
A Framework for AI-enabled Proactive mHealth with Automated
Decision-making for a User’s Context
Muhammad Sulaiman, Anne Håkansson and Randi Karlsen
Department of Computer Science, UiT The Arctic University of Norway, Tromsø, Norway
Keywords: mHealth, Proactive Health, Artificial Intelligence, Machine Learning, Wearables, Just-in-Time Adaptive
Interventions, Automated Decision-making, Digital Health Intervention, Self-empowerment.
Abstract: Health promotion is to enable people to take control over their health. Digital health with mHealth empowers
users to establish proactive health, ubiquitously. The users shall have increased control over their health to
improve their life by being proactive. To develop proactive health with the principles of prediction, prevention,
and ubiquitous health, artificial intelligence with mHealth can play a pivotal role. There are various challenges
for establishing proactive mHealth. For example, the system must be adaptive and provide timely
interventions by considering the uniqueness of the user. The context of the user is also highly relevant for
proactive mHealth. The context provides parameters as input along with information to formulate the current
state of the user. Automated decision-making is significant with user-level decision-making as it enables
decisions to promote well-being by technological means without human involvement. This paper presents a
design framework of AI-enabled proactive mHealth that includes automated decision-making with predictive
analytics, Just-in-time adaptive interventions and a P5 approach to mHealth. The significance of user-level
decision-making for automated decision-making is presented. Furthermore, the paper provides a holistic view
of the user's context with profile and characteristics. The paper also discusses the need for multiple parameters
as inputs, and the identification of sources e.g., wearables, sensors, and other resources, with the challenges
in the implementation of the framework. Finally, a proof-of-concept based on the framework provides design
and implementation steps, architecture, goals, and feedback process. The framework shall provide the basis
for the further development of AI-enabled proactive mHealth.
1 INTRODUCTION
Center for disease control and prevention (CDC)
defined public health as "the science and art of
preventing disease, prolonging life, and promoting
health through the organized efforts and informed
choices of society, organizations, public and private
communities, and individuals" (Winslow, 1920).
This definition likewise emphasizes the need of
promoting health and preventing disease providing a
holistic solution for the individual. To promote health,
people must be enabled to increase control over their
health to be able to improve it, World health
organization (WHO) (WHOa, 2021).
Health promotion and wellbeing are vital as
healthcare globally is dealing with many challenges
(Haseltine, 2021). One major challenge is an aging
population, life expectancy has increased in the last
century or so for instance in Norway it is 84.2 years
for women and 80.6 years for men (NIPH, 2018).
This increase intensifies the development of multiple
chronic diseases like cardiovascular disease, stroke,
cancer, osteoarthritis, and dementia (Atella et al.,
2018). WHO estimates that about half of the disease
burden is from chronic illness (WHOb, 2021). In the
US, about 6 out of 10 adults suffer from chronic
diseases (CDC, 2021).
The healthcare sector must endure the pressure of
dealing with a public health crisis. A recent example
is the pandemic (WHOc, 2020) coronavirus (COVID-
19) that provides insights on how healthcare has to
cope with one of the most contagious diseases that hit
mankind in the past decades. COVID-19 is not the
first and certainly not the last of these viruses. During
a public health crisis, it is important to provide regular
care to people at a distance. COVID-19 certainly
fueled the need for new tools and practices for
healthcare digitalization to provide care to people
away from the hospital settings.
Digitalization in healthcare to support self-
management is not a new concept. Digital health is
playing a pivotal role to support healthcare by
Sulaiman, M., Håkansson, A. and Karlsen, R.
A Framework for AI-enabled Proactive mHealth with Automated Decision-making for a User’s Context.
DOI: 10.5220/0010843200003123
In Proceedings of the 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2022) - Volume 5: HEALTHINF, pages 111-124
ISBN: 978-989-758-552-4; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
111

transforming existing practices (Hermes, Riasanow,
Clemons, Böhm & Krcmar, 2020). It contributes to
promoting health by providing tools to empower the
user (FDA, 2021). Digital health also incorporates
mobile health (mHealth) to provide healthcare
services using mobile and wireless technology.
mHealth combines wearables to render health
services to anyone, anywhere at any time (WHOd,
2018). This ubiquitous notion is the key in mHealth
to deal with health delivery constraints like location,
time, and cost. mHealth and wearables market is
growing and is estimated to reach 149.3 billion USD
by 2028 (GRAND View Research, 2021).
mHealth facilitates the paradigm shift in self-
management by providing tools to the users, so they
can become more aware and conscious about their
health. The user-centric approach can empower the
user by providing new insights into the health
information gathered from wearables and mobile
devices. These devices that users carry at all times,
and the collected health information they generate
provide the need for user-level decision-making.
The reactive approach in health is to act when a
crisis occurs with damage control (Amir, 2019). It is
practical in many circumstances, but it diminishes
health promotion and self-management. Proactive
health, in contrast, is to act before a crisis to predict and
prevent a situation promptly (Sharma, Singh Aujla &
Bajaj, 2019). Proactive health promotes wellbeing by
empowering the user and making them aware of an
anomaly beforehand. The active participation of the
user in their health enables more health information.
Proactive health can promote wellbeing, so the
ultimate goal of proactive health is to be predictive and
preventive with personalization. The system should
account for the uniqueness of the user. This can enable
care for the user ubiquitously but can also save lives
and support the healthcare system.
To develop proactive health with the principles of
prediction, prevention, and ubiquitous health
Artificial Intelligence (AI) with mHealth can play a
pivotal role. Many different definitions of AI are
available over the decades that serve well for many
use cases. IBM defined AI as "artificial intelligence
is a field, which combines computer science and
robust datasets, to enable problem-solving. It also
encompasses sub-fields of machine learning and deep
learning, which are frequently mentioned in
conjunction with artificial intelligence. These
disciplines are comprised of "AI algorithms which
seek to create […] systems which make predictions
or classifications based on input data (IBMa, 2021).
This definition serves well for enabling AI in
proactive health.
Wearable and mobile devices which the user
carries, have many sensors to collect health data,
which can be the key for finding patterns and making
accurate predictions for early intervention. AI can
apply reasoning and negotiation to the gathered data
to automate processes and facilitate decision-making.
This paper explores the fundamentals of AI-
enabled proactive mHealth by a comprehensive study
for the framework, challenges in design and
implementation of a system with automated decision-
making. The paper also presents the implementation
goals, and a model with an architecture for developing
AI-enabled proactive mHealth based on the proposed
framework. The result is a proof-of-concept that
renders an implementation view of the system with
technical aspects of design steps, goals, and a proposed
input/output mapping with the architecture. The paper
will provide the basis for further development of AI-
enabled proactive mHealth.
2 RELATED WORK
Proactive mHealth is to predict and prevent a
situation beforehand. A system that can provide
proactiveness must have a clear goal to predict and
prevent. The level of proactiveness when it comes to
proactive mHealth is broad. A basic level of
proactiveness provides benefits of being proactive to
manage a disease, a medium level corresponds to
being predictive, and a high level of proactiveness
allows a system to be predictive and preventive. Some
studies (McConnell et al., 2018; Aguilera et al., 2020;
Korpershoek et al., 2020; Baig, 2017) presented a
basic level of proactiveness, and the benefits of being
proactive. These are targeted for a specific need to
self-manage the disease. Hence, they are not adaptive
to new situations which require more level of
proactiveness. A few studies (Aguilera et al., 2020;
Baig, 2017) focused on managing a chronic disease
proactively.
A study (Nag, Pandey & Jain, 2017) presented the
importance of proactive health and significance by
giving a health map example. The health-map has
states of the user drawn in form of a map.
