Equation 2
results in two values representing the follower’s over-
all ability and willingness behavior O.
O
t
=
n
∑
c=1
weight
c
∗ v
c,t
(2)
There are two different thresholds each for deter-
mining whether a follower has low or high ability and
willingness. For the first, the performance thresholds
shown in Table 1 are used to determine whether a fol-
lower has high or low ability and willingness. When
using the performance thresholds in equation 1 for
both e
c
and v
c,t−1
, and then using the resulting v
c,t
value in equation 2, we achieve the overall ability per-
formance threshold of 0.8525 and the overall willing-
ness performance threshold of 0.625. If a follower has
an ability value below 0.8525, they have low ability,
and if that value is above or equal to 0.8525, they have
high ability. If a follower has a willingness value be-
low 0.625, they have low willingness, and if that value
is at or above 0.625, they have high willingness.
The second threshold is defined by ability and
willingness equal to or greater than 0.95. This value
was devised by examining example follower behavior
and determining which were able to self-lead without
the leader’s help. Followers with both an ability and
a willingness value equal to or greater than 0.95 are
considered to be in R4. See Figure 2 for a visualiza-
tion of the thresholds and readiness levels.
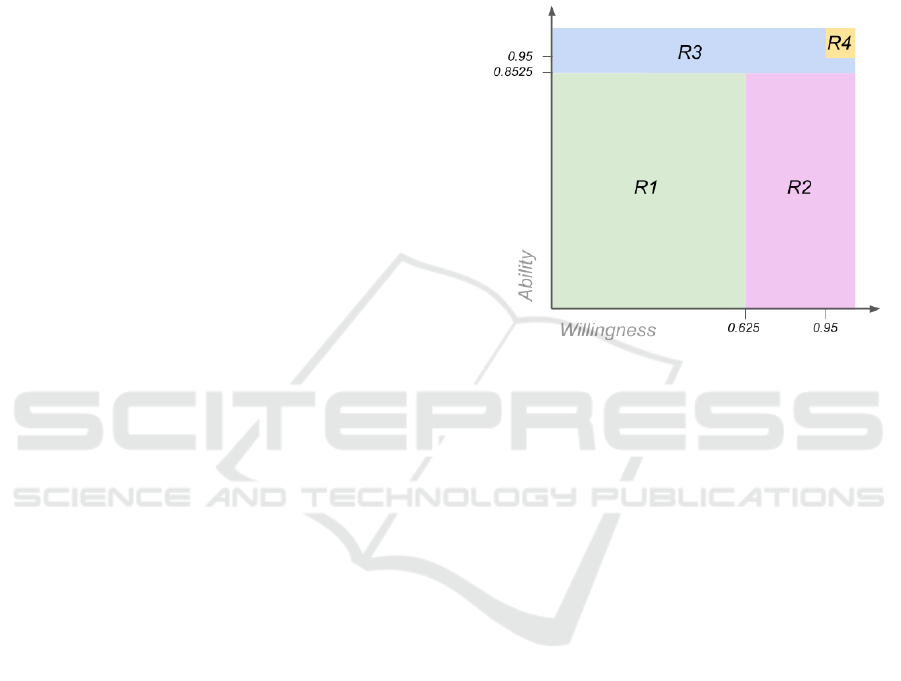
Figure 2: A visualization of the four readiness levels and
the performance values needed in order to move between
them.
As shown, each readiness level is color-coded
uniquely. A follower’s ability is contained on the ver-
tical axis while willingness is described on the hori-
zontal axis. Once the initial thresholds of 0.825 and
0.625 are reached for ability and willingness respec-
tively, a follower is considered to be R3. Because
R4 is designated for completely self-sufficient follow-
ers, the thresholds for R4 are higher. Ensuring that
movement between the readiness levels is linear is
discussed later in this section.
For examples of how this all works, refer to Fig-
ure 3. In this example procedure, Error: action out-
side task is examined. There are ten actions with the
following action difficulties: 3, 3, 3, 3, 2, 2, 1, 2, 1,
and 2. A follower with an existing readiness level of
R1 and a follower with an existing readiness level of
R4 perform the exact same steps; they each try to do
an action that is outside the scope of the task for ac-
tions 5, 7, and 9. As shown, the performance value
v dips for both the R1 and R4 follower, but the er-
rors have a greater effect on the R4 follower who is
supposed to be an expert.
