
Benefits and Limitations of Age Group-Adjusted Average in the
Profitability Audit for Pharmocotherapy
Reinhard Schuster
1,*
, Thomas Ostermann
2,†
, Timo Emcke
3,‡
and Fabian Schuster
1,4,§
1
Department of Health Economics, Epidemiology and Medical Informatics, Medical Advisory Board of Statutory Health
Insurance in Northern Germany (MD Nord), 23554 Lübeck, Germany
2
Department of Research Methodology and Statistics in Psychology, Witten/Herdecke University, 58448 Witten, Germany
3
Department of Prescription Analysis, Association of Statutory Health Insurance Physicians, 23812 Bad Segeberg,
Germany
2
Sigmund-Freud-PrivatUniversity SFU Vienna, Faculty of Law, 1020 Vienna
Keywords: Drug Prescriptions in Outpatient Treatment, Statutory Health Insurance in Germany, Sickness (Health
Insurance) SHI Funds in Germany, Morbidity Related Groups (MRG), Risk Structure Compensation between
the Health Insurance Companies (RSC), Gini Coefficients, Lorenz Curves.
Abstract: Benchmarks for pharmaceuticals have been used for over 25 years to limit the cost increase in the second
largest cost block in statutory health insurance in Germany with financial punishments for the physicians. The
Regional Social Court of Dresden declares such a payback practice to be inadmissible if no age reference is
used. In 2016, in most regions of the statutory health insurance associations, the division into status groups
members, family members and pensioners has been changed into four age groups. The Supply Strengthening
Act has opened up the possibility of drafting regional agreements. In Schleswig-Holstein, Morbidity Related
Groups (MRG) were introduced for morbidity-related considerations. A number of other regions are currently
using retrospective average cost limitations, which have the same problems as the benchmark restrictions.
The aim of this paper is to investigate the influence of the type of health insurance (sickness) fund on the
benchmark result with status and with age groups. Different morbidity structures between the health insurance
funds are the subject of the risk structure compensation. For doctors, this aspect is not given sufficient
consideration with respect to patient-specific morbidity characteristics till now.
1 INTRODUCTION
Drug prescriptions in outpatient treatment of SHI
(statutory health insurance) physicians are subject to
the economic efficiency requirement according to
German Law with respect to §§ 2 and 12 SGB V.
This means that all drug treatments that are provided
in the statutory medical practice must be sufficient,
appropriate and economical and that what is
necessary must not be exceeded. A control instrument
that has been used for a long time was the so called
“Richtgrößen” benchmark, cf. (Busse et. al., 2015),
(Bratzke et. al., 2012). Based on the average actual
situation in the SHI-insured groups M (members), F
*
https://md-nord.de
†
https://uni-wh.de
‡
https://kvsh.de
§
https://sfu.ac.at
(family members) and pensioners (R) as well as the
expenditure volume determined in negotiations
between the contracting parties (health insurance
companies and the Association of Statutory Health
Insurance Physicians), benchmarks were set for
assessing the drug expenditure. Depending on the
negotiation region, drugs were removed from the
restrictions if it should be assumed that their
prescription was not inefficient („Anlage-Präparate”,
“drug contract annex”). In December 2013, the
Dresden Social Court considered exams to be
unlawful because there were no age-related patient
groups. The Federal Social Court ruled in June 2013
that the review committees have a duty to investigate
atypical prescription cases. Since they had data on the
390
Schuster, R., Ostermann, T., Emcke, T. and Schuster, F.
Benefits and Limitations of Age Group-Adjusted Average in the Profitability Audit for Pharmocotherapy.
DOI: 10.5220/0010807500003123
In Proceedings of the 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2022) - Volume 5: HEALTHINF, pages 390-396
ISBN: 978-989-758-552-4; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

doctor to be examined and the comparison group,
they would have to investigate deviations and discuss
the reasons with the doctor. These judgments are a
step towards morbidity-related considerations, cf.
(Urt. LSG Sachsen-Anhalt, 2014), (Urt. BSG Juni,
2013), (Urt. SG Dresden, 2013), (GKV-Versorgungs-
stärkungsgesetz, 2015), (Gottwald, 2015), (Korzilius,
2015), (Sinowatz, 2015), (Wersborg, 2006). As will
be described in more detail below, there are data in
the big data environment, which results opportunities
and difficulties for doctors, negotiators and
examination boards.
