
Clinical Presentation and Risk Factor of Cruris Ulcer in Sanglah
General Hospital, Denpasar, Indonesia
Made Wardhana
1*
, Martina Windari
1
, Sissy
1
, Hasri Dewi
1
, Vebryanti Karna
1
, L. M. Rusyati
1
1
Department of Dermatology and Venereology, Faculty of Medicine, Udayana University/
Sanglah General Hospital, Bali
*
Corresponding author
Keywords: ulcus cruris, clinical pretersation, risk factors
Abstract: Leg ulcers often referred to as cruris ulcers refer to skin discontinuities with the loss of the epidermis, and
part of the dermis or the entire dermis, generally occurring in the lower limbs due to various disease
processes and other causative factors. Cruris ulcers can also be defined as leg ulcers that do not show signs
of healing in less than four weeks. The exact cause has not been acknowledged, but some conditions such as
illness can play a role in causing this disease. Some theories related to the diseases underlying the cruris
ulcer are venous disorders around 80%, arterial disorders around 5%, and trauma or infections around 5%.
The cruris ulcer due to neuropathic disease occurs in about 5% of cases, as a result of peripheral neuropathy,
usually in patients with diabetes and leprosy, local paresthesias, or lack of sensation, at pressure points on
the feet can cause prolonged microtrauma, eventually ulceration. Other causes are systemic disease and
malignancy. Ulcers are often preceded by a disruption of venous flow (chronic venous insufficiency) which
then develops into static dermatitis, which in turn develops into small ulcers that are increasingly larger.
Cruris ulcers are usually chronic, occur in overweight patients, pregnancy, smoking, using tight clothing,
and long-standing physical activities.
In this retrospective descriptive study, clinical forms were observed, and several factors were considered as
triggers for the leg ulcers. In the present study, the cruris ulcer was caused by the weakness of the vein 18
(58.1%), neuropathic 6 (19%), arterial 4 (12.9%), and infection/trauma 3 (9.8%).
1 INTRODUCTION
Leg ulcers often referred to as cruris ulcers refer to
skin discontinuities with the loss of the epidermis,
and part of the dermis or the entire dermis, generally
occurring in the lower limbs due to various disease
processes, such as chronic venous insufficiency.
Cruris ulcers are usually chronic, occur in
overweight patients, pregnancy, smoking, using tight
clothing, and long-standing physical activities.
Cruris ulcers can also be defined as leg ulcers that
do not show signs of healing in less than four weeks.
It is often preceded by chronic venous insufficiency
and then develops into static dermatitis and
eventually becomes a small ulcer.
Classification of cruris ulcer, varies greatly, but
in principle, are: 1. Tropic ulcer, due to trauma,
hygiene and nutrition, and infection by Bacillus
fusiformis and Borreliaviincentii, 2. Varikosum
ulcer, due to chronic venous insufficiency, 3.
Arteriosum ulcer, caused by disturbed circulation
which results in arterial failure in sending oxygen
and nutrients to the lower limbs, resulting in cell
death and tissue damage, and 4. Neurotrophic ulcers,
due to peripheral neuropathy, and nerve damage,
causing disturbances in the legs, due to increased
pressure or mild injury, the most common cause of
peripheral neuropathy is diabetes and morbus
Hansen.
This disease is generally caused by several
conditions as follows; chronic venous insufficiency
- around 80%, arterial disorders - around 15%, and
other causes (including diabetes and rheumatoid
arthritis, systemic diseases and malignancies) -
around 5%.
Wardhana, M., Windari, M., Sissy, ., Dewi, H., Karna, V. and Rusyati, L.
Clinical Presentation and Risk Factor of Cruris Ulcer in Sanglah General Hospital, Denpasar, Indonesia.
DOI: 10.5220/0009991204450448
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 445-448
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
445
2 METHODS
In this study using retrospective observations, we
observed medical records of patients diagnosed with
cruris ulcer from 2015-2018. Thirty-one cases of
cruris ulcer were observed. All patients aged
between 45-65 years. Several factors are listed as
possible trigger factors such as family history,
activity, obesity, and underlying disease. Also noted
clinical forms such as; form of ulcer, ulcer size,
number of ulcers, and location of ulcer.
