
Disaster Mitigation Strategies to Maintain Mental Health Stability in
Society Facing Covid-19 Pandemic: A Systematic Review
Sarah Salsabila Ichwanhaq
1
, Novi Qonitatin
2
and Dian Ratna Sawitri
2
1
Master of Psychology,Universitas Diponegoro, Semarang, Indonesia
2
Faculty of Psychology, Universitas Diponegoro, Semarang, Indonesia
Keywords: Mental Health, Disaster Mitigation, Pandemic, COVID-19.
Abstract: The COVID-19 Pandemic has been declared as a public health emergency and the virus already spread
around the world. This has an impact on mental health in the community. The systematic review aims to
review all research on mitigation to maintain mental health stability in the community facing the COVID-19
pandemic. Article searches were obtained from PubMed, Science Direct, Google Scholar, Cambridge Core,
ProQuest, and SpringerLink. The research method uses Preferred Reporting Items for Systematic Review
and Meta-Analysis (PRISMA). The search identified 46 articles and used 9 articles that match the criteria.
Analysis of 9 relevant articles shows that disaster mitigation was carried out with targets in society,
specifically on healthcare workers. Healthcare workers are mostly in the form of education on anti-
contagion measures by using Personal Protective Equipment (PPE) and interventions in the form of training
or crisis response services. Disaster mitigation in society takes the form of strengthening crisis center
services, education on the applications of a healthy lifestyle, and increasing positive thinking to reduce
negative emotions as well as education on limiting information from social media to reduce anxiety and fear
related to the COVID-19 pandemic.
1 INTRODUCTION
COVID-19 is a disease caused by novel coronavirus
or better known as SARS-CoV-2 which was
discovered in 2019 at Wuhan, China for the first
time. SARS-CoV-2 was identified and the genetic
was shared publicly in early January 2020 (World
Health Organization, 2020). World Health
Organization declared that COVID-19 was a public
health emergency on January 30, 2020, and COVID-
19 was declared as a pandemic on March 11, 2020
(Balkhair, 2020). COVID-19 was declared a
pandemic due to the high risk of spreading the virus
to other countries around the world (WHO, 2020).
The status of COVID-19 that has been determined
by the World Health Organization is then followed
up limiting society’s mobility, implementing social
interaction, and conducting self-isolation or self-
quarantine. This has a long-term impact on society’s
mental health (Ridlo, 2020).
Mental health is an individual’s ability to adapt
to various circumstances, both in adjusting to
oneself and adjusting to society (Santoso, 2016).
Then, mental health is how individuals think, feel,
and act when faced with the realities of life. Mental
health can be optimal when individuals can
overcome the problems that occur in life and
individuals can deal with these problems well
(Hadjam & Widhiarso, 2011). The balance between
physical and psychological conditions of the
individuals also reflects mental health where these
two conditions are interconnected and mutually
reinforcing so that individuals can adapt to the
surrounding environment (Fridayanti et al., 2019).
Mental health can’t distribute properly due to the
problems that individuals faced. Individuals who
have a high risk of experiencing mental health
disorders are individuals who have a low social level
and individuals are in a vulnerable position (Power
et al., 2020). A study showed that the current
COVID-19 pandemic causes uncertainty in life and
slowing the pace of the economy can reduce mental
health. Declining mental health can increased
anxiety in individuals (Soklaridis et al., 2020).
Another study showed that 64.3% of the total 1522
respondents experienced anxiety disorders,
depression, and psychological trauma during the
COVID-19 pandemic (Ross et al., 2020). Ages that
94
Ichwanhaq, S., Qonitatin, N. and Sawitri, D.
Disaster Mitigation Strategies to Maintain Mental Health Stability in Society Facing Covid-19 Pandemic: A Systematic Review.
DOI: 10.5220/0010809200003347
In Proceedings of the 2nd International Conference on Psychological Studies (ICPsyche 2021), pages 94-102
ISBN: 978-989-758-580-7
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
are vulnerable to increased stress and anxiety due to
the COVID-19 pandemic are teenagers where there
is occur due to limited access to outdoor activities
(Iqbal & Rizqulloh, 2020).
Mental health disorders are not only experienced
by teenagers but also experienced by adults. A study
showed that adults experienced mild to moderate
symptoms of depression and increased symptoms of
anxiety due to the fear that arises as a result of the
COVID-19 pandemic (Haider et al., 2020). High
levels of anxiety can harm individuals and society.
The adverse effects caused lead to maladaptive
behavior (Vigo et al., 2020). The global situation
that has occurred due to the COVID-19 pandemic is
important to realize the trauma can affect each
individual in different ways. This can create mental
health challenges for society (Otu et al., 2020). The
implications for mental health are long-lasting and
have a greater prevalence than the virus itself.