A few research studies (Dijkhuis et al., 2018;
Baig, 2017; Rojas & Dey, 2019) used wearables as
data sources but with activity data only. Activity data
can be useful for promoting health but when it comes
to providing prediction activity. A study (Baig, 2017)
concludes wearables as a key in providing health for
anyone at any time. Another study (Menictas, Rabbi,
Klasnja, & Murphy, 2019) highlights the importance
of decision-making with mHealth.
HEALTHINF 2022 - 15th International Conference on Health Informatics
112

2.1 Applications of AI in mHealth
AI is one of the factors driving healthcare towards
digitalization. It represents several technologies that
enable machines to sense, comprehend, act, and learn
(Matthew & Richard, 2021). The booming increase in
generated data today (Statista, 2021) has fuelled the
need for AI to support and automate healthcare
dilemmas. Some examples of domains where AI
contributes are administrative workflows, fraud
detection, dosage error detection, diagnosis
assistance, virtual assistance, decision-support,
automated processes, drug discovery, personalized
treatment, disease screening and early detection
(Matthew & Richard | Accenture, 2021). These
application areas provide the basis for the framework
of AI-enabled proactive mHealth.
mHealth application and available wearables data
have proven another domain where AI is
contributing. Many studies have used mHealth with
AI, a review (Naseer Qureshi, Din, Jeon & Piccialli,
2020) presented mHealth applications that use
machine learning. People are becoming more aware
of their health. Statistics show that 62% of
smartphone owners search the internet for health-
related information (Smith | Pew research, 2015).
Estimation indicates that about 80% of mHealth
applications will use AI by 2025 (Ghazaryan, 2021).
However, not all websites contain the correct
information, and an AI system shall be able to filter
out the non-correct parts and provide information
about the valid and trustworthy websites.
Some use cases (Ghazaryan, 2021) of mHealth
with AI are prediction models, personalized
treatments, early detection, recommender systems,
screening, and triage, and chatbots. For the
framework some of these use-cases are included.
mHealth with AI can support users in decision-
making to promote health. mHealth is beneficial
because of the features it provides e.g.,
personalization and ubiquitousness. It is utterly
necessary to account for the uniqueness of the user,
handled by user preferences. Table 1 presents some
mHealth applications and their features.
Table 1: mHealth applications.
Purpose Features
Diabetes control (Curran,
Nichols, Xie & Harper,
2010)
The paper focuses on
adjusting insulin levels
using mHealth
Activity (Yom-Tov et al.,
2021
)
The aim of the study is to
p
romote walkin
g
Blood pressure level
(Toro-Ramos et al., 2017)
The aim of the study is BP
monitoring
The related work provides the effectiveness of
being proactive but in the context of self-managing
the disease. There is no prior research that defines
proactive mHealth with AI with the capabilities of
prediction and prevention. A system to predict and
prevent a situation promptly, targeting a user for
promoting wellbeing before becoming sick. Such a
system can consider multiple parameters of wellbeing
i.e., environment or surroundings and current state of
the user. The critical analysis determines that AI in
mHealth is rapidly growing, but with a focus on
monitoring and self-management which depreciates
proactiveness.
3 USER-LEVEL
DECISION-MAKING FOR
SELF-EMPOWERMENT
Decision-making is the process that can have an
impact on our lives (Steph | Medium, 2020).
Decision-making requires time and effort to
comprehend details, make decisions on knowledge at
hand, plus decision alternatives to choose from based
on the circumstances. Effective decision-making
requires a step-by-step approach. One strategy
proposes a seven-step model for effective decision-
making (Dartmouth, 2021). The steps are as follows:
to identify the decision, collect information, identify
alternatives, weigh the evidence, choose among
alternatives, take action and finally, review the
decision.
Decision-making in healthcare often involves
several stakeholders in this process, such as doctors,
and nurses. Most health-related decisions are said to
be in the grey area of decision-making
(Abbasgholizadeh Rahimi, Menear, Robitaille &
Légaré, 2017). The grey area represents the scenario
where there is no right or wrong approach. Health-
related decisions can be critical with life-threatening
impacts for the users. Thus, there is a need to have
more informed choices and insights on the patient to
help with effective decision-making. mHealth is
contributing to this process by engaging patients in
decision-making to support health professionals with
new insights.
Most of these mHealth solutions are decision-
support systems for clinical decision-making. This is
an approach where the system supports evidence-
based decision-making. These solutions are crucial,
and many healthcare professionals rely on them to
provide shared decisions by having a combined
A Framework for AI-enabled Proactive mHealth with Automated Decision-making for a User’s Context
113

opinion between the healthcare professional and the
mHealth solution (Abbasgholizadeh et al., 2017).
These shared decisions are indeed beneficial
although, this diminishes the fact that many decisions
are taken at the user level (Krist, Tong et al., 2017).
The health decisions or health choices can have a
direct impact on their health, i.e., prevent disease,
prolong life, and promote wellbeing. Table 2 presents
the types of decisions that can have an impact on the
health of a user and the contributors involved in this
decision-making. mHealth and wearables are being
used by users all the time. There is new health
information about the states of the user that is
dynamic and can provide health data required for
decision-making. The table has two columns, first
column provides a case of decision-making. The
following column renders detail about contributors in
making that decision.
Table 2: User-level decisions with contributors’ example.
Cases for decision-
making
Contributors involved in
decision-making
From Air quality index
(AQI = 157), the user
profile (asthma), The air
quality tomorrow is
unhealthy. You are in a
risk group, stay home or
wear a mask when you go
out.
Sensors, mobile and the
user
Low activity, the user
profile (goals), You are
not very active lately. The
weather is pleasant today,
have a walk for ten
minutes.
Wearables, sensors,
mobile devices, and the
user
The pollen count, User
profile (have pollen), The
pollen count will be
higher tomorrow. You are
in a risk group, stay home
or wear a mask when you
go out.
Meteorological data,
user profile, mobile
device
These decisions cases are significant for a person
since they are not part of the clinical decision-making
approach that requires a doctor to examine but must
be handled by the user. Let us consider the case of a
user called “A” that is wearing a sleep tracker to sleep
every day. The information from that tracker can lead
to choices that user can take to improve his/her health.
These decisions are taken by User-A at the user level
and can promote health.
4 THE CONTEXT OF THE USER
The user’s context is "the interrelated conditions in
which something exists or occurs" (Merriam-
Webster, 2021). Context is important when providing
proactive mHealth because it consists of parameters
that can have a direct impact on the health of the user.
Many different circumstances e.g., environment,
surroundings, and user-profiling contribute to the
context. To emphasize, consider an example of a
system that can predict a health issue – atrial
fibrillation. Which is a heart condition that causes an
irregular heart rate. The system must include every
attribute about the user, family history, disease
history, current and previous states from the
wearables and sensors and user-profiling with user
characteristics. A context is anything relevant, can
have an adverse impact on health.
A context-aware system must be able to collect
information about surroundings and adapt to the
environment. Forming a context is vital because it
considers the uniqueness of the users and more
information on the states of the user. To define the
context, it is required to determine the target person
by choosing a user or group.
A user’s context accounts for user characteristics
and profiling. For someone who is suffering from
asthma caused by an inflammatory reaction
(Djukanović, 2021) the context of air pollution shall
be included.
Moreover, for a user in a risk group of infectious
disease it is essential to know about an outbreak of flu
or the rise of a number of flu cases in the area. In
contrast, for a specific group of people in risk groups
like the elderly or multi-disease, the context of flu
spread can be the same. In addition, a storm warning
can have a similar impact on everyone in the area.
