
Migration of Telemedicine Applications to National Telematics
Infrastructure using Epilepsy Treatment as an Example
Salima Houta
1 a
, Tim Wilking
1
, Marcel Kl
¨
otgen
1 b
and Falk Howar
2 c
1
Fraunhofer Institute for Software and Systems Engineering, Dortmund, Germany
2
Department of Computer Science, TU Dortmund University Dortmund, Dortmund, Germany
Keywords:
Telematics Infrastructure, IHE, HL7 FHIR, Epilepsy, Electronic Case Record, Electronic Patient Record.
Abstract:
Digitization in epilepsy treatment, which usually is an intersectoral effort, offers great potential. Aggregated
healthcare information from different actors involved in the treatment process provides an important basis for
therapy decisions. More and more telemedicine solutions for the treatment of patients with epilepsy focus in
particular on patient involvement via a digital seizure diary. This is intended to replace the currently mostly
paper-based diaries. However, there is no widespread use in practice. The introduction of the national telem-
atics infrastructure (TI) offers the opportunity to make telemedical applications accessible to a larger group
of patients and medical institutions in Germany. The E-Health Act, which came into force on December 29,
2015, defines a roadmap for the gradual introduction of a telematics infrastructure in the German healthcare
system. In addition to the specified TI components for secure and standardized data exchange, health IT ser-
vice providers can migrate their existing digital solutions for healthcare in the TI. This article describes the
migration of a developed telemedical infrastructure for epilepsy care into the national telematics infrastruc-
ture. First, an analysis of the telemedicine infrastructure is made with regard to supported integration options.
Then, considering the chosen approach, an integration concept is designed using an example scenario.
1 INTRODUCTION
Epilepsy is considered a complex chronic disorder
that is highly prevalent worldwide (Beghi, 2020) and
requires treatment by multiple healthcare providers
(Bast et al., 2017). In addition, patient self-
management and family involvement can be critical
to identify and optimize an appropriate diagnosis and
treatment (Kobau and DiIorio, 2003). Telemedicine
can support the coordination of epilepsy care among
stakeholders by using communication and informa-
tion technologies in order to share relevant data for
diagnosis and treatment. A major leap in the develop-
ment of telemedicine solutions for epilepsy patients
was triggered by the Corona pandemic (Power et al.,
2020; Cross et al., 2021; Datta et al., 2021; Banks
et al., 2021). Previously, there were few studies de-
scribing the use of telemedicine health technologies
in epilepsy care, mainly with the aim of providing
consistent care in rural and geographically isolated ar-
eas (Ahmed et al., 2008; Rasmusson and Hartshorn,
a
https://orcid.org/0000-0001-8452-4263
b
https://orcid.org/0000-0003-4109-8641
c
https://orcid.org/0000-0002-9524-4459
2005; Haddad et al., 2015; Lua and Neni, 2013).
Most of them cite benefits in terms of patient satis-
faction and lower treatment costs. Although improv-
ing the quality and performance of care through in-
tegrated and comprehensive data collection as a basis
for therapeutic interventions is obvious, health tech-
nologies for cross-sector communication with elec-
tronic health records are not consistently used in
epilepsy care. Recent studies also emphasize that the
implementation of a solution is not sufficient, but its
integration into existing processes and systems is es-
sential to achieve adoption by clinicians. Integrat-
ing epilepsy self-management applications into the
treatment process can also create benefits. Typically,
these applications include modules such as seizure di-
aries, medication adherence protocols, medication re-
minders, medication allergy diaries, and support in
emergency situations (Alzamanan et al., 2021; Es-
coffery et al., 2018; Liu et al., 2016; Ranganathan
et al., 2015). Page et al. (2018) criticizes that the
information collected by self-management applica-
tions cannot be transferred easily to the clinical sys-
tem and must be recorded in a redundant and time-
consuming manner. In contrast to this, he positively
Houta, S., Wilking, T., Klötgen, M. and Howar, F.
Migration of Telemedicine Applications to National Telematics Infrastructure using Epilepsy Treatment as an Example.
DOI: 10.5220/0010904000003123
In Proceedings of the 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2022) - Volume 5: HEALTHINF, pages 697-704
ISBN: 978-989-758-552-4; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
697

highlights that a health record co-authored by the pa-
tient has the potential to reduce effort. Technologies
for seamless data integration increase the acceptance
of such solutions. Changing existing ways of collabo-
ration supported by new technologies is challenging,
and the management of separated electronic health
records consumes additional effort if they are not in-
tegrated in the medical process and existing technol-
ogy (Page et al., 2018). Project MOND, funded by
the Ministry of Health, aims to integrate a developed
telemedicine infrastructure for epilepsy treatment into
the existing system infrastructure. This includes an
epilepsy self-management application, a web portal
for patient (and family) communication with physi-
cians, and solutions for physician-to-physician com-
munication based on international standards (Houta
et al., 2020). Standardized integration into existing
system landscapes has not yet been implemented and
are subject of this paper.
