
Doctor's Interpersonal Communication on the Quality of Life of
Diabetes Mellitus Patients
Pimpin Tanadi, Ermi Girsang*, Sri Lestari R. Nasution and Chrismis Novalinda Ginting
Faculty of Medical, Universitas Prima Indonesia, Indonesia
Keywords: Interpersonal communication, quality of life, diabetes mellitus.
Abstract: A doctor's communication competence determines the level of success in helping the treatment of a patient's
illness. Preliminary survey results show that many patients consider doctors rarely greet patients at the
beginning of a consultation session, so that it has a direct impact on patients who are afraid to express their
complaints. This study aims to analyze the effect of interpersonal communication in improving the quality of
life of patients with diabetes mellitus. This type of research was a type of quantitative survey with a cross-
sectional approach with a sample of 60 respondents. The variables included in the study were openness,
empathy, supportive attitude, positive attitude, equality, and quality of life of patients. Data were analyzed
using chi-square test and logistic regression test. The results showed that the variables that influence the
improvement of the quality of life of patients with diabetes mellitus on average around 55 - 72%. These results
indicate that the quality of doctor communication still needs to be improved. This improvement is expected
to be able to improve the quality of life of DM patients who are currently still around 43.3%.
1 INTRODUCTION
Diabetes mellitus is currently increasing in number
and is one of the world's health problems including in
Indonesia. The International Diabetes Federation
(IDF) reports that currently, around 425 million
adults (20-79 years old) are living with diabetes
mellitus, and by 2045 it is expected to increase to 629
million. The proportion of people with type 2 diabetes
mellitus increased by 79% in adults living in low and
middle income countries. In addition IDF also said
that more than 1,106,500 children live with type 1
diabetes mellitus and more than 21 million live births
(1 in 7 births) are affected by diabetes mellitus during
pregnancy. Diabetes mellitus also causes at least 727
billion dollars for health expenditure in 2017 or 12%
of total expenditure for adults (Cho, 2018).
Some data about diabetes mellitus in Indonesia is
also quite astonishing. In 2017 Indonesia was ranked
5th for the country with the highest number of people
with diabetes mellitus in the world with 114,069
fatalities (International Diabetes Federation, 2017).
In addition, Basic Health Research (Riskesdas) in
2007 and 2013 also conducted interviews to calculate
the proportion of diabetes mellitus at the age of 15
years and over. Defined as a person with diabetes
mellitus if a doctor has been diagnosed with diabetes
or has never been diagnosed with diabetes by a doctor
but in the last 1 month experiencing symptoms of
frequent hunger, frequent thirst, frequent urination
with large amounts and weight loss. The results of the
interview found that the proportion of diabetes
mellitus at Riskesdas 2013 almost doubled compared
to 2007. For North Sumatra province itself the
proportion of diabetes mellitus also increased, in
2013 the number of people with diabetes mellitus
diagnosed by doctors reached 160,913 people
(Ministry of Health, Republic of Indonesia, 2014).
Management and control of chronic diseases such
as diabetes mellitus is very important because of the
dangerous complications, as well as a large economic
burden if the disease is not controlled. The role of
health workers and doctors in helping patients with
diabetes mellitus control their blood sugar is very
important because this is a chronic disease (Masriadi,
2016). In diabetes mellitus, basically the real doctor
is the patient himself. The patient determines when he
should seek treatment, when to check blood sugar
levels or how to regulate diet. Therefore, diabetic
patients really need the figure of a friend to manage
the disease through a doctor.
According to the Law of No. 29/2004 concerning
Medical Practice, doctors, specialists, doctors,
specialists, dentists and specialist dentists have
Tanadi, P., Girsang, E., R. Nasution, S. and Ginting, C.
Doctor’s Interpersonal Communication on the Quality of Life of Diabetes Mellitus Patients.
DOI: 10.5220/0010286500350041
In Proceedings of the International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical (HIMBEP 2020), pages 35-41
ISBN: 978-989-758-500-5
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
35

graduated from medical or dental education, both
domestically and abroad, which are recognized by the
Government of the Republic of Indonesia in
accordance with statutory regulations. In the medical
profession, doctor and patient communication is one
of the competencies that must be mastered by doctors.