3 RESULTS
A total of 31 cases of cruris ulcer were observed, all
patients aged between 45-65 years. Eleven cases
(61.1%) were preceded by static dermatitis (venous
insufficiency), in nine female patients who had a
body mass index above 26. Eighteen cases (58.1%)
due to chronic venous insufficiency, 6 cases (19.4%)
with neuropathic (3 with morbus Hansen, 3 with
diabetic ulcers), 4 cases with arterial insufficiency
ulcers and 3 cases (9.8%) due to infections such as
cellulitis/erysipelas. Factors that play a role in the
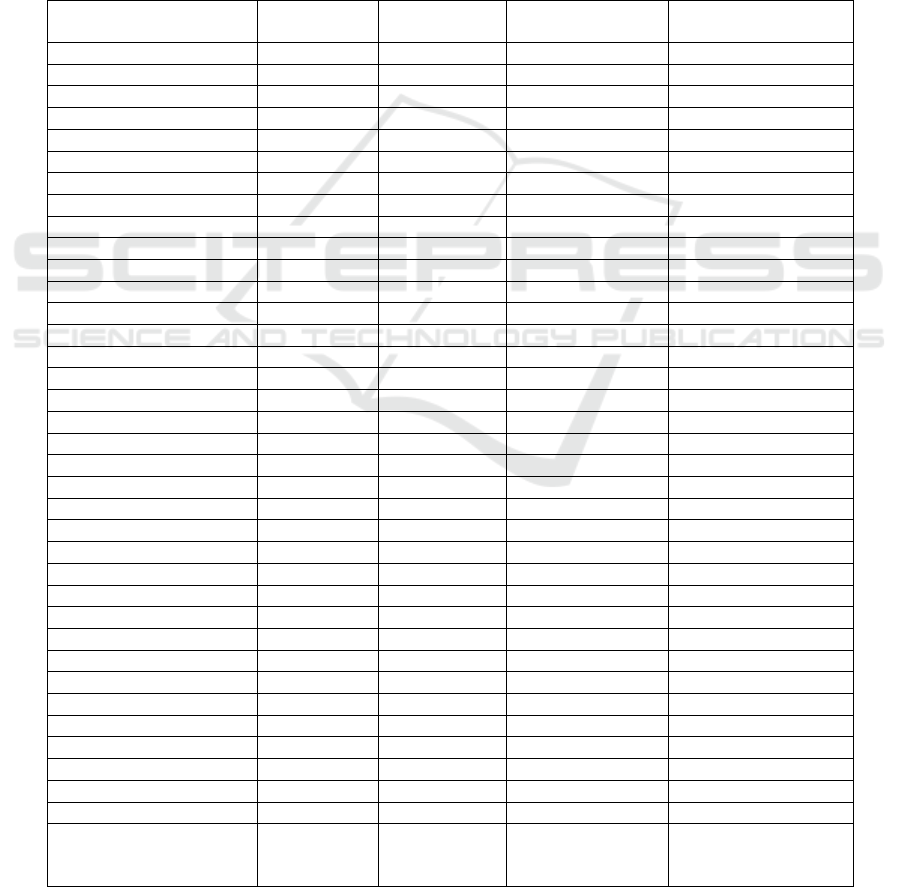
cruris ulcer can be seen in Table 1. below.