In (Schuster et. al., 2016) the influence of the
changeover from the status groups to the age groups
0-15 years, 16-49 years, 50-64 years and 65 years of
the patients and over on the database 3/2014 - 2/2015
as a first calculation and a second calculation for the
first two quarters of 2018 for Schleswig was
examined. One way of assessing the fairness of the
changeover is to compare the subdivision only
according to status groups or only according to age
groups with a combined view. Morbidity-related
misjudgments that occur in the combined groups are
not recorded.
The combination of patient members and age
group 16-49 years, with 30.7% of patients, which is
the strongest combination among general
practitioners, is assessed by the age assessment
almost as in the combination of status group and age,
so that the age groups appear fair from a combination
perspective. But they lose 37% of their benchmark
drug volume according to status groups. In the third
largest combination group of members and ages 50-
64, this group was underrated by 29% according to
status group and 12% overrated according to age
group.
The comparison of the benchmark fulfillment
according to status and age groups results in a
correlation coefficient R^2 between 0.9724 for
pediatricians and 0.9999 for hematologists/
oncologists and rheumatologists, for the largest group
of general practitioners it is 0.9784. The rather rough
age division into only four groups had a much smaller
effect in terms of a fairer assessment than was
expected from the court judgments examined. The
main points of criticism in the grounds for the
judgment therefore remain.that papers in a technically
unsuitable form will be returned for retyping. After
returned the manuscript must be appropriately
modified.
In Schleswig-Holstein, the pharmaceutical
partnership agreement between the SHI physician
organization and the SHI funds for 2017 was changed
to Morbidity Related Groups (MRG), cf. Emcke
et.al., 2017), (Prüfvereinbarung, 2016), (Schuster et.
Al., 2017), (Schuster et. al. ,2016). The relationship
to morbidity is established on the basis of the
prescribed drugs and the active substance
classification (international ATC classification) and
not on the basis of the diagnostic data (international
ICD classification). The relationship between MRG
and ICD diagnoses is examined in (Schuster et. al.,
2017), (Schuster et. al. 2017). Diagnostic data are
only available on a quarterly basis, prescription data
according to Section 300 SGB V have a prescription
date. The diagnostic data differentiate between acute
illness and permanent diagnosis, but there is no main
diagnosis like in the inpatient area.
The active ingredient classification is based on the
international ATC (anatomical-therapeutic-chemical)
classification with national characteristics on the
basis of drug approval law. The MRG classification
has analogies to the Diagnoses Related Groups
(DRG) in the inpatient area, but does not serve to
reimburse medical services. For MRG, the patient and
his entire morbidity are the focus of considerations.
For each quarter and medical specialty, the drug
group at the level of the ATC four-digit code with the
highest costs is selected as dominating for the patient.
For all patients in this base group, it is considered how
age in 5-year steps, multimorbidity in the sense of
multi-medication and prescription intensity affect the
average costs in a comparison of specialist groups. On
this basis, a prospective guaranteed value for its
pharmaceutical expenditure is first determined for
each doctor. If the morbidity of the patients or their
number increases in the prescription year, the
guaranteed value will increase. With this approach,
particularities in practice are generally well captured.
A fair assessment is achieved if all doctors and all
patients are included in the evaluations. The MRG
concept for general assessment is supplemented by a
drug agreement in which specific control effects are
to be achieved in selected areas.
In the following, it will be examined to what
extent the morbidity differences occurring in the
types of health insurance funds influence the results
of profitability analyzes. This also includes the
question of the extent to which a doctor bears an
increased or decreased risk of exams due to the
different structure of the insurance type of the patients
with regard to the health insurance companies. In
order to counteract the different morbidity of the
insured persons, there is a risk structure compensation
between the health insurance companies (RSC). In
relation to a doctor, this has not been considered for
benchmarks and average values. In the MRG system,
such differences are taken into account in the case
Benefits and Limitations of Age Group-Adjusted Average in the Profitability Audit for Pharmocotherapy
391

groups. In contrast, morbidity differences are
essentially not taken into account in drug agreements.
Differences in the distribution are to be examined
with Gini coefficients for Lorenz curves.
