
User Models for Post-stroke Therapies and Consequences for the
Interaction with a Humanoid Robot
Alexandru Bundea
a
and Peter Forbrig
b
Universität Rostock, Fakultät für Informatik, Lehrstuhl für Softwaretechnik, Albert-Einstein-Str. 22, 18059, Germany
Keywords: Social Robot, Human-Robot-Interaction, User Model, Therapy.
Abstract: In the future, social robots may become a viable help to provide more patient therapy sessions for post-stroke
patients. Certain therapies require still another person to work with the patient. If a non-medically skilled
helper person could be used, this could dampen the lack of available therapists worldwide. But for this,
strategies how robots may best advise a patient and the helper must be found. This paper aims to find a
common basis, where to formulate rules how a social robot could react and act in a therapy session. We
present the focused therapy and propose our model and give an exemplary idea how to use this framework.
1 INTRODUCTION
A worldwide shortage of medical personnel in all
areas is forcing medicine to innovate. In order to cope
with the increasing number of stroke patients,
research is being carried out in some places on how
robots can help patients in neurorehabilitation
therapy. Further subdivided, there is the possibility of
doing this with a physical aid, in which a mechanical
system moves the limbs by a robot and socially
assistive robots (SAR). Their task is, among other
things, to accompany the patient through verbal
instructions and feedback through a therapy session.
The main goal of the robot is to let patients perform
their training exercises in a good way and to keep the
patient motivated throughout the therapy.
An important aspect is a continuously verbal
feedback during therapy. This was observed during
sessions with a human therapist, but becomes even
more important in the case of SAR as the robot cannot
provide physical assistance and body contact to the
patient. In addition, an intelligent recognition of
parameters must already be available for the feedback
in order to optimally adapt the feedback with regard
to the current therapy situation. While the recognition
of a specific therapy session situation represents a
multimodal recognition challenge with the use of, for
example, several sensors like cameras, sensors for
a
https://orcid.org/0000-0001-8315-3405
b
https://orcid.org/0000-0003-3427-0909
sound or devices analyzing the interaction of a
patient.
Based on the sensed situation actions have to be
specified that should be activated. Rules can be used
for this purpose. They can e.g. specify when the robot
should say something to a patient. This aspect of rules
will become a topic that we want to discuss in this
paper. We will focus on cases with 2 people present,
the patient and a helper. Because of the lack of
professional therapists, a helper that might come from
the family will support the patient.
Most social robot therapies deal with robot-to-
patient cases. This works in cases in which the patient
can carry out the therapy alone with the robot. In
certain forms of stroke therapy, however, the main
feature is that the severely handicapped patient's
limbs have to be moved by a therapist. Here now adds
an idea, to substitute this therapist, with a non-
medically skilled “helper”, to move the limbs of the
patient. For this approach, the robot would then not
only have to instruct and motivate a patient, but also
this other person.
In order to carry out a suitable spontaneous,
helpful feedback strategy, one has to define rules of
what to do. Here we look into finding a common basis
and a structure, on where rules could be applied to.
Thereby we aim to incorporate a way, how we can use
a user model and the personality of the therapy
participants to consider how the robot provides his
Bundea, A. and Forbrig, P.
User Models for Post-stroke Therapies and Consequences for the Interaction with a Humanoid Robot.
DOI: 10.5220/0010722100003060
In Proceedings of the 5th International Conference on Computer-Human Interaction Research and Applications (CHIRA 2021), pages 283-290
ISBN: 978-989-758-538-8; ISSN: 2184-3244
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
283

feedback. The corresponding user models were based
on interviews using the Repertory Grid Technique
(George A. Kelly, 2001).
The further structure of this paper first shows the
related works and then the stroke therapy considered
here and then presents a model of when feedback
from the robot is appropriate. This is followed by a
discussion and a summary.
2 RELATED WORKS
Winkle researched in (Katie Winkle, 2020) how a
SAR can be used as a treadmill running instructor and
how participants would accept it. She uses an input
space of 20 features with different dimensions to
monitor a runner approach. It includes features like
heart rate, speed, activity level and also psychological
traits combined in the Big 5 model.