In this paper we contribute integration approaches
for telemedicine infrastructures into existing system
landscapes. We use the national telematics infras-
tructure (TI), which has created the prerequisites for
a nationwide exchange of medical data (Jorzig and
Sarangi, 2020). In the Background section, this ar-
ticle first describes our telemedical solution to be in-
tegrated. Then, in the same chapter, Digital Health
Applications and the TI, which are both regulated by
law, are presented. Afterwards, the applied methods
are explained in detail. In the Results section, deci-
sions on the classification of our solution as well as
different integration settings are presented using an
epilepsy reference scenario as an example. This is fol-
lowed by a discussion of the different integration ap-
proaches. The paper concludes with a summary and
an outlook on the next steps.
2 BACKGROUND
2.1 Telemedical Infrastructure for
Epilepsy Treatment with Electronic
Case Record Integration
In a project funded by the German Federal Ministry of
Education and Research, hospitals, technical partners,
scientists as well as patients and relatives have jointly
designed a telemedical infrastructure for epilepsy care
with Electronic Case Record integration (TEPI). The
compontents of TEPI (Figure 1) are described in more
detail in the following sections.
2.1.1 Sensor-based Mobile Application
The sensor-based mobile application is a daily com-
panion for the patient. The patient can record data
(e.g., seizures, side effects, medication use, and
mood) and share it with their therapists and family
members via secure sharing mechanisms. In addition,
the patient can receive data from their therapists. If
a shared structured medication schedule is available,
it can be used in the patient application as a basis for
medication reminders. The mobile application is con-
nected to a sensor that measures vital signs and events
(e.g., seizure events). It uses the security and data
exchange services of the telemedicine infrastructure
to securely edit, store and share data. The developed
mobile application is currently being restructured ac-
cording to the guidelines of a Digital Health Applica-
tion (BfArM, 2020).
2.1.2 Web Portal
Depending on the user role, the web portal either in-
tegrates just the services of the telemedicine infras-
tructure (e.g., if the user is a patient or informal care-
giver), or the services of the ECR infrastructure (e.g.,
if the user is a physician) in addition. The portal
provides authenticated physicians with a view of all
epilepsy case records from their medical institution
that are stored in the ECR infrastructure. The case
records are created after the patient has provided a
valid consent. Physicians can store various medi-
cal information relevant to intersectoral epilepsy care
within the ECR and share it with other medical in-
stitutions involved in the treatment, provided they are
also authorized by the patient to access the ECR. The
portal allows storage of both unstructured information
such as physician letters in PDF format and structured
data such as the structured medication plan based on
the FHIR format. Physicians can share medical infor-
mation (e.g., medication plan) with the patient, and
they can see if new data has been received from the
patient (e.g., seizure documentation) and store that
data in their own medical data management system.
The web portal can also be used by patients and infor-
mal caregivers (e.g., parents) with the telemedicine
infrastructure.
2.1.3 FHIR-based Telemedical Infrastructure
The patient as well as relatives are connected via the
telemedicine infrastructure. The implementation is
based on the lightweight HL7 FHIR standard, as the
focus is on the connection of mobile devices as well
as the transmission of structured data collected via the
HEALTHINF 2022 - 15th International Conference on Health Informatics
698
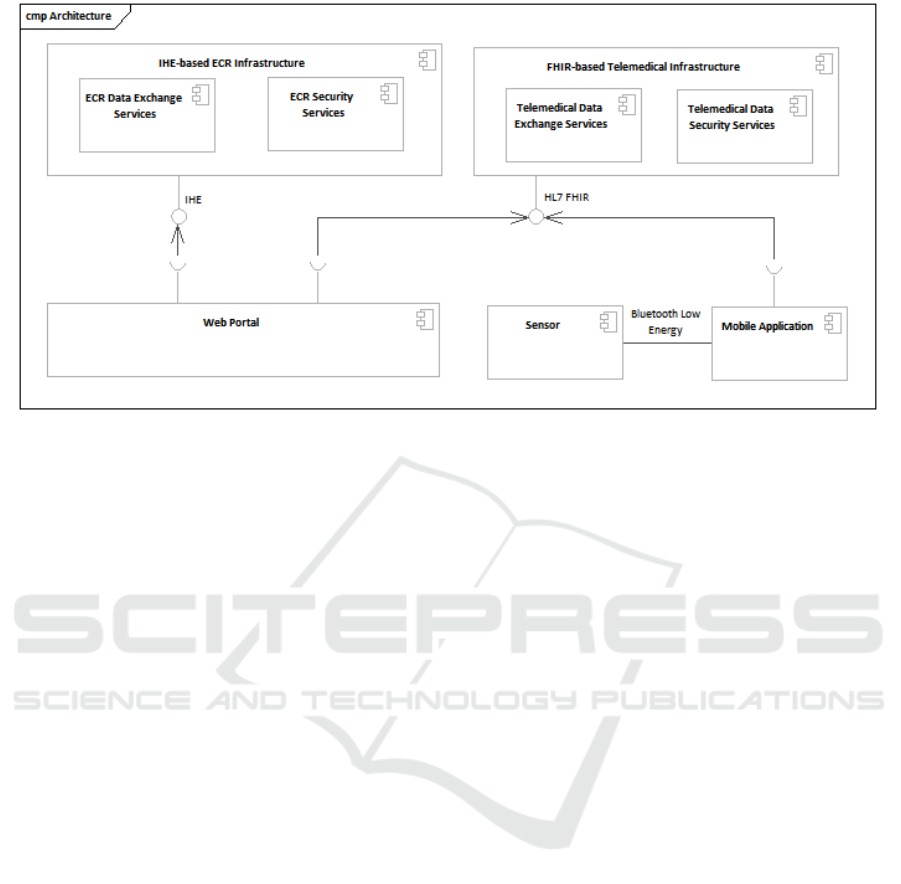
Figure 1: Telemedical Infrastructure for Epilepsy Treatment.