Table 1: Clinical presentation and risks
Venous(%)
18 (58.1)
Arterial (%)
4 (12.9)
Neuropathic (%)
6 (19.4)
Infection/Injury(%)
3 (9.8)
Gender
Male (%) 4 (12.9) 2 (6.4) 1(3.2) 2(6.4)
Female (%) 14 (45.2) 2 (6.4) 5(16.1) 1(3.2)
Age
< 50 years (%) 3(9.7) 1(3.2) 2(6.4) 1(3.2)
> 50 years (%) 15(48.4) 3(9.7) 4(12.9) 2(6.4)
Lama sakit (durasi)
1-5 tahun 5(16.1) 1(3.2) 1(3.2) 2(6.4)
> 5 tahun 13(41.9) 3(9.7) 5(16.1) 1(3.2)
Localization (dominant)
Area I-Tungkai (%) 5(16.1) 1(3.2) 1(3.2) --
Area II-Pedis (%) 10(32.2) 2(6.4) 2(6.4) 3(9.7)
Area III-Plantar pedis (%) 3(9.7) 1(3.2) 3(9.7) --
Clinical features
Round shape 5(16.1) 1(3.2) 2(6.4) 1(3.2)
Geographical shape 13(41.9) 3(9.7) 4(12.9) 2(6.4)
Number of ulcers
Single 7(22.6) 1(3.2) 4(12.9) 2(6.4)
Multiple 11(35.5) 3(9.7) 2(6.4) 1(3.2)
Size of ulcer
Mild < 2 cm
2
(%) 6(19.3) 1(3.2) 1(3.2) --
Moderate 2-5 cm
2
(%) 9(29.0) 2(6.4) 3(9.7) 1(3.2)
Severe > 5 cm
2
(%) 3(9.7) 1(3.2) 2(6.4) 2(6.4)
Family history
Yes (%) 10(32.2) 2(6.4) 3(9.7) 2(6.4)
No (%) 8(25.8) 3(9.7) 3(9.7) 1(3.2)
Activity
Standing > 8 hrs (%) 11(35.5) 3(9.7) 3(9.7) --
Standing < 8 hrs (%) 7(22.6) 1(3.2) 3(9.7) 3(9.7)
Obese (BMI)
BMI < 25 5 1(3.2) 2(6.4) 1(3.2)
BMI > 25 13(41.9) 3(9.7) 4(12.9) 2(6.4)
Underlying diseases
Static dermatitis/venous 8(25.8) 2(6.4) 3(9.7) 1(3.2)
Diabetes 3(9.7) 1(3.2) 2(6.4) 2(6.4)
Hipertensi 7(22.6) 1(3.2) 1(3.2) --
Vascuilardoppler
(ABPI)
(No data)
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
446

Figure 1. Clinical presentation
4 DISCUSSION
Leg ulcers often referred to as cruris ulcers refer to
skin discontinuities with the loss of the epidermis,
and part of the dermis or the entire dermis, generally
occurring in the lower limbs and soles of the feet
caused by various disease processes. The most
common cause is chronic venous insufficiency.
Classification of cruris ulcer, varies greatly, but in
principle, are: 1. Tropic ulcer, due to trauma,
hygiene and nutrition, and infection by Bacillus
fusiformis and Borreliaviincentii, 2. Varikosum
ulcer, due to chronic venous insufficiency, 3.
Arteriosum ulcer, caused by disturbed circulation
which results in arterial failure in sending oxygen
and nutrients to the lower limbs, resulting in cell
death and tissue damage, and 4. Neurotrophic ulcers,
due to peripheral neuropathy, and nerve damage,
causing disturbances in the legs, due to increased
pressure or mild injury, the most common cause of
peripheral neuropathy is diabetes and morbus
Hansen.
Cruris ulcers are usually chronic, occur in
overweight patients, pregnancy, smoking, using tight
clothing, and long-standing physical activities. A
total of 31 cases of cruris ulcer were observed, all
patients aged between 45-65 years. Eleven cases
(61.1%) were preceded by static dermatitis (venous
insufficiency), in nine obese female patients.
Eighteen cases (58.1%) due to chronic venous
insufficiency, 6 cases (19.4%) with neuropathic (3
with morbus Hansen, 3 with diabetic ulcers), 4 cases
with arterial insufficiency ulcers and 3 cases (9.8%)
due to infections such as cellulitis/erysipelas.