This is one of the commonly used model to assess
the personality of patients as shown by Dwan et al.
(Toni Dwan and Tamara Ownsworth, 2019). Coming
from the field of psychology, the five personality
factors are “Neuroticism”, “Extraversion”,”
Openness to experience”, “Agreeableness”,
“Conscientiousness”. A person’s factors will be
determined through questionnaires.
The Robot has many different actions as a coach
for a treadmill like reminding about time or how to
correct the pose of the runner. Winkle uses an
interactive machine learning approach, whereby a
trainer enters during a live-session with a runner new
state-action pairs into the system. The robot then
improves his next autonomous action from the
previously gathered examples from the trainer.
Casas et al. (Jonathan A. Casas, et al., 2019) use a
NAO Robot in a therapy setup to increase cardiac
function. Patients run on a treadmill and the nearby a
robot provides verbal and gestural feedback. Inside
their patient-robot interaction they monitor the level
of exertion with the “Borg scale” (Bahar Irfan, et al.,
2020) and the patient’s heart rate. The Borg scale is a
method to quantify perceived exertion and aims to
make it comparable between individuals. Even with
its subjective nature, this method proved to have a
good correlation with the level of more measurable
effort metrics in diverse application.
Additionally, they watch several cases with these
two metrics and switch between different interaction
modes. Depending on a “high” or “low” exertion
and/or heart rate they ask the patient if he is feeling
alright. For cases whereby, the exceeds the heart rate
exceeds for too long the normal values, the robot will
e.g. be saying: “Doctor, the patient needs help.”. This
interaction mode then can only be switched off, when
the medical staff touches the head of the robot.
A lately, different approach has been done by
Irfan et al. (Bahar Irfan, et al., 2020) by measurements
with an ECG, Borg Scale entered thorugh the patient
via a tablet, a laser range finder and an inertial
measurement unit and a tablet camera. Next to
predefined phrases at certain points in the session, and
alerting the patient and medical staff about a high
exertion or Heart rate, the robot will provide prompts
if the patient should improve his cervical posture.
A rather different perspective to look on the
provision of feedback to the patients comes directly
from medical literature. Bachelor et al. (Alexandra
Bachelor, 1991) state, that the success of the therapy
outcome and the “alliance” between patient and
therapist is that the patients perception yields a better
prediction of the success than the therapist
perception. Furthermore, from a patient’s perspective
therapist-provided aid, warmth, caring, emotional
involvement are factors which truly helped in
therapies.
Duncan et al. (Barry L. Duncan, et al., 1994) adds
to these findings and states, that in the “alliance”
literature, the therapy progresses the most, if the
therapist talks about what the patients see as
important for them. Additionally the therapist should
have chosen methods, that the patient will think, that
it helps him to reach the goal specified by the patient.
Because of these finding, we would primarily
target the patient’s needs and we later present robot
actions, which we try to tailor to the findings of
Bachelor and Duncan et al.
3 ARM BASIS TRAINING (ABT)
3.1 Classic ABT with a Therapist
ABT has been designed for severe arm impairment.
The focus lies on improving the patient’s capabilities
for selected movements of the patients’ arms as
displayed in figure 1. The ABT will be done in a
structured repetitive training manner with each
session to complete a set of arm and hand exercises
(Thomas Platz, Bernhard Elsner, and Jan Mehrholz.
2015). The therapy’s’ movements are starting with
joint movements “without” the factor of gravity (step
1), meaning that the therapist is holding the extremity
of the patient up and manually assists the movement
of the patients arm, hand or finger during the exercise.
The next step -after the patient acquires the full range
of motion of the movement- is to let the patient do the
exercises with gravity (step 2), whereby the patient is
Humanoid 2021 - Special Session on Interaction with Humanoid Robots
284

supposed to do single joint movements, while the
therapist is still holding the hand or arm, letting the
patient focus only on selected joint movements of the
rest of his arm. Ideally, the patient performs multiple-
joint-movements on his own (step 3). Until then, the
supporting therapist needs to hold the weight of the
arm and to ensure that the patient does not need a
postural control by himself during the exercise.