app or transmitted by the sensor. The telemedicine in-
frastructure includes both data exchange and security
services. Security mechanisms ensure that authenti-
cated patients can give selected healthcare providers
access to therapy-relevant data. Access is possible
both via the mobile application and the web portal.
Authenticated and authorized healthcare providers
can use the web portal to retrieve patient data or share
data with the patient.
2.1.4 IHE-based ECR Infrastructure
For the exchange between medical stakeholders in-
volved in the treatment we use the Electronic Case
Record (ECR). The ECR was developed in Germany
to support communication between physicians in-
volved in a treatment case (Kuhlisch et al., 2012).
It targets the treatment of diseases involving multi-
ple physicians and focuses in particular on ”long-term
patients” with severe or chronic diseases, whose treat-
ment progress needs to be tracked and regularly coor-
dinated by multiple stakeholders. The architecture of
the ECR is based on Integrating the Healthcare Enter-
prises (IHE) profiles and takes into account national
privacy and data security requirements. Case records
are tied to a diagnosis or purpose and thus are not
non-specific data collections. The ECR is ”physician-
led,” meaning it is authored and controlled by physi-
cians, and thus, unlike patient-managed records, pro-
vides a reliable basis for treatment decisions. The
ECR infrastructure includes data exchange and secu-
rity services. In order to involve non-medical actors
in the data exchange, the ECR Infrastructure can be
connected with the telemedical services (Deiters and
Houta, 2015).
2.2 Digital Health Applications
Digital health applications (DiGA) are medical de-
vices of risk class I and IIa according to the Medi-
cal Device Regulation (MDR). Physicians and phys-
iotherapists can prescribe DiGAs for health insur-
ance benefits as a part of a therapy since the Digital
Health Care Act (DVG) came into force on Decem-
ber 19, 2019. Patients and physicians are the target
users of the developed DiGA. Thus, physicians will
receive additional remuneration if additional services
become necessary with the use of the DiGA. For a
DiGA to be prescribed, it must be listed in the so-
called DiGA directory. Manufacturers must provide
scientific evidence of a positive supply effect of the
application. After inclusion in the DiGA directory,
the medical reimbursement system is adjusted with
the medical services required in connection with the
DiGA. In addition to demonstrating a positive care
effect, manufacturers of DiGAs must meet require-
ments including security and functional suitability,
conformity with the General Data Protection Regu-
lation, user-friendliness, and compatibility commit-
ments regarding support for standards and the telem-
atics infrastructure. (BfArM, 2020)
2.3 National Telematics Infrastructure
in Germany
According to § 291a (7) (2) SGB V, the company
Gesellschaft f
¨
ur Telematikanwendungen der Gesund-
heitskarte mbH (gematik) creates an interoperable
and compatible TI and coordinates its operation. The
TI is a closed network that can only be used by reg-
Migration of Telemedicine Applications to National Telematics Infrastructure using Epilepsy Treatment as an Example
699

istered users with special ID cards and connectors or
access gateways (Figure 2). It connects stakeholders
in the field of health (e.g. doctors, hospitals, phar-
macies, patients) and ensures the cross-system and
secure exchange of information (Jorzig and Sarangi,
2020). The complete specification is available on the
gematik portal. The rough architecture is described
below.
2.3.1 Consumer Zone
The Consumer Zone is located in healthcare organi-
zations and consists of information systems and their
interaction logic. TI applications can be integrated via
client modules (e.g., medication add on) into existing
systems.
2.3.2 TI Core - Decentralized and Central Zone
The core of the TI infrastructure is comprised of the
decentralized zone and the central zone. The compo-
nents of the decentralized zone include all TI compo-
nents that are set up and installed in a healthcare or-
ganization to enable the secured use of the TI. These
are, for example, smart cards, card terminals and
the connectors. Smartcards are issued to individuals
or healthcare organizations and aim to ensure secure
data exchange through authentication and encryption.
