
Comparison of Obesity Indices in Predicting Diabetes Mellitus, Heart
Disease, Chronic Kidney Disease, and High Blood Pressure among
Adults in Kalimantan, Indonesia
Ayunina Rizky Ferdina
a
and Wulan Sari Rasna Giri Sembiring
b
Tanah Bumbu Unit of Health Research and Development, National Institute of Health Research and Development
Indonesia
Keywords: Waist-to-Height Ratio, obesity, Waist Circumference, Body Mass Index, chronic diseases
Abstract: There has been evolving evidence that waist-to-height ratio (WtHR) may be a better obesity index compared
to body mass index (BMI) and waist circumference (WC). We would like to compare the performance of
those indices in identifying the risk of several chronic diseases among the adult population in Kalimantan,
Indonesia. This is a cross-sectional study using data from the latest Basic Health Research (Riskesdas).
Multivariate logistic regression analysis was performed to investigate the odds ratios (OR) relating three
obesity indices (BMI, WC, and WtHR) to diabetes mellitus (DM), heart disease, chronic kidney disease
(CKD), and high blood pressure (HBP). High WtHR (>0.5) was found to have significant relationships with
the aforementioned diseases. Among the investigated indices, high WtHR had the highest OR in relation to
DM (3.365; 95% CI 2.707-4.182), CKD (1.935; 95% CI 1.309-2.861), and HBP (2.008; 95% CI 1.866-2.160).
Its OR for heart disease (1.549; 95% CI 1.247-1924) was just slightly lower than the OR of high WC (1.589;
95% CI 1.277-1.979). Meanwhile, BMI was significant only for DM and HBP. High BMI consistently showed
the lowest OR values among the three indices. These results suggest that chronic diseases can be predicted
better by the measurement of WtHR.
1 INTRODUCTION
Obesity can be defined as excessive fat accumulation
that may impair health (World Health Organisation
(WHO), 2006). Indonesia is experiencing a severe
problem of double burden of malnutrition due to the
rise of obesity and overweight (Popkin, Corvalan and
Grummer-Strawn, 2020). According to data from the
biggest national health survey, Riskesdas or the Basic
Health Research year 2007 and 2018, the prevalence
of general and central obesity had been increasing by
over 10% (Kementerian Kesehatan RI, 2007, 2018).
Kalimantan, referring to the Indonesian part of
Borneo Island, follows a similar trend. The
prevalence of general and central obesity in two of its
provinces, North and East Kalimantan, are bigger
than the national prevalence (Kementerian Kesehatan
RI, 2018).
Consequently, the rise of non-communicable
chronic diseases or NCDs in the region should also
a
https://orcid.org/0000-0001-9025-9689
b
https://orcid.org/0000-0003-1552-183X
be anticipated. The Framingham Heart Study
showed obesity as an independent risk factor for
cardiovascular diseases (Hubert, Mcnamara and
Castelli, 1983). Obesity status is traditionally
determined by calculating body mass index (BMI).
However, other anthropometric measures reflecting
abdominal adiposity have been endorsed as being
superior to BMI in predicting the risk of
cardiovascular diseases (CVD) (World Health
Organisation (WHO), 2008). This is based basically
on the justification that increased visceral adipose
tissue is related to a range of metabolic
abnormalities which become the risk factors for type
2 diabetes and CVD (Frank et al., 2019).
Waist circumference (WC) as the discriminator
of central obesity is shown to be a reliable proxy of
visceral adiposity across a wide age range in a
population with a high incidence of metabolic
syndrome (Onat et al., 2004). Central obesity is
officially recognized as a core component in
100
Ferdina, A. and Sembiring, W.
Comparison of Obesity Indices in Predicting Diabetes Mellitus, Heart Disease, Chronic Kidney Disease, and High Blood Pressure among Adults in Kalimantan, Indonesia.
DOI: 10.5220/0010759900003235
In Proceedings of the 3rd International Conference on Social Determinants of Health (ICSDH 2021), pages 100-105
ISBN: 978-989-758-542-5
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

diagnosing metabolic syndrome (International
Diabetes Foundation, 2006).
More recent studies have found that waistline
measurement shows better correlations with chronic
diseases when used in conjunction with body height,
which also became the hypothesis of our present
study. Waist-to-height ratio (abbreviated as WtHR,
WHtR, or W/Ht) with a general cut-off value of 0.5
has been proposed as a novel obesity index (Ashwell
and Gibson, 2014). This study would like to compare
the three obesity indices, namely BMI, WC, and
WtHR; in predicting the risk of several chronic
diseases that are increasingly prevalent in
Kalimantan, Indonesia.