Note that the extent values for each criterion re-
main the same until there is another opportunity to
change that value. For example, the extent value e
of Error: action outside task only changes when the
Simulations of a Computational Model for a Virtual Medical Assistant
99
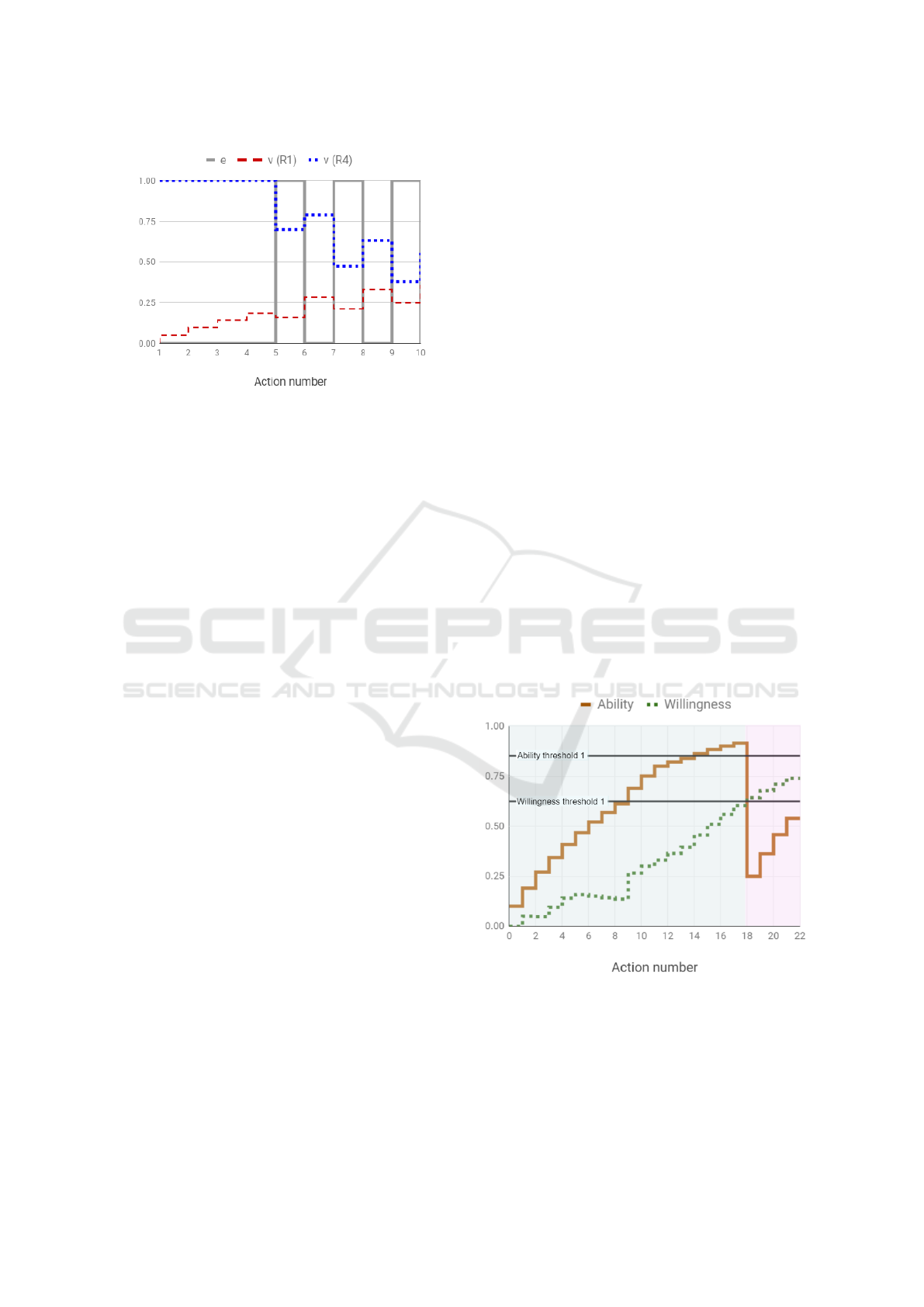
Figure 3: Two examples of the evolution of the performance
value v in a procedure in which an R1 and an R4 follower
perform the criterion Error: action outside task at actions
5, 7, and 9.
follower has the opportunity to make or not make an-
other error (i.e., when it is time for the caregiver to
begin a new action). The performance values v are
only calculated when e changes. The overall ability
and willingness values are updated when the individ-
ual v values change.