The context can be elaborated and defined in many
ways, but the limitation comes to what is measurable
from the sensors and other sources and what can be
predicted and prevented. The context can also include
another person in the surroundings, i.e., one infected
person can infect another person. In the same way, a
driver on the road who suffers from a heart problem or
epilepsy can be a threat to the nearby surroundings. But
this is not measurable or predictable, in the current
systems. With the usage of the Internet of Things, IoT,
and autonomous vehicles, it can be a possibility to
provide solutions for measuring and predicting failures
and epileptic seizures.
Context is dynamic with ever-changing
surroundings. A system must be adaptive to cope with
the dynamic changes in context. A person suffering
from a pollen allergy shall have as context the amount
HEALTHINF 2022 - 15th International Conference on Health Informatics
114
of pollen in the environment, which is fluctuating over
time. Everything that can have an impact on one's
health, shall be part of the person’s /user’s context.
With the above-mentioned definition of context, it
is assumed to have different attributes e.g.,
environment, surroundings, user-profile, and
characteristics. The table shows several parameters,
used for developing the context and how they are
related to a user.
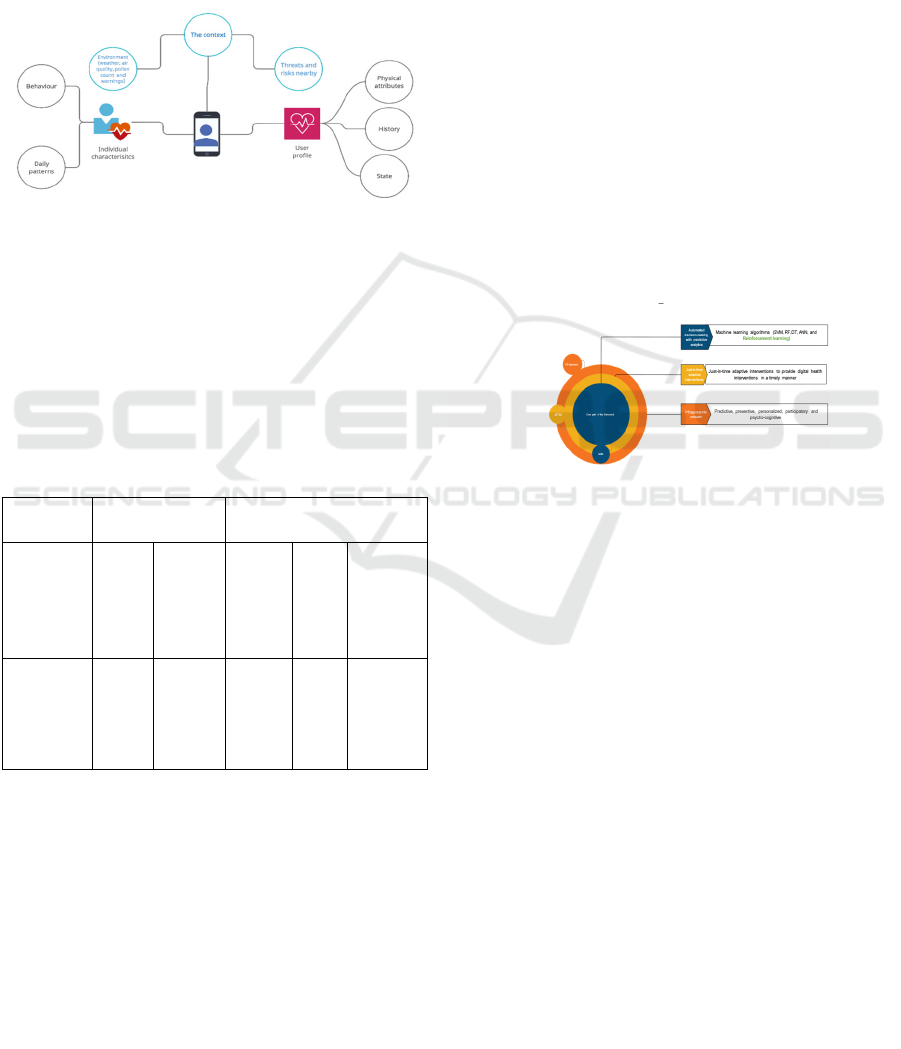
Figure 1: The context of a user.
An example of a user’s context is presented with
details on what it holds. The figure, Figure 1, shows
how a user’s context can be and what parameters it
includes. The center of the figure displays a user with
a user profile. Different parameters that form the
context are presented: user’s profile, characteristics,
environment. Table 3 demonstrates each parameter in
detail.
Table 3: Parameters for a user’s context
The context
User characteristics User profiling
Environment
(anything
that is
around and
can have an
impact)
Daily
patterns
Behaviour Physical
attributes
History
State
Weather, air
pollution,
threats, and
outbreak
Physical
activity
Screen
time
To adapt,
actions
and
behaviour
BMI
Allergies
Weight
Family,
Disease
Location,
Health
information
,
Activity
data, SpO2,
and feve
r
These parameters require multiple data sources as
input to the system. In section 5, a comparison of
available resources with the parameters of the context
is established.
5 THE FRAMEWORK OF
PROACTIVE mHealth
A framework provides the supporting structure
(Cambridge, 2021) to support building software. The
specified framework provides abstraction, which
supports the development of systems over it. The
framework also defines a set of rules to follow when
developing applications.
A conceptual framework defines concepts
collected after extensive research into a topic. A
definition of the conceptual framework is a
"conceptual framework as a network, or a plane, of
interlinked concepts that together provide a
comprehensive understanding of a phenomenon or
phenomena" (Jabareen, 2021). It is essential to
understand the link between these concepts.
This paper presents, a framework of AI-enabled
proactive mHealth. The framework is derived from a
systematic literature review of the topic and existing
systems. To show proof-of-concept, each part of the
framework is defined with examples and use-cases.