There is no specific performance-related feedback
from the therapist to the patient predefined, so the
therapist may engage in feedback as he wants.
In the first session of a patients’ therapy, a human
therapist will do an intensive assessment and
introduce him to the therapy. Only after this, the next
therapy session will include the robot.
Figure 1: Three Arm Basis Training exercises with a human
therapist. The start- and endpoints for each movement are
here displayed (Thomas Platz, 2019).
3.2 ABT with Helper and Robot
This will be the later setup for our robot study and at
first adds only the robot to the therapy session. Of
course, there needs to be more technical measurement
systems like cameras to recognize the movements, the
emotional state, body positions and verbal
communication.
Figure 2: Exemplary execution of the ABT therapy (non-
medical envirionment).
It is the idea to check with sensors whether the
execution of the exercises is correct. This means e.g.
the speed and the extend of the movement.
Figure 3 gives an impression of the models that
our analysis software provides. The (upper) image
shows what the system calculates with the angles of
the limbs. In this one the patient is supposed to do an
arm curl. Thereby we analyse the degree of the angle
and this may come into consideration of what we
would express as feedback e.g. “Move your hand
closer to your shoulder.”
The lower image displays the situation with a
helper from a different perspective. We will provide
similar hints
Figure 3: Examples of the visualisation of sensor tracking
of arm movements.
Additionally, it is intended to identify the
emotions of the patient and the helper. The humanoid
robot Pepper provides a quite good solution based on
facial expression and voice that works quite well for
one person. We did not have a solution for two
persons yet. However, in this paper we want to focus
on a different aspect, the rule model.
User Models for Post-stroke Therapies and Consequences for the Interaction with a Humanoid Robot
285
4 PROPOSED RULE MODEL
FOR
4.1 Basic Patient/Helper Model
Starting with the basic form of one robot to one
patient, we also use an exertion metric with binary
values, in this case “low” and “high” engagement. For
emotional states we use “neutral”, “unhappy” and
“happy.
Table 1: Basic state table.
Emotion
High
En
g
a
g
ement
Low
En
g
a
g
ement
Unha
ppy
Neutral
Happy
Table 1 presents 6 different states of a patient, to
which a robot could react and provide spontaneous
feedback. Note that this is only a general framework
for such an arm rehabilitation scenario. More specific
feedback for arm posture is not the main focus of this
model.
Currently with this table alone, one would only
describe the person’s state. We now need to introduce
the robot’s possible actions. After this, we can
combine both the patient/helper state with the
possible robot actions to design a “grid”. With this
grid, we have one simple way how to define rules for
the interaction. So, in the next subsection we will
focus on a model for the action space of the robot.
4.2 Robot Actions
From the robot side we need to model the possible
robot actions according to what the robot should
achieve. The selection of goals and actions, depicted
in table 1 are only a subset of what could be perceived
as useful. These actions can be done in different ways,
such as “positive”, e.g. to generate a good, confirming
way, so that the patient gets confirmed, that what he
already does, is good. Otherwise a “challenging” style
e.g. tries to tell the person, that he is already ok, but
he can do it even better. Styles will be more
highlighted in a moment.
For our work here, we identify four important
feedbacks for the patient.
“Provide task-related feedback” (PTR) is directly
linked how the patient performs his task. “Provide
social Feedback” (PSF) aims to motivate the person.
Then to make a conversation a bit more memorisable,
the robot may “provide small talk” (PST), this is
mainly for cases, to improve a therapy scenario,
where no one talks and the atmosphere between the
two persons may become too uncomfortable. Finally,
the robot may ask a person, e.g. to enter how the
session is going on today or the current exertion level,
we call this action “Request information” (RI). This
is the only robot action, where we would not include
a positive or challenging style, as the person should
only focus on entering data as directly as possible.
We intent to use the systems decision making to
determine, if a certain action/feedback should be
provided by the robot. If an action has been triggered,
the style, “how the robot” should formulate his verbal
prompt is determined by the psychological profile of
this person.