4.5 Adhering to Situational Leadership
Finally, there are two possible issues that should be
avoided when using this model: (1) the skipping
of readiness levels (followers that move directly be-
tween R1 and R3 as well as R2 and R4) and (2) fol-
lowers moving between levels too quickly (Hersey
et al., 1988; Bosse et al., 2017). To combat these
issues, we implement a method of artificially lower-
ing ability and lowering or raising willingness values
as needed, which is similar to dynamic range com-
pression (Kates, 2005). This allows for one domain’s
overall performance to wait while the other domain’s
performance catches up.
There are several of instances in which the abil-
ity or willingness value would need to be artificially
changed:
• An R1 follower whose ability rises faster than
willingness will need their ability value low-
ered when their willingness crosses the high-
willingness threshold to ensure they move from
R1 to R2 (see Figures 4 and 5c);
• An R3 follower whose ability drops below the
high-ability threshold but whose willingness is
still low will need their ability value lowered and
may need their willingness value raised to ensure
they move from R3 to R2 (see Figures 5j, 5k, 5m,
and 5o);
• An R2 follower whose willingness drops below
the high-willingness threshold but whose ability
is high will need their ability value lowered to en-
sure they move from R2 to R1;
• An R4 follower whose ability or willingness drops
below the R4 thresholds of 0.95 will need the
other domain’s value lowered to either 0.8525
(ability) or 0.625 (willingness) in order to ensure
that the follower moves from R4 to R3 and from
R3 to R2 smoothly (see Figure 5m.
Because our context is a medical procedure in
which a patient’s health is at risk, when in doubt, we
always assume that a follower’s ability is lower than
it might be (Hjortdahl et al., 2009). For this reason,
followers’ ability values are only artificially lowered.
As explained in section 6, the agent’s communication
content does not vary much between levels R1 and
R2 or R3 and R4, and so willingness values can be
lowered or raised when necessary.
As an example of how values might be artificially
changed, examine an R1 follower whose ability and
willingness increase at different rates. Before exam-
ining what this looks like, we can refer to Figure 2
and see that this would mean that the follower would
move directly from R1 to R3. Because a follower can
only progress from one readiness level to the next, we
artificially lower the overall ability value in order to
wait for the willingness performance to catch up. See
Figure 4 for a demonstration of how this works.
Figure 4: An example of how ability values are artificially
lowered in order to ensure the follower progresses from one
level to the next. Green represents readiness level R1 while
pink represents readiness level R2.
In Figure 4, the follower passes the threshold for
high ability at action 14. At this point, however,
the willingness value is still low, so the follower is
ICAART 2022 - 14th International Conference on Agents and Artificial Intelligence
100

still considered to be R1. The procedure continues,
and at action 18, the follower’s willingness passes the
threshold for high willingness. Since their willingness
performance has increased above the threshold, the
follower can now be considered to be in R2. Readi-
ness level R2 is defined by low to some ability and
high willingness, and so the follower’s ability value is
artificially decreased to 0.25, a value we chose in or-
der to allow the system to “remember” the follower’s
performance history somewhat. In Figure 4, we can
see that for actions 18-22, the follower is clearly in
R2. In this way, the follower can progress until their
ability once again passes the ability threshold. If, at
that point, willingness has remained high, then the
follower will progress to R3.
By manually lowering the ability and willingness
values as needed, the system acts similarly to dynamic
range compression in which signals are limited once
they reach a certain threshold (Kates, 2005). Unlike
compression, we lower the values in order to allow the
follower to progress themselves through to the next
readiness level. This is how we ensure that not only
do followers progress from one readiness level to the
next without skipping levels, but we also ensure that a
follower does not move between readiness levels too
quickly.
In the following section, we demonstrate how
readiness level evolves in a variety of scenarios.
5 SIMULATIONS OF FOLLOWER
PROGRESSION
In order to visualize how readiness level might
change during a medical procedure and evaluate those
changes to ensure they are indicative of the correct
readiness level in practicality, we establish four start-
ing states (R1, R2, R3, and R4 followers) and four
possible progressions: (1) ability increases or de-
creases, willingness stays the same; (2) ability stays
the same, willingness increases or decreases; (3) abil-
ity increases or decreases, willingness increases or de-
creases; and (4) ability remains the same, willingness
remains the same. This results in sixteen different sce-
narios.