Following are the components of the framework:
Automated decision-making with predictive
analytics
P5 approach to mHealth
Just-in-time adaptive interventions
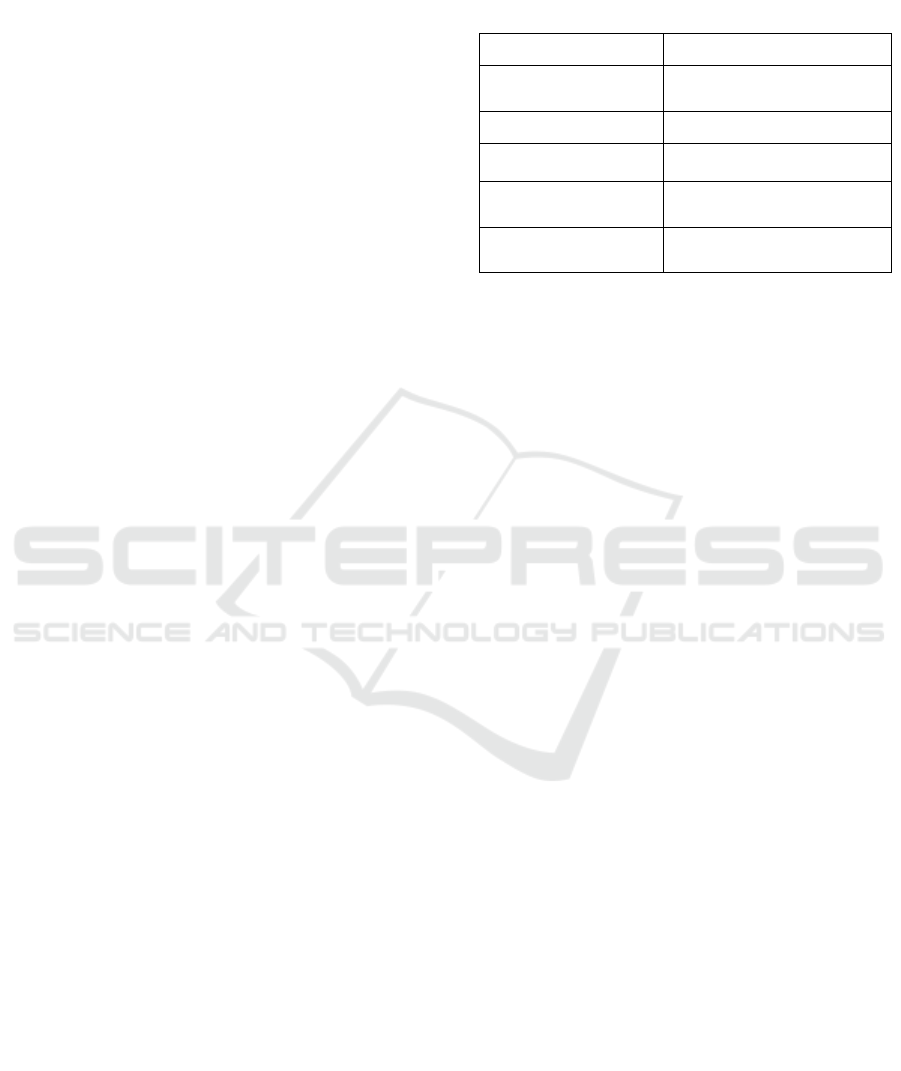
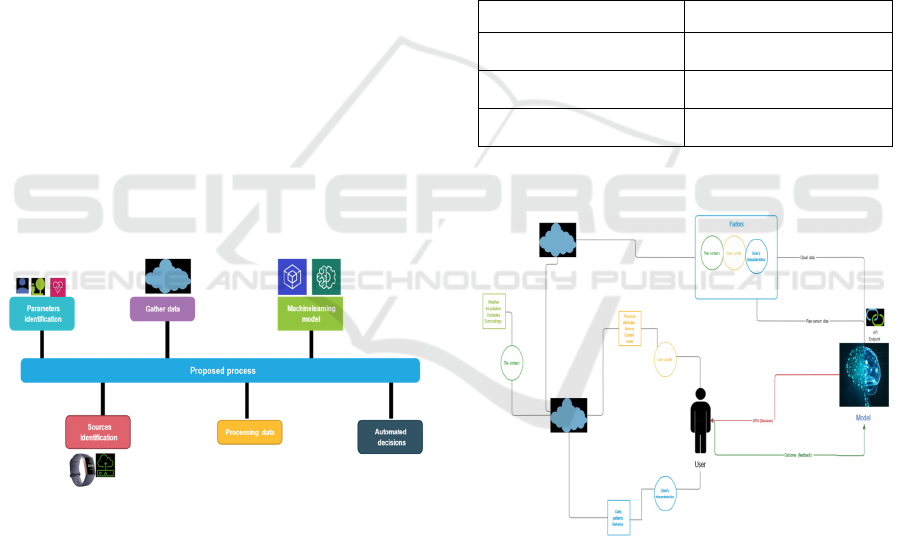
Figure 2: Proactive mHealth framework.
Figure 2 shows the components of the framework:
AI with automated decision-making, Just-in-time
adaptive intervention, and the P5 approach to
mHealth. Each component has variables with relation
to other components.
5.1 Automated Decision-making with
Predictive Analytics
Automated decision-making (ADM) with predictive
analytics is defined as “decisions by technological
means without human involvement" (EDPB, 2021)
recognizing patterns from extensive information to
provide decisions (data-driven). Booming increase in
the amount of digital data and ever-growing AI,
decision-making is empowered to automated
processes (Saha, 2021).
The first step is to process information by
applying algorithms and making informed decisions.
ADM that is powered with predictive analytics can
gather, process, and model health information to
render an automated decision (Araujo, Helberger,
Kruikemeier & H. de Vreese, 2020).
A Framework for AI-enabled Proactive mHealth with Automated Decision-making for a User’s Context
115
As presented in section-3, user-level decision-
making with multiple use-cases and examples. The
emphasis on user-level decision-making proves to be
the basis of providing ADM for AI-enabled proactive
mHealth. A system must consider multiple factors as
input and adapt to sudden changes in the states but
eventually, the benefit for the user is to get an
automated decision from the system, which is valid
for the user. These automated decisions are a part of
the prediction and prevention mechanism to promote
wellbeing.
Machine learning algorithms such as random
forest (RF), decision trees (DT), regression models,
artificial neural networks (ANN) can contribute to
developing the engine for ADM. Choosing the
technique depends on the type of data and decisions
to provide to the user.
It is imperative to understand the types of
decisions. These automated decisions are for
predicting and preventing health issues to promote
wellbeing. The system does not provide clinical
decision-making and hence, cannot be used as one.
Some examples of automated decisions are:
The system predicts the air quality to be
unhealthy tomorrow, wear a mask.
High pollen in the area tomorrow you are in
the risk group, please use medication.
There is an outbreak in the area you are in the
risk group. Stay home stay safe.
These decisions are based on the parameters (user
profiling, context, and characteristics) of the user.
The decisions are provided as information to the user
to prevent a possible illness or health issue.
5.2 P5 Approach to mHealth
The P5 approach to mHealth is based on the P4
(Sagner et al., 2018) spectrum of medicine presented
as an extension to personalized medicine. It proffered
new insights into designing health systems to be more
vigilant in considering users’ uniqueness and
timeliness. The spectrum is described as predictive,
preventive, personalized and participatory.
There have been many additions to this P4
spectrum. A P5 approach was presented (Gorini et al.,
2018) that added a P as Psycho-cognitive to provide
more details on the user’s decision-making regarding
their health. P5 approach to mHealth is relevant
because of the capabilities of mHealth to provide
more information about the user and a platform to
observe timeliness.
Table 4 illustrates the P5 principles for designing
health systems in detail. The 5 P’s are predictive,
preventive, personalized, participatory, and psycho-
cognitive.
Table 4: P5 Approach to mHealth (Gorini et al., 2018).
5 Ps Definition
Predictive
Allowing a precise prediction
about the future state
Preventive Timely preventive interventions
Personalized The uniqueness of the user
Participatory Not as passive recipients rather
active decision-makers
Psycho-cognitive Improving the ability to make
decisions
AI-enabled proactive mHealth system must
adhere to this design principle to be more effective for
the users. These design principles are part of our
framework of AI-enabled proactive mHealth.
The order of these principles or implementation
depends on the use case at hand or the targeted
outcome of the application. A motivating factor is the
availability of resources and tools to implement that.
With AI and the availability of wearable devices,
most of the health can be gathered for a more precise
targeted outcome. The design implementation can be
at different levels as well. Personalization can be
achieved for a user by targeting user preferences, but
at a community level, it depends on the characteristics
of the society.
5.3 Just-in-Time Adaptive
Interventions
Just-in-time adaptive interventions (JITAI) are based
on health interventions which are a way of providing
health services using mobile applications. Digital
health intervention aims to deliver information that is
useful for the user using digital platforms (Soobiah,
Cooper & Kishimoto, 2021).
Interventions are categorized as nudges, boosts
and recommendations (Hertwig & D Ryall, 2020). A
nudge is defined as "A nudge is an aspect of the
choice architecture that alters people's behavior in a
predictable way without forbidding any options or
significantly changing their economic incentives"
(Osman, 2016). A boost differs as its objective is to
improve someone's ability to make their own
decisions (Hertwig & D Ryall, 2020). In this study,
the focus is not on the behavioral science aspect of
these interventions. The property relevant to the
framework is the importance of interventions and
their impact.
HEALTHINF 2022 - 15th International Conference on Health Informatics
116
The focus of the framework is on the architecture
of digital interventions that can provide timely
interventions to the user but with adaptive behavior.