The communication competence determines success
in helping treat a patient's illness. During this time,
the communication competence of a doctor can be
said to be often overlooked.
In Indonesia, some doctors feel they don't have
enough time to talk with their patients, so they can
only ask as needed. This causes the doctors tend not
to get enough information to establish the diagnosis
and determine further planning and action. While in
terms of the patient himself, patients generally feel in
a lower position before the doctor (superior-inferior),
so that the patient is feel afraid to ask questions and
tell stories or just answer according to doctors'
questions (Foursanalitywati, 2015; Turnip et al,
2020).
In general, the definition of communication is the
process of delivering ideas, hopes and messages
conveyed through certain symbols that contain
meaning carried out by the messenger addressed to
the recipient of the message. The application of the
definition of communication in the interaction
between doctor and patient is interpreted as the
achievement of understanding and agreement that is
built by the doctor with the patient at each step in
solving the patient's problem (Adriyani, 2018; Wijaya
et al, 2019).
Kurzt (1998) suggests two approaches about
communication in the field of medicine. First is the
disease centered communication style or doctor
centered communication style, where communication
is based on the doctor's interest in trying to establish
a diagnosis, including investigation and clinical
reasoning about signs and symptoms. The second
approach is an illness centered communication style
or patient centered communication style, where
communication is based on what the patient feels
about his illness which individually unique
experience. The aim is to create comfort and
satisfaction for both parties to create effective
communication between doctors and patients (Kurtz,
1998).
A doctor's communication ability to have good
communication skills with his patients has different
goals. There are three types of goals for the doctor's
communication with his patient, namely, creating
good interpersonal relationships, exchanging
information, and making medical decisions. The
goals that are considered the most important in
solving patient's health problems especially in
patients with chronic diseases such as diabetes
mellitus that is creating good interpersonal and
communicative relationships will have a positive
impact on patients such as the realization of patient
knowledge and understanding, adherence to
medication and measurable health outcomes (Konsil)
Indonesian Medicine, 2006). In building good
interpersonal relationships, it takes important
elements, namely intimacy, attention, lack of tension,
and non-verbal expressions from doctors and patients.
In particular, good doctor and patient interpersonal
relationships will increase when the context of the
doctor's communication capabilities with patients
takes place with doctor friendliness, courtesy
behavior, social behavior and empathy behavior
during consultation (Larasati, 2019).
The results of the initial survey of several patients
who were willing to be interviewed found that many
patients considered doctors rarely greet patients at the
beginning of a consultation session, so this had an
impact on patients who were afraid to express their
complaints. Similarly, doctors do not provide
opportunities for patients to ask questions. The
average patient complains of not having enough
courage to ask about his illness in detail, so that in the
end it only follows the direction of the doctor. The
same applies to patients' complaints that doctors feel
less empathetic, such as eye contact with patients
during consultation sessions, or doctors who are
reluctant to touch in the sense of shaking hands with
patients. Yet through empathy with small things like
that, could be one of the factors that foster a sense of
trust in others. This study aims to analyze the effect
of interpersonal communication in improving the
quality of life of patients with diabetes mellitus.
Many patients with chronic diseases such as
diabetes mellitus have difficulty achieving optimal
blood glucose control, communication by medical
personnel plays an important role in supporting
patient health. Medical personnel may be more
successful when providing behavioral change
counseling based on psychological principles of self-
regulation, for example, setting goals, achieving
additional performance, and planning actions in
managing diabetes (Mulder, 2017).
Based on the review above, researchers feel that
until now there has been no research that examines
the effect of doctor communication on the quality of
life of patients with chronic diseases such as diabetes
mellitus. So in this study will summarize in detail
about how much impact the doctor's communication
in improving the quality of life of patients with
diabetes mellitus, and what communication factors
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
36
influence the improvement of the quality of life of
patients with diabetes mellitus itself.
2 METHOD
The type of research used in this study was a
quantitative survey using a cross-sectional approach.