Table 2: Social robot action space.
Action goal Action Style Example
Improve
Performance
PTR
P
“You do well, but you
should move the arm
higher up in each
repetition.”
N “move the arm higher”
C
“Dear <name>, are your
arms tiring? Move the
patients arm higher up”
Improve
Motivation
PSF
P
“Great results with your 40
points, you’re approaching
your goal fast!
N
“You reached 40 points,
remember your goal to be
able to play again.”
C
“With 40 points, I’m sure
you’re still holding back
your performance”
relax
interaction
PST
P
“We’re halfway through
the exercises, you are a
good team!”
N
“We’re halfway through
the exercise.”
C
“I think we as a team can
work harder to achieve a
better performance! There
is only half of the exercises
left to prove it!”
Ask for user
data (only to
Patient)
RI
P -
N
“Please enter your exertion
level.”
C -
The column “style” means “feedback style”,
which will be either “neutral” (n), “positive” (p) and
“challenging” (c). We use the “Big 5” or “OCEAN”
Model as the foundation to decide in which
conversation style the robot’s action should be
formulated.
In this manner, for a person being less “open to
experience” new things according to the “Big 5”
Humanoid 2021 - Special Session on Interaction with Humanoid Robots
286

model, we may not use the challenging style often,
whereby a more open person may find this style more
engaging than others.
The idea, is, that a robot will always say the same,
when providing a certain action, but the patient
profile will determine, which feedback style will be
used.
4.3 Patient + Helper Model
The main point here is that we try to look on both
persons separately. Therefore, we have two user
models. However, in this paper we focus on the
models for patients only. For helpers the structure of
the model looks similar. However, the spoken phrases
of the robot are different.
If we try to summarize the possible states of a
participant’s states (table1) with all possible robot
actions (table 2), we have 72 state and action
combinations. This means, that the robot says one or
several phrases for each of these states. Additionally,
for the aspect of engagement of either person, the
robot could integrate a more precise answer for task-
related feedbacks, since the patient is the more
passive one and the helper will be the more active
executor in the first stage of the therapy. But this
would result in even more sentences and more
detailed feedback, which need to be prepared
beforehand and also be recognized.
4.4 Patient and Helper Attributes and
Metrics and Its Role for the
Feedback Style
As mentioned before we base our decision which
feedback style the robot should use on the Big 5
Model, as briefly explained in section 2. The arm and
hand speed of the participants detected by devices are
what we specifically want to use for the low/high
engagement. Since the whole therapy is based that the
patient’s arm and hands should be moved by the
helper and later by the patient alone, this will be the
main metric for engagement. This will be a dynamic
value recognized by sensors and cameras.
For the static values of the Big 5 factors, both the
patient and helper should fill out a questionnaire
before the first therapy session.
4.5 History of Previous Commands
The previously performed actions as “chain” of
actions can be added. In theory, the robot should take
his previous actions into account, of what to do next.
Saying e.g. for the fourth consecutive time, that the
helper should better his performance, might be an
annoying for him and the patient.
To prevent this, a chain of previous actions can be
added to each patient or helper state and add rules
basing on them as well. On the other hand, this
temporal aspect could become unnecessary if a robot
action is triggered at a certain time.
A verbal utterance could only be triggered once
e.g. 10 or 15 seconds. It needs to be evaluated how
the frequency of feedback should be.
5 DEFINING THE RULES
The next step would now to define the rules that,
when a certain action happens, which style of the
feedback should be used. This will mostly due
determined by the style of the clinicians and or system
designer when to use what and when a high or low
engagement has been detected.
For the exemplary case we defined an exemplary
list of rules:
1. The positive Style will not be used on
already happy participants with a high
engagement.
2. The “challenging” style should only be used
carefully and when appropriate. (This
feedback style can be perceived as “social
pressure”.)
3. If the hand/arm movement speed moves
below a certain speed X, the engagement
level becomes “low”.
4. The robot should ask less often for more
information about the participant, if he is
more introverted (has not so much
extraversion).