2 MATERIAL AND METHODS
We analyze all treatments and prescriptions of
physicians for patients of the statutory health
insurance (SHI) by SHI physicians in Schleswig-
Holstein in the first and second quarter of 2018. The
datasets of all treatments and prescriptions of all
physicians with respect to a patient are used. The
dataset of the second quarter of 2018 covers around
1,700,000 patients with diagnoses and around
1,400,000 patients with drug prescriptions using a
pseudonymized patient identity with age, gender and
insurance fund information. We utilize the
International Statistical Classification of Diseases
and Related Health Problems [ICD]. The knowledge
of the total number of patients is a side-effect of the
diagnose statistic. The same diagnoses for the same
patient by different physicians are counted
repeatedly, if the analysis is aimed for drug economy
with respect to physicians, with respect to
epidemiologic analysis it can be more adequate to
analyze all diagnoses and treatments for a patient with
respect to all physicians. For prescription analysis the
International Anatomic Therapeutic Chemical (ATC)
classification system with German specifications
provided by the German Institute of Medical
Documentation and Information (DIMDI) is used.
Statutory health insurance (SHI) in Germany
through sickness funds is compulsory for workers
whose gross income does not exceed a certain level,
for unemployed and retired people, and for certain
other population groups (such as farmers, artists, and
students). Employees with incomes above the
threshold may be voluntary sickness fund members if
they have been members before. Around 88 percent
of the total population in Germany is covered by the
SHI (74 percent obligatorily and 14 percent
voluntarily).
Sickness (health insurance) SHI funds in
Germany are differentiated into the following types:
- general regional funds (Ortskrankenkassen
AOK)
- substitute funds (Ersatzkassen, VdEK)
- company-based funds (Betriebskranken-
kassen, BKK)
- guild funds (Innungskrankenkassen, IKK)
- farmers funds (Landwirtschaftliche
Krankenkassen, LKK)
- miners fund (Bundesknappschaft, BKN)
- sailors fund (See-Krankenkasse, SEE).
All funds have a not-for-profit status and are
based on the principle of self-government. Miners
fund and sailors fund are merged now.
To avoid having all insured people choose funds
with a low contribution rate because of a historically
good risk profile a risk structure compensation (RSC)
scheme was introduced on the level of funds. But a
risk compensation on the level of physicians with
respect to drug economic considerations which can
lead to paying-back regulations for the doctors was
not established.
The health funds and each regional association of
SHI physicians set target volumes for physicians in
each medical specialty in annual negotiations. These
correspond to the average prescription volume per
calendar quarter for each specialty which may be
done with prospective and with retrospective
considerations. SHI physicians who exceed their
individual target limit by more than 15% with
regional exceptions related to medicines and patients
may be advised in writing to critically reconsider their
prescription behaviour to the joint examination office
of the SHI association and the health insurance funds.
The SHI-limit for overprescribing and paying-back
has been set at 125% of the individual target. Those
physicians who exceed the target by 25% are asked to
justify the overprescription although this would
actually already be possible to a considerable extent
on the basis of the data records available in the
examination office. If their arguments are rejected,
they are subject to recourse and usually pay back the
difference between the overprescribed amount and
115% of the target.
In the discussion between the doctors and the
examining body, the doctors have a lack of
information because they know their own
prescriptions but not those of their specialist group.
Ideally, this is balanced out by joint advisory services
by the SHI association and the health insurance funds.
With regard to the doctors, this justification
procedure sometimes delivers very different results,
depending on whether one adjusts for status groups or
age groups. If you look at the more than half a million
different drugs according to the product designation
(pharmaceutical central number, PZN) and the widely
spread diagnosis according to ICD, in connection
with the specified number of patients, one can see that
it situated in the big data environment.
HEALTHINF 2022 - 15th International Conference on Health Informatics
392
The KM6 statistics of the statutory health
insurance companies describe the number of insured
persons at the annual mean. Population statistics are
based on the status at the end of the year. From the
difference between the two, one can deduce the
proportion of persons SHI-insured with a certain
degree of accuracy.