The study was conducted at Dr. R.M. Djoelham City
of Binjai, which began in July-September 2019. The
population was all DM patients who were
hospitalized. From the medical records of general
inpatients there were 157 people and using an
accidental sampling technique, 60 respondents were
selected with criteria must be DM patients who
routinely undergo treatment / therapy more than once
as evidenced by medical records. In addition,
thepatients must be able to communicate well (can
read and write), be willing to be a respondent.
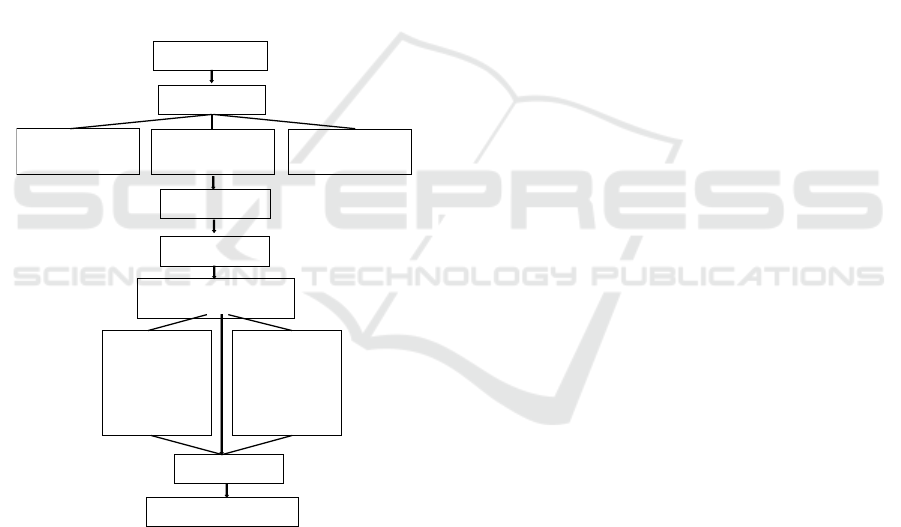
Figure1. Scheme of Research Process
Primary data were directly obtained through
interviews with respondents who were undergoing
DM treatment. Primary data include respondent
characteristics, doctor communication variables
(doctor's openness, doctor's empathy, doctor's
supporting attitude, doctor's positive attitude and
doctor's equality) and DM patients' quality of life
variables. Interviews were conducted based on a
questionnaire that had previously been tested for
validity and reliability. The doctor communication
variable contained 23 question items and 14 question
items for the variable quality of life of doctor patients.
Measurement results of the questionnaire using the
Guttman scale. The scale developed by Louis
Guttman is a scale that requires firm answers from
respondents, such as yes or no, true or false, ever or
never, and others. Evaluation of answers on the
Guttman scale, for a positive answer or yes given a
score of 1, while for a negative answer or not given a
score of 0. To anticipate the results of measurements
that are not absolute 100% or 0%, the researchers
used a range of percentage scale. The percentage
range in this study is <70% which means no role and>
70% is meant to play a role. The results of the
questionnaire were then analyzed using the chi-
square test to see the relationship between the
independent variables and the dependent variable.
Followed by logistic regression tests to see the effect
of the entire independent variable on the dependent.
The research procedure can be seen in Figure 1.
3 RESULTS
3.1 Validity and Reliability Analysis
Primary data were obtained directly through
interviews with respondents who were undergoing
DM treatment. Primary data include respondent
characteristics, doctor communication variables
(doctor's openness, doctor's empathy, doctor's
supporting attitude, doctor's positive attitude and
doctor's equality) and DM patients' quality of life
variables. Interviews were conducted based on a
questionnaire that had previously been tested for
validity and reliability. The doctor communication
variable contained 23 question items and 14 question
items for the variable quality of life of doctor patients.
