
A Case Series: A Successful of Alternative Modality with Red Light
Low Level Laser Therapy for Acne Vulgaris
Rudi Chandra
1*
, Nelva K. Jusuf
1
, Khairina Nasution
1
1
Department of Dermatology & Venereology, Universitas Sumatera Utara,
Universitas Sumatera Utara Hospital, Medan
*Corresponding auhtor
Keywords: Acne vulgaris, low level laser therapy, red light
Abstract: Introduction: acne vulgaris is a chronic inflammatory disease ofpilosebaceous units where the key factors of
pathogenesis including follicular hyperkeratinization, microbial colonization of Propionibacterium acnes,
increase sebum production, and complex inflammatory mechanisms. Low level laser therapy (LLLT) has
been proposed as an alternative therapeutic modality to treat acne vulgaris with less side effects compared to
other treatment options. Case: 22-yo man and 28-yo woman, who were suffering from moderate acne
vulgaris, treated with red light LLLT (655 nm, <5mW CW, 57 mrad) twice a week, interval 3 days, and 3
minutes duration per treatment area. Follow up was taken for 4 weeks by lesions count and photographs.
Both patients got significant lesions reduction, with final total reduction after 8 sessions in 4 weeks for both
patients were 63,3% and 74%, respectively. Final reductions of inflammatory lesions in both patients were
69,7% and 75,9%, respectively. And final reduction of non-inflammatory lesions (comedones) in both
patients were 56% and 70,6%, respectively. Discussion: Red light LLLT plays roles in the pathogenesis of
acne, through its mechanism of actions in interfere sebum secretion of sebaceous glands, change
keratinocytes behaviors, modulate cytokines to reduce inflammations, and suppressing microbial
colonization of Propionibacterium acnes. Conclusion: Red light LLLT was effective as an alternative
modality in reducing both non-inflammatory and inflammatory type lesions in acne vulgaris. The
mechanism of actions of LLLT as the treatment of acne vulgaris are through its roles in the pathogenesis of
acne.
1 INTRODUCTION
Acne vulgaris is a chronic inflammatory disease of
the pilosebaceous units. Acne vulgaris is the most
common skin disorder, affects virtually all
individuals at least once.Incidence peaks in 18-
years-old, but substantial numbers of 20- to 40-
years-old also develop the disease and observed
equally in both genders (Aydemir et al, 2014). Acne
vulgaris is characterized by skin with scaly red skin
(seborrhea), comedones, papules, nodules, pimples
and scarring. Acne affects skin having dense
sebaceous follicles in areas including face, chest and
back. Acne may be of inflammatory or non-
inflammatory forms (Suva et al, 2014).
Acne is a complex disease with multifactorial
pathogenesis and considerable variation in severity.
Key factors in the pathogenesis of acne including
follicular hyperkeratinization, microbial colonization
of Propionibacterium acnes(P. acnes), increase
sebum production, and complex inflammatory
mechanisms (Zaenglein et al, 2016). Various
modalities had been proposed for the treatment of
acne, where most modalities work by counteracting
microcomedones formation, sebum production,
Propionibacteriumacnes, and inflammation.
Unfortunately these currently available treatment
options, still show an inadequate response in several
patients, while others suffer from actual adverse
effects (Zaenglein et al, 2012).
Low level laser therapy (LLLT) has been
proposed as an alternative therapeutic modality to
treat acne vulgaris with less side effects compared to
other treatment options (Avci et al, 2013). LLLT
uses either coherent light sources (lasers) or non-
coherent light sources consisting of filtered lamps or
light-emitting diodes (LED) or, on occasion, a
combination of both. The mechanism of action of
402
Chandra, R., Jusuf, N. and Nasution, K.
A Case Series: A Successful of Alternative Modality with Red Light Low Level Laser Therapy for Acne Vulgaris.
DOI: 10.5220/0009990204020406
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 402-406
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
LLLT for acne is through the absorption of light
(specifically blue light) by porphyrins that have been
produced by P. acnes as a part of its normal
metabolism, that act as endogenous photosensitizers,
and causes a photochemical reaction and forms
reactive free radicals and singlet oxygen species,
which in turn lead to bacterial destruction. Red light
is known to penetrate deeper in tissues when
compared with blue light, can affect the sebum
secretion of sebaceous glands and change
keratinocyte behavior. Furthermore, red light might
also exert its effects by modulating cytokines from
macrophages and other cells, which in turn could
reduce inflammation (Avci et al, 2013; Al-Salam et
al, 2014).