Specific e-Health Card terminals for use with the TI
can be connected to the TI connector. Each time a
connection between an e-Health card terminal and a
connector is established, the terminals must authenti-
cate themselves to the connector. Access to a patient’s
medical data located in the Provider Zone of the TI is
only possible via a two-factor authentication process.
Both the physician and the patient must authenticate
themselves with their smartcard using the card termi-
nals. The connector then represents a gateway to the
TI network with security features such as a firewall
and VPN connections. It enables information sys-
tems of the healthcare organizations to securely ac-
cess smart cards and the e-Health card terminal. The
TI connector also ensures that systems in the medical
organisations are protected against attacks originating
from the TI network. The central zone hosts central
services of the TI that are essential for communica-
tion and data exchange. These include, among others,
the OSCP responder and the configuration services as
well as a healthcare directory service.
2.3.3 Provider Zone
The Provider Zone is directly connected to the Cen-
tral Zone and includes all TI applications. Appli-
cations of the TI are standardized solutions that ad-
dress central and modular use cases in healthcare.
The goal of this approach is to create uniform imple-
mentations of these use cases in the health IT land-
scape and thus to facilitate and support development
of added value and interoperability. The TI defines
the following applications: Electronic Prescription,
Electronic Patient Record (ePA), KIM - Communica-
tion in Medicine, Electronic Medication Plan, Emer-
gency Data Management, Qualified Electronic Signa-
ture, Management of Patient Data and TI Messenger.
All TI applications must comply with the specifica-
tions of the TI platform to ensure secure and standard-
ized operation. Applications are accessed via client
modules that are part of the Consumer Zone.
The core application of the TI is the ePA, which
supports data exchange between the patient and the
healthcare provider, but also data exchange between
several healthcare providers. The patient can use the
ePA via an access gateway of the ePA front end, which
is provided by the patient’s health insurance company.
Healthcare providers can access the ePA via the TI
connector, but must be authorized to access data by
the patient using an identification card. The connec-
tor establishes the secure and standardized exchange
of systems in medical organisations with the ePA sys-
tem in the TI. A new draft law from the German Fed-
eral Ministry of Health stipulates that patients should
be able to send data from DiGAs to the ePA and vice
versa from April 2023 (
¨
Arzteblatt, 2021). Prerequi-
sites for this are created with the ongoing specifica-
tion of HL7 FHIR-based medical information objects
(MIO) (Weber and Heitmann, 2021).
2.3.4 Existing Application Zone
gematik intends to ensure the use of the telematics
infrastructure for other applications of the healthcare
system as well as health research in accordance with §
291a (7) sentence 3 SGB V. For this purpose, gematik
sets the conditions for the use of TI by other appli-
cations to be met by providers, as well as the de-
tails of the confirmation process as well as the neces-
sary test criteria. These “other applications” (“Weit-
ere Anwendungen f
¨
ur den Datenaustausch in der TI”,
WANDA) are distinguished into the WANDA Basic
and WANDA Smart applications. WANDA Smart ad-
dresses other health care applications which are em-
bedded in the Provider Zone of the TI. These appli-
cations have access to TI services. WANDA Basic
are other health care applications without access to
services of the TI in connected healthcare networks.
The difference between these application types is the
degree of integration into the TI. The deeper the inte-
gration, the more complex the approval process. After
a successful approval, an application is listed in the
HEALTHINF 2022 - 15th International Conference on Health Informatics
700
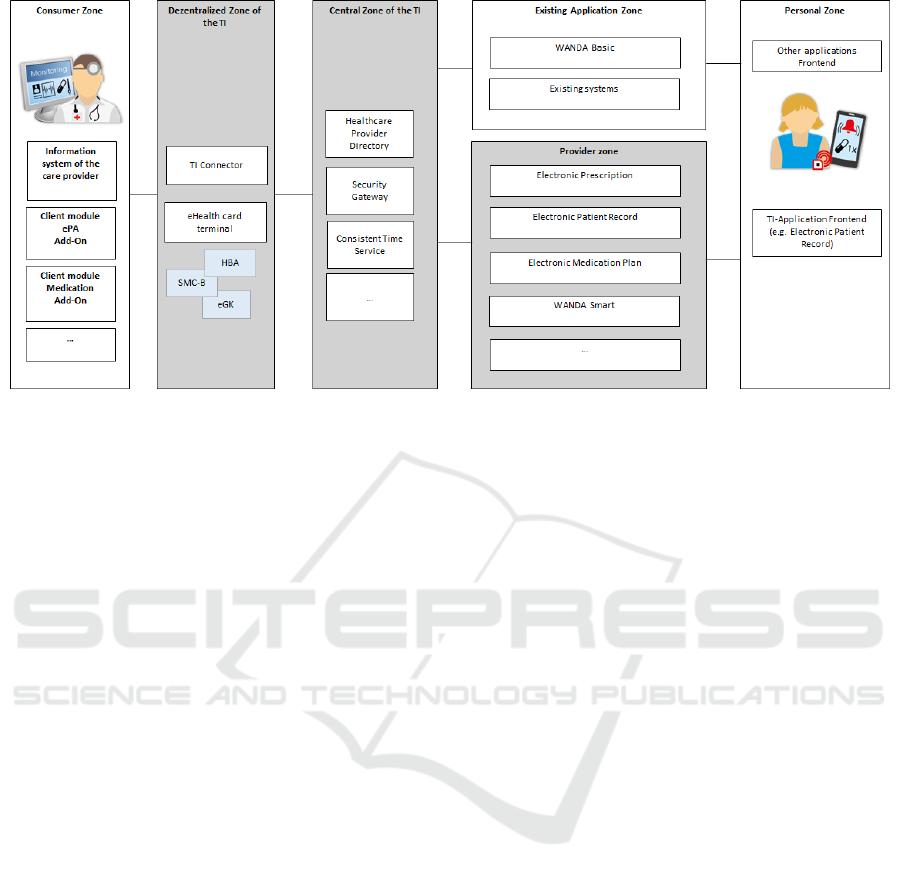
Figure 2: German National Telematics Infrastructure.