Costs per patients are used for benchmark
calculations and average value checks. The point of
reference here are the medical treatment cases, this
also includes those patients without medication
prescriptions, which can be calculated by the ICD
statistic. Alternatively, prescription patients (i.e. only
patients with drug prescriptions) or all SHI-insured
persons can be used, with advantages and
disadvantages. The choice of all patients as a
reference point is intended to support the limitation of
minor prescriptions. In the MRG system, the
prescription patients are the reference point. Since
comparisons are made based on morbidity, the
“thinner problem” (patents with few cheap drugs) is
not an obstacle due to regulations. In the case of
regional morbidity analyzes, the insured person's
reference (in relation to statutory health insurance,
GKV) is relevant. This is different from the
population reference. The information provided by
insured persons is available with the KM6 statistics
differentiated according to federal state and type of
insurance fund (insurance members in month 6,
middle of the year). Unfortunately, the reference
point is the middle of the year, as opposed to the
majority of population statistics which refer to the end
of the year.
The script languages gawk and perl were used for
the calculations. These were carried out for a joint
working group of the health insurance companies and
the Association of Statutory Health Insurance
Physicians with their drug billing data for the second
quarter of 2018.
3 COSTS PER CASE AND COST
SHARES ACCORDING TO
TYPE OF INSURANCE
Age information is only available for the age group 0-
14 and then in 5-year steps up to 89 years and a group
from 90. This means that the age and gender-related
share of statutory health insurance insured persons
can only be estimated with a higher resolution using
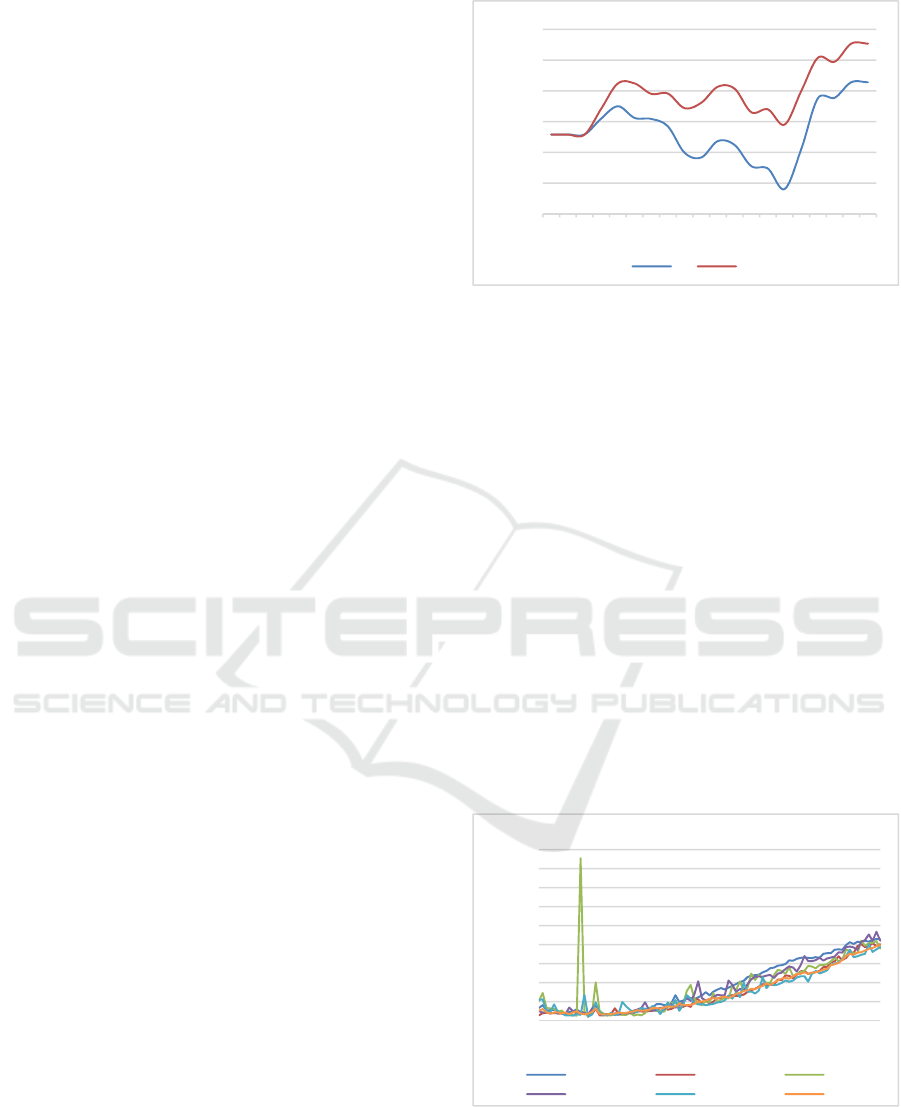
interpolation methods, cf. Figure 1.
