
Federated Learning in Healthcare is the Future, But the Problems
Are Contemporary
Mustafa Y. Topaloglu
1
, Elisabeth M. Morrell
1
and Umit Topaloglu
2
a
1
Department of Computer Science, Wake Forest University, Winston Salem, NC, 27109, U.S.A.
2
Departments of Cancer Biology and Biostatistics, Wake Forest School of Medicine, Winston Salem, NC, 27157, U.S.A.
Keywords: Federated Learning, Machine Learning, Privacy, Machine Learning Ethics, Machine Learning Legal Issues.
Abstract: Federated Learning (FL) has originated out of a need to mitigate certain inherent limitations of ML,
particularly the capability to train on larger datasets for improved performance, which is typically an unwieldy
coordination for an inter-institutional collaboration due to existing patient protection laws and regulations. FL
may also play a crucial role in bypassing ML’s innate algorithmic discrimination issues via the access of
underrepresented groups’ data spanning across geographically distributed institutions and the diverse
populations. FL inherits many of the difficulties of ML and as such we have discussed two pressing FL
challenges, namely: privacy of the model exchange as well as equity and contribution considerations.
1 INTRODUCTION
Machine Learning (ML) is poised to provide an
incomparable opportunity to overcome the traditional
paradigms of the healthcare (Griffin et al., 2020;
Topol, 2019). However, data availability and
underrepresentation of minorities in healthcare
datasets are traditionally accepted disadvantages to
ML research(Obermeyer et al., 2019) and lead to
relatively low performance for disproportionately
represented ethnic and minority groups due to bias
that the model might develop(Gao & Cui, 2020).
Correspondingly, the training data from these
populations result in distribution discrepancies that
are highly susceptible to biases. Problems that arise
from data heterogeneity, depth, and breadth are a
hindrance to the generalization of ML approaches.
Given the data intensive nature of model training,
Federated Learning (FL) approaches may provide a
novel opportunity for the future of ML
applications(Rajendran et al., 2021; Sarma et al.,
2021). FL is a collaborative ML training approach
illustrated in Figure 1.
FL has recently received a greater emphasis in
recent years due to its privacy preserving potential in
healthcare despite certain structural issues which
necessitate an address. Characteristic of many recent
a
https://orcid.org/0000-0002-3241-8773
advancements, the Friedman curve indicates that
technological advancement has overtaken present
human governing capacity, and the only way to
bridge the gap in the case of FL is through the
introduction of rapid problem identification and
prudent regulation of FL and cooperation from the
public and private sector respectively(Friedman,
2016).
Figure 1: Federated Learning Overview.
Protected Health Information (PHI) is covered by the
Health Insurance Portability and Accountability Act
(HIPAA). Due to existing risk for FL models as
shown by attacks, it would be appropriate to classify
the model under the definition of PHI, as there is a
Topaloglu, M., Morrell, E. and Topaloglu, U.
Federated Learning in Healthcare is the Future, But the Problems Are Contemporary.
DOI: 10.5220/0010722600003058
In Proceedings of the 17th International Conference on Web Information Systems and Technologies (WEBIST 2021), pages 593-598
ISBN: 978-989-758-536-4; ISSN: 2184-3252
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
593

risk of the model itself containing the PHI of patients.
This classification would be beneficial to the overall
security of FL on account of the HIPAA Security
Rule which outlines specific guidelines for the
utilization, employment, and protection of PHI.
2 CHALLENGES
Among the issues, training data variations due to data
types and their capture quality make data preparation
salient to the success of the endeavor. Some of the
most relevant clinical information may not be
accessible or be recorded incorrectly in a way that is
not representative of the studied population or
missing. Moreover, data quality challenges in
healthcare are an acknowledged barrier to research in
general and ML in particular, however it is not within
the scope of this work. Despite the perceived and
studied benefits, there are some challenges for wider
implementation and acceptance of FL that can be
categorized in two: privacy and equity and
contribution considerations.