The Just-in-time adaptive intervention (JITAI) is an
intervention design that provides the right type of
support at the right time, by adapting to one's varying
internal and contextual state (Nahum-Shani et al.,
2017). JITAI intervention design focuses on 3
principles that are more of a challenge when it comes
to implementing JITAI.
When: When to intervene
What: What information to provide
Whom: To whom, the target user receiver of
the intervention
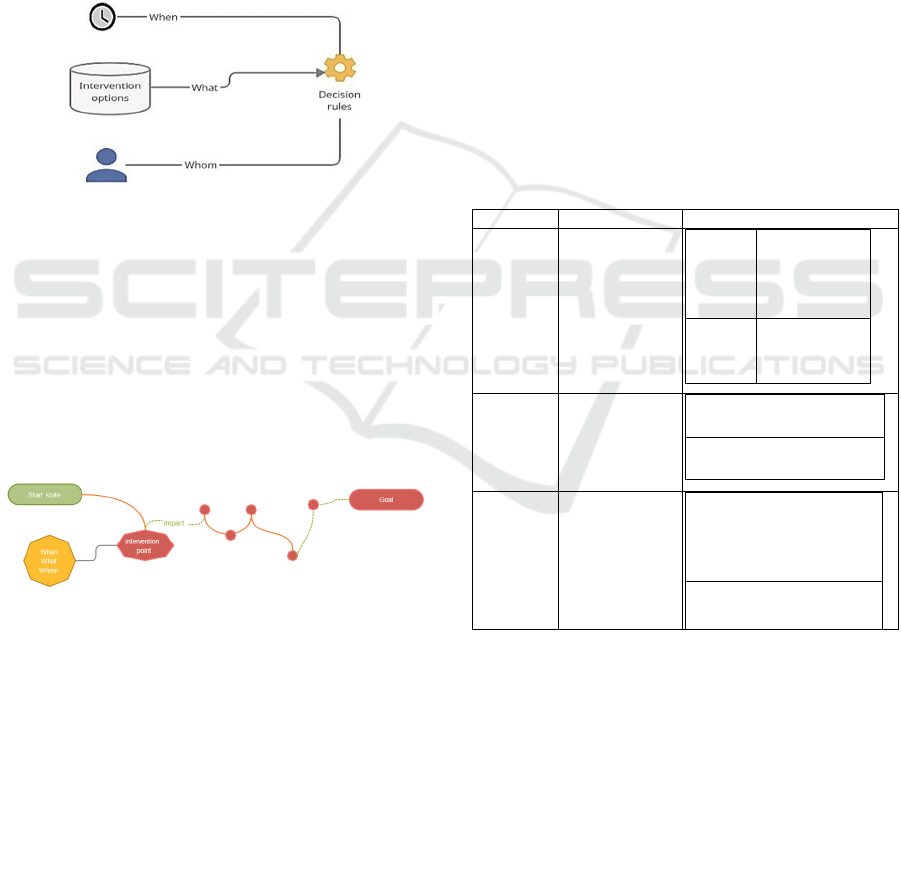
Figure 3: JITAI intervention points (Nahum-Shani et al.,
2017).
Figure 3 shows JITAI intervention points: when
in time, what intervention options, to whom who is
the target user and decision rules. An AI-enabled
proactive mHealth system must adhere to these
principles to provide timely interventions. That also
means it is necessary to understand the current state
of the target user before providing interventions. The
term internal and contextual state refers to the current
state of the user as well as its context.
Figure 4: Health map JITAI intervention points.
Figure 4 shows the health map, to highlight the
use of JITAI benefits for health promotion. The start
state represents the state of the user. The goal state is
the state representing goal. The intervention point is
a user-level decision required to change the state of
the user. The impact after this intervention is
displayed with an ascent in green.
6 IDENTIFICATION OF
SOURCES: WEARABLES,
SENSORS, AND AVAILABLE
RESOURCES
Identification of data collecting sources is the first
step in developing an AI-enabled proactive mHealth
system using the framework. The parameters that
provide health information about the user and its
context must be gathered as input. Most importantly,
information about the current state of the user is
crucial when providing JITAI.
Several different resources shall be included for
information collection to provide a holistic view of
the user’s preferences and current health. Table 5
provides some details about the most commonly used
sources and features they offer. The first column
identifies different sources, the second column
features list the detail of each. Finally, the listed
factors match what to collect from each source.
Table 5: Sources with features and factors.
Sources Features Factors
Wearables activity data SpO2
(oxygen
saturation), heart
rate, body temp,
Physical activity
and Screen time
(inactivity time)
User
profile
User
characteristics
Current
state
Daily patterns
Sensors Weather, Air
pollution
Context
Environment/Surroundings
Available
sources
Outbreaks,
Threats, risks in
the nearby area.
Pollen, Storms,
cyclone, and
avalanche
Context
Environment/Surroundings
In this paper, sources are categorized as
wearables, other sensors, and available resources.
Each source is examined with an example to collect
data necessary to build a holistic view of the user, but
also the challenges it possesses
6.1 Wearable Devices
Wearable devices have sensors that the user wear, are
portable, comfortable, and can collect data, which are
combined to produce information (Wu & Luo, 2021).
A Framework for AI-enabled Proactive mHealth with Automated Decision-making for a User’s Context
117
These devices also provide data even when they are
not being used (running in the background).
Another definition of wearable technology is
“seamlessly embedded portable computers … worn
on the body” (Janet, 2016). In health, wearables are
adopted as e.g., fitness trackers, biosensors, and smart
health watches (Janet, 2016).
Some key features (Bove, 2019) that wearable
provides are: Accelerometer, Altimeter,
Electrocardiogram, Location GPS, Microphone,
Oximeter, Thermometer, Pressure, and Stress.
Table 6 shows common fitness trackers (Fitbit
charge 4, Garmin Vivosmart 4, OURA Ring, Polar
M430, and Mi band 6) with their features.
Table 6: Wearables with features: a comparison.
Fitbit Charge
4
Garmin
Vivosmart
4
OURA Ring Polar
M430
Mi band 6
Activity
tracking,
GPS,
Continuous
heart rate,
breathing
rate, Stress
management
score, SpO2,
Skin
temperature,
sleep and
inactivity
Activity,
Sleep, heart
rate
measureme
nt and
inactivity
Sensors:
accelerome
ter,
pedometer
Activity,
Steps,
Inactivity
time, heart
rate, body
temperature
and sleep
Sensors:
acceleromete
r, optical
heart rate
monitor
Activity,
Sleep,
heart rate
measurem
ent and
inactivity
Sensors:
accelerom
eter,
optical
heart rate
monitor
Activity
tracking,
GPS,
Continuous
heart rate,
Stress
management
score, SpO2,
sleep and
inactivity
time
Data produced by these wearable devices can be
collected and used for AI-enabled proactive mHealth.
Unfortunately, the interoperability challenges
between vendors complicate this data collection
process. Most modern wearable sensors provide their
software development kit (SDK). An SDK is a set of
tools and programs made available by the vendor for
developers to work on. It provides several APIs for
the developers to use. Although it is a challenge when
it comes to data collection and having different
sensors connected to a single platform.
Vendors are working on solving the problem with
the non-compatibility of wearables, and there have
been many recent developments in this. For a clear
view of the compatibility problem, a comparison is
drawn between two of the vendors and the SDKs they
provide. Tables 7 present a comparison between
Google Fit and Apple HealthKit in terms of systems
and options available and data transfer options.
Table 7: System and options available (De Arriba-Pérez et
al., 2016).
Platforms SDK-
Sensors
SDK-
Warehouse
REST API
Apple
HealthKit
Google Fit
For storage, Google Fit provides warehouse and
cloud services with an SDK for developers. It also
provides REST API for third-party systems, a very
beneficial feature for to getting endpoint access.