2 METHODS
2.1 Study Design and Population
This is a cross-sectional study using secondary data
from the latest Basic Health Research (Riskesdas
2018) directed by the Ministry of Health of Indonesia.
The population of interest was adults residing in
Kalimantan, Indonesia. The sample in this study was
adults aged 18 years old and older in Kalimantan who
were selected as the 2018 Riskesdas participants and
met the inclusion criteria. The inclusion criteria were
adults aged > 18 years whose blood pressure was
measured at least once and answered survey questions
about their chronic disease history. Since we would
like to compare differences associated with obesity
status, all pregnant respondents were purposively
excluded in this study.
2.2 Data Collection
All subjects were interviewed and physically
examined for survey purposes. The interview
included questions about whether they had been
diagnosed having certain diseases, such as diabetes
mellitus, heart disease, and chronic kidney disease.
Measurement of blood pressure, body weight, body
height, and waist circumference (WC) were part of
the physical examination.
2.3 Variables
High BMI is defined following the Asia-Pacific
definition for general obesity, which is having a
body mass index (BMI) > 25 kg/m
2
(Kanazawa et
al., 2005). High WC is defined according to the
central obesity criteria for the South Asian ethnic
group, which is WC > 90 cm for men and > 80 cm
for women (International Diabetes Foundation,
2006). Waist-to-Height Ratio (WtHR) is calculated
by dividing the WC by the body height. High WtHR
is defined as WtHR > 0.5 (Browning, Hsieh, and
Ashwell, 2010).
Diabetes mellitus (DM), heart disease, and
chronic kidney disease (CKD) are determined by the
relevant report provided by the subjects for the
interview on the questions about their history of
being diagnosed with the aforementioned diseases.
High blood pressure (HBP) is defined as having
systolic blood pressure > 140 mmHg and/or
diastolic blood pressure > 90 mmHg when
examined in the Riskesdas survey (Kementerian
Kesehatan RI, 2018).
2.4 Ethical Consideration
For the primary data collection of Riskesdas 2018,
the Ethical Committee of Health Research, NIHRD,
Ministry of Health of Indonesia had given their
approval with the reference number
LB.02.01/2/KE.267/2017. All subjects were asked
for their consent and signed the informed consent
form in the survey. No additional ethical clearance
is required for secondary analysis of the obtained
data.
2.5 Statistical Analysis
The statistical analyses were performed using the
International Business Machines Statistical Package
for the Social Sciences (IBM SPSS) version 25.
Multivariate logistic regression analyses with a
complex samples analysis design were performed to
calculate the odds ratios (OR) relating obesity status
to DM, heart disease, chronic kidney disease (CKD),
and HBP.
3 RESULTS
Subjects included in this study had a total number of
61,140. The prevalence of general obesity, central
obesity, and high WtHR among the subjects who