2.1 Privacy
The purpose of Federated Learning is to train
machine learning models while preserving the
privacy of individual contributors. However, the
models are capable of unintentionally revealing
sensitive information, therefore the security and
privacy of FL has become an area of extensive
research (Beaulieu-Jones et al., 2018; Duan et al.,
2020; Hitaj et al., 2017; Li et al., 2019). The main
methods of protecting training data in the FL process
are differential privacy, model encryption,
blockchain based computing, and homomorphic
encryption.
Differential privacy is performed by randomly
perturbing the parameters of the local model with
noise (e.g., Gaussian noise, Laplacian noise) before
communicating with and incorporating into the global
model (Li et al., 2020). Model encryption is
accomplished by encrypting the parameters of the
global model before they are sent to local data
collection for training. Local models are
communicated back to the global model with
encrypted local gradients (Lu, 2021). Homomorphic
encryption is implemented by computing on
encrypted models (Kim et al., 2018).
Despite the improvements in security, FL privacy
methods continue to prove vulnerable to attacks.
These breaches and data leaks fit into two main
categories: inference during the learning process, and
inference over the output(Truex et al., 2019). In
general, the more overfitted the model is to its
training data, the more vulnerable it is to an
attack(Shokri et al., 2017).
While troubleshooting these flaws in the FL
process, new research shows that a variety of privacy
features can prove a suitable defense (Beaulieu-Jones
et al., 2018; Li et al., 2020; Li et al., 2019; Shokri &
Shmatikov, 2015; Truex et al., 2019; Wei et al.,
2020).
In some cases, research will stray from the
centralized FL system and perform all model training
decentralized as an additional security measure. For
example, Swarm Learning (SL) builds ML models
from local data. These models never leave the host
site and instead the learning parameters are shared via
blockchain with other local models. After the arrival
of new parameters, the local models train with the
new parameters until standards for synchronization
are met. Each contributing site has locally installed
nodes which are responsible for building and
synchronizing models and implementing the
blockchain (Warnat-Herresthal et al., 2021).
Blockchain provides a secure distributed ledger-
based computing framework that has started to show
promise in healthcare(Norgeot et al., 2019). Several
studies proposed a Blockchain implementation for
ML models to benefit security and privacy promised
by the Blockchain(Hathaliya et al., 2019; Vyas et al.,
2019). Despite the consensus of Blockchain being
very secure, its security level is directly correlated
with the hashing power an implementation may have.
Some of the known attacks on Blockchain include
Finney attack, race attack, 51% attack (i.e., majority
attack), eclipse attack, Sybil attack, routing attack,
Decentralized Autonomous Organization (DAO)
attack. Other than the 51% attack, the aforementioned
attacks depend on the implementation and may not be
very common. In spite of the numerous
vulnerabilities blockchain implementations produce,
methods to counter and mitigate the risks posed rely
on computationally expensive measures, which
entails an honest dialogue about the fruitfulness of
these models (Aggarwal & Kumar, 2021).