As discussed in section 4.3, the criteria in each
scenario are created with help from the medical pro-
fessional on our team and are based on real-world
errors that followers in each readiness level would
make. Therefore, creating these scenarios is also a
method of testing our model and the values for the
parameters described in section 4.3. The simulations
included in this section are not exhaustive; many more
were tested in order to ensure that the values for the
parameters in our model returned accurate readiness
levels.
The scenarios use a sample of a procedure which
comprises a total of 22 actions. The first 9 actions
have the least difficulty, actions 10-12 have the most
difficulty, actions 13-14 have the least difficulty, and
actions 15-22 have medium difficulty.
Figures 5a-5p display the 16 scenarios and are
color-coded according to Figure 2: green represents
R1, pink represents R2, blue represents R3, and yel-
low represents R4. Note that unless a follower is
making every possible error constantly throughout the
procedure, which often isn’t possible, ability and will-
ingness will increase from 0.
6 AGENT FRAMEWORK
Figure 6 describes the flow of information and how
interaction is possible in our agent framework based
on Mascaret. The agent platform contains the means
to calculate readiness level and the information re-
garding the nominal procedure. The nominal pro-
cedure contains all information regarding resources,
roles, procedure steps, and also allows for changes to
be made to the procedure.
When a caregiver makes an error in Table 1, a cri-
teria event is created which describes the error. The
agent platform calculates readiness level from the hu-
man caregiver’s speech and behavior, and then readi-
ness level and criteria events stemming from care-
giver behavior are created and work together to cre-
ate communication intentions. The modality for agent
communication is both verbal and non-verbal behav-
ior, so communication intentions (verbal behavior)
are paired with appropriate non-verbal behavior in the
behavior planner (Collins Jackson et al., 2020).
The Mascaret framework permits the modeling of
semantic, structural, geometric, and topological prop-
erties of the entities in the virtual environment and
their behaviors. Mascaret also defines the notion of
a virtual agent by their behaviors, their communica-
tions, and their organisation. Essentially, it is a frame-
work in which an embodied virtual human can inter-
act with a user.
In Mascaret, human activities can be described in
the virtual environment by using predefined collabo-
rative scenarios (called procedures) which represent
plans of actions for agents or instructions provided
to users for assisting them. With Mascaret, a whole
medical procedure with roles, resources, and trajecto-
ries can be formalized and virtually executed to assist
a caregiver to go through this same procedure in the
real world.
Simulations of a Computational Model for a Virtual Medical Assistant
101

(a) R1: Ability rises, will-
ingness remains low.
(b) R1: Willingness rises
above the threshold.
(c) R1: Ability and willing-
ness rise above the thresh-
olds.
(d) R1: Ability and willing-
ness remain low.
(e) R2: Ability rises above
the threshold, willingness
remains high.
(f) R2: Ability remains low,
willingness drops below the
threshold.
(g) R2: ability rises above
the threshold, willingness
drops below the threshold.
(h) R2: Ability remains
low, willingness remains
high.
(i) R3: Ability remains
high, willingness rises
above the threshold.
(j) R3: Ability drops be-
low the threshold, willing-
ness remains low (but is ar-
tificially raised).
(k) R3: Ability drops be-
low the threshold, willing-
ness rises above the thresh-
old.
(l) R3: Ability remains
high, willingness remains
low.
(m) R4: Ability drops be-
low the threshold, willing-
ness remains high (but is ar-
tificially lowered).
(n) R4: Ability remains
high, willingness drops be-
low the threshold.
(o) R4: Ability and willing-
ness drop below the thresh-
olds.
(p) R4: Ability and willing-
ness remain high.
Figure 5: Sixteen simulations demonstrate how readiness level evolves when ability and willingness increases, decreases, or
remains the same, four starting in each readiness level. The solid brown line indicates the overall ability performance, and the
dotted green line indicates the overall willingness performance. Green shading refers to R1, pink shading refers to R2, blue
shading refers to R3, and yellow shading refers to R4.