interoperability directory vesta (Grode and L
¨
uckhof,
2021).
2.3.5 Personal Zone
The patient’s applications are located in the personal
zone and are also under the patient’s control there.
Access to the TI (e.g. via the ePA front end) is se-
cured via access gateways.
3 METHOD
With the analysis of the legally regulated DiGAs and
TI, we were able to identify basically two integration
paths for TEPI.
• Integration as a WANDA
• Integration via the ePA
To conceptualize the integration as a WANDA, we
first applied gematik’s criteria to TEPI to determine
which type of application best represented our appli-
cation. Subsequently, based on the medical guide-
line for epilepsy (Bast et al., 2017), we formulated
an example scenario describing different sections in
the treatment process in different participating insti-
tutions and considering patient involvement via an
epilepsy self-management application. Along the sce-
nario, we have outlined a hybrid integration design
considering integration as a WANDA and integration
via the ePA.
4 RESULTS
4.1 Classification
Since we develop and operate several telemedical ap-
plications with ECR integration that we intend to mi-
grate to the TI, we are pursuing the integration of an
Existing Application Zone in the TI. For the use case
we are developing, using TI services does not add sig-
nificant value to interoperability. For example, the TI
directory service does not map all the groups of peo-
ple that should have access to the epilepsy data in our
use case, and therefore cannot be used. Thus, our inte-
gration strategy follows the WANDA Basic approach.
4.2 Integration Settings
With the approval as WANDA Basic, the TEPI re-
mains in its own network, but is accessible via the TI
for other TI users. Moreover, linking the ePA with our
Mobile Application, which is intended to be approved
as a DiGA, enables the exchange of structured data,
such as seizure documentation via the ePA. Thus, sev-
eral integration settings are conceivable, which are
outlined in Figure 3 and discussed below.
4.2.1 WANDA Basic - Loose Integration
This integration solution uses the TEPI, which is in-
tegrated in the TI as WANDA, for data exchange in
the context of epilepsy treatment. All TI users have
the option of using the TEPI applications, provided
this is defined organizationally. In this solution, only
the web portal and the mobile app are used for the
Migration of Telemedicine Applications to National Telematics Infrastructure using Epilepsy Treatment as an Example
701
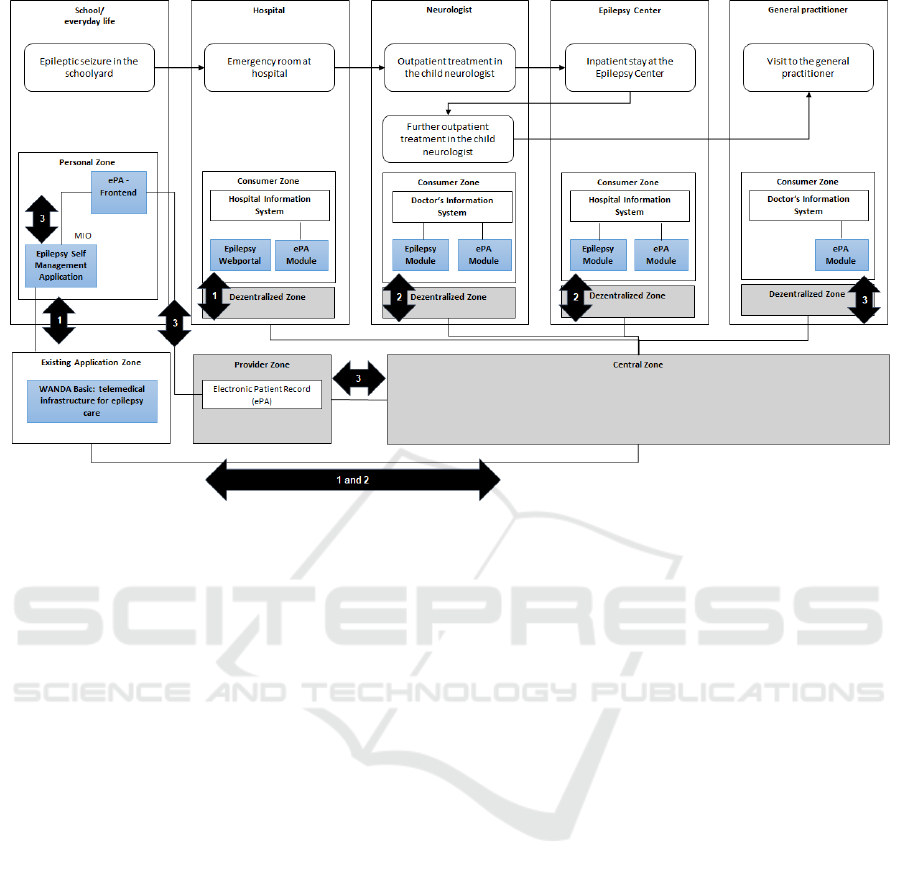
Figure 3: Integration Settings in Epilepsy Treatment. 1: WANDA - loose integration; 2: WANDA - deep integration; 3:
DiGA-ePA integration.