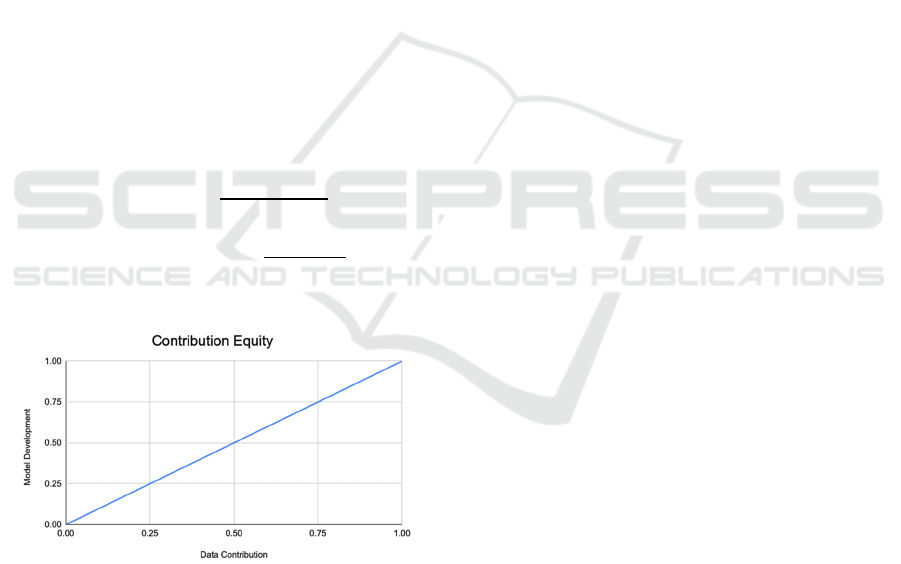
2.2 Equity and Contribution Valuation
A tradeoff for collaborating institutions exists
between the privacy of the data and the joint effort of
model development(Rieke et al., 2020). For example,
since the training data will be decentralized and if
there are two institutions developing a model, it
would be beneficial to have them coordinate on such
tasks as taking measurements. Potential solutions
DMMLACS 2021 - 2nd International Special Session on Data Mining and Machine Learning Applications for Cyber Security
594
could include having a restricted access for limited
amounts of coordinators in order to compromise, or
to simply decline sharing any information not
explicitly related to the model. Deciding between
lacking the ability to investigate the data or possible
privacy issues is a difficult dilemma. Due to the
unique and distributed nature of FL, it would be
advantageous to have a standard evaluation strategy
for purposes such as determining remuneration. The
Gini coefficient ("Gini Index," 2008), which
determines income inequality could be employed to
assess the contribution (figure 2). Even though the
Information Gain Function could be considered as an
alternative, Raileanu et al. have proved that the Gini
coefficient only disagrees by 2% with Information
Gain in all cases(Raileanu & Stoffel, 2004). In a
similar vein, we utilize two factors to determine the
level of participation: model development
contribution, and data contribution; formula (1) is for
the total contribution and (2) can be used to calculate
an individual site’s contribution.
Mi= Model development contribution level of ith site:
Mi ɛ ℝ = [0,1]
Di= Data contribution level of ith site: Di ɛ ℝ = [0,1]
𝑇𝑜𝑡𝑎𝑙 𝐶𝑜𝑛𝑡𝑟𝑖𝑏𝑢𝑡𝑖𝑜𝑛
∑
𝑀
𝐷
2∗𝑁
(1)
𝐶𝑜𝑛𝑡𝑟𝑖𝑏𝑢𝑡𝑖𝑜𝑛 𝑜𝑓 𝑖𝑡ℎ 𝑛𝑜𝑑𝑒
𝑀
𝐷
∑
𝑀
∑
𝐷
(2)
N= Number of participants in a FL framework
Figure 2: Contribution Equity representation for data and
model based on Gini Index.
2.2.1 Model Development Expertise (Mi)
Model development requires understanding the
problem domain with adequate subject matter
expertise and ability to translate that knowledge into
ML models. In classical ML algorithms, this involved
extracting features and designing a ML task (e.g.,
classifier). With Deep Learning, the initial feature
engineering can be done by the algorithms. Model
development can be broken into the three following
subcategories:
Model Development Cost: The Cost here refers to
such efforts as the labor behind the creation of the
algorithm until initial operating capacity and
implementation occur. This is a multifaceted
component, which will be able to leverage a certain
institution's healthcare informatics and data science
expertise if they lack significant Data Contribution.
Model Validation and Benchmarking Cost:
Without proper validation and benchmarking, the
algorithms cannot be integrated into clinical care[49].
Over the years, the machine learning community has
developed several statistical methods to properly
evaluate AI algorithms. The “intrinsic uncertainty” in
medicine introduces variations in result
interpretation, which suggest that model performance
criteria should be use case specific vs. using standard
scoring metrics[50].