To allow Mascaret to interact with the user in
a natural way, we introduce an embodied conversa-
tional agent (ECA) based on the SAIBA framework
(Vilhj
´
almsson et al., 2007) and which has an intent
planner which generates the communicative inten-
tions of the agent, a behavior planner which trans-
lates communicative intentions into verbal and non-
verbal signals, and a behavior realizer which trans-
ICAART 2022 - 14th International Conference on Agents and Artificial Intelligence
102
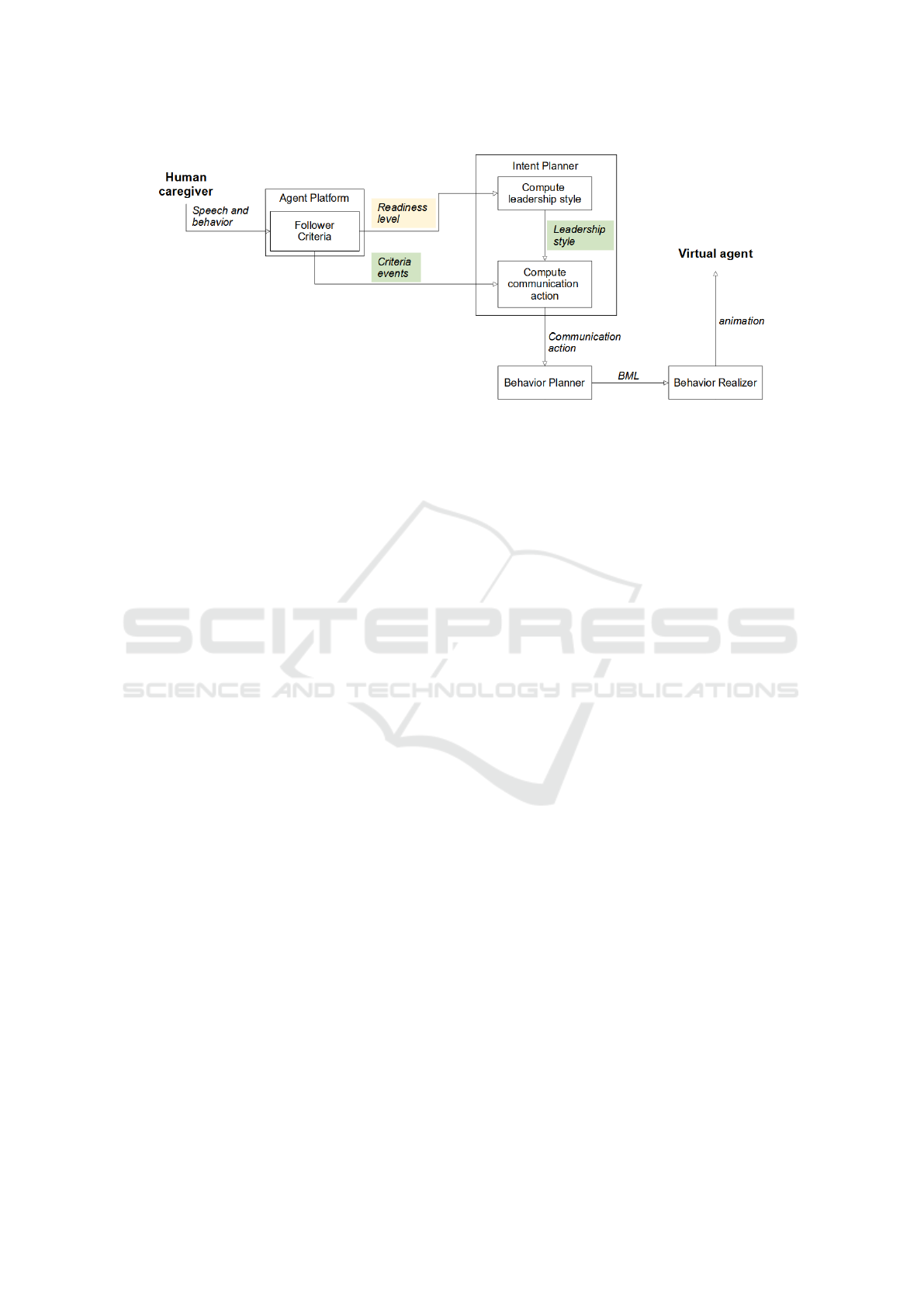
Figure 6: The general flow of information within our agent framework. Readiness level (highlighted in yellow) informs
leadership style. Criteria event and leadership style (highlighted in green) inform the communication actions.
forms these signals in animation.