Mental health is an important aspect in realizing
overall health (Ridlo, 2020).
Efforts to maintain mental health stability in
society can be carried out in disaster mitigation
strategies. Mitigation is an activity to reduce and
minimize the impact of disasters (Niode et al.,
2016). Mitigation is also an effort to reduce the
impact of disasters such as natural disasters, non-
natural disasters, or a combination of both disasters
in a country or society (Ma’ruf, 2010). Then,
disaster mitigation is the first step to do in
preventing disaster (Buchari, 2020). Disaster
mitigation is also an effort to reduce the occurrence
of disaster risk, both through physical development
as well as awareness and capacity building in
dealing with disaster threats (Sunarti, 2014).
One of the disaster mitigation strategies is
providing education on implementing a healthy
lifestyle, such as regulating sleep patterns and
increasing physical activity to reduce the emergence
of negative emotions during the COVID-19
pandemic (Zhang et al., 2020). Disaster mitigation
can also be done by providing services by telephone
to individuals who have a high level of risk of
experiencing mental health disorders (Momoi et al.,
2020). The authors would like to conduct a further
systematic review of disaster mitigation strategies to
maintain mental health stability in a society facing
the COVID-19 pandemic. This systematic review
aims to summarize and identify disaster mitigation
to maintain mental health stability in a society facing
the COVID-19 pandemic.
2 METHOD
Article searches were obtained from PubMed,
Science Direct, Google Scholar, Cambridge Core,
ProQuest, and SpringerLink with the keywords
relevant to the topic, which were “Disaster
mitigation AND “COVID-19” OR “Mental health”
AND “COVID-19” in English as well as “Mitigasi
bencana” AND “COVID-19” OR “Kesehatan
mental” AND “COVID-19” in Indonesian. This
systematic review was conducted and reported under
the Preferred Reporting Items for Systematic
Review and Meta-Analysis (PRISMA).
The articles found would be reviewed based on
the inclusion criteria: 1) disaster mitigation to
maintain mental health stability in society; 2) the
publication of the articles between 2020-2021; 3)
full text; 4) the articles in English and Indonesian.
The search identified 46 articles (PubMed 14
articles, Science Direct 10 articles, Google Scholar 8
articles, Cambridge Core 6 articles, ProQuest 4
articles, and SpringerLink 4 articles). 18 articles
were issued which mental health articles that did not
lead to disaster mitigation and articles that were not
in the form of publication such as letters to the
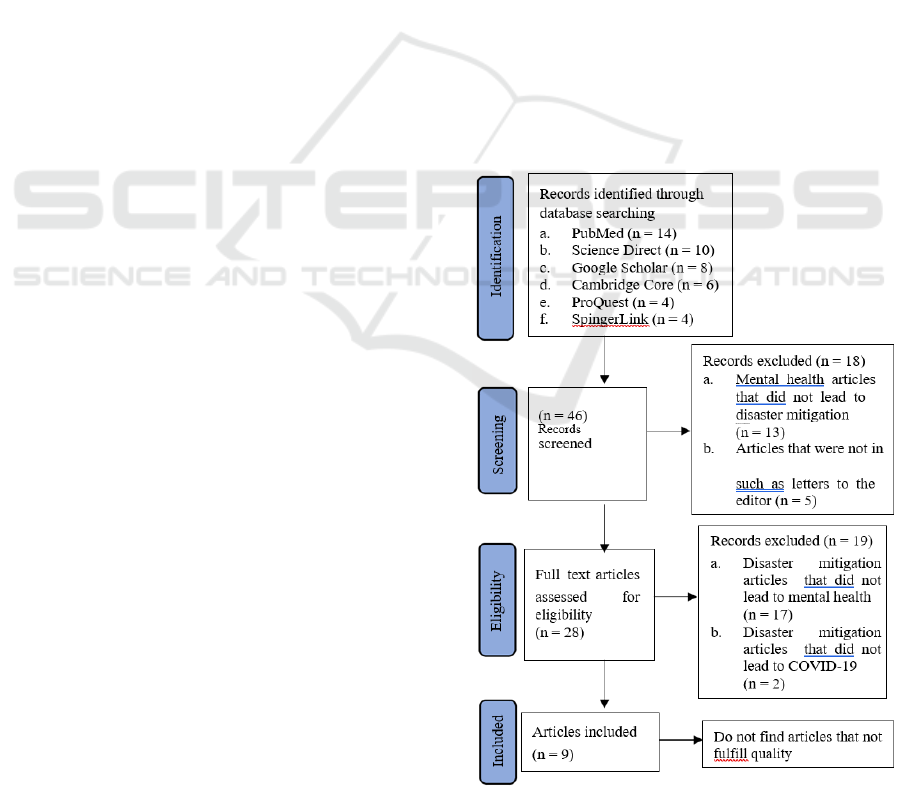
Figure 1: Article Selection Flow.