Continuous Model Improvement Cost: The Model
itself will see countless iterations and frequent
evolution to accommodate new aspects and features.
The work put into the model after deployment will be
factored in accordingly to reward constant
improvements and reflect the reality of Model
Development.
3 CONCLUSION
Data and model privacy is essential for any FL
implementation in healthcare in order to realize its
potential. We have discussed current privacy
challenges and corresponding proposals to address
those deficiencies. We believe that none of the
proposed solutions have sufficient safeguards that is
practical to implement. Therefore, further studies and
solutions are needed for FL to strive.
Another identified challenge is the contribution
assessment and corresponding profit (or
responsibility) sharing among the FL participating
institutions. Unfortunately, there is no widely
accepted models for such collaboration. We have
proposed a conceptual model that relies on the Gini
coefficient. The model considers the model
development attributes that need to be taken into
account along with the data that each institutions
contributes. There are some proposed models for data
contribution but not for the model and data, to our
knowledge.
Upon addressing these challenges, we strongly
believe that FL will be widely accepted and
contribute to the biomedical advancements.
Federated Learning in Healthcare is the Future, But the Problems Are Contemporary
595

ACKNOWLEDGEMENTS
We would like to thank Drs. Can Bora Unal and Todd
Morrell for their invaluable feedback. The work is
partially supported by the Cancer Center Support
Grant from the National Cancer Institute to the
Comprehensive Cancer Center of Wake Forest
Baptist Medical Center (P30 CA012197). The
authors also acknowledge use of the services and
facilities, funded by the National Center for
Advancing Translational Sciences (NCATS),
National Institutes of Health (UL1TR001420).
REFERENCES
Aggarwal, S., & Kumar, N. (2021). Chapter Twenty -
Attacks on blockchain☆☆Working model. In S.
Aggarwal, N. Kumar, & P. Raj (Eds.), Advances in
Computers (Vol. 121, pp. 399-410). Elsevier.
https://doi.org/https://doi.org/10.1016/bs.adcom.2020.
08.020
Allen, B., Agarwal, S., Kalpathy-Cramer, J., & Dreyer, K.
(2019). Democratizing AI. Journal of the American
College of Radiology, 16(7), 961-963. https://
doi.org/10.1016/j.jacr.2019.04.023
Azoulay, A. Towards an Ethics of Artificial Intelligence.
Beaulieu-Jones, B. K., Yuan, W., Finlayson, S. G., & Wu,
Z. S. (2018). Privacy-Preserving Distributed Deep
Learning for Clinical Data. arXiv e-prints. Retrieved
December 01, 2018, from https://ui.adsabs.harvard.edu/
abs/2018arXiv181201484B
Bujalkova, M. (2001). Hippocrates and his principles of
medical ethics. Bratisl Lek Listy, 102(2), 117-120.
Caribbean, R. o. A. I. T. A. a. t. https://www.loc.gov/law/
help/artificial-intelligence/americas.php#us. Retrieved
February 2021 from
Char, D. S., Abràmoff, M. D., & Feudtner, C. (2020).
Identifying Ethical Considerations for Machine
Learning Healthcare Applications. Am J Bioeth, 20(11),
7-17. https://doi.org/10.1080/15265161.2020.1819469
Cheng, K., Fan, T., Jin, Y., Liu, Y., Chen, T., & Yang, Q.
(2019). SecureBoost: A Lossless Federated Learning
Framework. ArXiv, abs/1901.08755.
Cohen Healthcare. Artificial Intelligence and the Health
Insurance Portability and Accountability Act of 1996
(HIPAA),. Retrieved February, 2021 from
Duan, R., Boland, M. R., Liu, Z., Liu, Y., Chang, H. H., Xu,
H., Chen, Y. (2020). Learning from electronic health
records across multiple sites: A communication-
efficient and privacy-preserving distributed algorithm.