In Mascaret, we introduce the concept of follower
criteria (see Table 1). After each action is performed
by the follower, each behavior criterion is evaluated
to see if it has been triggered (e.g., if the person has
tried to do an action that is outside the task, if they
have asked a question because they are stuck, etc.).
According to the triggered criteria, the readiness level
is computed (as explained in section 4).
The readiness level is used to compute the leader-
ship style which is then stored in the intent planner
(Collins Jackson et al., 2021)). The intent planner
then generates a communicative intention each time
a new action in the procedure must be done or when
a follower criterion that needs attention has been trig-
gered (for example, the virtual agent must inform the
caregiver if they have made a mistake, must answer a
question that the caregiver has asked, etc.).
To determine the ECA’s communicative intention,
we implement a set of rules which dictates how and
what the agent will communicate according to its
leadership style to be used in conjunction with lin-
guistic rules specified in previous work (Collins Jack-
son et al., 2022):
Directing and coaching leadership (correspond-
ing to readiness levels 1 and 2):
• Agent communicates every action to do;
• Agent communicates every time there is a criteria
event.
Supporting leadership (corresponding to readi-
ness level 3):
• Agent only communicates when criteria events
are generated by criteria 1-7 and 9 have occurred
(see Table 1 for criteria numbers).
Delegating leadership (corresponding to readi-
ness level 4):
• Agent only communicates when 1, 2, 7, or 9 have
occurred.
Thus readiness level and by extension, leadership
style, criteria events, and procedure actions inform the
communication actions that are created in the intent
planner.
Note that unstructured dialogue between the care-
giver and the agent is not possible. If the caregiver
asks a question, the agent is able to respond, but the
agent’s speech is limited to only the actions and re-
sources within the procedure.
To ensure additional safety, the caregiver can de-
cline the agent’s help at any time. When the caregiver
feels competent without the agent’s assistance, they
can decline the agent’s guidance during the procedure
as a whole. In these situations, the agent will only
act as a conduit of communication from the team of
medical experts.
The agent itself is built in Unity and assumes the
appearance of a doctor. In Figure 7, the agent is
shown next to a dummy patient in augmented reality
(AR) which we use for testing. However, our frame-
work also allows for the agent to be displayed on a
computer screen or on a tablet. When testing the sys-
tem in AR, all follower behavior criteria can be mon-
itored in the virtual system. Questions can be asked
via the interface as well and are limited to requests
for help regarding actions, resources, or roles and re-
quests for clarification regarding trajectory.
Through both the virtual and augmented reality
environments, remote medical experts can visualize
the patient, the caregiver, and the procedure steps
done thus far in 3D physical space and make deci-
sions regarding procedure changes accordingly. In
augmented reality, the caregiver can interact with the
augmented reality environment by selecting which ac-
tions have been completed (as shown in Figure 7). For
Simulations of a Computational Model for a Virtual Medical Assistant
103
more information regarding the virtual environment
set-up, please refer to (Querrec et al., 2018).
Figure 7: Our agent built with Unity pictured in augmented
reality.
7 CONCLUSIONS AND FUTURE
WORK
In this paper, we have described a novel model and
the architecture of a novel system in which situational
leadership is applied in a virtual agent system. Simu-
lations of our model demonstrate how follower readi-
ness level can be calculated for use in an agent frame-
work that generates personalized agent behavior to
each unique human user. Using our model, a virtual
agent can lead a novice or expert caregiver through a
medical procedure. This interaction is possible in our
SAIBA-compliant agent framework using Mascaret,
where interaction is completed with communication
actions actuated by both caregiver behavior and infor-
mation from the formalized procedure.
Our algorithms for determining readiness level
and leadership style can be adapted to other circum-
stances outside the medical sphere as well when it
is appropriate for an agent to lead a human being
through any kind of task.
We aim to evaluate this system to determine
whether an agent employing situational leadership is
more effective (preserves the patient’s health, is more
efficient, and reduces stress of the caregiver) than an
agent using the same leadership style throughout the
procedure regardless of readiness level. Measuring
trust and engagement from participants might come
from non-anatomical behavior such as speed of ac-
cepting tasks. We plan to also measure trust and en-
gagement with the agent with survey questions both
before and after the procedure.