Measurement results of the questionnaire using
the Guttman scale. The scale developed by Louis
Guttman is a scale that validity test is done using the
Pearson correlation method (Pearson Correlation)
where a question item can be said to be valid if the
product moment correlation coefficient value is
greater than the r table. From the test results of 25
questions for the doctor communication variable, 23
items were declared as valid statements, while the
remaining 2 question items were invalid. In 14 items
the statement of quality of life of DM patients was
declared valid. Furthermore, the reliability
measurement uses Cronbach's Alpha as a reference,
where if it is greater than 0.600 then the variable is
declared valid. The test results show the Cronbach's
Alpha value of the doctor communication variable
Preliminary Survey
Research Proposal
Research Design:
Cross Sectional Analysis
Population and Sample:
157 and 60 Respondents
Research Sites:
RSUD dr. Djoelham Binjai
Data Collection
Data Input and Coding
Data Analysis
Chi Square & Logistic Regression
Independent Variable:
Openness, empathy,
supportive attitude,
positive attitude, and
doctor's equality
Dependent Variable:
DM Patients Quality of
life
Analysis Results
Conclusions and Recommendations
Doctor’s Interpersonal Communication on the Quality of Life of Diabetes Mellitus Patients
37

and the quality of life of DM patients has a value >
0.6, which means that each variable was reliable.
Table 1. Characteristics of Respondents
No Characteristics n %
1
Sex
Female
Male
48
12
80,0
20,0
2 Age
≤40 years old
>40 years old
4
56
6,7
93,3
3 Level of education
High School
College
36
24
60,0
40,0
4 Type of work
Government employees
Entrepreneur
Housewife
Other types of work
11
15
10
24
18,3
25,0
16,7
40,0
5 Income
≤ Rp. 3.000.000
> Rp. 3.000.000
8
52
13,3
86,7
Table 1 shows frequency distribution of
respondent characteristics based on demographic data
which includes gender, age, education, occupation
and income. The characteristics of respondents
consists of 60 observed respondents, the majority of
respondents were female of 48 people (58.5%), aged>
40 years there were 56 people (93.3%), SLTA 36
people (60,0%), there were 24 other types of work
(40.0%), with income> Rp. 3,000,000 there were 52
people (86.7%).
3.2 Assessment Doctor’s Interpersonal
Communication
Based on the results of the questionnaire assessment
on doctor’s interpersonal communication indicators,
showed that of the 82 respondents, the majority of
respondents rated physician openness as good
(63.3%), the empathy of the doctor was good
(68.3%), the attitude of supporting the doctor was
good (71.7%), the positive attitude of the doctor was
good (63.3%), and the doctor's openness was also
categorized as good (55.0%). The results of
questionnaire measurements can be briefly seen in
Figure 1.
Figure 1 Measurement results of the questionnair
3.3 Chi Square Analysis
Table 2 shows the cross tabulation between the
independent and dependent variables. It is known that
based on the doctor's interpersonal communication,
the majority of patients consider doctors to be good
enough to serve diabetic patients. This can be seen
from several communication indicators such as
openness of doctors who are considered good
(63.3%), empathy of a good doctor (68.3%), good
doctor supportive attitude (71.7%), good doctor's
positive attitude (63.3%) and doctor's equality with
patients who are also good (55.0%). Furthermore,
from the results of the chi square analysis it is known
that only the variables of physician openness and
doctor empathy have a value of p <α, it can be
concluded that only physician openness and empathy
are related to the quality of life of patients with
diabetes mellitus and can proceed to further analysis.
Whereas the variables of supportive attitude, positive
attitude and equality have a value of p> α, so it was
concluded not having a significant relationship with
the quality of life of patients with diabetes mellitus.
In the results of the analysis with chi square it was
known that only the variables of physician openness
and doctor empathy have a value of p <α, it can be
concluded that there was a significant relationship
between openness and empathy variables with the
quality of life of DM patients. While the variables of
supportive attitude, positive attitude and equality
have a value of p> α, it can be concluded that there
was no significant relationship between the variables
of supportive attitude, positive attitude and equality
with the quality of life of DM patients. More details
can be seen in Table 2.