Disaster Mitigation Strategies to Maintain Mental Health Stability in Society Facing Covid-19 Pandemic: A Systematic Review
95

editor. Then, 28 full-text articles were obtained
which were assessed for eligibility. 19 articles were
issued where disaster mitigation articles that did not
lead to mental health and disaster mitigation articles
that did not lead to COVID-19. 9 full-text articles
match the criteria as shown in Figure 1.
3 RESULT
Table 1: Article Review Summary.
References Country Respondents
Disaster Mitigation
Strategies
Outcomes Related to Review Aims
Giorgi et
al., 2020
Italy
673 office
workers
Education of Personal
Protective Equipment
(PPE)
Respondents who returning to their duties
after protracted lockdown, showed that
respondents are facing post traumatic stress
disorder (10,8%). Meanwhile, respondents
reported a low prevalence of anxiety
(3,8%), depression (3,7%), stress (1,5%),
and insomnia (2,3%). Disaster mitigation
carried out by the organization are
improving infrastructure at workplace,
implementing anti-infectious measures
where Personal Protective Equipment (PPE)
provided, and implementing resilience
training programs to increase understanding
the psychological conditions during the
COVID-19 pandemic.
Gray et al.,
2021
USA
1170
healthcare
workers
a. Mental Health
Liaison (MHL)
b. Mental Health
Crisis Response
Team (MHCRT)
Disaster mitigation that carried outs is to
form a program with the Mental Health PPE
model to support the mental health of
healthcare workers during COVID-19
pandemic. Mindfulness and breathing
exercises that include on effective support
techniques having ability to text someone
when they needed to access to referrals for
mental health treatment.
Matto &
Sullivan,
2021
UK
100
emergency
services
personnel
Mindfulness
techniques with art
therapy from
Ashes2Art
Organization
Ashes2Art is a non-profit organization that
works with firefighters who promote
creativity to offset exposure to extreme loss
and trauma. Ashes2Art has around 100
emergency services personnel and family
members actively participating during the
crisis during COVID-19 pandemic.
Mindfulness techniques that integrated with
art therapy to reduce burnout and enhance
self-care in healthcare workers to provide a
community of support.
ICPsyche 2021 - International Conference on Psychological Studies
96

Table 1: Article Review Summary (cont.).
References Country Respondents
Disaster
Mitigation
Strategies
Outcomes Related to Review Aims
Momoi et
al., 2020
Japan
210.000
respondents
Intervention by
Telephone
Disaster mitigation that carried out by sending a
mental health and lifestyle survey to the society
and then providing interventions by telephone
to individuals who is at high risk based on the
survey results. This is done to help individuals
at risk cope with stress, reduce emotional
burden, provide information on social resources
(e.g., schools, public offices, or medical
facilities), and provide advice related to
lifestyle. Respondents who received telephonic
system help in the form of stress coping method
(36,6%), social resource information (29,4%),
and lifetsyle advice (28,8%).
Otu,
Charles, &
Yaya, 2020
UK
775
respondents
of adults
a. Eductaion of
Personal
Protective
Equipment
(PPE)
b. Education of
Implementin
g Positive
Thinking
a. Disaster mitigation that provide education
related to the proper use of Personal
Protective Equipment (PPE) and to
understand the main principles underlying
the management of patients COVID-19.
Healthcare workers trained to be able to
identify the early signs of stress or burnout
that arise at workplace and seek help
immediately.
b. Disaster mitigation that carried out for
society are provide education related to
positive thinking and full of hope and build
a positive image. Then, society is also
taught to be able to limit exposure the news
that related to COVID-19 which can cause
anxiety and psychological stress.
Sheek-
Hussein,
Abu-Zidan,
& Stip,
2021
UAE
a. Healthcar
e Workers
b. Society
a. Academic
Journal Club
b. Education of
Implementin
g Positive
Thinking
Disaster mitigation that carried out includes two
targets which is healthcare workers and society.
a. Disaster mitigation for healthcare workers is
to form the Academic Journal Club. This
club was formed to increase the reading
interest of healthcare workers. This club
was also formed to reduce negative
emotions and improve stress management.
Read at one’s own pace with a follow-up
session by phone or video call.
b. Disaster mitigation for society is provide
education that related to positive thinking.
Another disaster mitigation for society is
also taught to be able to limit themselves
from news that related to COVID-19 which
can cause anxiety and psychological stress.
Disaster Mitigation Strategies to Maintain Mental Health Stability in Society Facing Covid-19 Pandemic: A Systematic Review
97

Table 1: Article Review Summary (cont.).