J Am Med Inform Assoc, 27(3), 376-385. https://
doi.org/10.1093/jamia/ocz199
Enterprise, T. C. f. O. D. (2019). Sharing and Utilizing
Health Data for AI Applications.
Esteva, A., Kuprel, B., Novoa, R. A., Ko, J., Swetter, S. M.,
Blau, H. M., & Thrun, S. (2017). Dermatologist-level
classification of skin cancer with deep neural networks.
Nature, 542(7639), 115-118. https://doi.org/10.1038/
nature21056
Evans, B., & Ossorio, P. (2018). The Challenge of
Regulating Clinical Decision Support Software After
21(st) Century Cures. Am J Law Med, 44(2-3), 237-251.
https://doi.org/10.1177/0098858818789418
FDA. Digital Health Software Precertification (Pre-Cert)
Program. Retrieved February, 2021 from
Friedman, T. (2016). Thank You for Being Late: an
Optimist's Guide to Thriving in the Age of
Accelerations. Farrar, Straus and Giroux.
Gao, Y., & Cui, Y. (2020). Deep transfer learning for
reducing health care disparities arising from biomedical
data inequality. Nature Communications, 11(1), 5131.
https://doi.org/10.1038/s41467-020-18918-3
Geis, J. R., Brady, A. P., Wu, C. C., Spencer, J., Ranschaert,
E., Jaremko, J. L., Kohli, M. (2019). Ethics of Artificial
Intelligence in Radiology: Summary of the Joint
European and North American Multisociety Statement.
Journal of the American College of Radiology, 16(11),
1516-1521. https://doi.org/10.1016/j.jacr.2019.07.028
Gini Index. (2008). In The Concise Encyclopedia of
Statistics (pp. 231-233). Springer New York. https://
doi.org/10.1007/978-0-387-32833-1_169
Griffin, A. C., Topaloglu, U., Davis, S., & Chung, A. E.
(2020). From Patient Engagement to Precision
Oncology: Leveraging Informatics to Advance Cancer
Care. Yearb Med Inform, 29(1), 235-242. https://
doi.org/10.1055/s-0040-1701983
Guidance, F. C. https://www.fda.gov/media/109618/
download. Retrieved November from
Haenssle, H. A., Fink, C., Schneiderbauer, R., Toberer, F.,
Buhl, T., Blum, A., Groups, l.-I. (2018). Man against
machine: diagnostic performance of a deep learning
convolutional neural network for dermoscopic
melanoma recognition in comparison to 58
dermatologists. Annals of Oncology, 29(8), 1836-1842.
https://doi.org/10.1093/annonc/mdy166
Hallevy, P. G. (November 17, 2015). AI v. IP - Criminal
Liability for Intellectual Property IP Offenses of
Artificial Intelligence AI Entities.
Hathaliya, J., Sharma, P., Tanwar, S., & Gupta, R. (2019,
13-14 Dec. 2019). Blockchain-Based Remote Patient
Monitoring in Healthcare 4.0. 2019 IEEE 9th
International Conference on Advanced Computing
(IACC),
Hitaj, B., Ateniese, G., & Perez-Cruz, F. (2017). Deep
Models Under the GAN: Information Leakage from
Collaborative Deep Learning Proceedings of the 2017
ACM SIGSAC Conference on Computer and
Communications Security, Dallas, Texas, USA.
Institute, F. o. L. (2021). https://futureoflife.org/lethal-
autonomous-weapons-pledge/?cn-reloaded=1&cn-
reloaded=1
Kim, M., Song, Y., Wang, S., Xia, Y., & Jiang, X. (2018).