were recorded as having DM, heart disease, CKD,
and HBP are presented in Table 1. Over 60% of
subjects who suffered any disease of concern were
categorized as having high WtHR. On the other hand,
only up to 55.5% were categorized as having central
or general obesity.
Comparison of Obesity Indices in Predicting Diabetes Mellitus, Heart Disease, Chronic Kidney Disease, and High Blood Pressure among
Adults in Kalimantan, Indonesia
101
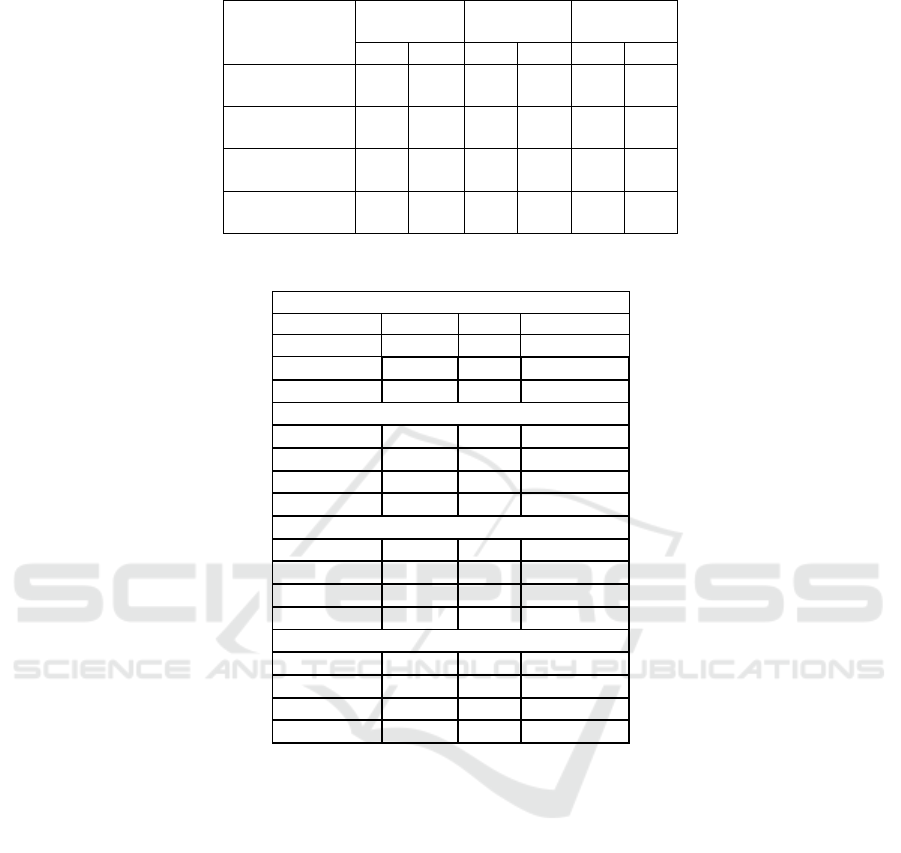
Table 1: Percentages of obesity status of subjects having DM, heart disease, CKD, and HBP.
WtHR
>= 0.5
Central
obesit
y
General
Obesity
Yes No Yes No Yes No
DM
(
n = 1,320
)
78.1 21.9 55.5 44.5 45.5 54.5
Heart disease
(
n = 1,143
)
67.3 32.7 47.4 52.6 44.4 55.6
CKD
(n = 270)
62.2 37.8 35.2 64.8 36.7 63.3
HBP
(
n = 13,763
71.2 28.8 48.7 51.3 29.4 70.6
Table 2: Multivariate analysis between DM, heart disease, CKD, and HBP with obesity indices
*)
.
DM
Variable
p
-value OR 95% CI
Hi
g
h WtHR < 0.001 3.365 2.707-4.182
Hi
g
h WC < 0.001 1.800 1.470-2.205
High BMI < 0.001 0.611 0.509-0.734
Heart disease
Variable
p
-value OR 95% CI
Hi
g
h WtHR < 0.001 1.549 1.247-1.924
Hi
g
h WC < 0.001 1.589 1.277-1.979
Hi
g
h BMI 0.725 0.964 0.786-1.183
CKD
Variable
p
-value OR 95% CI
High WtHR 0.001 1.935 1.309-2.861
High WC 0.543 1.140 0.747-1.740
Hi
g
h BMI 0.116 0.717 0.473-1.085
HBP
Variable
p
-value OR 95% CI
High WtHR < 0.001 2.008 1.866-2.160
High WC < 0.001 1.440 1.341-1.546
High BMI < 0.001 1.367 1.277-1.464
*)
Reference category for each index:
WtHR: < 0.5
WC: < 90 cm for men, < 80 cm for women
BMI: < 25
Table 2 shows that WtHR was the only index
showing significant relationships with all the
aforementioned diseases (p-value < 0.001 except for
CKD). Compared to other indices, high WtHR also
had the highest OR in relation to DM (3.365; 95% CI
2.707-4.182), CKD (1.935; 95% CI 1.309-2.861), and
HBP (2.008; 95% CI 1.866-2.160). Its OR for heart
disease (1.549; 95% CI 1.247-1.924) was just slightly
lower than the OR of high WC (1.589; 95% CI 1.277-
1.979). Meanwhile, the ORs from high BMI were
consistently the lowest among the three indices.
General obesity also showed negative associations
(OR < 1) for the concerned diseases except in relation
to HBP (Table 2).
4 DISCUSSION
Hypertension is known to happen more commonly in
obese than in lean individuals at practically every age
(Thakur, Richards and Reisin, 2001). Obesity status,
especially central obesity, increases sodium
reabsorption in the kidneys and affects the renin-
angiotensin-aldosterone hormone production system
that regulates blood pressure (Hall, 2003). In our
analyses, high BMI showed a positive association
(OR > 1) only with HBP. There is indeed a significant
linear relationship between blood pressure and BMI
found among Indonesian population (Peltzer and
Pengpid, 2018). It has also been established general
ICSDH 2021 - International Conference on Social Determinants of Health
102

and central obesity were associated with hypertension
in Indonesian women (Nurdiantami et al., 2018).