exchange via TEPI. This enables cross-institutional
secure exchange between care providers involved in
treatment and between care providers and patients via
the TI for all TI users. However, requirements for
seamless communication without media disruptions
are not met. Data must be recorded redundantly and
time-consumingly by the service providers in order
to get from the TEPI to the existing systems or vice
versa, since there is no integration in the existing sys-
tem landscape in this setting.
4.2.2 WANDA Basic - Deep Integration
In this setting, a greater depth of integration is sought.
Since TEPI is based on IHE and ECR, systems sup-
porting these standards can easily be extended with
client functionalities for importing or exporting data.
For example, seizure documentation from TEPI can
be displayed via a hospital information system and
transferred to the local patient record after validation
by healthcare providers. Similarly, data originating
from hospital information systems can be shared with
additional healthcare providers or the patient. In addi-
tion to the interfaces for sending data, security func-
tions (e.g., authentication to TEPI) must be consid-
ered in the primary systems separately, since the au-
thentication services of the TI are not used for TEPI.
4.2.3 WANDA Basic - DIGA-ePA Integration
In this setting, the mobile application (DiGA) is in-
tegrated via the ePA. The patient sends data (MIOs)
from his DiGA to his ePA and authorizes relevant
healthcare providers for access via the ePA front end
(Figure 4). Authorized physicians can view and use
the patient’s data via the ePA module in the medical
facility. The implementation of integrating DiGAs
and ePAs is still in its early stages, but promises to
be far-reaching as data from the DiGA reaches physi-
cians who do not (want to) use other systems besides
the ePA to exchange data with other physicians or pa-
tients.
4.2.4 Discussion
This paper discussed the importance of integrating
existing telemedicine solutions into the existing sys-
tem landscape in medical facilities. The basis for in-
tegration is the legally required TI. The integration
approaches described are not mutually exclusive, but
represent approaches that can be operated in parallel.
While the loose integration of WANDA can be de-
ployed quickly with little effort and adaptation of ex-
isting systems, the other integration settings involve
greater implementation effort. This The additional
effort is beneficial, since a deeper integration of pa-
tient co-authored data supports the medical and orga-
nizational process by avoiding redundant documenta-
HEALTHINF 2022 - 15th International Conference on Health Informatics
702
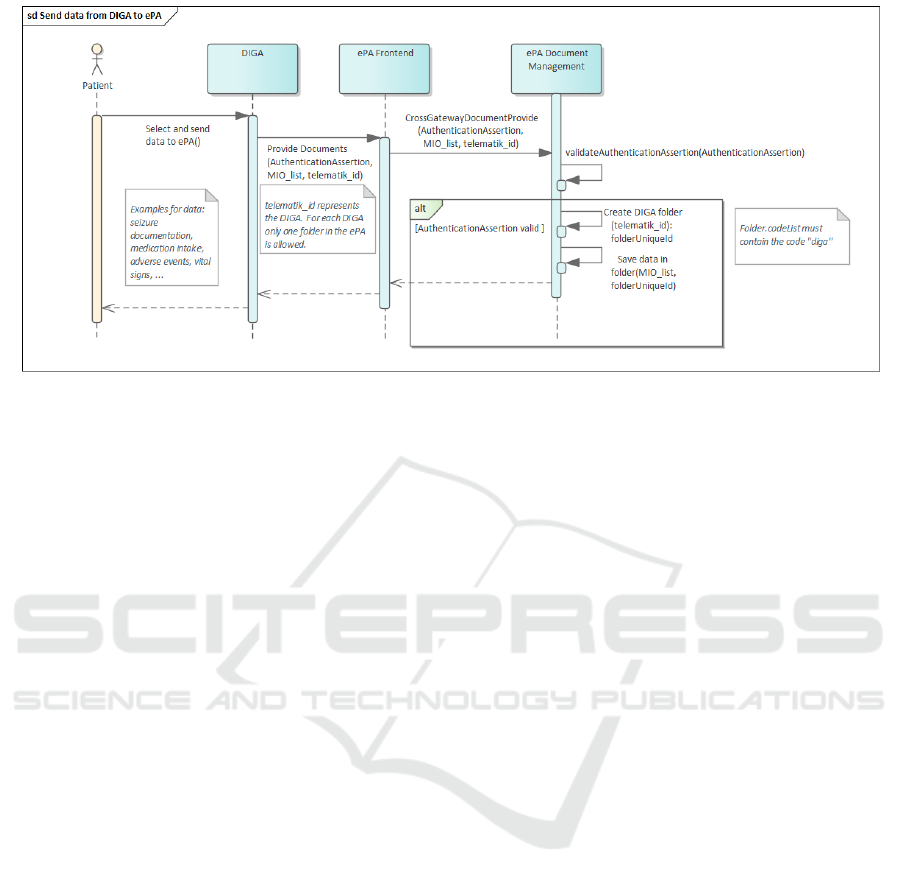
Figure 4: Sequence Diagram Send Data from DIGA to ePA.