References Country Respondents
Disaster Mitigation
Strategies
Outcomes Related to Review Aims
Skilbeck,
Spanton, &
Roylance,
2020
UK
a. Healthcare
Frontline
and Non-
Frontline
Workers
b. Society
Improving Access to
Psychological Therapies
(IAPT) Services:
a. Stepped-care model of
talking therapy for
low-intensity (guided
self-help)
b. Stepped-care model of
talking therapy for
high-intensity (CBT)
Disaster mitigation with Improving
Access to Psychological Therapies
(IAPT) is a mental health service
that has shown variability in
response to COVID-19. Several
IAPT services are adapting quickly
to reduce anxiety and fear of
uncertainty condition during
COVID-19 pandemic.
Suyadi,
Nuryana, &
Fauzi, 2020
Indonesia
3917 patients
in 79 hospitals
Fikih Kebencanaan
(Coping with Disaster)
Disaster mitigation that carried out
by Fikih Kebencanaan (Coping with
Disaster) where the medical health
movement and the reconstruction of
fiqh worship are about the rules to
adapt with emergencies or COVID-
19 pandemic situation. Fikih
Kebencanaan teaches how to deal
with disasters from a general
religious perspective.
Zhang et
al., 2020
China
66 college
students
Education of Implementing
Healthy Lifestyle
Respondents reported a high
prevalence of stress (71,21%),
anxiety (54,55%), and depression
(77,27%). Disaster mitigation that
carried out is to provide education
on implementing a healthy life such
as doing regular exercise by physical
activities that are in accordance with
the physical abilities of each
individual and regular sleep.
Disaster mitigation to reduce
negative emotions of everyone.
4 DISCUSSION
This study aims to find out about disaster mitigation
to maintain mental health stability facing the
COVID-19 pandemic. There are found two main
targets of disaster mitigation that related to mental
health based on 9 articles, such as healthcare
workers and society. Many of the articles were
reported from overseas and only one article was
conducted in Indonesia. The results show that
disaster mitigation to maintain mental health
stability mostly to prevent the emergence of negative
emotions and psychological stress as well as the
form of intervention to manage a crisis or emotional
burdens that occur during the pandemic.
Disaster Mitigation for Healthcare Workers.
Disaster mitigation can be done by establishing a
service program for healthcare workers. First,
disaster mitigation to maintain mental health
stability by educating to use and provision of
Personal Protective Equipment (PPE) to avoid
susceptibility to COVID-19 transmission (Gray et
al., 2021). Completeness of Personal Protective
Equipment (PPE) was found to have a significant
ICPsyche 2021 - International Conference on Psychological Studies
98

relationship with decreasing anxiety about being
infected with COVID-19 in healthcare workers
(Asriyani & Sriningsih, 2021; Irmayanti et al.,
2021). Healthcare workers’ perceptions of Personal
Protective Equipment (PPE) the availability that
complete and good are related to an increase in
symptoms of anxiety and depression (Smith et al.,
2021). The government and health agencies need to
be aware of the magnitude of mental health
problems in healthcare workers and expected to
always be vigilant in providing adequate Personal
Protective Equipment (PPE) when the pandemic
continues (Arnetz et al., 2020).
Second, Disaster mitigation that carried out to
maintain mental health stability by implementing
resilience training programs, providing Personal
Protective Equipment (PPE), and improving
infrastructure (Giorgi et al., 2020). Disaster
mitigation can be done by establishing a service
program for healthcare workers. The program of
disaster mitigation is divided into two teams, Mental
Health Liaison (MHL) where the team provides
prevention support to the COVID-19 hospital unit
and the emergency unit, and Mental Health Crisis
Response Team (MHCRT) were the team that has
crisis response services for 7 days 24 hours to
support and reduce the crisis in healthcare workers
as needed (Gray et al., 2021). Healthcare workers
also need help to maintain their mental health
through actions to reduce negative emotions and
improve stress management (Sheek-Hussein et al.,
2021).
Healthcare workers are also trained to be able to
identify the early sign of stress or burnout that
appear at the workplace and seek help immediately
(Otu et al., 2020). Resilience is very important to
deal with stress and important to keep it balance
during pandemics (Vinkers et al., 2020). The
resilience training program is seen as an alternative
to disaster mitigation measures that can be used to
maintain mental health disabilities. Resilience is
described as an individual’s capacity to rise above
adversity, conflict, confusion, and failure and the
ability to make positive changes (Gatt et al., 2020).
High resilience is associated with good mental
health (Xu et al., 2020). That is very important for
intervention programs and support strategies to be
developed during the COVID-19 pandemic to
protect mental health and against mental distress and
increase psychological resilience (Bakioğlu et al.,
2020).