Another essential feature is access to raw sensor data.
It is vital when real-time data from the user is needed.
An example of this is to use Sensor API for access to
raw sensor data in Google Fit.
The Apple HealthKit does not provide direct data
access to the wearable or the warehouse. The only
way is to access data by a query. A REST API service
is not provided which must be built first to store or
retrieve desired data.
Choosing the wearables for AI-enabled proactive
mHealth depends on the following factors: what we
want to measure, what is essential and what features
we can use.
6.2 Other Sensors
To collect real-time information about the context
more information from sensors is needed. A proposed
project can use the following setup to render
information.
A microcontroller: Arduino Uno Rev3
(Arduino, 2021): It is based on ATmega328P,
has 14 digital input/output pins, a 16 MHz
ceramic resonator.
Sensor: MQ-135 (Winsen, 2021): It is a
semiconductor sensor to measure air quality, it
is widely used as an alarm.
Sensor: BME 280 (Bosch, 2021): It is an
environmental sensor that measures humidity,
pressure and temperature.
Sensor: PM 2.5 (Adafruit, 2021): It is an air
quality sensor that measures air quality in real-
time.
For AI-enabled proactive mHealth to adapt to
real-time context, it is imperative to use these sensors
together to aim an overall view of surroundings.
6.3 Other Available Resources
To make accurate predictions, historical data of
context is required, i.e., air quality data from previous
HEALTHINF 2022 - 15th International Conference on Health Informatics
118

years can contribute to early detection. These
historical data can contribute to an early detection of
an outbreak. Cities or communities already provide
datasets for their environments. For example,
metrological data provide information measured with
different parameters regarding the environment,
including weather data, warnings data, temperature,
outbreaks, and cyclones. The predictions using these
resources are possible by training and modelling
systems.
This metrological data, combined with other
sensors and wearables cover the need for AI-enabled
proactive mHealth. A system must consider using
multiple parameters as input to provide automated
decision-making to the user.
7 CHALLENGES
To establish AI-enabled proactive mHealth many
challenges must be tackled.
One challenge is the complexity of being
proactive. In terms of implementation or design, it is
difficult for defining proactive. As discussed, the
system must consider multiple parameters, i.e.,
environment, surroundings, user profile, and
characteristics, but it makes the system more complex
when not every parameter is relevant for automated
decision-making. Another challenge is the
availability of these various parameters. To address
this issue a clear target must be considered. For
example, if a system is to provide timely intervention
to support a user at the right time, the system must
alert the user and show if it is safe to go outside or not
before the user leaves the house. The goal reduces
complexity to exclude data as not relevant for the
moment. For example, sleep data is not applicable for
air quality. Hence, it is to use the right, proper data at
the right time and for the right purpose. In the case of
air quality, it is data from the city's sensors that have
collected information about the current air quality, the
user's existing health information like asthma and
user preferences like personal acceptance of the air
quality in the surroundings outside the house.
Another challenge is to understand the target of
AI-enabled proactive mHealth, that is if the target is
for a user or a specific population. The
implementation for a user must adhere to the
uniqueness of the user, choices, and patterns essential
to have an efficient system implementation.
One system challenge is the importance of human
behavior as a part when implementing a system. The
system must cope with user characteristics and adapt
to a healthy lifestyle. The system must adapt to
change in lifestyle and the actions that can impact
health. This requires the system to constantly get
feedback, as a feedback loop from the user to model
the behavior and capture user preferences. The
feedback shall not require the user to provide
information manually. Rather, the systems shall learn
from how the user act, in a situation. For example, did
the user go out, although the system has alerted the
user about the bad air quality.
The timeliness of JITAI is an implementation
challenge, as well. A well-directed timely
intervention can save lives. Thus, a system must
handle precisions, i.e., when is the time for an
intervention with what type of information to the user
and finally, considering the user preferences when
providing this intervention.
Wearables and sensors provide great details into
real-time information, such as about the current state
of the user. Wearables and sensors indeed support the
timeliness principle of these interventions, since real-
time data is necessary to provide just-in-time
information to the user.
Using this real-time information is beneficial but
also a challenge when it comes to implementation.
Decision rules that include this information
simultaneously with the historical data are tricky to
implement because any sudden change must be
accepted by the model. Different viewpoints i.e.,
conditions that can suddenly change are a must for
designing decision rules with real-time data. Raw
data processing is another complicated process
because gathered data from sensors are to be filtered
before inclusion.
Sudden change in the context and user
characteristics is difficult to include in the system. It
produces a challenge of using real-time raw data with
historical data. So, the more information sources and
resources, the better the adaption mechanisms
because raw data must be filtered and processed
before inclusion. A system must update itself with the
incorporation of new information.
An added challenge is the evaluation of the system
and if it works, the accuracy of interventions and their
impact on health. It is beneficial to get feedback from
the user or a design principle where the system gets a
notification from the user, i.e., if they endure a
decision or not is beneficial.
Choosing the precise machine learning algorithms
depends on the available datasets. Many machine
learning techniques i.e., Support-vector machines,
SVM, decision trees, DT, and artificial neural
networks, ANN, are proven to be accurate. A system
must adapt to variations and the accuracy of the
predictions and preventions must be evaluated by a
A Framework for AI-enabled Proactive mHealth with Automated Decision-making for a User’s Context
119

defined evaluation mechanism to determine the best
model for the dataset.
In decision-making, it is very crucial to interpret
and provide transparency. But there is a trade-off
between automation and transparency. This
opaqueness and black-box system directly impact
trustworthiness. eXplainable AI (XAI) (IBMb, 2021)
can be applied to making AI techniques more
explainable. That is to have a system whose decisions
are understandable by humans.
Implementation of the system requires starting
from prediction, then moving towards prevention. So,
to promote the health of a user the system is built like
a stack.
a prediction that someone can become sick.
an action, i.e., activity or prevention for the
user (a personalized activity)
Feedback from the user, which becomes a new
input for the system.
User participation is a design principle called
participatory from the P5 principles of system
implementation, which is very complicated when
designing the system. The system must handle
usability, i.e., to make the system easy to use and
acceptable for everyone. The usability of the system
is about engaging the user to contribute to the system.
8 PROPOSED DESIGN AND
IMPLEMENTATION
The implementation goal is to adopt the framework
of AI-enabled proactive mHealth explained in Figure
2. The AI-enabled proactive mHealth system must
incorporate automated decision-making with
predictive analytics, the P5 approach for design, as
well as JITAI for providing interventions to the user.
Implementation of a system using the AI-
enabled proactive mHealth framework includes steps,
architecture, and processes.
8.1 Building Systems using the
Framework
The framework presented above, supports building
AI-enabled proactive mHealth systems.
8.1.1 Implementation Steps
The implementation phase starts with identifying
sources, then collecting relevant data, preparing data
for feature extraction, choosing the algorithms,
defining decision rules, training the model, and
making a prediction. Also matching the outcome with
an automated decision, and finally allowing feedback
for evaluation must be taken into account.
Identification of parameters: This step is
necessary when considering what to predict
and what attributes to include. For AI-enabled
proactive mHealth, the system must recognize
parameters of the context, user characteristics,
and user profiling.
Classifying sources: Another step is to look for
sources and resources for the parameters. For
the AI-enabled proactive mHealth system,
these are wearables, other sensors and
available resources.
Collecting data: Data collection is a challenge,
considering different heterogeneous sources.
In addition, information is required from the
user to provide intervention, such as, JITAI.
So, this step is significant to collect every
possible data from the available sources and
then provide a just-in-time module.