tion. For a short time-to-market, it is advisable to start
with loose integration and, if the system manufactur-
ers are willing to implement appropriate interfaces, to
replace the loose integration with deep integration.
We decided to take a hybrid approach, as both
ePA and ECR-based solutions like TEPI have differ-
ent goals. While ePA pursues a digital aggregation of
all patient data from different medical facilities and is
patient-driven, ECR addresses case-related commu-
nication between service providers and is controlled
by them. Thus, TEPI can be used as a WANDA in
the narrow treatment concept of epilepsy and can be
specifically used and coordinated by physicians in-
volved in the treatment of epilepsy. Nevertheless,
there are information objects that are also relevant in
other treatment contexts (e.g., medications). Here, the
integration to the ePA offers a possibility to exchange
them across treatment cases.
A restriction with regard to the integration of all
actors in our use case via the TI still exists due to the
restriction of the possibility of also connecting infor-
mal caregivers to the TI. Therefore, an informal care-
giver can only be integrated into the data exchange via
the patient as an intermediary.
5 CONCLUSION
Our goal in this paper was to present a concept for
integrating a telemedicine infrastructure with the TI.
A detailed analysis of the types of systems (DiGA) or
infrastructures (TI) in healthcare driven by law was
our starting point. Using an example scenario, we de-
veloped and discussed integration settings for TEPI.
There is no solution that can be applied to all medical
facilities. Here, depending on the willingness of sys-
tem vendors to adapt their systems as well as on the
treatment context, it has to be decided which integra-
tion setting is suitable in a medical organization.
We are currently working on a regulatory roadmap
for the introduction of the developed system solutions
into the healthcare market. A prerequisite for the op-
erationalization of our solution is the successful com-
pletion of the confirmation procedure, taking into ac-
count the gematik approval criteria, as well as the ap-
proval of the mobile application as a DiGA. A com-
plete implementation of our integration approach is
not yet possible, as concepts for the integration of
DiGA and ePA still have to be awaited. Here, we
want to get involved in the development of MIOs to
harmonize epilepsy data nationwide. Another impor-
tant step is to approach the manufacturers of the sys-
tems of the participating hospitals in order to pre-
pare a deep integration into their systems. Ideally,
this should also be based on already established user-
centered concepts of process support in epilepsy treat-
ment by technical systems in order to promote accep-
tance by users.
ACKNOWLEDGEMENTS
The authors acknowledgement the financial support
by the Federal Ministry of Health in the framework of
MOND (project number G512F11007).
REFERENCES
Ahmed, S. N., Mann, C., Sinclair, D. B., Heino, A., Iskiw,
B., Quigley, D., and Ohinmaa, A. (2008). Feasibil-
ity of epilepsy follow-up care through telemedicine:
Migration of Telemedicine Applications to National Telematics Infrastructure using Epilepsy Treatment as an Example
703

A pilot study on the patient’s perspective. Epilepsia,
49(4):573–585.
Alzamanan, M. Z., Lim, K.-S., Ismail, M. A., and Ghani,
N. A. (2021). Self-management apps for people with
epilepsy: Systematic analysis. JMIR mHealth and
uHealth, 9(5):e22489.
Banks, J., Corrigan, D., Grogan, R., El-Naggar, H., White,
M., Doran, E., Synnott, C., Fitzsimons, M., Delanty,
N., and Doherty, C. P. (2021). Love in a time of covid:
Clinician and patient experience using telemedicine
for chronic epilepsy management. Epilepsy & Behav-
ior, 115:107675.
Bast, T., Bauer, J., Berkenfeld, R., Elger, C. E., Hamer,
H., Malter, M., Mayer, T., von Podewils, F., Runge,
U., Schmidt, D., et al. (2017). Erster epileptischer
anfall und epilepsien im erwachsenenalter. Aktuelle
Neurologie, 44(09):603–636.