Disaster Mitigation for Society. Disaster mitigation
in society can be done by providing interventions in
the form of education or opening mental health crisis
center services for society. This service aims to
reduce the level of anxiety, emotional burden, and
fear, especially during the uncertainty of the
COVID-19 pandemic (Momoi et al., 2020; Skilbeck
et al., 2020). Providing education-related to positive
and hopeful thinking as well as building a positive
self-image, especially in a pandemic situation (Otu
et al., 2020). Maintain mental health stability should
be made to overcome stress, provide information
that is available on social resources, and provide
advice related to a better lifestyle (Momoi et al.,
2020). Disaster mitigation is also carried out by
providing education related to implementing a
healthy lifestyle to increasing positive emotions and
reducing exposure to COVID-19 news. Education on
the application of a healthy lifestyle such as doing
regular exercise by doing physical activity,
managing to sleep well, and reduce the negative
emotions of each individual (Zhang et al., 2020).
Identification to get more precise targets in
providing services through surveys to society, such
as collecting data on society’s health and lifestyle
then followed up by providing interventions by
telephone that have adjusted to the needs based on
the results of the survey (Momoi et al., 2020). The
interventions by telephone have the beneficial
impact of reducing psychological distress. In
addition, interventions by telephone that are carried
out consistently are also for the treatment of anxiety
and depression (Martin et al., 2020). Mental health
services are changing due to the COVID-19
pandemic. The demand for face-to-face mental
health services decreased significantly because of
fear of infection (United Nations, 2020). Restrictive
measures on physical and social contact hinder
traditional face-to-face psychological services
during the COVID-19 pandemic. This is in line with
the passing of the acute phase during the pandemic
where it is very likely that people who are more
vulnerable (both biomedically and psychologically)
will avoid face-to-face contact (Ribeiro et al., 2020).
Another important thing that was found was the
need for restrictions to news-related COVID-19 in
society who are vulnerable to mental health.
Excessive coverage in the mass media can cause
anxiety and psychological stress (Lin et al., 2020).
Individuals who sit more and spend more time
reading news related to COVID-19 can increase
anxiety and depression (Huckins et al., 2020). The
importance of credibility through mass media and
social media as well as the right strategy to fight
misinformation during the pandemic. The role of
social media is very necessary to provide correct
Disaster Mitigation Strategies to Maintain Mental Health Stability in Society Facing Covid-19 Pandemic: A Systematic Review
99

information during the COVID-19 health crisis. On
the other hand, wrong or correct information is
received by the public it will have a global negative
impact on mental health (Abbas et al., 2021).
The special thing that appears in the study of
research article found in Indonesia is the effort to
maintain mental health stability in society through a
religious or religious approach which is Fikih
Kebencanaan (in the form of coping strategies in
dealing with disasters). Fikih Kebencanaan teaches
how to deal with disaster from a general religious
perspective. Disaster mitigation through a religious
approach also teaches the rules of worship to be able
to adapt the emergencies or the COVID-19
pandemic (Suyadi et al., 2020). This is supported by
research results show that a strong relationship
between religiosity and mental health, especially in
the form of social welfare (Winurini, 2019).
Religiosity has an important role in relieving
suffering, having an influence on health outcomes,
and minimizing the consequences of social isolation
(Lucchetti et al., 2020). That is necessary to
highlight religious activities during the pandemic as
a step in maintaining mental health stability.
Disaster mitigation can also be done using art
media, such as Ashes2Art as a non-profit
organization based in the UK apart from using a
religious approach. This organization has creative
activities to offset exposure to extreme loss and
trauma. Another purpose of this activity as an effort
to help manage the short-term and long-term
emotional impact of the activity or work that is
carried out (Matto & Sullivan, 2021). Art is related
to the positive mental health domain. The effect of
art goes beyond the scope of energizing, relaxing, or
bringing relief to positive psychological aspects.
These are attention, autonomy, flexibility, social
relationship with others, emotional well-being,
experiencing freedom, play, and self-directed
(Haeyen et al., 2018). Art as a tool to improve
mental health well-being and in line with global
health challenges. Art activities have been
documented as non-medic, holistic, low-cost with the
potential to promote mental health and community
well-being (Jensen, 2018). Art engagement amongst
society may help to enhance positive mental health
and life satisfaction, especially against mental distress
(Wang et al., 2020).
5 CONCLUSION
Various disaster mitigation methods were carried out
to reduce and minimize the impact caused by the
COVD-19 pandemic situation. Disaster mitigation
by providing education on healthy lifestyle and other
intervention services to reduce stress and emotional
burden as well as increase positive thinking that is
full of hope. Disaster mitigation during the COVID-
19 pandemic is related to mental health is not only
given to the society in general but also needs to be
done to healthcare workers who are in direct contact
with COVID-19 patients who give anxiety of
transmission. Further research can conduct studies
related to disaster mitigation that leads to mental
health stability in Indonesia as well as disaster
mitigation services that can be accessed and
accepted by all levels of society in Indonesia to deal
with the COVID-19 pandemic situation.