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
38

Table 2. Chi square analysis results
Quality of Life for DM
Patients
p-
value
Good Not good
n % n %
Doctor's
openness
Goo
d
22 57,9 16 42,1 0,003
Not goo
d
4 18,2 18 81,8
Empathy
the doctor
Goo
d
22 53,7 19 46,3 0,025
Not goo
d
4 21,1 15 78,9
Attitude
supports
Goo
d
21 48,8 22 51,2 0,249
Not goo
d
5 29,4 12 70,6
Positive
attitude
Goo
d
21 51,2 20 48,8 0,095
Not goo
d
5 26,3 14 73,7
E
q
ualit
y
Goo
d
13 39,4 20 60,6 0,603
Not
g
oo
d
13 48,1 14 51,9
In the results of the analysis with chi square it was
known that only the variables of physician openness
and doctor empathy have a value of p <α, it can be
concluded that there was a significant relationship
between openness and empathy variables with the
quality of life of DM patients. While the variables of
supportive attitude, positive attitude and equality
have a value of p> α, it can be concluded that there
was no significant relationship between the variables
of supportive attitude, positive attitude and equality
with the quality of life of DM patients.
3.4 Logistic Regression Analysis
Based on the candidate test results with chi square
obtained the results of the independent variables
openness, empathy, supportive attitude and positive
attitude have a p value <0.25. It can be concluded that
the independent variables of openness, empathy,
supportive attitude and positive attitude can be
continued to multivariate logistic regression analysis.
Multivariate analysis used is multiple logistic
regression analysis with prediction models that aim to
obtain a model consisting of several independent
variables that are considered best for predicting the
occurrence of the dependent variable. Variables that
are considered influential in the multivariate model
are variables that have p values <0.05.
In Table 3 shows the final model of the influence
of the variables openness and empathy) on improving
the quality of life of DM patients. The analysis
showed that the variables of physician's openness and
empathy had p value <0.05. This means that only the
two independent variables have a significant effect on
improving the quality of life of DM patients.
Table 3. Multivariate final model
Variable B
S.
E
Wald
D
f
p value OR
Openness
0,2
71
0,
04
1
3,711 1 0,006
3,50
1
Empathy
0,3
20
0,
13
6
5,292 1 0,001
4,52
0
Predictions of improving the quality of life of DM
patients affected by openness and empathy can be
explained as follows: in physicians' openness the
regression coefficient (𝛽) or OR was positive,
meaning that the better the doctor's openness was
likely to improve the quality of life of DM patients by
3,501 times higher when compared with doctor's
openness that was not good. In the doctor's empathy
variable the value of the regression coefficient (OR)
or OR was positive, meaning that the better the
empathy of the doctor has the opportunity to improve
the quality of life of DM patients about 4,520 times
higher when compared to the poor quality of life.
4 DISCUSSION
One element that will bring good relations between
doctors and patients is openness in communication.
In the element of openness, the doctor has the full
duty of making the patient believe in the services
provided by the doctor, so that the patient wants to
open himself honestly on the condition of his illness.
The effect of interpersonal communication between
doctor and diabetic patient which is seen from
openness starts from the interaction between doctor
and patient providing information about the patient's
health condition, about the procedure that the patient
must undergo during diabetes treatment and about
service facilities. Besides that, the doctor also
provides an explanation and understanding of the
benefits of treatment to patients during the
consultation session.
In the hospital studied, researchers saw that
interpersonal communication made by doctors while
conducting therapy was effective. Even under certain
conditions, some patients are still reluctant to give an
immediate description of their physical health.
Doctor’s Interpersonal Communication on the Quality of Life of Diabetes Mellitus Patients
39

According to several doctors interviewed, even
though it looks difficult, patient openness is needed
in the management of diabetes. Where there must be
a willingness to open up and reveal hidden
information such as being honest in terms of diet,
physical activity carried out up to taking medication
regularly. This is supported by the opinion of
Claramita (2013) who revealed that regardless of the
level of education, the form of communication that is
highly desired by many patients in Indonesia is more
open communication with their doctors.
Another aspect of interpersonal communication
that also plays a role in improving the quality of life
of diabetic patients is empathy from the doctor.
Empathy is one's ability to "know" what other people
are experiencing at any given moment, from that
other person's point of view. In the case of diabetes,
the empathy aspect is seen from the situation where
the doctor feels something like that experienced by
his patient. Empathic doctors are able to understand
the motivation and experience, feelings and attitudes
of patients, as well as the hopes and desires of patients
for the future.