However, BMI alone is not appropriate to
properly assess the cardiometabolic risk associated
with increased adiposity in adults (Ross et al., 2020).
In those who are not classified as obese based on
BMI, abdominal fat accumulation is associated with
HBP and predisposes people to diseases associated
with metabolic syndrome (Frank et al., 2019).
Looking at the subjects having HBP in our present
study, only less than a third of them were categorized
as having high BMI (Table 1). Additionally, our
analysis showed that with ORs < 1, high BMI failed
to predict the occurrence of DM, heart disease, and
CKD.
Although BMI is popularly used to describe
obesity, WC has emerged as a more specific indicator
of metabolic risk. Centralized obesity measures,
especially WtHR, have been proved to be superior to
BMI for detecting cardiovascular risk factors (Lee et
al., 2008; Schneider et al., 2010). Not only it does not
differentiate between lean and fat mass, but BMI also
does not indicate the distribution of the body fat. For
assessing obesity, BMI has high specificity but low
sensitivity (Okorodudu et al., 2010).
The result from our analyses shows that
concerning heart disease, WC was the best predictor
while WtHR performed just almost the same based on
their ORs (Table 2). Prospective studies and meta-
analyses of adults have revealed that the WtHR is
comparable to WC and superior to BMI in predicting
advanced cardiometabolic risk (Yoo, 2016).
Unfortunately, WC and BMI do not have
universal obesity thresholds. They are ethnic-
specific, while WC is gender-specific as well. The
boundary values are relatively lower for the Asian
population. As such, Asians pose a higher risk of
getting diabetes and dying prematurely at lower levels
of BMI and WC, from cardiovascular problems
(Naser, Gruber and Thomson, 2006). Use of Asian
BMI threshold improved detection of DM and
hypertension in Filipino-American women (Battie et
al., 2016).
WtHR has been endorsed as a novel obesity index
with a cut-off value of 0.5 that can be applied
globally, across age groups and genders (Ashwell and
Hsieh, 2005; Browning, Hsieh and Ashwell, 2010;
Ashwell, Gunn and Gibson, 2012; Ashwell and
Gibson, 2016). Besides its simple boundary value, it
is more sensitive than BMI or WC alone to evaluate
clustering of coronary risk factors among non-obese
men and women (Hsieh and Muto, 2005). WtHR also
performed better than BMI and WC for the
association with hypertension and diabetes (Cai et al.,
2013). Table 1 shows that people having history of
DM, heart disease, CKD, or HBP were dominated by
those having high WtHR.
This index was shown to be the best
anthropometric measure than BMI and WC in
identifying the risk of diabetes among Indonesian
population and suitable for both genders (Djap et al.,
2018). In our present analyses, WtHR was superior
not only to BMI but also to WC in predicting the risk
of DM, CKD, and HBP.
Another remark from our study is that WtHR was
found to be the only index having a significant
relationship with CKD. Although the biological
mechanism is not fully understood, obesity is a risk
factor for the development and progression of kidney
disease. It may promote kidney damage directly over
hormonal and hemodynamic effects or indirectly by
favoring the progress of diabetes and hypertension,
and disorders with strong kidney involvement (Wang
et al., 2008). A cohort study of hypertensive patients
found that overweight and obesity were associated
with a 20–40% increased risk for the development of
CKD (Kramer et al., 2005). A recent meta-analysis
reported that WtHR appears to be the best predictor
of CKD compared to other physical measurements
(Liu et al., 2019).
With these findings of the usefulness of WtHR as
an index for obesity, keeping waistline to be less than
half of the body height is worth being a treatment
target in preventing adverse health risks for adults.
Dietary interventions, as well as routine, moderate-
intensity exercise, have been suggested to reduce WC
(Ross et al., 2020) and ultimately, WtHR.
5 CONCLUSION
Our results suggest that chronic diseases can be
predicted better by the measurement of WtHR. WtHR
has better performance than BMI and WC in
identifying the risk of developing DM, CKD, and
HBP; while for identifying the risk of heart disease,
its performance was similar to WC. Despite its
widespread use, BMI was found to be a weak
predictor of chronic diseases as it only showed a
positive correlation with HBP but not with other
chronic diseases of interest. We support the measures
of centralized obesity, especially WtHR, to detect the
risk of non-communicable chronic diseases.
