
Probable Dress Syndrome: A Case of Drug Hypersensitivity
in Young Man
Vera Madonna Lumbantoruan1*, Edison Harianja2
1Department of Dermato-Venereology, Faculty of Medicine, Mulawarman University, Samarinda East Kalimantan and
Samarinda Medika Citra Hospital, Samarinda East Kalimantan, Indonesia
2Department of Clinical Pathology Samarinda Medika Citra Hospital, Samarinda East Kalimantan, Indonesia
*Corresponding author
Keywords: DRESS syndrome, RegiSCAR, steroid systemic
Abstract: Drug reaction with eosinophilia and systemic symptoms (DRESS) is one of drug hypersensitivity reaction.
This condition shows a broad spectrum of clinical manifestations and severity. RegiSCAR scoring system is
one of the diagnostic criteria exist for the diagnosis DRESS syndrome. The objective of this case report is to
present a case of Probable DRESS syndrome without eosinophilia as one of Drug induced Severe Cutaneous
Adverse Reactions (SCARs) in a young man. A 23 years old man admitted to hospital with generalized
cutaneous rash and blood laboratory abnormality after consumed cefadroxyl, paracetamol and allopurinol for
2 weeks. Diagnosis Probable DRESS syndrome was made using RegiSCAR scoring system. Treatment with
prolonged steroid systemic showed good clinical and laboratory result.
1 INTRODUCTION
Drug induced Severe Cutaneous Adverse Reactions
(SCARs) include drug reaction with eosinophilia and
systemic symptoms (DRESS), Acute Generalized
Exanthematous Pustulosis (AGEP) and Stevens-
Johnson Syndrome - Toxic Epidermal Necrolisis
(SJS-TEN). DRESS syndrome is a rare case of drug
reaction, comes with extensive rash, haemotology
abnormalities and systemic involvement. This
condition could be fatal with high mortality rate if it
not handled immediately (Waseem et al, 2016;
Choudhary et al, 2013).
Clinical manifestations in DRESS Syndrome is
occuring about 2-8 weeks after introduction of the
causative drug. Pruritic maculopapular and purpura
cutaneous rash, with edema on fasial and extremities,
fever and periferal lymphadenopathies are the usual
symptoms of DRESS syndrome. Eosinophilia with
atypical lymphocytes, elevated liver enzymes and the
renal involvement were usually found in DRESS
syndrome (Choudhary et al, 2013; Watanabe, 2018).
Making diagnosis for DRESS syndrome could be a
challenging for the clinicians since the clinical
manifestations are not immediately appeared after
introduction of causative drugs (Choudhary et al,
2013). The diagnosis of DRESS syndrome is mainly
clinical and clinician must consider the latency period
and the diversity of signs and symptoms. Use of the
term DRESS has been sometimes doubtful, because
eosinophilia is not constantly found in clinical
finding and the cutaneous and systemic signs are
variable (Um et al, 2010). Making the right
differential diagnosis of the type of SCARs is
important since treatment, follow up and prognosis of
different SCARs may not be the same (Casagrada et
al, 2017). It is essential to consider this diagnosis
since the life-threatening potential of DRESS
syndrome is high and mortality is estimated as
about10 percents (Choudhary et al 2013). The
International study group investigating severe
cutaneous reactions (SCAR) has developed
RegiSCAR as one of diagnostic criteria for DRESS
syndrome (Waseem et al, 2016).
The objective of this case report is to present a case
of Probable DRESS syndrome without eosinophilia
as one of Drug induced Severe Cutaneous Adverse
Reactions (SCARs) in a young man.
Lumbantoruan, V. and Harianja, E.
Probable Dress Syndrome: A Case of Drug Hypersensitivity in Young Man.