Preparing data: Data preparation is the step
where data is processed, to find duplications,
noise, distortion, and skewed data. Well-
processed and prepared data improves the
quality of the system.
Choosing the algorithm: Choosing the machine
learning algorithm is dependent on the type of
data that is available at this stage. Several
techniques can be adopted, i.e., Deep learning
(DL) for image and speech processing, and
reinforcement learning (RL) which enables an
agent to learn through actions in a specific
environment. RL can improve precision by
learning optimal decision rules, adapts and
adjusts to user preferences to enhance the
accuracy of the system.
Defining decision rules: Decision rules are
what make this system operational and reach
decisions. A better design is to adapt, though,
with more inputs, and the current state of the
user.
Training the model: In this step, algorithms are
applied to train the model by loading data and
get an outcome from the system.
Making a prediction: The outcome of the
model is the prediction that is interpreted and
processed to match a decision based on the
user. For example, a prediction that the air
quality will be unhealthy tomorrow.
Matching the prediction with an automated
decision: A processed outcome is matched
with a decision to provide the user with an
HEALTHINF 2022 - 15th International Conference on Health Informatics
120
automated decision on time. The prediction
that the air quality will be unhealthy tomorrow
will follow up with a decision to use an
antihistamine.
Feedback for evaluation: The system must
adapt to the user’s actions, i.e., behavior, by
automatically getting feedback from the user
on an intervention. The feedback is the user’s
action after an intervention. This feedback
works as an input to the system.
8.1.2 APIs Endpoints
The system shall have an API for sending requests
and receiving a response. Using an application
programming interface (APIs) enhances the system
effectiveness. The endpoint allows a layer or a system
to use this to build the applications. The endpoint
provides the following operations.
Receiving a request
Loading the model
Making the prediction
Sending back the response
It allows an application to use the operations
where information is added as input and an output is
a response from the model.
8.1.3 The Proposed Process with Steps
Figure 5: Proposed process with steps.
Figure 5 presents the proposed model with an
iterative approach from the parameter’s identification
on the left to automated decision on the right.
8.1.4 The Feedback Mechanism for Inputs
The outcome of a JITAI is feedback from the user. It
is used as an input to the system. This feedback is
either explicit or implicit:
Implicit feedback: This is the feedback is
automatically collected from the user based on
the decision provided to the user and the action
user takes. The health map provides a way to
gather implicit feedback.
Explicit feedback: It is the feedback provided
directly by the user of the system. The JITAI
must have a mechanism to collect the feedback
this. It can be a simple question to the user
regarding the intervention.
8.1.5 Features Important for Systems Built
on the Framework
Table 8 below presents other features that contribute
to the system strength. The features of a system are
robust, secure, and private. These features are
important for the system that is built on the
framework.
Table 8: Features of the system.
Features Definition
Robust The system must be robust
Secure It should account for the
CIA principle of security
Private User data must be private
8.1.6 The Architecture of the System
Figure 6: Architecture of the system.
Figure 6 presents the architecture of the system. The
figure is drawn in three segments, the user, AI-model
and sources with parameters (attributes). Cloud
presents storage of data from sources into two
sections, raw data, and historical data. This data is an
input for the AI model and is provided via an API
endpoint. The model then makes a prediction and
provides an automated decision in red to the user. The
outcome of this is feedback from the system to learn
from, presented in green.
A Framework for AI-enabled Proactive mHealth with Automated Decision-making for a User’s Context
121

8.1.7 Categorization of Interventions
In a proposed model, JITAI or automated decisions
can be categorized as Red, yellow, and green. Red-
colored intervention is critical and needs urgent
attention i.e., a vibration along with the intervention
to get the user’s attention. Yellow intervention does
not have an immediate effect, A green intervention is
an acknowledgement.
Figure 7: Categorization of interventions with examples.
Figure 7 presents some examples of this approach
using a mobile application screen. The colours
represent the type of intervention with notifications.
9 CONCLUSIONS AND FUTURE
WORK
In this paper, the impact of user-level decision-
making for AI-enabled proactive mHealth is
presented. The paper reasons the importance of
context for establishing proactiveness and provides a
framework of AI-enabled proactive mHealth. The
framework aims at providing insights into the design
and implementation goals of the system. This paper
also considers various implementation challenges.
The framework identifies the need for multiple
attributes as input and sources e.g., wearables,
sensors, and other resources. Finally, a system is
proposed based on the framework, which is adaptive
and provide timely interventions, JITAI architecture
with automated decision-making is fundamental for
the implementation. To this extent, the proposed
system considers multiple sources as input to provide
timely intervention to the user. This intervention is an
automated decision, which is built on the user’s
preferences. The outcome of the system is collected
implicitly or explicitly as feedback for ensuring
adaptiveness.
For future work, the system will be developed
using the proposed framework. The system will
adhere to the prediction and prevention mechanism to
provide timely intervention with personalization.
Multiple parameters will provide a holistic view of
the user. The implementation will be an AI engine,
which depending on the datasets and availability of
the features will handle different machine learning
algorithms for clustering and classifications. The
core part of the system depends on machine learning
techniques for providing an automated decision that
is beneficial for the user. The proof-of-concept model
can then be used for further developing an AI-enabled
proactive mHealth system.
REFERENCES
Winslow, C. (2021). Introduction to Public Health|Public
Health 101 Series|CDC. Cdc.gov. Retrieved 5 October
2021, from https://www.cdc.gov/training/public
health101
WHOa (2021). Health promotion. Who.int., Retrieved 5
October 2021, from https://www.who.int/health-topics
Haseltine, W. (2021). Aging Populations Will Challenge
Healthcare Systems All Over The World. Forbes.
Retrieved from https://www.forbes.com/sites/
williamhaseltine
NIPH (2018). Norwegian Institute of Public Health. Life
expectancy in Norway. from https://www.fhi.no/en/op/
hin/population
Atella, V., Piano Mortari, A., Kopinska, J., et al., (2018).
Trends in age-related disease burden and healthcare
utilization. Aging Cell, 18(1), e12861.
WHOb (2021). GHO. Global Health Estimates: Life
expectancy and leading causes of death and disability.
Who.int., from https://www.who.int/data/gho/data/
themes/mortality-and-global-health-estimates.
CDC (2021). Chronic Diseases in America, from
https://www.cdc.gov/chronicdisease/resources/infogra
phic/chronic-diseases.htm.
WHOc (2020). Director-General's opening remarks at the
media briefing on COVID-19 - 11 March 2020.
Retrieved from https://www.who.int/director-general/
speeches/detail/
Hermes, S., Riasanow, T., Clemons, E., Böhm, M., &
Krcmar, H. (2020). The digital transformation of the
healthcare industry: exploring the rise of emerging
platform ecosystems and their influence on the role of
patients. Business Research, 13(3), 1033-1069.
FDA (2021). What is Digital Health?. U.S. FDA. Retrieved
5 October 2021, from https://www.fda.gov/medical-
devices/digital-health-center-excellence/what-digital-
health.
HEALTHINF 2022 - 15th International Conference on Health Informatics
122

WHOd (2018). GoE. Who.int. Retrieved 5 October 2021,
from https://www.who.int/observatories/global-
observatory-for-
GRAND View Research. (2021). mHealth Apps Market
Growth & Trends. February 2021. Retrieved from
https://www.grandviewresearch.com/press-release/
Amir, M. (2019). The Shift from Reactive to Proactive
Healthcare | Blackcreek. Blackcreek.io. Retrieved 5
October 2021, from https://blackcreek.io/insights/the-
shift-from-reactive-to-proactive-healthcare.
Sharma, D., Singh Aujla, G., & Bajaj, R. (2019). Evolution
from ancient medication to human-centered Healthcare
4.0: A review on health care recommender systems.