We also plan to further explore the co-occurrence
of criteria to understand better how criteria that
happen concurrently affect overall performance and
whether these interaction effects should be taken into
account when calculating readiness level.
ACKNOWLEDGEMENTS
This work has been carried out within the French
project VR-MARS which is funded by the National
Agency for Research (ANR).
REFERENCES
Araszewski, D., Bolzan, M. B., Montezeli, J. H., and Peres,
A. M. (2014). The exercising of leadership in the
view of emergency room nurses. Cogitare Enferm,
19(1):40–8.
Bedford, C. and Gehlert, K. M. (2013). Situational super-
vision: Applying situational leadership to clinical su-
pervision. The Clinical Supervisor, 32(1):56–69.
Bernard, C. (2020). Analyse de l’activit
´
e de soignants
m
´
edicaux et param
´
edicaux sur simulateur haute-
fid
´
elit
´
e lors de simulations d’urgence, en vue de
la conception d’un environnement de soins er-
gonomique. PhD thesis, University of Lorient.
Bickmore, T., Asadi, R., Ehyaei, A., Fell, H., Henault, L.,
Intille, S., Quintiliani, L., Shamekhi, A., Trinh, H.,
Waite, K., Shanahan, C., and Paasche-Orlow, M. K.
(2015). Context-Awareness in a Persistent Hospital
Companion Agent. In Proceedings of the 15th In-
ternational Conference on Intelligent Virtual Agents,
IVA, pages 332–342, Delft, The Netherlands. ACM.
Bosse, T., Duell, R., Memon, Z. A., Treur, J., and van der
Wal, N. (2017). Computational model-based design
of leadership support based on situational leadership
theory. SIMULATION: Transactions of The Society
for Modeling and Simulation International, 93(7).
Castellano, G., Paiva, A., Kappas, A., Aylett, R., Hastie,
H., Barendregt, W., Nabais, F., and Bull, S. (2013).
Towards empathic virtual and robotic tutors. In Pro-
ceedings of the 16th International Conference on Ar-
tificial Intelligence in Education, AIED, pages 733–
736, Memphis, TN, USA. Springer-Verlag.
Cisneros, F., Mar
´
ın, V. I., Orellana, M. L., Per
´
e, N., and
Zambrano, D. (2019). Design process of an intelli-
gent tutor to support researchers in training. In Pro-
ceedings of EdMedia and Innovate Learning, pages
1079–1084, Amsterdam, Netherlands. AACE.
Collins Jackson, A., Bevacqua, E., De Loor, P., and Quer-
rec, R. (2019). Modelling an embodied conversational
agent for remote and isolated caregivers on leadership
styles. pages 256–259. IVA ’19.
Collins Jackson, A., Bevacqua, E., De Loor, P., and Quer-
rec, R. (2021). A computational interaction model for
a virtual medical assistant using situational leadership.
WI-IAT, Essendon, VIC, Australia. ACM.
Collins Jackson, A., Bevacqua, E., DeLoor, P., and Quer-
rec, R. (2020). A taxonomy of behavior for a medical
coordinator by utilizing leadership styles. pages 532–
543. International Conference on Human Behaviour
and Scientific Analysis.
Collins Jackson, A., Gl
´
emarec, Y., Bevacqua, E., De Loor,
ICAART 2022 - 14th International Conference on Agents and Artificial Intelligence
104

P., and Querrec, R. (2022). Speech perception and im-
plementation in a virtual medical assistant. ICAART.
Dermouche, S. and Pelachaud, C. (2019). Engagement
modeling in dyadic interaction. In Proceedings of the
21st International Conference on Multimodal Interac-
tion, ICMI, page 440–445, Suzhou, Jiangsu, China.
ACM.
Flin, R., Patey, R. E., Glavin, R., and Maran, N. (2010).
Anaesthetists’ non-technical skills. BJA: British Jour-
nal of Anaesthesia, 105(1):38–44.
Henrickson, P., Flin, R., McKinley, A., and Yule, S. (2013).
The surgeons’ leadership inventory (sli): a taxonomy
and rating system for surgeons’ intraoperative leader-
ship skills. BMJ Simulation and Technology Enhanced
Learning, 205(6):745–751.
Hersey, P., Blanchard, K. H., and Johnson, D. E. (1988).