Figure 1: Age and gender-dependent proportion of
GKV insured persons in Schleswig-Holstein (man = m,
woman = w).
There was a particularly high proportion of privately
insured persons in the low-birth year 1945, at the
height of the baby boom a (locally) minimal and then
at the point of the pill break again a (locally) maximal
proportion of privately insured persons. In connection
with the higher average social status of privately
insured persons compared with those with statutory
health insurance, a lower risk of morbidity is to be
expected. The gender-specific proportion of people
insured with statutory health insurance can also result
in differences in morbidity when looking at the
insured person or the number of cases. Population
models over long periods of time are considered in
(Schuster et. al., 2017).
Figure 2 gives an overview of the gender-
differentiated influence of age in annual resolution on
the average case costs for general medicine
depending on the types of insurance.
Figure 2: Case costs according to type of insurance.
70%
75%
80%
85%
90%
95%
100%
0 5 10 15 20 25 30 35 40 45 50 55 60 65 70 75 80 85 90 95
fraction
age
Statutory funds fraction
m w
0 €
50 €
100 €
150 €
200 €
250 €
300 €
350 €
400 €
450 €
0 5 10 15 20 25 30 35 40 45 50 55 60 65 70 75 80 85 90
cost
age
case costs
AOK BKK BKN
IKK LKK VdEK
Benefits and Limitations of Age Group-Adjusted Average in the Profitability Audit for Pharmocotherapy
393
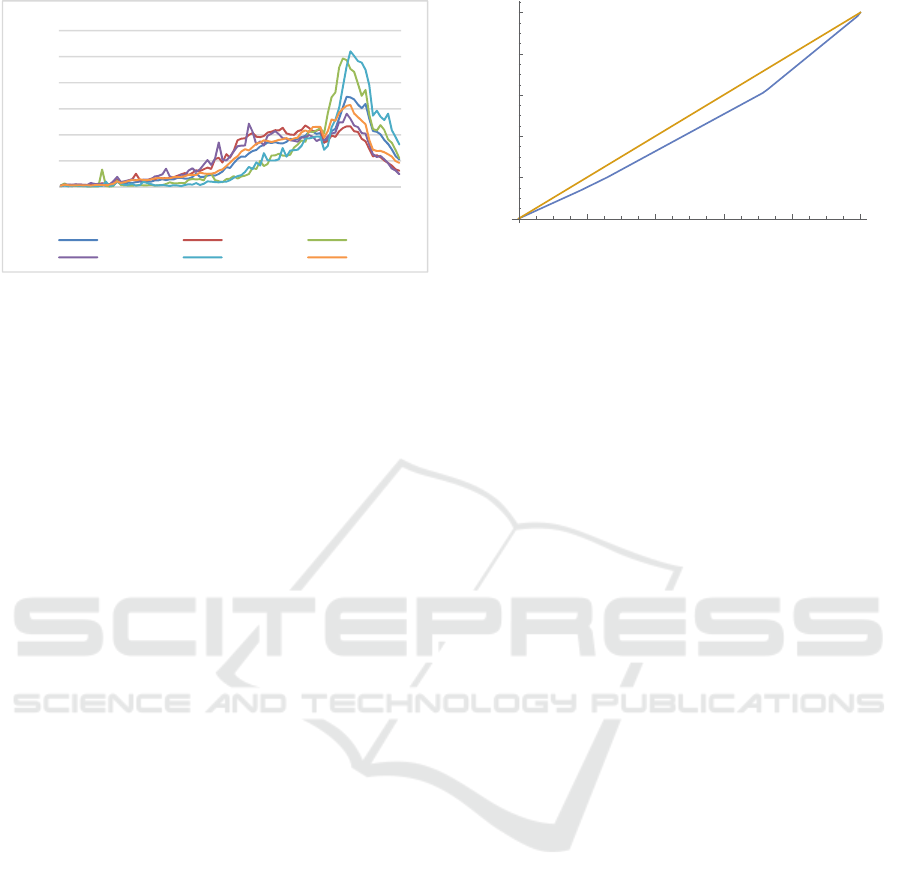
Figure 3: Number of cases according to health.