2 CASE REPORTS
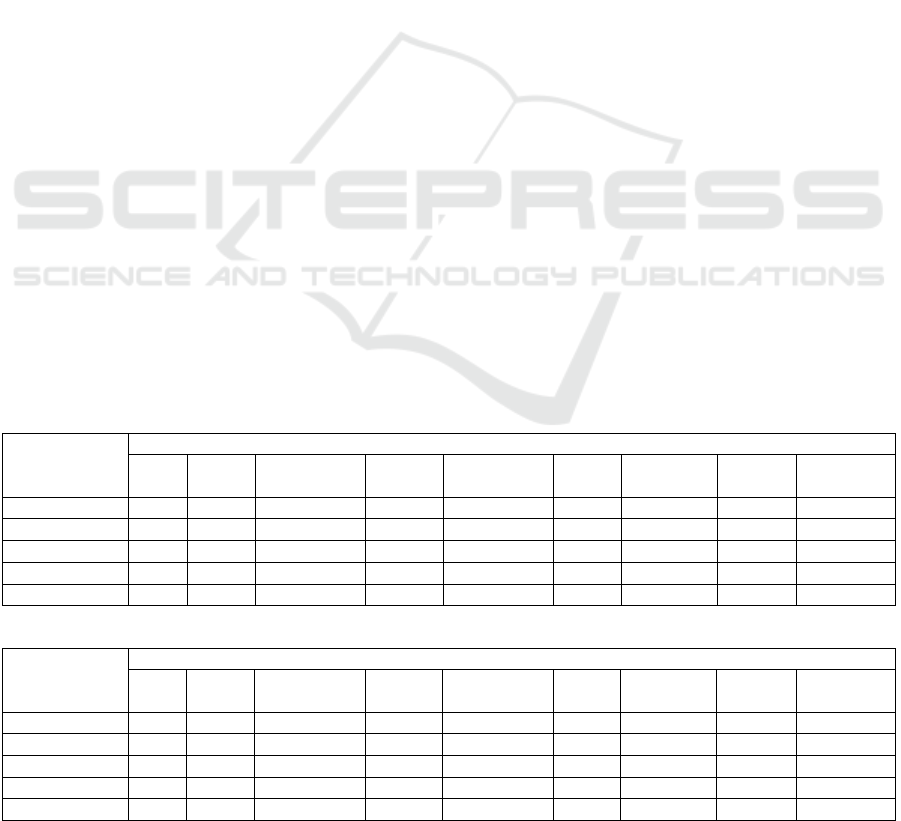
2.1 Patient 1
A 22-year-old man who has been suffering from
acne vulgaris since he was fifteen. He complained
from acneiform eruptions and scars, mainly affecting
his forehead, cheeks, and chin. Patient had positive
family history for acne vulgaris. Patient never
treated his acne, but patient often squeezed his
pimples.On dermatological examination found
mainly papules, some pustules, nodules, and
comedones (Figure1). Based on acne grading
evaluation by Lehmann in 2002, the lesions were
counted (table 1) total 60 lesions and categorized as
moderate acne vulgaris. Patient was treated with
visible red light LLLT (655 nm, <5mW CW, 57
mrad) twice a week, interval 3 days, and 3 minutes
duration per treatment area. Follow up was taken for
4 weeks by lesions count and photographs.
2.2 Patient 2
A 28-year-old woman who has been suffering from
acne vulgaris since one year ago. She complained
from acneiform eruptions, mainly affecting her
forehead, cheeks, and chin. Patient had negative
family history for acne vulgaris. Patient had treated
her acne with several topical treatment from online
store, but no significant effect. On dermatological
examination found mainly papules, some pustules,
and comedones (Figure 2). Based on acne grading
evaluation by Lehmann in 2002, the lesions were
counted (table 1) total 46 lesions and categorized as
moderate acne vulgaris. Patient was treated with
visible red light LLLT (655 nm, <5mW CW, 57
mrad) twice a week, interval 3 days, and 3 minutes
duration per treatment area. Follow up was taken for
4 weeks by lesions count and photographs.
At follow up, both patients got significant
lesions reduction, with final total reduction after 8
sessions in 4 weeks for both patients were 63,3%
and 74%, respectively. Final reduction of papules
were 40% (patient 1) and 64,3% (patient 2). Final
reduction of pustules were 93% (patient 1) and
86,7% (patient 2). Final reduction of nodules were
100% (patient 1). Final reductions of inflammatory
lesions after 8 sessions in 4 weeks in both patients
were 69,7% and 75,9%, respectively. And final
reduction of non-inflammatory lesions (comedones)
in both patients were 56% and 70,6%, respectively.