DOI: 10.5220/0009991104410444
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 441-444
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
441

2 CASE
A 23 years-old man was admitted to hospital with
three days history of generalized rash, starting on the
face and then extending to the trunk and lower
extremities. He also complained of swelling and
erosion on the lips. From anamnesis there is history
of fever 3 weeks before. He went to a clinic and
doctor gave him antibiotic cefadroxyl and
paracetamol. In addition he consumed allopurinol by
himself. After 2 weeks consumed the medications, he
realized had skin rash appeared on the face. He
immediately stopped consumed all of the pills but
rash still widespread to the trunk and ekstremities,
and also he got swelling in his lips. On physical
examination he presented fever of 390C with
generalized erythema maculopapular rash, purpuric
lesions on the trunk and lower extremities, edema and
erosion on the lips. Lymphadenopathy was found on
the coli region. Laboratory examination showed a
slightly increased of Serum Glutamic Pyruvate
Transaminase (SGPT) 33 µ/L (Normal value (NV) 5-
31µ/L), blood ureum 62,2 mg/dl (NV 10-50 mg/dl)
and the presence of lymphocyte athypical. According
to RegiSCAR diagnosis criteria this patient’s score of
5 that could be classified as Probable DRESS
syndrome. Systemic corticosteroid therapy with
methylprednisolone intravenous was started from the
first day at a dose of 90mg (Body weight 85 kg) a day
and gradually decrease over a week, and supportive
local treatment for the skin and mucosal involvement.
Any other medications were also stopped. Within a
week we observed a significant improvement in
clinical condition and laboratory result showed SGPT
14µ/L. We continued therapy with
methylprednisolone oral and tappered off slowly for
2 weeks later.
Figure 1. Cutaneous rash found on the trunk and face of the patient on 1st day
Figure 2. Clinical improvement after 3 weeks followed up
3 DISCUSSION
Drug reaction with eosinophilia and systemic
symptoms (DRESS) was first defined in 1996 by
Bocquet et al, present with extensive rash, fever,
lymphadenopathy, hematologic abnormalities and
organ involvement(Waseem et al, 2016). Use of the
term DRESS has been inconsistent, since
eosinophilia is not a constant clinical finding. Some
literature use Drug-induced hypersensitivity
syndrome (DIHS)/DRESS to include both the DIHS
and DRESS syndrome. DHIS/DRESS was first
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
442
described by Chaiken et al in 1950. The most
common clinical presentation of DHIS/DRESS are
cutaneous eruption, fever and enlarged lymph nodes
4
.
RegiSCAR scoring system is one of the most
used diagnostic criteria exist for diagnosis of DRESS
syndrome.This RegiSCAR was developed by an
international study group investigating severe
cutaneous reactions (SCAR).
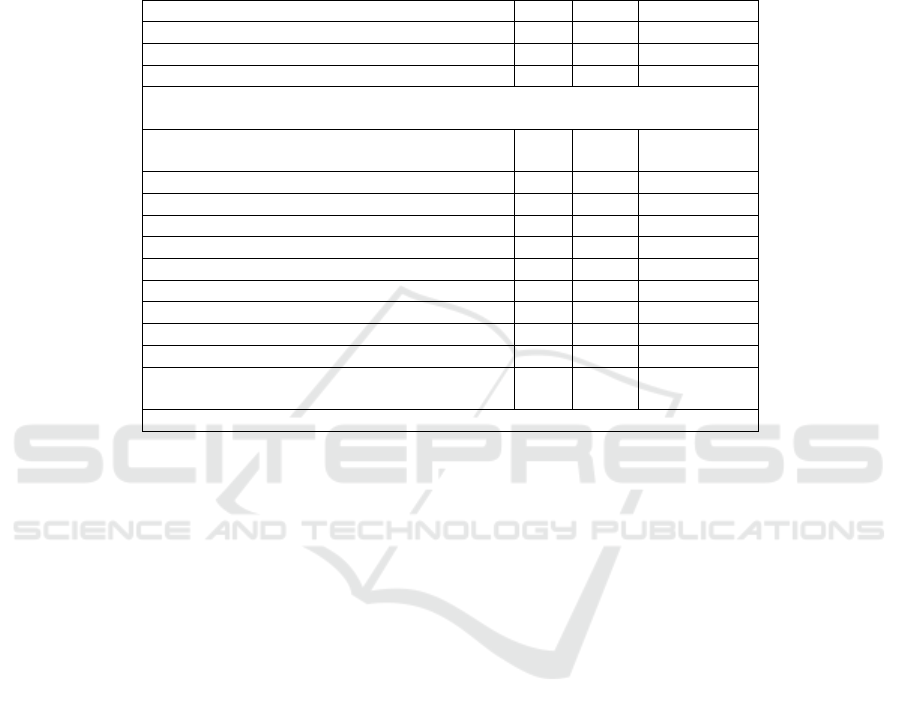
Table 1. RegiSCAR diagnosis score for DRESS
1
Features no Yes Unknown
Fever (≥ 38,5
0
C) -1 1 -1
Enlarged lymph nodes (≥2 sites, ≥1cm) 0 1 0
Athypical lymphocytes 0 1 0
Eosinophilia:
700-1499 or 10%-19,9%
0 1 0
≥ 1500 or ≥ 20% 0 2 0
Skin rash :
Extent >50% 0 1 0
At least 2: edema, infiltration, purpura, scalling -1 1 0
Biopsy suggesting DRESS -1 0 0
Internal organ involvement:
one 0 1 0
Two or more 0 2 0
Resolution in more than 15 days -1 0 -1
At least 3 biological inv done and negative to
exclude alternative diagnosis
0 1 0
Final score: <2 = no ; 2-3= possible; 4-5= probable; >5= definite.