Secure Logistic Regression Based on Homomorphic
Encryption: Design and Evaluation. JMIR Med Inform,
6(2), e19. https://doi.org/10.2196/medinform.8805
Köchling, A., & Wehner, M. C. (2020). Discriminated by
an algorithm: a systematic review of discrimination and
DMMLACS 2021 - 2nd International Special Session on Data Mining and Machine Learning Applications for Cyber Security
596

fairness by algorithmic decision-making in the context
of HR recruitment and HR development. Business
Research, 13(3), 795-848. https://doi.org/10.1007/
s40685-020-00134-w
Lee, S. S., Kelley, M., Cho, M. K., Kraft, S. A., James, C.,
Constantine, M., Magnus, D. (2016). Adrift in the Gray
Zone: IRB Perspectives on Research in the Learning
Health System. AJOB Empir Bioeth, 7(2), 125-134.
https://doi.org/10.1080/23294515.2016.1155674
Li, T., Sahu, A. K., Talwalkar, A., & Smith, V. (2020).
Federated Learning: Challenges, Methods, and Future
Directions. IEEE Signal Processing Magazine, 37(3),
50-60. https://doi.org/10.1109/MSP.2020.2975749
Li, W., Milletarì, F., Xu, D., Rieke, N., Hancox, J., Zhu, W.,
Feng, A. (2019). Privacy-preserving Federated Brain
Tumour Segmentation. arXiv e-prints. Retrieved
October 01, 2019, from https://ui.adsabs.harvard.edu/
abs/2019arXiv191000962L
Lu, X. Y. a. Y. F. a. W. F. a. J. S. a. X. T. a. S.-T. X. a. R.
(2021). Computation-efficient Deep Model Training
for Ciphertext-based Cross-silo Federated Learning.
arXiv:2002.09843.
Markose, A., Krishnan, R., & Ramesh, M. (2016). Medical
ethics. J Pharm Bioallied Sci, 8(Suppl 1), S1-S4.
https://doi.org/10.4103/0975-7406.191934
Mulshine, M. A major flaw in google's algorithm allegedly
tagged two black people's faces with the word 'gorillas'.
In BusinessInsider, 2015.
Nicholas Carlini, C. L., Úlfar Erlingsson, Jernej Kos, Dawn
Song. (2019). The Secret Sharer: Evaluating and
Testing Unintended Memorization in Neural Networks.
arXiv:1802.08232
Noor, P. (2020). Can we trust AI not to further embed racial
bias and prejudice? BMJ, 368, m363. https://
doi.org/10.1136/bmj.m363
Norgeot, B., Glicksberg, B. S., & Butte, A. J. (2019). A call
for deep-learning healthcare. Nature Medicine, 25(1),
14-15. https://doi.org/10.1038/s41591-018-0320-3
Obermeyer, Z., Powers, B., Vogeli, C., & Mullainathan, S.
(2019). Dissecting racial bias in an algorithm used to
manage the health of populations. Science, 366(6464),
447-453. https://doi.org/10.1126/science.aax2342
Policy, T. W. H. O. o. S. a. T. (2018). Summary Of The 2018
White House Summit On Artificial Intelligence For
American Industry https://www.hsdl.org/
?view&did=811092.
Price, W. N. (2018). Big data and black-box medical
algorithms. Sci Transl Med, 10(471). https://doi.org/
10.1126/scitranslmed.aao5333
Raileanu, L. E., & Stoffel, K. (2004). Theoretical
Comparison between the Gini Index and Information
Gain Criteria. Annals of Mathematics and Artificial
Intelligence, 41(1), 77-93. https://doi.org/10.1023/
B:AMAI.0000018580.96245.c6
Rajendran, S., Obeid, J. S., Binol, H., D Agostino, R.,
Foley, K., Zhang, W., . . . Topaloglu, U. (2021). Cloud-
Based Federated Learning Implementation Across
Medical Centers. JCO Clin Cancer Inform, 5, 1-11.
https://doi.org/10.1200/CCI.20.00060
Rieke, N., Hancox, J., Li, W., Milletarì, F., Roth, H. R.,
Albarqouni, S., Cardoso, M. J. (2020). The future of
digital health with federated learning. NPJ Digit Med,
3, 119. https://doi.org/10.1038/s41746-020-00323-1
Rodrigues, R. (2020). Legal and human rights issues of AI:
Gaps, challenges and vulnerabilities. Journal of
Responsible Technology, 4, 100005. https://doi.org/
https://doi.org/10.1016/j.jrt.2020.100005
SaMD, F. https://www.fda.gov/media/122535/download.