Figure 3 shows the number of cases that are
specific to the health insurance scheme, which
represent the age structures of the patients relevant to
treatment. The importance of the risk structure
compensation for the health insurance funds is clearly
evident here, but also that certain areas are of
considerable importance within age groups.
4 LORENZ CURVES AND GINI
COEFFICIENTS
As an example, we consider in Table 1 the mean case
costs in the age group 0-14 years, depending on the
type of health insurance, as well as the associated
cumulative patient and cost shares.
Table 1: Case costs, cumulative patient and cost shares
according to insurance fund.
Fund
type
Case
costs €)
pat.-frac.cum.
(%)
Cost-part.cum.
(%)
2 34,35 17,99 13,58
5 36,93 26,01 20,10
6 40,93 71,45 60,98
3 55,10 72,87 62,70
4 61,47 99,19 98,27
1 97,40 100,00 100,00
This gives us a corresponding Lorenz curve in
Figure 4 with the Gini coefficient 0.12 (area between
the curve determined by patient and cost shares and
the diagonal; alternatively, a normalization with a
factor of 2 between the curves is used in the
literature).
Figure 4: Lorenz curve for patient and cost shares in the age
group 0-14 years with the proportion of patients on the
vertical axis and the proportion of costs on the vertical axis.
For the Gini coefficients of the specialist groups,
there are clear differences with regard to the types of
health insurance fund, cf. Table 2.
Table 2: Gini coefficients for the type of health insurance
for medical specialty group.
Gini
coefficent (%) medical specialty group
1,02 Oral, maxillofacial and facial surgeons
1,42 Internists (pulmonology)
3,17 Pediatricians
3,41 Child / adolescent psychiatrist
3,94 Dermatologists
4,10 Internists (hematology / oncology)
4,49 Ophthalmologists
4,67 Gynecologists
4,97 Internists (rheumatology)
5,02 Surgeons
5,41 Urologist
5,61 ENT doctors
5,72 Internists (cardiology)
5,94 Orthopedists
6,19 Neurology / Neurology
7,45 Anesthetists
8,94 General practitioners
8,94 Radiologists
9,08 Psychiatry and psychotherapy / neurology
10,02 Internists (nephrology)
10,62 Internists (specialists)
10,64 Medical psychotherapists
11,32 Internists (gastroenterology)
13,50 Internists (endocrinology)
24,14 Radiation therapists
For The smallest differences in costs with regard
to the types of insurance are next to the small
specialist group of oral and maxillofacial surgeons for
pulmonologists and paediatricians. Gastroentero-
0%
1%
2%
3%
4%
5%
6%
0 5 10 15 20 25 30 35 40 45 50 55 60 65 70 75 80 85 90
fraction
age
number of cases
AOK BKK BKN
IKK LKK VdEK
0.2 0.4 0.6 0.8 1.0
0.2
0.4
0.6
0.8
1.0
HEALTHINF 2022 - 15th International Conference on Health Informatics
394

logists and radiation therapists have the greatest cost
differentiation with regard to the type of health
insurance. The General practitioners are in the
middle.
5 DISCUSSION AND
CONCLUSION
The considerable influence of the type of insurance
funds on the cost structure makes it clear that case
costs specific to age groups should be used depending
on the type of insurance fund. This approach
describes a morbidity-related risk structure
compensation for the physician. The application of
the risk structure compensation (RSC, Morbi-RSA),
which is common for health funds, to doctors appears
to be a necessary consequence. As an example,
consider in Table 3 the effects at the upper and lower
limit points for general practitioners.
Table 3: Profitability evaluation with and without risk
structure compensation (RSC) for the doctor.
Physician
with
Compensation
for morbidity
(€)
without
Compensation
for morbidity
(€)
Over- /
under-
payment
(%)
result
(%)
1 1.534,91 1.346,52 87,73 114
2 533.128,00 473.200,02 88,76 113
3 55.261,27 49.869,03 90,24 111
4 715.327,48 656.349,11 91,76 109
5 631.481,05 579.615,71 91,79 109
6 138.328,83 127.563,42 92,22 108
7 353.775,03 326.719,76 92,35 108
8 254.136,29 236.049,46 92,88 108
9 356.234,76 331.451,26 93,04 107
10 259.817,72 241.763,38 93,05 107
… … … … ..