This list should only show an idea, how the Table
3 can be used, especially if this framework would be
used for other therapies, different therapies involving
different tasks for patients and helpers. Only rule 1 &
2 are visually shown in Table 3.
Phrases within a style and the patient's
engagement are the same for the sake of simplicity.
In contrast to our example, individual phrases can be
determined for each different patient state. On the
other hand, depending on the application, there are
many other opportunities where spontaneous
feedback can be given. In the case of the ABT, we
have 17 different exercises, which all can be executed
wrong in several ways and therefore could integrate
multiple correctional feedback options.
User Models for Post-stroke Therapies and Consequences for the Interaction with a Humanoid Robot
287
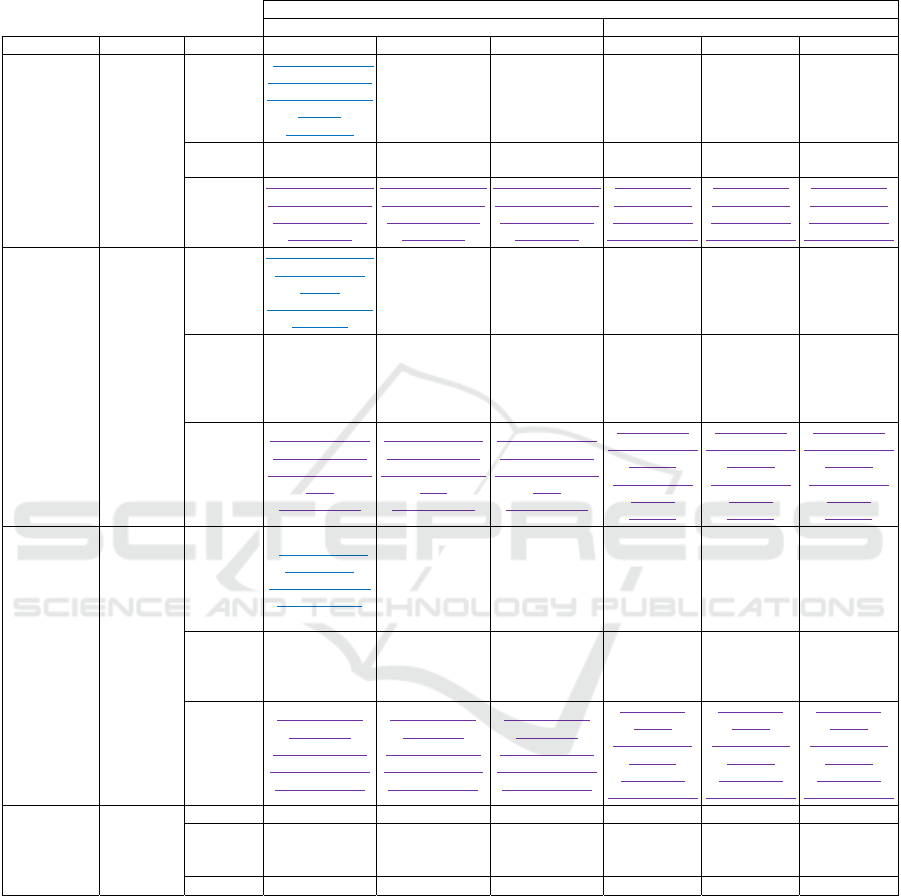
Table 3: Exemplary table for an exemplary patient for which we do not want to challenge him/her verbally. In this example
we would not use the "challenging" style (1
st
rule with purple text). Additionally, we wouldn't use the positive style, if the
person is already in a happy state (2
nd
rule with blue lines) and highly engaged. Here we regard ABT step 3 (patient trains
by himself). Crossed out sentences means that the robot will not use this feedback option.
Patient/Helper
High Engagement Low Engagement
Action goal Action Style Happy Neutral Unhappy Happy Neutral Unhappy
Improve
Performance
Provide
Task-related
Feedback
Positive
“You do well, but
you should move
the arm higher up
in each
repetition.”