ACKNOWLEDGMENT
We thank the Faculty of Psychology Universitas
Diponegoro for supporting the study. The authors
declared no potential conflict of interests concerning
the research, authorship, and publication of this
article. The study is based on literature that is
publicly available and does not require any
declaration.
REFERENCES
Abbas, J., Wang, D., Su, Z., & Ziapour, A. (2021). The
role of social media in the advent of covid-19
pandemic: Crisis management, mental health
challenges and implications. Risk Management and
Healthcare Policy, 14, 1917–1932.
https://doi.org/10.2147/RMHP.S284313
Arnetz, J. E., Goetz, C. M., Sudan, S., Arble, E., Janisse,
J., & Arnetz, B. B. (2020). Personal protective
equipment and mental health symptoms among nurses
during the covid-19 pandemic. Journal of
Occupational and Environmental Medicine, 62(11),
892–897. https://doi.org/10.1097/JOM.000000000000
1999
Asriyani, D., & Sriningsih, N. (2021). Hubungan tingkat
kecemasan penggunaan alat pelindung diri (apd)
terhadap pencegahan penularan covid-19 pada perawat
di ruang rawat inap rumah sakit umum (rsu) kabupaten
tangerang tahun 2020. Nusantara Hasana Journal.
1(1), 95–101.
Bakioğlu, F., Korkmaz, O., & Ercan, H. (2020). Fear of
covid-19 and positivity: Mediating role of intolerance
of uncertainty, depression, anxiety, and stress.
International Journal of Mentah
Health and Addiction, 1-14. https://doi.org/10.1007/
s11469-020-00331-y
ICPsyche 2021 - International Conference on Psychological Studies
100

Balkhair, A. A. (2020). Covid-19 pandemic: A new
chapter in the history of infectious diseases. Oman
Medical Journal, 35(2), 2–3.
https://doi.org/10.5001/OMJ.2020.41
Buchari, R. A. (2020). Manajemen mitigasi bencana
dengan kelembagaan masyarakat di daerah rawan
bencana kabupaten garut indonesia. Sawala : Jurnal
Pengabdian Masyarakat Pembangunan Sosial, Desa
Dan Masyarakat, 1(1), 1.
https://doi.org/10.24198/sawala.v1i1.25836
Fridayanti, F., Kardinah, N., & Nurul Fitri, T. J. (2019).
Peran workplace well-being terhadap mental health:
Studi pada karyawan disabilitas. Psympathic : Jurnal
Ilmiah Psikologi, 6(2), 191–
https://doi.org/10.15575/psy.v6i2.5754 Gatt, J. M.,
Alexander, R., Emond, A., Foster, K.,
Hadfield, K., Mason-Jones, A., Reid, S., Theron, L.,
Ungar, M., Wouldes, T. A., & Wu, Q. (2020). Trauma,
resilience, and mental health in migrant and non-
migrant youth: An international cross-sectional study
across six countries. Frontiers in Psychiatry, 10
(March). 1-15. https://doi.org/10.3389/fpsyt.2019.0
00997
Giorgi, G., Lecca, L.I., Alessio, F., Finstad, G.L.,
Bondanini, G., Lulli, L.G., Arcangeli, G., & Mucci, N.
(2020). Covid-19-mental health effects in the
workplace. International Journal of Environmental
Research and Public Health, 17(21). 1-22.
https://doi.org/10.3390/ijerph17217857
Gray, B., Eaton, J., Duncan, J., Hanna, F., & Kasi, S.
(2021). A proactive approach: Examples for
integrating disaster risk reduction and mental health
and psychosocial support programming. International
Journal of Disaster Risk Reduction, 54.
https://doi.org/10.1016/j.ijdrr.2021.102051
Hadjam, M., & Widhiarso, W. (2011). Pengujian model
peranan kecakapan hidup terhadap kesehatan mental.
Jurnal Psikologi UGM, 38(1), 61-72.
https://doi.org/10.22146/jpsi.7665
Haeven, S., van Hooren, S., van der Weld, W. M., &
Hutschemaekers, G. (2018). Promoting mental health
versus reducing mental illness in art therapy with
patients with personality disorders: A quantitative
study. Arts in Psychotherapy, 58, 11-16.
https://doi.org/10.1016/j.aip.2017.12.009
Haider, I.I., Tiwana, F., & Tahir, S.M. (2020). Impact of
the Covid-19 pandemic on adult mental health.