1.203 369.268,96 398.390,82 107,89 93
1.204 266.444,41 287.501,12 107,90 93
1.205 160.722,60 173.465,69 107,93 93
1.206 215.969,65 234.045,34 108,37 92
1.207 35.858,68 38.910,51 108,51 92
1.208 227.612,77 247.060,47 108,54 92
1.209 103.938,17 113.090,71 108,81 92
1.210 104.004,85 114.433,94 110,03 91
1.211 3.410,21 3.766,44 110,45 91
1.212 52.584,56 58.213,02 110,70 90
Failure to take account of the type of health fund
with a view to compensating for morbidity ranges
from a disadvantage of 14% to an advantage of 10%
for general practitioners, whereby the drug costs
involved are also very different. Large amounts play
a role in both the upward and downward deviations.
In the case of benchmark and average restrictions,
an excess of 25% can trigger a pay-back procedure (if
the physician is included permanent in the
contractually agreed sample). If 14% of these cases it
can already be due to the insurance fund
(disadvantage due to the patient structure), it seems
advisable to take insurance fund into account. Table
4 shows the budget overrun with and without
insurance dependent compensation for morbidity.
Table 4: Deviances in the profitability evaluation with and
without morbidity risk structure compensation (RSC) for
the doctor.
medical
speciality
group
Physician
Drug costs
(€)
Budget
overrun with
Compensation
for morbidity
(%)
Budget
overrun
without
Compensation
for morbidity
(%)
GP 1 532.498,04 123,7 131,4
GP 2 713.782,57 123,4 125,4
GP 3 715.327,48 118,5 129,2
GP 4 652.004,87 123,4 125,9
GP 5 350.017,51 124,9 127,1
GP 6 189.596,78 122,6 125,0
GP 7 17.059,82 119,3 126,2
GP 8 610.218,21 122,8 126,3
GP 9 854.378,71 122,6 125,7
Anesthetists 10 937.725,13 124,5 126,4
Gynecologists
11 1.040.364,55 124,6 125,5
Urologist 12 295.275,67 123,1 125,3
Internists 13 289.871,33 122,0 131,0
Internists 14 341.535,80 118,5 126,4
Depending on the starting point in the calculation
that is not adjusted for the type of health insurance
fund, the 25% range will then be exceeded. In the
period under review (first calculation), there were 14
physicians that would not come into the area of pay-
back with morbidity adjustment with regard to the
health fund using the age group adjustment, but
would fall into the anomaly area without the
additional adjustment with respect to the health
insurance fund.
The problems presented do not occur when the
MRG model is used. The problems presented do not
occur when the MRG model is used. If, however,
economic feasibility analyzes are carried out without
prescription-related morbidity evaluations, an
additional adjustment of the type of health insurance
Benefits and Limitations of Age Group-Adjusted Average in the Profitability Audit for Pharmocotherapy
395

provider is required in addition to the age group
adjustment in order to meet the conditions required in
the social court judgments cited above.
Till 2020 in the majority of the federal states in
Germany (more precisely: in the regions of the
Association of Statutory Health Insurance Physicians
SHI), the economic feasibility studies with regard to
the drug prescriptions were carried out with the help
of the discussed problematic benchmarks and average
calculations. The service providers (doctors) are
largely satisfied with this because the limits of the
problematic sanctions (pay-back) have been
significantly increased. This evaluation largely (with
the exception of the exceptions discussed) contains all
drug prescriptions, which leads to a fairness between
the doctors. The necessary increase in equity for
doctors with regard to the membership of their
patients in the health insurance funds was not
implemented in a single German region. In some
federal states, the economic feasibility study has been
switched to target agreements, which only include a
certain part of the drug ordinances and thus leads to a
limited degree of justice between doctors. Target
agreements have a normative character and only take
regional characteristics into account to a certain
extent. In Schleswig-Holstein, in addition to a target
agreement with a compensatory effect, an MRG
(morbidity related groups) analysis was carried out in
2020, in which patient-centered features regarding the
diseases and the prescribed drugs were taken into
account and thus a risk compensation with regard to
the health insurance companies was fully
implemented. For the most part, the fairness of the
examination for doctors with regard to health
insurance companies has not yet been adequately
resolved.