“You do well, but
you should move
the arm higher up
in each
repetition.”
“You do well, but
you should move
the arm higher up
in each
repetition.”
“You’re on a
good track, but
can you maybe
move your arm
higher up?”
“You’re on a
good track, but
can you maybe
move your arm
higher up?”
“You’re on a
good track, but
can you maybe
move your arm
higher up?”
Neutral
“Move your arm
higher”
“Move your arm
higher”
“Move your arm
higher”
“Move your
arm higher”
“Move your
arm higher”
“Move your
arm higher”
Challenging
“Dear [name], are
your arms tiring?
Move your arm
higher up”
“Dear [name], are
your arms tiring?
Move your arm
higher up”
“Dear [name], are
your arms tiring?
Move your arm
higher up”
“[name] you
are supposed
to move your
arm higher up”
“[name] you
are supposed
to move your
arm higher up”
“[name] you
are supposed
to move your
arm higher up”
Keep/Improve
Motivation
Provide
social
Feedback
Positive
“Great result with
your 40 points,
you’re
approaching your
goal fast!
“Great result with
your 40 points,
you’re
approaching your
goal fast!
“Great result with
your 40 points,
you’re
approaching your
goal fast!
“Awesome
results with
your 40
points!”
“Awesome
results with
your 40
points!”
“Awesome
results with
your 40
points!”
Neutral
“You reached 40
points, remember
your goal to be
able to play
again.”
“You reached 40
points, remember
your goal to be
able to play
again.”
“You reached 40
points, remember
your goal to be
able to play
again.”
“You reached
40 points,
remember your
goal to be able
to play again.”
“You reached
40 points,
remember your
goal to be able
to play again.”
“You reached
40 points,
remember your
goal to be able
to play again.”
Challenging
“With 40 points,
I’m sure you’re
still holding back
your
performance”
“With 40 points,
I’m sure you’re
still holding back
your
performance”
“With 40 points,
I’m sure you’re
still holding back
your
performance”
“I’m sure in
the next round,
you can
achieve more
than 40
p
oints.”
“I’m sure in
the next round,
you can
achieve more
than 40
p
oints.”
“I’m sure in
the next round,
you can
achieve more
than 40
p
oints.”
Change
interaction
climate
Small talk/
Tell a joke
Positive
“We’re halfway
through the
exercises, we are
a good team!”
“We’re halfway
through the
exercises, we are
a good team!”
“We’re halfway
through the
exercises, we are
a good team!”
“We’re already
in the 2
nd
half
of the
exercises we
are a good
team!”
“We’re already
in the 2
nd
half
of the
exercises we
are a good
team!”
“We’re already
in the 2
nd
half
of the
exercises we
are a good
team!”
Neutral
“We’re halfway
through the
exercise.”
“We’re halfway
through the
exercise.”
“We’re halfway
through the
exercise.”
“We’re
halfway
through the
exercise.”
“We’re
halfway
through the
exercise.”
“We’re
halfway
through the
exercise.”
Challenging
“There is only
half of the
exercises left to
show everything
what you got!”
“There is only
half of the
exercises left to
show everything
what you got!”
“There is only
half of the
exercises left to
show everything
what you got!”
“Come on,
only 8
exercises left
to show
everything
what you got!”
“Come on,
only 8
exercises left
to show
everything
what you got!”
“Come on,
only 8
exercises left
to show
everything
what you got!”
Ask for
wellbeing
Request for
more
information
Positive - - - - - -
Neutral
“Please enter
your exertion
level.”
“Please enter
your exertion
level.”
“Please enter
your exertion
level.”
“Please enter
your exertion
level.”
“Please enter
your exertion
level.”
“Please enter
your exertion
level.”
Challenging - - - - - -
6 DISCUSSION AND
LIMITATION
Finding a common basis to further discuss when to
intervene and how that intervention should look like
for two persons is a challenging task. We think of our
presented work as a starting point of how to formalize
the provision of feedback to patient and helper.
Additionally, we have to track two persons
simultaneously. We will focus on the ideas mentioned
by Winkle et. al and the ideas discussed in section 2.