Beghi, E. (2020). The epidemiology of epilepsy. Neuroepi-
demiology, 54(2):185–191.
BfArM (2020). Das fast-track-verfahren f
¨
ur digitale
gesundheitsanwendungen (diga) nach § 139e sgb v–
ein leitfaden f
¨
ur hersteller, leistungserbringer und an-
wender.
Cross, J. H., Kwon, C.-S., Asadi-Pooya, A. A., Bal-
agura, G., Gomez-Iglesias, P., Guekht, A., Hall, J.,
Ikeda, A., Kishk, N. A., Murphy, P., et al. (2021).
Epilepsy care during the covid-19 pandemic. Epilep-
sia, 62(10):2322–2332.
Datta, P., Barrett, W., Bentzinger, M., Jasinski, T.,
Jayagopal, L. A., Mahoney, A., Pearon, C., Swami-
nathan, A., Vuppala, A., Samson, K. K., et al. (2021).
Ambulatory care for epilepsy via telemedicine dur-
ing the covid-19 pandemic. Epilepsy & Behavior,
116:107740.
Deiters, W. and Houta, S. (2015). Entwicklung
telemedizinischer l
¨
osungen auf basis der elek-
tronischen fallakte. Bundesgesundheitsblatt-
Gesundheitsforschung-Gesundheitsschutz,
58(10):1079–1085.
Escoffery, C., McGee, R., Bidwell, J., Sims, C., Thropp,
E. K., Frazier, C., and Mynatt, E. D. (2018). A re-
view of mobile apps for epilepsy self-management.
Epilepsy & Behavior, 81:62–69.
Grode, A. and L
¨
uckhof, S. (2021). Interoper-
abilit
¨
atsverzeichnis vesta. In Telemedizin, pages 375–
387. Springer.
Haddad, N., Grant, I., and Eswaran, H. (2015).
Telemedicine for patients with epilepsy: a pilot ex-
perience. Epilepsy & Behavior, 44:1–4.
Houta, S., Meschede, C., Beeres, K., Surges, R., and
Kl
¨
otgen, M. (2020). User-centered design and
evaluation of standard-based health technologies for
epilepsy care.
Jorzig, A. and Sarangi, F. (2020). E-health-gesetz. In
Digitalisierung im Gesundheitswesen, pages 95–103.
Springer.
Kobau, R. and DiIorio, C. (2003). Epilepsy self-
management: a comparison of self-efficacy and
outcome expectancy for medication adherence and
lifestyle behaviors among people with epilepsy.
Epilepsy & Behavior, 4(3):217–225.
Kuhlisch, R., Kraufmann, B., and Restel, H. (2012). Elec-
tronic case records in a box: Integrating patient data
in healthcare networks. Computer, 45(11):34–40.
Liu, X., Wang, R., Zhou, D., and Hong, Z. (2016). Fea-
sibility and acceptability of smartphone applications
for seizure self-management in china: questionnaire
study among people with epilepsy. Epilepsy & Be-
havior, 55:57–61.
Lua, P. L. and Neni, W. S. (2013). Health-related
quality of life improvement via telemedicine for
epilepsy: printed versus sms-based education inter-
vention. Quality of Life Research, 22(8):2123–2132.
Page, R., Shankar, R., McLean, B. N., Hanna, J., and New-
man, C. (2018). Digital care in epilepsy: a conceptual
framework for technological therapies. Frontiers in
neurology, 9:99.
Power, K., McCrea, Z., White, M., Breen, A., Dunleavy,
B., O’Donoghue, S., Jacquemard, T., Lambert, V., El-
Naggar, H., Delanty, N., et al. (2020). The develop-
ment of an epilepsy electronic patient portal: Facilitat-
ing both patient empowerment and remote clinician-
patient interaction in a post-covid-19 world. Epilep-
sia, 61(9):1894–1905.
Ranganathan, L. N., Chinnadurai, S. A., Samivel, B., Ke-
savamurthy, B., and Mehndiratta, M. M. (2015). Ap-
plication of mobile phones in epilepsy care. Interna-
tional Journal of Epilepsy, 2(01):028–037.
Rasmusson, K. A. and Hartshorn, J. C. (2005). A compar-
ison of epilepsy patients in a traditional ambulatory
clinic and a telemedicine clinic. Epilepsia, 46(5):767–
770.
¨
Arzteblatt (2021). Diga sollen ab 2023 interoperabel mit
elektronischer patientenakte sein.
¨
Arzteblatt.
Weber, S. and Heitmann, K. U. (2021). Interoper-
abilit
¨
at im gesundheitswesen: auch f
¨
ur digi-
tale gesundheitsanwendungen (diga) verordnet.
Bundesgesundheitsblatt-Gesundheitsforschung-
Gesundheitsschutz, pages 1–7.
HEALTHINF 2022 - 15th International Conference on Health Informatics
704