Management of Organizational Behavior: Leading
Human Resources, chapter Situational Leadership,
pages 169–201. Prentice-Hall, 5 edition.
Hjortdahl, M., Ringen, A. H., Naess, A.-C., and Wisborg,
T. (2009). Leadership is the essential non-technical
skill in the trauma team - results of a qualitative study.
Scandinavian Journal of Trauma, Resuscitation and
Emergency Medicine, 17(48).
Hoegen, R., Aneja, D., McDuff, D., and Czerwinski, M.
(2019). An end-to-end conversational style matching
agent. https://arxiv.org/pdf/1904.02760.pdf.
Kates, J. M. (2005). Principles of digital dynamic-range
compression. Trends in Amplification, 9:45 – 76.
Kulms, P. and Kopp, S. (2016). Test. In Proceedings of
the 16th International Conference, Intelligent Virtual
Agents, IVA, pages 75–84, Los Angeles, CA, USA.
ACM.
Lee, S. K., Kavya, P., and Lasser, S. C. (2021). Social
interactions and relationships with an intelligent vir-
tual agent. International Journal of Human-Computer
Studies, 150.
Lourdeaux, D., Afoutni, Z., Ferrer, M.-H., Sabouret, N.,
Demulier, V., Martin, J.-C., Bolot, L., Boccara, V., and
Lelong, R. (2019). Victeams: A virtual environment
to train medical team leaders to interact with virtual
subordinates. page 241–243. IVA ’19.
Montenegro, C., Zorrilla, A. L., Olaso, J. M., Santana, R.,
Justo, R., Lozano, J. A., and Torres, M. I. (2019). A
dialogue-act taxonomy for a virtual coach designed to
improve the life of elderly. Multimodal Technologies
and Interaction, 3(52).
Nakhal, B. (2017). Generation of communicative intentions
for virtual agents in an intelligent virtual environment
: application to virtual learning environment. PhD
thesis.
Pecune, F., Cafaro, A., Ochs, M., and Pelachaud, C. (2010).
Evaluating social attitudes of a virtual tutor. In Pro-
ceedings of the 16th International Conference on In-
telligent Virtual Agents, IVA, pages 245–255, Los An-
geles, CA, USA. ACM.
Philip, P., Dupuy, L., Auriacombe, M., Serre, F., de Sevin,
E., Sauteraud, A., and Franchi, J.-A. M. (2020).
Trust and acceptance of a virtual psychiatric interview
between embodied conversational agents and outpa-
tients. NPJ Digital Medicine, (1).
Querrec, R., Taoum, J., Nakhal, B., and Bevacqua, E.
(2018). Model for verbal interaction between an em-
bodied tutor and a learner in virtual environments.
pages 197–202.
Saerbeck, M., Schut, T., Bartneck, C., and Janse, M. D.
(2010). Expressive robots in education: varying the
degree of social supportive behavior of a robotic tutor.
In Proceedings of the SIGCHI Conference on Human
Factors in Computing Systems, CHI, page 1613–1622,
Atlanta, GA, USA. ACM.
Sims, H. P., Faraj, S., and Yun, S. (2009). When should a
leader be directive or empowering? how to develop
your own situational theory of leadership. Business
Horizons, 52(2):149–158.
Taoum, J., Raison, A., Bevacqua, E., and Querrec, R.
(2018). An adaptive tutor to promote learners’ skills
acquisition during procedural learning.
Vilhj
´
almsson, H., Cantelmo, N., Cassell, J., Chafai, N.,
Kipp, M., Kopp, S., Mancini, M., Marsella, S., Mar-
shall, A., Pelachaud, C., Ruttkay, Z., Th
´
orisson, K.,
Welbergen, H., and Werf, R. (2007). The behav-
ior markup language: Recent developments and chal-
lenges. volume 4722, pages 99–111.
Yang, P.-J. and Fu, W.-T. (2016). Mindbot: A social-based
medical virtual assistant. In Proceedings of the 2016
International Conference on Healthcare Informatics,
ICHI, pages 319–319, Chicago, IL, USA. IEEE.
Yule, S., Flin, R., Maran, N., Rowley, D., Youngson, G., and
Paterson-Brown, S. (2008). Surgeons’ non-technical
skills in the operating room: Reliability testing of
the notss behavior rating system. World journal of
surgery, 32:548–56.
Simulations of a Computational Model for a Virtual Medical Assistant
105