Both patients showed satisfactory results in acnes’
reductions (table 1 and 2).
Table 1. Acne lesions count in patient 1.
Lesions Patient 1
Day
0
Day 7 Reduction
(%)
Day 14 Reduction
(%)
Day
21
Reduction
(%)
Day 28 Reduction
(%)
Papules 15 19 +26 13 13 10 33 9 40
Pustules 14 7 50 5 64 4 71 1 93
Nodules 4 2 50 1 75 - 100 - 100
Comedones 27 23 15 17 37 15 44 12 56
Total 60 51 15 32 47 29 52 22 63,3
Table 2. Acne lesions count in patient 2.
Lesions Patient 2
Day
0
Day 7 Reduction
(%)
Day 14 Reduction
(%)
Day
21
Reduction
(%)
Day 28 Reduction
(%)
Papules 14 18 +29 10 29 8 43 5 64,3
Pustules 15 11 27 8 47 3 80 2 86,7
Nodules - - - - - - - - -
Comedones 17 13 33 10 41 5 71 5 70,6
Total 46 42 9 28 39 16 65 12 74
A Case Series: A Successful of Alternative Modality with Red Light Low Level Laser Therapy for Acne Vulgaris
403
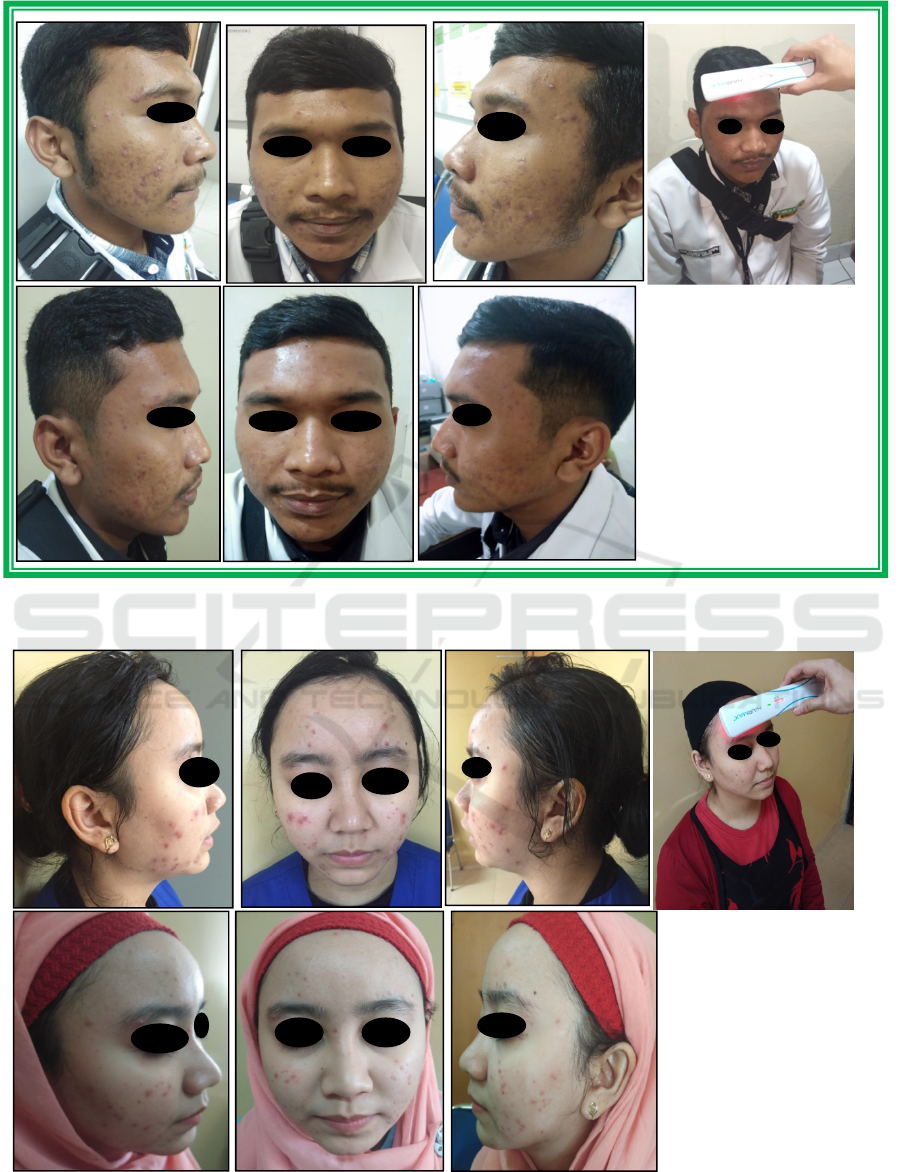
Figure 1. A 22-yo male with moderate acne vulgaris; (A), (B), (C) before treatment ; and (D), (E), (F) after 8 sessions of red
light LLLT treatments.