From the work of Duncan et al. and Bachelor and
other related works on the subject of the strategic
work alliance (section 2), we have taken the paradigm
of focusing on the patient. Due to lack of paper space,
only one example targeting the patient alone was
shown in this work in therapy. Table 3 would also
Humanoid 2021 - Special Session on Interaction with Humanoid Robots
288

exist in a similar form for the helper. However, it can
be argued that the "Request information" action is less
important and will not be carried out often, since the
helper should be fit for the role as helper and it slows
down the therapy session, but the benefit to measure
the helper’s exertion is rather small. The "relax
interaction" action no longer needs to be used,
because it is primarily intended for situations when
both people no longer interact with each other. If this
happens, the robot action will automatically affect the
helper. Consequently, the monitoring for this action
does not have to be done for the helper.
The actions to motivate the helper and to correct
his performance will be changed to suit to his role as
supporter. But other than there will be no systematic
changes. Also, the feedback styles are used and their
usage is derived from the psychological Big 5 profile.
For a practical implementation, one could follow
the idea from (Katie Winkle, 2020) and construct an
interactive-machine-learning setup. Patient and
helper states can be stored as “tuples” of a
<(multi-)state, robot action, (assigned) reward>.
At a given t, one would pick the next best robot
action. In this way, a state could then contain the
whole patient’s profile, engagement level, and the so
far elapsed therapy session.
Looking into the limitations, it is clear, that
integrating personality traits into the process of
choosing the appropriate feedback is a very
challenging task. Due to the complexity of this
problem, the upcoming evaluation could be viewed
only as a preliminary study with the ideas presented
here. The results of that study might show that a
different approach might be more suitable.
Furthermore, the introduction of more states in
the user model can describe the therapy situation
better, but adds more complexity for the robot’s
action space. It is yet not clear whether this is really
necessary. Currently, we have the opinion that six
states are appropriate. However, this has to be
evaluated with patients and helpers.
If we use the same framework for helper and
patient, we would also need to consider to add a
suitable robot action and or phrase for him as well.
More importantly, there should be variation inside
every robot action to avoid a therapy experience and
situations where patients and helper perceive the
robot as boring or monotonous, especially, if these
robot actions get triggered more often than others.
It might be necessary to specify more than one
sentence in each situation and implement an arbitrary
selection of one of those phrases. Thus, the actual
number of predefined sentences or general
vocabulary increases and also the work behind that.
In table 3 we briefly showed the case with 2 examples
per robot action, depending on low and high
engagement. But in reality, one should aim for several
utterances more, since the therapy may take several
weeks of daily sessions.
One may argue, that certain sentences or phrases
displayed here are not particularly positive. But for a
first evaluation, we wanted to let the whole utterance
sound “positive” and focus on exact words later.
Finally, we have to consider the extent to which a
regular big 5 questionnaire can be used for stroke
patients and may instead use a big 5 questionnaire
specifically for stroke survivors.
7 CONCLUSIONS
In this paper we introduced a framework of
observable states of patient and a non-medically
skilled helper to execute a post-stroke therapy for arm
and hand rehabilitation. The training tasks are guided
by a social humanoid robot Pepper. This framework
is intended to be used as a user model of a patient and
a helper. The frameworks are based on the Big 5
Model and further therapy-specific attributes. The
model supports the decision when to take an action by
the robot and also how the feedback should be
expressed. We concentrated on six states for each
person, determined by a high or low engagement that
is analysed from the data of the patient that were
created after an initial interview with a human
therapist. Additionally, the emotions unhappy,
neutral or happy are identified from facial
expressions.
Moreover, the robot may take spontaneous
actions in different conversation styles, to e.g.
challenge or to compliment the users. How the style
will be chosen, depends on pre-defined rules to better
fulfil the patient’s wishes.
We intend to use the framework and define a
detailed list of rules, for an ABT-study inside our E-
BRAiN (Peter Forbrig, et al., 2020) project. In this
project we mainly focus to research how to motivate
patients with a social robot in post-stroke therapies.