International Journal Of Communication Systems,
e4058.
IBMa 2021. Education, I. (2021). What is Artificial
Intelligence (AI)?. Ibm.com. Retrieved 5 October 2021,
from https://www.ibm.com/cloud/learn/
McConnell, M., Turakhia, M., Harrington, R., King, A., &
Ashley, E. (2018). Mobile Health Advances in Physical
Activity, Fitness, and Atrial Fibrillation. Journal Of
The American College Of Cardiology, 71(23), 2691-
2701.
Aguilera, A., Figueroa, C., Hernandez-Ramos, R., Sarkar,
U., Cemballi, A., & Gomez-Pathak, L. et al. (2020).
mHealth app using machine learning to increase
physical activity in diabetes and depression: clinical
trial protocol for the DIAMANTE Study. BMJ Open,
10(8),
Korpershoek, Y., Hermsen, S., Schoonhoven, L.,
Schuurmans, M., & Trappenburg, J. (2020). User-
Centered Design of a Mobile Health Intervention to
Enhance Exacerbation-Related Self-Mgt in Patients
With COPD (Copilot): Mixed Methods Study. JMIR,
22(6)
Baig, M. (2017). Early Detection and Self-management of
Long-term Conditions Using Wearable Technologies.
Auckland University of Technology.
Nag, N., Pandey, V., & Jain, R. (2017). Health Multimedia.
Proceedings Of The 2017 ACM On International
Conference On Multimedia Retrieval. https://doi.org/
10.1145/3078971.3080545
Dijkhuis, T., Blaauw, F., van Ittersum, et al., (2018).
Personalized Physical Activity Coaching: A Machine
Learning Approach. Sensors, 18(2), 623.
Rojas, J., & Dey, A. (2019). The Personalization of Mobile
Health Interventions. Corpus ID: 208153767
Steph U. Medium. (2020). How do the choices we make
affect our lives?. In Medium.
https://stephup.medium.com/how-do-the-choices-we-
make-affect-our-lives-20f287487966
Dartmouth, U. (2021). Decision-making process. Retrieved
5 October 2021, from https://www.umassd.edu/fycm
Abbasgholizadeh Rahimi, S., Menear, et al., (2017). Are
mobile health applications useful for supporting shared
decision-making in diagnostic and treatment
decisions?. Global Health Action, 10(sup3), 1332259.
Matthew, C, Richard, F. Artificial Intelligence in
Healthcare | Accenture. (2021). from https://www.
accenture.com/us-en/
Statista (2021). Total data volume worldwide 2010-2025
|.from https://www.statista.com/statistics/871513/
Naseer Qureshi, K., Din, S., (2020). An accurate and
dynamic predictive model for a smart M-Health system
using machine learning. Information Sciences, 538,
486-502.
Smith, A. (2021). U.S. Smartphone Use in 2015. Retrieved
5 October 2021, from https://www.pewresearch.org/
internet
Araujo, T., Helberger, N., et al., (2020). In AI we trust?
Perceptions about automated decision-making by
artificial intelligence. AI & Society, 35(611-623).
Curran, K., Nichols, E., (2010). An intensive insulin
therapy mobile phone application built on artificial
intelligence techniques. Journal Of Diabetes Science,
4(1), 209-220.
Merriam-Webster (2021). Definition of context. (2021).
Retrieved 6 October 2021, from https://www.merriam-
webster.com/dictionary/context
Djukanović, R. (2021). Asthma: A disease of inflammation
and repair. The Journal Of Allergy And Clinical
Immunology, 105(2 Pt 2), S522–S526.
European Data Protection Board (EDPB). guidelines on
automated individual decision-making and profiling –
(2021).
Cambridge (2021). Framework. Retrieved 6 October 2021,
from https://dictionary.cambridge.org/dictionary/
english
Ghazaryan, A. (2021). Applications of AI and ML in 2021
mHealth. DZone.
Gorini, A., Mazzocco, K., Triberti, S., Sebri, V., Savioni,
L., & Pravettoni, G. (2018). A P5 Approach to m-
Health: Design Suggestions for Advanced Mobile
Health Technology. Frontiers In Psychology, 9(2066).
Hertwig, R., & D Ryall, M. (2020). Nudge Versus Boost:
Agency Dynamics Under Libertarian Paternalism. The
Economic Journal, 130
(629), 1384–1415.
Jabareen, Y. (2021). Building a Conceptual Framework:
Philosophy, Definitions, and Procedure. International
Journal Of Qualitative Methods, 8(4), 49-62.
Sagner, M., McNeil, et al. (2018). The P4 Health Spectrum
- A Predictive, Preventive, Personalized and
Participatory Healthspan. Progress In Cardiovascular
Diseases, 59(5).
Saha, D. (2021). How The World Became Data-Driven,
And What’s Next. Retrieved 6 October 2021, from
https://www.forbes.com/sites
Soobiah, C., Cooper, M., (2021). Identifying optimal
frameworks to implement or evaluate digital health
interventions: a scoping review protocol. BMJ Open
2020, 10.
Toro-Ramos, T., Kim, Y., et al. (2017). Efficacy of a mobile
hypertension prevention delivery platform with human
coaching. Journal Of Human Hypertension, 31(12),
795.
Yom-Tov, E., Feraru, G., Kozdoba, et al., (2021).
Encouraging Physical Activity in Patients With
Diabetes: Intervention Using a Reinforcement Learning
System. Journal Of Medical Internet Research, 19(10).
A Framework for AI-enabled Proactive mHealth with Automated Decision-making for a User’s Context
123

Bove, L. (2019). Increasing Patient Engagement Through
the Use of Wearable Technology. The Journal For
Nurse Practitioners, 15(8), 535-539.
IBMb (2021). Explainable AI IBM. Retrieved 6 October
2021, from https://www.ibm.com/watson/explainable-
ai
Winsen (2021). MQ 135 manual. Retrieved 6 October
2021, from https://www.winsensensor.com/d/files/
PDF/
Nahum-Shani, I., Smith, S, et al., (2017). Just-in-Time
Adaptive Interventions (JITAIs) in Mobile Health: Key
Components and Design Principles for Ongoing Health
Behavior Support. Annals Of Behavioral Medicine,
52(6), 446-462.
Osman, M. (2016). Nudge: How Far Have We Come?.
Oeconomia, (6-4), 557-570. doi: 10.4000/oeconomia.2
490
Adafruit 2021. PM2.5 Air quality sensor. (2021). Retrieved
6 October 2021, from https://cdn-learn.adafruit.com/
downloads/pdf/
Bosch (2021). BME280. Retrieved 6 October 2021, from
https://www.bosch-sensortec.com/products/
environmental-
Arduino (2021). UNO R3. Retrieved 6 October 2021, from
https://docs.arduino.cc/hardware/uno-rev3
Janet, H., (2016). Wearable Technology and Mobile
Innovations for Next-Generation Education. Advances
In Educational Technologies And Instructional Design.
Wu, M., & Luo, J. (2021). Wearable Technology
Applications in Healthcare: A Literature Review.
Retrieved 6 October 2021, from https://www.
himss.org/resources/wearable
Menictas, M., Rabbi, et al., (2019). Artificial intelligence
decision-making in Mobile health. The Biochemist,
41(5), 20-24.
De Arriba-Pérez, F., Caeiro, et al., (2016). Collection and
processing of data from wrist wearable devices in
multiple-user scenarios. Sensors, 16(9), 1538. MDPI
AG,
Krist, Alex H et al. “Engaging Patients in Decision-Making
and Behavior Change to Promote Prevention.” Studies
in health technology and informatics vol. 240 (2017):
284-302.
HEALTHINF 2022 - 15th International Conference on Health Informatics
124