Comparison of Obesity Indices in Predicting Diabetes Mellitus, Heart Disease, Chronic Kidney Disease, and High Blood Pressure among
Adults in Kalimantan, Indonesia
103

REFERENCES
Ashwell, M. and Gibson, S. (2014) ‘A proposal for a
primary screening tool: “Keep your waist
circumference to less than half your height”’, BMC
Medicine, 12(1), pp. 1–6. doi: 10.1186/s12916-014-
0207-1.
Ashwell, M. and Gibson, S. (2016) ‘Waist-to-height ratio
as an indicator of early health risk: Simpler and more
predictive than using a matrix based on BMI and waist
circumference’, BMJ Open, 6(3), p. 10159. doi:
10.1136/bmjopen-2015-010159.
Ashwell, M., Gunn, P. and Gibson, S. (2012) ‘Waist-to-
height ratio is a better screening tool than waist
circumference and BMI for adult cardiometabolic risk
factors: Systematic review and meta-analysis’, Obesity
Reviews. John Wiley & Sons, Ltd, pp. 275–286. doi:
10.1111/j.1467-789X.2011.00952.x.
Ashwell, M. and Hsieh, S. D. (2005) ‘Six reasons why the
waist-to-height ratio is a rapid and effective global
indicator for health risks of obesity and how its use
could simplify the international public health message
on obesity’, International Journal of Food Sciences and
Nutrition, 56(5), pp. 303–307. doi:
10.1080/09637480500195066.
Battie, C. A. et al. (2016) ‘Comparison of body mass index,
waist circumference, and waist to height ratio in the
prediction of hypertension and diabetes mellitus:
Filipino-American women cardiovascular study’,
Preventive Medicine Reports, 4, pp. 608–613. doi:
10.1016/j.pmedr.2016.10.003.
Browning, L. M., Hsieh, S. D. and Ashwell, M. (2010) ‘A
systematic review of waist-to-height ratio as a
screening tool for the prediction of cardiovascular
disease and diabetes: 05 could be a suitable global
boundary value’, Nutrition Research Reviews, 23(2),
pp. 247–269. doi: 10.1017/S0954422410000144.
Cai, L. et al. (2013) ‘Waist-to-Height Ratio and
Cardiovascular Risk Factors among Chinese Adults in
Beijing’, PLoS ONE, 8(7), p. 69298. doi:
10.1371/journal.pone.0069298.
Djap, H. S. et al. (2018) ‘Waist to height ratio (0.5) as a
predictor for prediabetes and type 2 diabetes in
Indonesia’, in IOP Conference Series: Materials
Science and Engineering. Institute of Physics
Publishing, p. 012311. doi: 10.1088/1757-
899X/434/1/012311.
Frank, A. P. et al. (2019) ‘Determinants of body fat
distribution in humans may provide insight about
obesity-related health risks’, Journal of Lipid Research.
American Society for Biochemistry and Molecular
Biology Inc., pp. 1710–1719. doi:
10.1194/jlr.R086975.
Hall, J. E. (2003) ‘The Kidney, Hypertension, and Obesity’.
doi: 10.1161/01.HYP.0000052314.95497.78.
Hsieh, S. D. and Muto, T. (2005) ‘The superiority of waist-
to-height ratio as an anthropometric index to evaluate
clustering of coronary risk factors among non-obese
men and women’, Preventive Medicine, 40(2), pp. 216–
220. doi: 10.1016/j.ypmed.2004.05.025.
Hubert, H. B., Mcnamara, P. M. and Castelli, W. P. (1983)
‘Obesity as an Independent Risk Factor for
Cardiovascular Disease: A 26-year Follow-up of
Participants in the Framingham Heart Study’,
Circulation, 67(5), pp. 968–976. Available at:
http://ahajournals.org (Accessed: 18 June 2021).
International Diabetes Foundation (2006) ‘The IDF
consensus worldwide definition of the Metabolic
Syndrome’. doi: 10.1159/000282084.
Kanazawa, M. et al. (2005) ‘Criteria and classification of
obesity in Japan and Asia-Oceania.’, World review of
nutrition and dietetics. World Rev Nutr Diet, pp. 1–12.
doi: 10.1159/000088200.
Kementerian Kesehatan RI (2007) ‘Laporan Nasional
Riskesdas 2007’, Laporan Nasional 2007, pp. 1–384.
Available at:
http://kesga.kemkes.go.id/images/pedoman/Riskesdas
2007 Nasional.pdf.
Kementerian Kesehatan RI (2018) Laporan Nasional
Riskesdas 2018.