Pakistan Journal of Medical Sciences, 36(COVID19-
S4). https://doi.org/10.12669/pjms.36.COVID19-
S4.2756
Huckins, J.F., da Silva, A. W., Wang, W., Hedlund, E.,
Rogers, C., Nepal, S.K., Wu, J., Obuchi, M., Murphy,
E. I., Meyer, M. L., Wagner, D. D., Holtzheimer, P.
E., & Campbell, A. T. (2020). Mental health and
behavior of college students during the early phases of
the Covid-19 pandemic: Longitudinal smartphone and
ecological momentary assessment study. Journal of
Medical Internet Research, 22(6).
htpps://doi.org.10.2196/20185
Iqbal, M., & Rizqulloh, L. (2020). Deteksi dini kesehatan
mental akibat pandemi Covid-19 pada Unnes sex care
community melalui metode self reporting
questionnaire. Praxis, 3(1). 20.
https://doi.org/10.24167/praxis.v3i1.2730
Irmayanti, A., Trisnawati, E., & Saleh, I. (2021). Faktor
yang berhubungan dengan kecemasan terinfeksi
Covid-19 pada tenaga keseharan di Puskesmas Kota
Pontianak. Riset Informasi Kesehatan, 10(1), 34-42.
https://doi.org/10.30644/rik.v8i2.517
Jensen, A. (2018). The use of arts interventions for mental
health and wellbeing in health settings. Perspectives in
Public Health, 138(4), 209-214. https://doi.org/10.11
77/1757913918772602
Lin, Y., Hu, Z., Alias, H., & Wong, L. P. (2020). Influence
of mass and social media on psychobehavioral
responses among medical students during the
downward trend of Covid-19 in Fujian, China: Cross-
sectional study. Journal of Medical Internet Research,
22(7), 1-13. https://doi.org/10.2196/19982
Lucchetti, G., Goes, L.G., Amaral, S.G., Ganadjian, G. T.,
Andrade, I., Almeida, P. O. de A., do Carmo, V. M., &
Manso, M. E. G. (2020). Spirituality, religiosity and
mental health consequences of social isolation during
Covid-19 pandemic. International Journal of Social
Psychiatry. https://doi.org/10.1177/0020764020970
996
Ma’ruf, M. (2010). Pedoman umum mitigasi bencana.
Pedoman Umum Mitigasi Bencana, 1-54.
Martin, A., Kilpatrick, M., Scott, J., Cocker, F., Dawkins,
S., Brough, P., Sanderson, K. (2020). Protecting the
mental health of small-to-medium enterprise owners,
Journal of Occupational and Environmental Medicine,
62(7), 503-510. https://doi.org.10.1097/JOM.0000000
000001882
Matto, H. C., & Sullivan, K. (2021). Ashes2Art:
Mitigation strategies for short- and long-term distress
in emergency services personnel during Covid-19.
Clinical Social Work Journal, Yancy 2020.
https://doi.org/10.1007/s10615-021-00797-w
Momoi, M., Murakami, M., Horikoshi, N., & Maeda, M.
(2020). Dealing with community mental health post
the Fukushima disaster: Lesson learnt for the Covid-19
pandemic. Ojm, 113(11), 787-788. https://doi.org/
10.1093/qjmed/hcaa213
Niode, D. F., Rindengan, Y. D. Y., & Karouw, S. D.
(2016). Geographical information system (GIS) untuk
mitigasi bencana alam banjir di Kota Manado. Jurnal
Teknik Elektro dan Komputer, 5(2), 14-20
Otu, A., Charles, C. H., & Yaya, S. (2020). Mental health
and psychosocial well-being during the COVID-19
pandemic. International Journal of Mental Health
Systems, 14(1), 1-5. https://doi.org/10.1186/s13033-
020-00371-w
Power, E., Hughes, S., Cotter, D., & Cannon. M. (2020).
Youth mental health in the time of COVID-19. Irish
Journal of Psychological Medicine, 37(4), 301-305.
https://doi.org/10.1017/ipm.2020.84
Ribeiro, E., Sampaio, A., Gonçalves, M. M., Taveira, M.
D. C., Cunha, J., Maia, Â, Matos, M., Gonçalves, S.
Disaster Mitigation Strategies to Maintain Mental Health Stability in Society Facing Covid-19 Pandemic: A Systematic Review
101

Figueiredo, B., Freire, T., & Soares, T. (2021)
Telephone-based psychological crisis intervention: the
Portuguese experience with COVID-19, Counselling
Psychology Quarterly, 34(3-4), 432-446,
https://doi.org/10.1080/09515070.2020.1772200
Ridlo, I. A. (2020). Pandemi Covid-19 dan tantangan
kebijakan kesehatan mental di Indonesia. INSAN
Jurnal Psikologi dan Kesehatan Mental, 5(2), 162.
https://doi.org/10.20473/jpkm.v5i22020.162-171
Ross, H. O., Hasanah, M., & Kusumaningrum F. A.