REFERENCES
Busse, R., Panteli D., Henschke C. (2015). Arzneimittel-
versorgung in der GKV und 15 anderen europäischen
Gesundheitssystemen: Ein systematischer Vergleich,
Universitätsverlag der TU Berlin.
Bratzke, Spies, Krebs (2012). Morbiditätskomponente bei
Arznei- und Heilmittelbudgets einführen, Deutsche
Ärztetag 2012, Drucksache V I – 37.
Emcke, T., Ostermann, Th., Heidbreder, M., Schuster, R.
(2017). Comparison of Different Implementations of a
Process Limiting Pharmaceutical Expenditures
Required by German Law. Proceedings of HealthInf.
GKV-Versorgungsstärkungsgesetz (GKV-VSG) (2015).
BGBl. I S. 1211, 2015
Gottwald, N. (2015). Damoklesschwert Richtgrößen-
prüfung. Im Dschungel der 25-Prozent-Regel, HNO-
Nachrichten, Springer.
Korzilius, H. (2015). Arzneimittelrichtgrössen, Ärzte sollen
angstfrei verordnen, Dtsch Arztebl 112.
Ostermann, Th., R.Schuster, R. (2015). An Information-
theoretical Approach to Classify Hospitals with
Respect to Their Diagnostic Diversity using Shannon’s
Entropy. HealthInf.
Prüfvereinbarung (2016). Prüfvereinbarung gemäß §§ 106
Abs. 1, 106a Abs. 4 und 106b Abs. 1 SGB V
wischender Kassenärztlichen Vereinigung Schleswig-
Holstein (KVSH), Bad Segeberg und den
Krankenkassen(-verbänden). www.kvsh.de.
Schuster, F., Ostermann, Th., Schuster R., Emcke, T.
(2017). Deviations in Birth Rates with Respect to the
Day of the Week and the Month for a 100 Year Period
Regarding Social and Medical Aspects in Explaining
Models. Proceedings of HealthInf.
Schuster, F., Ostermann, Th., Emcke, T. (2017). Age and
Gender Structures for ICD 10 Diagnoses in Outpatient
Treatment using Shannon Entropy, GMDS, German
Medical Science.
Schuster, R. (2015). Morbidity Related Groups (MRG) and
drug economic efficiency index - a new concept after
the age of “Richtgrößen” benchmarks in Germany,
GAA-Jahrestagung, German Medical Science.
Schuster, R., Heidbreeder, M., Emcke, T. (2017).
Relations of Morbidity Related Groups (MRG), ICD 10
diagnoses and age structures in outpatient treatment.
GMDS, German Medical Science.
Schuster, R., Emcke, T., Arnstedt, E.v., Heidbreder M.
(2016). Morbidity Related Groups (MRG) for
epidemiological analysis in outpatient treatment, IOS
Press 783-787.
Schuster, R., Emcke, T., Schuster, F. (2016). Vergleich der
Richtgrößenauswertungen für Arzneimittel im
Vertragsärztlichen Bereich mit Statusgruppen und
Altersgruppen. GMDS-Jahrestagung, German Medical
Science.
Sinowatz F. (2015). Ressourcenallokation in der haus-
ärztlichen Versorgung: eine empirisch-ethische
Untersuchung, Dissertation, LMU München:
Medizinische Fakultät.
Urt. LSG Sachsen-Anhalt (2013) v. 15.01.2014 - L 9 KA
5/12.
Urt. BSG Juni (2013). http://www.medical-tribune.de:
Amtsermittlungspflicht bei Praxisbesonderheiten.
Urt. SG Dresden (2013) v. 11.12.2013, Az. S 18 KA 31/10,
S 18 KA 71/10, S 18 KA 266/10, S 18 KA 268/10 und
S 18 KA 269/10.
Wersborg, T. (2006). Morbiditätsbezogene Richtgrößen zur
Steuerung einer bedarfsgerechten und wirtschaftlichen
Arzneimittelversorgung innerhalb der gesetzlichen
Krankenversicherung in Deutschland, Dissertation,
LMU München: Medizinische Fakultät.
HEALTHINF 2022 - 15th International Conference on Health Informatics
396