Kramer, H. et al. (2005) ‘Obesity and prevalent and
incident CKD: The hypertension detection and follow-
up program’, American Journal of Kidney Diseases,
46(4), pp. 587–594. doi: 10.1053/j.ajkd.2005.06.007.
Lee, C. M. Y. et al. (2008) ‘Indices of abdominal obesity
are better discriminators of cardiovascular risk factors
than BMI: a meta-analysis’, Journal of Clinical
Epidemiology. Elsevier, pp. 646–653. doi:
10.1016/j.jclinepi.2007.08.012.
Liu, L. et al. (2019) ‘Waist height ratio predicts chronic
kidney disease: A systematic review and meta-analysis,
1998-2019’, Archives of Public Health, 77(1). doi:
10.1186/s13690-019-0379-4.
Naser, K. A., Gruber, A. and Thomson, G. A. (2006) ‘The
emerging pandemic of obesity and diabetes: Are we
doing enough to prevent a disaster?’, International
Journal of Clinical Practice. John Wiley & Sons, Ltd,
pp. 1093–1097. doi: 10.1111/j.1742-
1241.2006.01003.x.
Nurdiantami, Y. et al. (2018) ‘Association of general and
central obesity with hypertension.’, Clinical nutrition
(Edinburgh, Scotland), 37(4), pp. 1259–1263. doi:
10.1016/j.clnu.2017.05.012.
Okorodudu, D. O. et al. (2010) ‘Diagnostic performance of
body mass index to identify obesity as defined by body
adiposity: A systematic review and meta-analysis’,
International Journal of Obesity. Int J Obes (Lond), pp.
791–799. doi: 10.1038/ijo.2010.5.
Onat, A. et al. (2004) ‘PAPER Measures of abdominal
obesity assessed for visceral adiposity and relation to
coronary risk’, International Journal of Obesity, 28, pp.
1018–1025. doi: 10.1038/sj.ijo.0802695.
Peltzer, K. and Pengpid, S. (2018) ‘The Prevalence and
Social Determinants of Hypertension among Adults in
Indonesia: A Cross-Sectional Population-Based
National Survey’, International Journal of
Hypertension, 2018. doi: 10.1155/2018/5610725.
Popkin, B. M., Corvalan, C. and Grummer-Strawn, L. M.
(2020) ‘Dynamics of the double burden of malnutrition
and the changing nutrition reality’, The Lancet. Lancet
ICSDH 2021 - International Conference on Social Determinants of Health
104

Publishing Group, pp. 65–74. doi: 10.1016/S0140-
6736(19)32497-3.
Ross, R. et al. (2020) ‘Waist circumference as a vital sign
in clinical practice: a Consensus Statement from the
IAS and ICCR Working Group on Visceral Obesity’,
Nature Reviews Endocrinology, 16(3), pp. 177–189.
doi: 10.1038/s41574-019-0310-7.
Schneider, H. J. et al. (2010) ‘The Predictive Value of
Different Measures of Obesity for Incident
Cardiovascular Events and Mortality’, J Clin
Endocrinol Metab, 95(4), pp. 1777–1785. doi:
10.1210/jc.2009-1584.
Thakur, V., Richards, R. and Reisin, E. (2001) ‘Obesity,
hypertension, and the heart’, in American Journal of the
Medical Sciences. Lippincott Williams and Wilkins, pp.
242–248. doi: 10.1097/00000441-200104000-00005.
Wang, Y. et al. (2008) ‘Association between obesity and
kidney disease: A systematic review and meta-
analysis’, Kidney International. Nature Publishing
Group, pp. 19–33. doi: 10.1038/sj.ki.5002586.
World Health Organisation (WHO) (2006) Obesity and
overweight. Available at:
https://www.who.int/en/news-room/fact-
sheets/detail/obesity-and-overweight (Accessed: 24
June 2021).
World Health Organisation (WHO) (2008) ‘WHO | Waist
Circumference and Waist–Hip Ratio. Report of a WHO
Expert Consultation. Geneva, 8-11 December 2008.’,
(December), pp. 8–11. Available at:
http://www.who.int.
Yoo, E. G. (2016) ‘Waist-to-height ratio as a screening tool
for obesity and cardiometabolic risk’, Korean Journal
of Pediatrics. Korean Pediatric Society, pp. 425–431.
doi: 10.3345/kjp.2016.59.11.425.
Comparison of Obesity Indices in Predicting Diabetes Mellitus, Heart Disease, Chronic Kidney Disease, and High Blood Pressure among
Adults in Kalimantan, Indonesia
105