(2020). Implementasi konsep sahdzan (sabar dan
huznudzan) sebagai upaya perawatan kesehatan
mental di masa pandemic Covid-19. Khazanah: Jurnal
Mahasiswa, 12(1). https://doi.org/10.20885/khazanah.
vol12.iss1.art7
Santoso, M. B. (2016). Kesehatan mental dalam perspektif
pekerjaan sosial. Share: Social Work Journal, 6(1).
https://doi.org/10.24198/share.v6i1.13160
Sheek-Hussein, M., Abu-Zidan, F. M., & Stip, E. (2021).
Disaster management of the psychosocial impact of
the Covid-19 pandemic. International of Emergency
Medicine, 14(1), 1-10. https://doi.org/10.1186/s12245-
021-00342-z
Skilbeck, L., Spanton, C., & Roylance, I. (2020). Beyond
the COVID-19 pandemic: ’Learning the hard way’-
adapting long-Term IAPT service provision using
lessons from past outbreaks. Cognitive Behaviour
Therapist, 13(2020), 1–12. https://doi.org/10.1017/
S1754470X20000379
Smith, P. M., Oudyk, J., Potter, G., & Mustard, C. (2021).
The association between the perceived adequacy of
workplace infection control procedures and personal
protective equipment with mental health symptoms: A
cross-sectional survey of canadian health-care workers
during the covid-19 pandemic. Canadian Journal of
Psychiatry, 66(1), 17–24. https://doi.org/10.1177/
0706743720961729
Soklaridis, S., Lin, E., Lalani, Y., Rodak, T., &
Sockalingam, S. (2020). Mental health interventions
and supports during covid-19 and other medical
pandemics: A rapid systematic review of the evidence.
General Hospital Psychiatry, 66, 133-146.
Sunarti, V. (2014). Peranan pendidikan luar sekolah dalam
rangka mitigasi bencana. Spektrum: Jurnal Pendidikan
Luar Sekolah (PLS), 2(2). https://doi.org/10.24036/
spektrumpls.v2i2.5044
Suyadi., Nuryana, Z., & Fauzi, N.A.F. (2020). The fiqh of
disaster: The mitigation of Covid-19 in the perspective
of Islamic education-neuroscience. International
Journal of Disaster Risk Reduction, 51, 1-9.
https://doi.org/10.1016/j.ijdrr.2020.101848
United Nations. (2020). Policy brief: Covid-19 and the
need for action on mental health. Policy Brief:
COVID-19 and the Need for Action on Mental Health,
1–17.
Vigo, D., Patten, S., Pajer, K., Krausz, M., Taylor, S.,
Rush, B., Raviola, G., Saxena, S.,Thornicroft, G., &
Yatham, L. N. (2020). Mental health of communities
during the Covid-19 pandemic. Canadian Journal of
Psychiatry, 65(10), 681–687. https://doi.org/10.1177/
0706743720926676
Vinkers, C. H., van Amelsvoort, T., Bisson, J. I., Branchi,
I., Cryan, J. F., Domschke, K., Howes, O. D.,
Manchia, M., Pinto, L., de Quervain, D., Schmidt, M.
V., & van der Wee, N. J. A. (2020). Stress resilience
during the coronavirus pandemic. European
Neuropsychopharmacology, 35, 12-16.
https://doi.org/10.1016/j.euroneuro.2020.05.00 3
Wang, S., Mak, H. W., & Fancourt, D. (2020). Arts,
mental distress, mental health functioning & life
satisfaction: Fixed-effects analyses of a nationally-
representative panel study. BMC
Public Health, 20(1), 1–9. https://doi.org/10.1186/s12889-
019-8109-y
WHO. (2020). Mental health and psychosocial
considerations during covid-19 outbreak. World
Health Organization, January, 1–6.
Winurini, S. (2019). Hubungan religiusitas dan kesehatan
mental pada remaja pesantren di Tabanan. Aspirasi:
Jurnal Masalah-Masalah Sosial, 10(2), 139–
153.https://doi.org/10.46807/aspirasi.v10i2.1428
World Health Organization. (2020). Covid-19 situation
report. World Health Organization, 31(2), 61–66.
Xu, C., Gong, X., Fu, W., Xu, Y., Xu, H., Chen, W., & Li,
M. (2020). The role of career adaptability and
resilience in mental health problems in Chinese
adolescents. Children and Youth Services Review,
112(30), 104893. https://doi.org/10.1016/j.child
youth.2020.1048 93
Zhang, Y., Zhang, H., Ma, X., & Di, Q. (2020). Mental
health problems during the Covid-19 pandemics and
the mitigation effects of exercise: A longitudinal study
of college students in China. International Journal of
Environmental Research and Public Health, 17(10).
https://doi.org/10.3390/ijerph17103722
ICPsyche 2021 - International Conference on Psychological Studies
102