Figure 2. A 28-yo female with moderate acne vulgaris; (A), (B), (C) before treatment ; and (D), (E), (F) after 8 sessions of
red light LLLT treatments.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
404

2 DISCUSSION
The pathogenesis of acne is not completely
understood, but the current hypothesis in the
pathogenesis of acne including four major events:
follicular hyperkeratinization, microbial colonization
of P. acnes, increase sebum production, and
complex inflammatory mechanisms. (Zaenglein et
al, 2012).
Usually the treatments of acne work by
counteracting microcomedones formation, sebum
production, P. acnes, and inflammation. Nowadays,
it has been proposed that low level laser therapy
could treat acne vulgaris with less side effects
compared to other treatment options. (Avci et al,
2013)
LLLT knows as biostimulation
orphotobiomodulation laser. Biomodulations defined
as changing the natural biochemical response of
cells or tissue within the normal range of its
function. (Avci et al, 2013) it appears that LLLT has
a wide range of effects at the molecular, cellular, and
tissue levels. The basic biological mechanism behind
the effects of LLLT is thought to be through
absorption of red and (nearly infrared) NIR light by
mitochondrial chromophores, in particular
cytochrome-c-oxidase (CCO), which is contained in
the respiratory chain located within the
mitochondria, (Avci et al, 2013;Karu et al,2005) and
perhaps also by photoacceptors in the plasma
membrane of cells. Consequently, a cascade of
events occur in the mitochondria, leading to
biostimulation of various processes. (Avci et al,
2013) Absorption spectra obtained for CCO in
different oxidation states were recorded and found to
be very similar to the action spectra for biological
responses to the light. (Avci et al, 2013;Karu et
al,2005) It is hypothesized that this absorption of
light energy may cause photo dissociation of
inhibitory nitric oxide from CCO, leading to
enhancement of enzyme activity, electron
transport,mitochondrial respiration, and adenosine
triphosphate production. (Papageorgiou et al,2000)
In turn, LLLT alters the cellular redox state, which
induces the activation of numerous intracellular
signaling pathways, and alters the affinity of
transcription factors concerned with cell
proliferation, survival, tissue repair, and
regeneration. (Avci et al, 2013;Karu et al,2005)
The mechanism of actions of red light LLLT in
the pathogenesis of acne are through its effects in
interfere sebum secretion of sebaceous gland sand
change keratino cytes behaviors. Furthermore, red
light might also exert its effects by modulating
cytokines from macrophages and other cells, which
in turn could reduce inflammation. Also, the
absorption of light by porphyrins that have been
produced by P. acnes as a part of its normal
metabolism, and that act as endogenous
photosensitizers. This process causes a
photochemical reaction and forms reactive free
radicals and singlet oxygen species which in turn
lead to bacterial destruction (Avci et al, 2013;Al-
Salam et al,2014)
From this mechanisms, it revealed
that LLLT plays role in reducing follicular
hyperkeratinization, suppressing microbial
colonization of P. acnes, decreasing sebum
production, and reducing inflammations in the
pathogenesis of acne.
In our case series, we modified the use of red
light LLLT tool which is usually used for alopecia or
hair loss, by treating acnes per area for 3 minutes.
Both patients got significant lesions reduction, with
final total reductions after 8 sessions in 4 weeks for
both patientswere 63,3% and 74%, respectively.
Final reduction of non-inflammatory lesions
(comedones) for both patients were 56% and 70,6%,
respectively. And final reduction of inflammatory
lesions for both patients were 69,7% and 75,9%,
respectively. Several studies had reported the usage
of LLLT in acne vulgaris, but most of them using
combination of blue and red light LLLT.