Based on the findings and analysis, researchers
see that most patients feel very satisfied with the
empathy of the doctor who handles the treatment.
This can be seen by doctors intensely asking patient
complaints, paying attention to patients, and
understanding how they feel. Many diabetic patients
feel happy because they have the opportunity to
discuss their health problems. Patients feel given the
right to speak and get involved in their treatment.
Some patients even revealed that the main reason for
choosing the same hospital for their treatment was
satisfaction with the doctor's empathy when serving
their patients.
Ideas related to the development of physician
empathy for patients have previously been carried out
in a variety of different conditions as in the research
of Hussain (2020), revealing the motivational
interview method and promoting in-depth
understanding related to health management for long-
term conditions to patients can provide better results.
Basically, a very high level of patient satisfaction will
arise if the doctor understands and responds to what
the patient feels. The maximum level of empathy can
result in patient openness, and can even help the
doctor penetrate into the patient's soul where no other
treatment can achieve it, in other words empathy is
the most powerful therapeutic tool for diabetic
patients to improve their quality of life.
5 CONCLUSIONS
Based on the findings and analysis, it was found that
both physician communication and the quality of life
of DM patients studied were in the majority in the
good category. On the openness variable of doctors,
38 people (63.3%) rated good, 41 people (68.3%)
rated the variables of empathy and positive attitude of
good doctors, 43 people (71.7%) rated the attitude of
supporting physicians as good, 33 people (55.0%)
rated the doctor's openness variable as good and as
many as 26 people (43.3%) rated the quality of life of
DM patients to be good.
Furthermore, it can be concluded that the
variables that influence the improvement of the
quality of life of DM patients were physician
openness (p value = 0.006 <α), and doctor empathy
(p value = 0.001 <α). While attitudes supporting
physician variables (p value = 0,150> α), positive
doctor attitudes (p value = 0,421> α), and physician
equality (p value = 0,310> α) have no effect on
improving the quality of life of DM patients.
REFERENCES
Adriyani S., 2018. Buku Ajar Komunikasi Dalam
Keperawatan. Bandung: PT Refika Aditama,.
Beverly, Elizabeth A., PhD., 2018. Patient-Doctor
Communication and Diabetes Self-Care; Journal of
Clinical Outcomes Management. 2018 November;23
(11). Diakses pada 26 April 2020.
Cho NH, Shaw JE, Karuranga S, et al. IDF Diabetes Atlas:
Global estimates of diabetes prevalence for 2017 and
projections for 2045. Diabetes Res Clin Pract 2018;
138: 271–281.
Claramita, Mora. Doctor–patient communication in
Southeast Asia: a different culture. Adv in Health Sci
Educ (2013) 18:15–31, DOI 10.1007/s10459-012-
9352-5.
Farah A. 2019. Effects of Doctor Interpersonal
Communication on Low Satisfaction Levels of
Inpatients; Jurnal Komunikasi: Malaysian Journal of
Communication 35(1):57-70DOI: 10.17576/JKMJC-
2019-3501-05 Project: Communication apprehension
Among Tourism and Social Science Students. Diakses
pada 25 April 2020.
Firdous J and S. Hiba. 2019. Good communication between
doctor and patient improves health outcomes; EJMED,
European Journal of Medical and Health Sciences Vol.
1, No. 4, October 2019. Diakses pada 26 April 2020.
Fourianalistyawati E. Komunikasi Yang Relevan Dan
Efektif Antara Dokter Dan Pasien. J Psikogenes 2015;
1: 82–87.
Hussain, Saad, Mir. Role of Health Literacy and
Motivational Interviewing in Building Insight for Self-
management of Diabetes Mellitus. World Family
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
40

Medicine/Middle East Journal Of Family Medicine
Volume 18 Issue 2 February 2020. Diakses pada 16
Juni 2020.
Jalil Aisha, Rubeena Zakar, Muhammad Zakria Zakar3 and
Florian Fischer. 2017. Patient satisfaction with doctor-
patient interaction: study of mixed methods among
patients with diabetes mellitus in Pakistan; BMC
Health Services Research (2017) 17:155. DOI
10.1186/s12913-017-2094-6. Diakses pada 25 April
2020.