According to RegiSCAR criteria this patient was
diagnosed with Probable DRESS syndrome with
score 5 for the presence of fever, athypical
lymphocyte, extent skin rash >50% with purpuric
lesions, facial edema and scalling with liver and renal
involvement.
The onset of symptoms in DRESS syndrome is
often delayed. It may took 2-8 weeks after
introduction of triggering drug. Fever and rash were
the most common symptoms. Lymphadenopathy in
more than one sites is common and may occur in 75%
cases (Choudhary et al, 2013; Corneli et al,2017). In
this case, cutaneous rash appeared after 2 weeks
consumed cefadroxyl, paracetamol and allopurinol.
There was also fever and lymphadenopathy found
only at coli region.
Systemic organ involvement was common in
DRESS syndrome and liver is the most common
organ involved. Liver failure is the most common
cause of death. Renal abnormalities may occur in
11% patients, and commonly associated with
allopurinol
(Lens et al, 2010;Alexander et al,2013). In
this case there was slightly elevated of SGPT and
blood ureum that considered as the involvement of
liver and renal organ.
Hematologic abnormalities in DRESS syndrome
present with leukocytosis or leucopenia, eosinophilia
or atypical lymphocytes. In this case there was no
eosinophilia but we found the presence of atypical
lymphocyte. The presence of atypical lymphocyte
was found in 67% cases reported by the RegiSCAR
study group, while eosinophilia was demonstrated by
95% cases (Watanabe, 2018; Corneli et al,2017).
Studies about atypical lymphocyte found that this
reactive lymphocyte have been associated with viral
infection and plays an important role in the immune
response (Cho.2017)
In this case there were some clinical entities share
same features with Stevens-Johnson syndrome (SJS),
the erosion of lip mucosal that usually found in SJS,
and eosinophil count still in normal range. But, the
delayed onset and the presence of fever and atypical
lymphocyte could be directing our diagnosis to
DRESS syndrome.
Some medicines had implicated in triggering
DRESS syndrome, there were anticonvulsants
(phenytoin,carbamazepine), antidepressants
(desipramine, amitriptiline), sulpha drugs,NSAIDS,
antibiotics (minocycline,linezolide, doxycycline,
piperacilin-tazobactam), antivirals (abacavir,
telaprevir, zalcitabine), ACE inhibitors (enalapril),
Beta blockers (atenolol) and also allopurinol
(Waseem et al, 2016). In this case we could not
identified the causal drug with certainty, since our
Probable Dress Syndrome: A Case of Drug Hypersensitivity in Young Man
443

patient consumed cefadroxyl (2
nd
generation of
sephalosporin), paracetamol and allopurinol in the
same time period. Literatures have been reported
sefalosporine and allopurinol as potential trigger
drugs in DRESS syndrome (Corneli et al,2017;Kim et
al,2014).
The pathophysiology of DRESS is still unclear. It
is hypothesized by a complex mechanism. Genetic
factor might be plays a role in the incidence of drug
hypersensitivity, including DRESS syndrome.