Retrieved February from
Sarma, K. V., Harmon, S., Sanford, T., Roth, H. R., Xu, Z.,
Tetreault, J., Arnold, C. W. (2021). Federated learning
improves site performance in multicenter deep learning
without data sharing. J Am Med Inform Assoc. https://
doi.org/10.1093/jamia/ocaa341
Scientist, F. o. A. (2021). Defense Primer: U.S. Policy on
Lethal Autonomous Weapon Systems. Retrieved May
2021 from https://fas.org/sgp/crs/natsec/IF11150.pdf
Shokri, R., & Shmatikov, V. (2015, 29 Sept.-2 Oct. 2015).
Privacy-preserving deep learning. 2015 53rd Annual
Allerton Conference on Communication, Control, and
Computing (Allerton),
Shokri, R., Stronati, M., Song, C., & Shmatikov, V. (2017,
22-26 May 2017). Membership Inference Attacks
Against Machine Learning Models. 2017 IEEE
Symposium on Security and Privacy (SP),
Technology, N. S. a. T. C. C. o. (October 2016).
https://obamawhitehouse.archives.gov/sites/default/fil
es/whitehouse_files/microsites/ostp/NSTC/preparing_f
or_the_future_of_ai.pdf. Retrieved February, 2021
from
Topol, E. J. (2019). High-performance medicine: the
convergence of human and artificial intelligence.
Nature Medicine, 25(1), 44-56. https://doi.org/10.1038/
s41591-018-0300-7
Truex, S., Baracaldo, N., Anwar, A., Steinke, T., Ludwig,
H., Zhang, R., & Zhou, Y. (2019). A Hybrid Approach
to Privacy-Preserving Federated Learning. Informatik
Spektrum, 42(5), 356-357. https://doi.org/10.1007/
s00287-019-01205-x
Vyas, S., Gupta, M., & Yadav, R. (2019, 4-6 Feb. 2019).
Converging Blockchain and Machine Learning for
Healthcare. 2019 Amity International Conference on
Artificial Intelligence (AICAI),
Warnat-Herresthal, S., Schultze, H., Shastry, K. L.,
Manamohan, S., Mukherjee, S., Garg, V., . . . Deutsche,
C.-O. I. (2021). Swarm Learning for decentralized and
confidential clinical machine learning. Nature. https://
doi.org/10.1038/s41586-021-03583-3
Wei, K., Li, J., Ding, M., Ma, C., Yang, H. H., Farokhi, F.,
Poor, H. V. (2020). Federated Learning With
Differential Privacy: Algorithms and Performance
Analysis. IEEE Transactions on Information Forensics
and Security, 15, 3454-3469. https://doi.org/10.1109/
TIFS.2020.2988575
Wiens, J., Saria, S., Sendak, M., Ghassemi, M., Liu, V. X.,
Doshi-Velez, F., Goldenberg, A. (2019). Do no harm: a
roadmap for responsible machine learning for health
care. Nature Medicine, 25(9), 1337-1340. https://
doi.org/10.1038/s41591-019-0548-6
Federated Learning in Healthcare is the Future, But the Problems Are Contemporary
597

Zhang, B., Anderljung, M., Kahn, L., Dreksler, N.,
Horowitz, M. C., & Dafoe, A. (2021). Ethics and
Governance of Artificial Intelligence: Evidence from a
Survey of Machine Learning Researchers. ArXiv,
abs/2105.02117.
DMMLACS 2021 - 2nd International Special Session on Data Mining and Machine Learning Applications for Cyber Security
598