Junaid, A., & Rafi, M. 2019. Communication Barriers
Between Doctors, Nurses and Patients in Medical
Consultans at Hospitals of Lahore Pakestan. Pakistan
Armed Forces Medical Journal, 69(3), 560-65.
https://www.pafmj.org
/index.php/PAFMJ/article/view/ 3027. Diakses pada 25
April 2020.
Kementerian Kesehatan. Info Datin: Situasi dan Analisis
Diabetes. Jakarta, 2014.
Kholil Syukur, Lahmuddin Lubis, Syafruddin Ritonga.
2019. Implementation of Communication Therapy at
Dr. Hospital Pirngadi; Budapest International
Research and Critics Institute-Journal (BIRCI-Journal)
Volume 2, No 4, November 2019, Page: 645-656 e-
ISSN: 2615-3076 (Online), p-ISSN: 2615-1715
(Print).DOI: https://doi.org/ 10.33258/birci. v2i4.673.
Diakses pada 26 April 2020.
Konsil Kedokteran Indonesia. Komunikasi Efektif Dokter-
Pasien. 2006.
Kurtz S, Draper J, Silverman J. Teaching and Learning
Communication Skills in Medicine. Oxon: Radcliffe
Medical Press, 1998.
Larasati TA. Komunikasi Dokter-Pasien Berfokus Pasien
pada Pelayanan Kesehatan Primer Patient Centered
Communication in Primary Care. J Kedokt Univ
Lampung 2019; 3: 160–166.
Masriadi. Epidemiologi Penyakit Tidak Menular. Jakarta:
Trans Info Media, 2016.
Mulder C, Anne Marike Lokhorst. 2017. Effective Nurse
Communication with Type 2 Diabetes Patients: An
Overview; Western Journal of Nursing Research. DOI:
10.1177/0193945914531077. Diakses pada 25 April
2020.
Passaribu B. 2019. Effect of Doctor's Interpersonal
Communication on Patient Satisfaction at Royal Prima
General Hospital Medan; International Journal of
Research & Review (www.ijrrjournal.com) 164 Vol.6;
Issue: 11; November 2019. Diakses pada 25 April 2020.
Pemerintah Republik Indonesia. Undang-Undang Nomor
29 Tahun 2004 Tentang Praktik Kedokteran. 2004.
Sarah. 2020. Impact of Communication in Health Care;
Institute for Healthcare Communication. Diakses pada
26 April 2020.
Susan C, Baker. Bernadette M, Watson. 2018. How
Patients Understand Their Doctor's Communication:
Implications for Patients' Willingness to Communicate;
Journal of Language and Social Psychology.
https://doi.org/10.1177/0261927X15587015. Diakses
pada 25 April 2020.
Tanveer Fahad, Sana Shahid2, Muhammad Mansoor
Hafeez. 2018. Impact of Doctor's Interpersonal
Communication Skills on Patient Satisfaction; Isra
Medical Journal | Volume 10 - Issue 5 | Sep–Oct 2018.
Diakses pada 26 April 2020.
Trinth Daniel. 2019. Trust Factors: The Role of
Interpersonal Communication and Physical Touch in
the Patient Physician Relationship. Thesis. Honors
Baccalaureate of Science in Biochemistry & Molecular
Biology. Diakses pada 26 April 2020.
Turnip, A., Andrian, Turnip, M., Dharma, A., Paninsari, D.,
Nababan, T., Ginting, C.N., 2020. An application of
modified filter algorithm fetal electrocardiogram
signals with various subjects, International Journal of
Artificial Intelligence, vol. 18, no., 2020.
Wijaya, C., Andrian, M., Harahap, M., Turnip, A., 2019.
Abnormalities State Detection from P-Wave, QRS
Complex, and T-Wave in Noisy ECG, Journal of
Physics: Conference Series, Volume 1230, (2019)
012015. doi:10.1088/1742-6596/1230/1/012015.
Doctor’s Interpersonal Communication on the Quality of Life of Diabetes Mellitus Patients
41