Genetic deficiency of detoxifying enzymes needed to
drug metabolism, and some Human Leucocyte
Antigen (HLA) have been reported associated with
drug hypersensitivity (Choudhary et al, 2013;
Watanabe, 2018). Reactivation of Human Herpes
Virus 6 (HHV-6), Epstein-Barr virus and
cytomegalovirus have been suggested had a close
relationship with DRESS syndrome
1,6
. However, the
exactly mechanism for this viral reactivation theory is
still unclear, is it direct effect of the defect in drugs
metabolism or effect of the “cytokine storm” that
could be found in viral reactivation (Waseem et al,
2016;(Cho et al,2017)
Systemic steroids have been used in the
management of drug hypersensitivity cases, including
DRESS Syndrome. In some cases of DRESS
syndrome, relapses have been occured after
withdrawal or tappering off. Dosage, duration of
treatment and situations where steroids should be
used are not clearly defined. Some authors suggest the
use of corticosteroid systemic at a dose equivalent to
1 mg/kg/day of prednisone in case with sign severity
including liver or renal involvement, pneumonia, or
cardiac involvement. The use of systemic steroids for
a prolonged period with a gradual decrease is
important in DRESS syndrome to avoid relapses
(Silva-Feistner et al,2017). In this case, we gave
methylprednisolone intravenous at 90 mg starting
dose and tappering off over a week, then continued
with slow tappering off oral methylprednisolon. Our
patient showed good improvement and there was no
relapses after 2 weeks followed up.
4 CONCLUSION
We report here a case of Probable DRESS syndrome
in a 28 years old man, probably due to cefadroxyl
and/or allopurinol, which was diagnosed by
RegiSCAR validation scores. Our patient showed
good clinical result with steroid systemic therapy in
a slowly tappering off within 3 weeks.
REFERENCES
Alexander T, Iglesia E, Park Y, Duncan D, Peden D, Sheikh
S, Ferris M. 2013. Severe DRESS syndrome managed
with therapeutic plasma exchange. Pediatrics. Vol. 131.
Number 3.
Casagranda A, Suppa M, Dehavay F, Marmol V. 2017.
Overlapping DRESS and Stevens-Johnson
Syndrome:case report and review of the Literature.
Case Rep Dermatol.
Cho Y, Yang C, Chu C. 2017. Drug reaction with
eosinophilia and systemic symptoms (DRESS): an
interplay among drugs, viruses, and Immune system.
Int. J. Mo. Sci. 18.
Choudhary S, McLeod M, Torchia D, Romanelli P. 2013.
Drug reaction with eosinophilia and systemic
symptoms (DRESS) syndrome. The journal of clinical
and aesthetic dermatology. Vol. 6. Number 6.
Corneli HM. 2017. DRESS Sundrome: Drug reaction with
eosinophilia and systemic symptoms. Pediatric
Emergency care. Vol. 13. Number 7.
Lens S, Crespo G, Carrion JA, Miquel R, Navasa M. 2010.
Severe acute hepatitis in the dress syndrome: report of
two cases. Annals of hepatology. Vol. 9. No.2.
Kim D, Koh Y. 2014. Comparison of diagnostic criteria
and determination of prognostic factors for drug
reaction with eosinophilia anda systemic symptoms
syndrome. Allergy Asthma Immunol Res. 6(3).
Silva-Feistner M, Ortiz E, Rojas-Lechuga MJ, Munoz D.
2017. Drug reaction with eosinophilia and systemic
symptoms (DRESS) syndrome in paediatrics. Clinical
case. Rev Chil Pediatr. 88.
Um SJ, Lee SK, Kim YH, Son CH, Roh MS, Lee MK. 2010.
Clinical features of Drug-Induced Hypersensitivity
Syndrome in 38 patients. J Investig Allergol Clin
Immunol. Vol. 20(7).
Waseem D, Latief M, Sofi N, Dar I, Khan Q, Abbas F, Sofi
P. 2016. Dress Syndrome: A review and update. Skin
diseases & skin care. Vol.1. No.18.
Watanabe H. 2018. Recent advances in drug-induced
hypersensitivity syndrome/Drug raction with
eosinophilia and systemic symptoms. Journal of
immunology research.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
444