In this retrospective descriptive study,
clinical forms were observed and several factors
were considered as triggers for the leg ulcer. In this
study the cruris ulcer was caused by the weakness of
veins 18 cases (58.1%), neuropathic 6 cases (19%),
arterial 4 cases (12.9%), and infection/trauma 3
cases (9.8%). Venous disease is the main causative
Clinical Presentation and Risk Factor of Cruris Ulcer in Sanglah General Hospital, Denpasar, Indonesia
447

factor for more than two-thirds of all leg ulcers:
Venous disease - about 80% of leg ulcers, Arterial
disease - about 15% of leg ulcers, and other causes
(including diabetes and rheumatoid arthritis and
some rare conditions) - about 5% of cruris ulcers. In
9 female patients and 4 male, who had a body mass
index above 26, eleven patients have long-standing
physical activities, (35.5%) with standing activities
more than 8 hours a day.
5 CONCLUSION
Most cases of cruris ulcers in this study were due to
chronic venous insufficiency, and neuropathic. The
clinical features are geographic, multiple, and have a
history of more than five years of ulcers. Obesity
and long-standing physical activities also play a role
in the cruris ulcer. The therapy given is generally
conventional, namely with ulcer treatment, and also
with some other modalities, such as PRP (platelet-
rich plasma) and Low Laser Biostimulation.
ACKNOWLEDGMENTS
I would like to thank our patients from the
Dermatology Department, Sanglah General Hospital,
for their technical help. I also thank all patients who
kindly participated in the study.
CONFLICT OF INTEREST
The authors declare that they have no conflict of
interest related to the publication of this manuscript.
REFERENCES
Agale SV. Chronic Ulkuskruriss: Epidemiology,
Aetiopathogenesis,and Management. Hindawi
Publishing Corporation Ulcers Volume 2013, Article
ID 413604, 9 pages
Prakash S, Tiwary KS, Mishra M, and Khanna AK.
Venous Ulkuskruris: Review Article. Surgical Science.
2013; 4: 144-150
Barbetta FM, Mazzucato EL, Salathiel AM, Foss NT, and
Frade MAC. Retrospective Analysis of Ulkuskruriss
cases at the Univercity Hospital, University of Sao
Paulo. Med CutanIberLat Am: 2009; 37[1]:28-32
Frade MAC, Soares SC, Foss NT, Cursi IB, Rubeiro WS,
Andrade FF, and Vantos SV.Ulkuskruris: An
Observational Study in Juiz de For a, MG Brazil and
Region. An Bras Dermatol. 2005;80[1]: 41-46
Robertson L, Amanda J. Gallagher K, Carmichael SJ,
Evans CJ, McKinstry BH, Simon CA. Paul L. et al.
Risk factors for chronic ulceration in patients with
varicose veins: A case control study. J VascSurg
2009;49:1490-8.)
Mekkes JR,Loots MA, Van Der Wal ACandBos JD.
Causes, investigation and treatment of
ulkuskrurisation.British Journal of Dermatology 2003;
148: 388–401.
Rayner R, Carville K, Keaton J, Prentice J &Santamaria N.
Ulkuskruriss: atypical presentations and associated
comorbidities .Wound Practice and Research Volume
17 Number 4 – November 2009 : 168-185
Wollina U,Naser MBA, Hansel G, Helm C, Koch A,
Konrad H, Schonlebe J, Unger L, and Köstler E.
Ulkuskruriss Are a Diagnostic and Therapeutic
ChallengeLower Extremity. Wounds 4(2);2005: 3-7
O'Brien', M. Clarke-Moloney PA. Perry G and Burke PE.
Ulkuskruriss: A Cross-Sectional Survey of
Management Practices and Treatment Costs in Ireland
1. F..Phlebology (2002) '7:98-102
Nelzn O, Bergqvist D, and Lindhagen A. Ulkuskruris
etiology-A population study cross sectional. J Vasc
Surg. 1991;14:557-64.
Vlajinac H, Marinkovic J, Maksimovic M, and Radak D.
Factors Related To Venous Ulceration: A Cross-
Sectional Study. Angiology 2014, Vol. 65(9) 824-830
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
448