It is our goal to start with evaluations by patients
very soon. This had unfortunately to be postponed
several times because of contact restrictions. Even
when the restrictions were lowered, patients did not
want to come to the hospital. Hopefully, this will
change in the near future.
User Models for Post-stroke Therapies and Consequences for the Interaction with a Humanoid Robot
289

ACKNOWLEDGEMENTS
This joint research project “E-BRAiN - Evidence-
based Robot Assistance in Neurorehabilitation” is
supported by the European Social Fund (ESF),
reference: ESF/14-BM-A55-0001/19-A01, and the
Ministry of Education, Science and Culture of
Mecklenburg-Vorpommern, Germany. The sponsors
had no role in the decision to publish or any content
of the publication.
REFERENCES
George A. Kelly. 2001. Clinical diagnosis and
psychotherapy (Reprinted.). The psychology of
personal constructs, / George A. Kelly; Vol. 2.
Routledge, London.
Katie Winkle. 2020. Expert-Informed Design and
Automation of Persuasive, Socially Assistive Robots.
Dissertation. The University of Bristol.
Toni Dwan and Tamara Ownsworth. 2019. The Big Five
personality factors and psychological well-being
following stroke: a systematic review. Disability and
rehabilitation 41, 10, 1119–1130. DOI: https://doi.org/
10.1080/09638288.2017.1419382.
Jonathan A. Casas, Nathalia Céspedes, Carlos A. Cifuentes,
Luisa F. Gutierrez, Mónica Rincón-Roncancio, and
Marcela Múnera. 2019. Expectation vs. Reality:
Attitudes Towards a Socially Assistive Robot in
Cardiac Rehabilitation. Applied Sciences 9, 21, 4651.
DOI: https://doi.org/10.3390/app9214651.
Stephen Hampton, Gina Armstrong, Monika S. Ayyar, and
Sheng Li. 2014. Quantification of perceived exertion
during isometric force production with the Borg scale
in healthy individuals and patients with chronic stroke.
Topics in stroke rehabilitation 21, 1, 33–39. DOI:
https://doi.org/10.1310/tsr2101-33.
Bahar Irfan, Nathalia C. Gomez, Jonathan Casas,
Emmanuel Senft, Luisa F. Gutierrez, Monica Rincon-
Roncancio, Marcela Munera, Tony Belpaeme, and
Carlos A. Cifuentes. 2020. Using a Personalised
Socially Assistive Robot for Cardiac Rehabilitation: A
Long-Term Case Study. In. IEEE. DOI: https://doi.org/
10.1109/ro-man47096.2020.9223491.
Alexandra Bachelor. 1991. Comparison and relationship to
outcome of diverse dimensions of the helping alliance
as seen by client and therapist. Psychotherapy: Theory,
Research, Practice, Training 28, 4, 534–549. DOI:
https://doi.org/10.1037/0033-3204.28.4.534.
Barry L. Duncan, Mark A. Hubble, and Greg Rusk. 1994.
To Intervene or Not to Intervene? That is Not the
Question. Journal of Systemic Therapies 13, 4, 22–30.
DOI: https://doi.org/10.1521/jsyt.1994.13.4.22.
Thomas Platz, Bernhard Elsner, and Jan Mehrholz. 2015.
Arm basis training and arm ability training: two
impairment-oriented exercise training techniques for
improving arm function after stroke. Cochrane
Database of Systematic Reviews 17, 6, 666. DOI:
https://doi.org/10.1002/14651858.CD011854.
Thomas Platz. 2019. Impairment-Oriented Training -
Official Homepage (May 2019). Retrieved March 25,
2020 from http://www.iotraining.eu/abt.html.
Peter Forbrig, Alexandru Bundea, Ann Pedersen, and
Thomas Platz. 2020. Digitalization of Training Tasks
and Specification of the Behaviour of a Social
Humanoid Robot as Coach. In Human-Centered
Software Engineering. Springer International
Publishing, Cham, 45–57.
Humanoid 2021 - Special Session on Interaction with Humanoid Robots
290