Papageorgiouet al. reported the mean improvement
of 76% in inflammatory lesions and 57% in
comedones. (Papageorgiou et al,2000) Goldberg et
al. reported mean lesion count reduction 46% after 4
weeks, after 12 weeks 81%, where the severe acne
showed a marginally better response than mild acne,
but comedones did not respond as well as
inflammatory lesions.(Goldberg et al,2006) Lee et
al. reported final mean improvements in non-
inflammatory lesions (34,28%) and infl ammatory
lesions (77.93%), and also brightened skin tone and
improved skin texture were spontaneously reported
by 14 patients. (Lee et al,2007). Sadick reported
final average reduction of acne was 69% at the
12
th
weeks assessment.(Sadick et al,2008) All the
reports above were using the combination of blue
and red light LLLT in their treatment of acne. Aziz-
Jalali et al. compared the usage of red light (630 nm)
and Infrared LLLT (890 nm) with results after 10
weeks treatment, acne lesions were significantly
decreased in the side treated by 630 nm (27.7±12.7
to 6.3±1.9), but not significant in the site treated by
890 nm (26.9±12.4 to 22.2±8.5).(Aziz-Jalali et
al,2012)
Our treatment method for acne, alternating red
light LLLT, was easy to deliver, well-tolerated,
pain- and side-effect free, and gave a satisfyingly
A Case Series: A Successful of Alternative Modality with Red Light Low Level Laser Therapy for Acne Vulgaris
405

high clearance rate in patients with non-
inflammatory and inflammatory acne. Unfortunately,
there was a limitation in this case series because of
relativelyshortfollow-upperiod to its longterm
efficacy and side effects. However,the high
percentage of clearance in the non-inflammatory and
inflammatory acne after 4 weeks treatment
assessment, and the concordance of this result with
other studies, mean that further investigationto
determine the efficacy and to optimize the treatment
parameters for red light LLLT.
3 CONCLUSION
Red light LLLT was effective as an alternative
modality in reducing both non-inflammatory and
inflammatory type lesions in acne vulgaris. The
mechanism of actions of red light LLLT as the
treatment of acne vulgaris are through its roles in the
pathogenesis of acne by reducing follicular
hyperkeratinization, suppressing microbial
colonization of P. acnes, decreasing sebum
production, and reducing inflammations.
REFERENCES
Al-Salam FA, Afify W. 2014. Low Level Laser Therapy in
Dermatology. The Gulf Journal of Dermatology and
Venereology 21(2):1-14.
Aydemir, E.H. 2014. Acne vulgaris.TürkPedArş. 49:13-6.
DOI:10.5152/tpa.2014.1943
Avci P, Gupta A, Sadasivam M, et al. 2013. Low-level
laser (light) therapy (LLLT) in skin: stimulating,
healing, restoring. SeminCutan Med Surg 32(1): 41–
52.
Aziz-Jalali MH, Tabaie SM, Djavid GE. 2012.
Comparison of Red and Infrared Low-level Laser
Therapy in the Treatment of Acne Vulgaris.Indian J
Dermatol. Mar 2012; 57(2):128–130.
Goldberg DJ, Russell BA. 2006. Combination blue (415
nm) and red (633 nm) LED phototherapy in the
treatment of mild to severe acne vulgaris. J Cosmet
Laser Ther. 8(2):71–75.
Lee SY, You CE, Park MY. 2007. Blue and red light
combination LED phototherapy for acne vulgaris in
patients with skin phototype IV. Lasers Surg Med.
39(2):180–188.
Karu TI, Kolyakov SF. 2005. Exact action spectra for
cellular responses relevant to phototherapy. Photomed
Laser Surg. 23(4):355–361. [PubMed: 16144476]
Papageorgiou P, Katsambas A, Chu A. 2000.
Phototherapy with blue (415 nm) and red (660 nm)
light in the treatment of acne vulgaris. Br J Dermatol.
142(5):973–978.
Sadick NS. 2008. Handheld LED array device in the
treatment of acne vulgaris. J Drugs Dermatol.
7(4):347–350.
Suva MA, Patel AM, Sharma N, et al. 2014. A Brief
Review on Acne Vulgaris: Pathogenesis, Diagnosis
and Treatment. RRJoP. 4(3):1-12.
Zaenglein AL, Pathy AL, Schlosser BJ, et al. 2016.
Guidelines of care for the management of acne
vulgaris. J Am AcadDermatol. J Am AcadDermatol,
Zaenglein AL, Graber EM, and Thiboutot DM. 2012. Acne
Vulgaris and Acneiform Eruptions. In : Goldsmith
L.A., Katz S.I., Gilchrest B.A., Paller A.S., Leffell
D.J., Wolff K. (Eds.) : Fitzpatrick’s Dermatology In
General Medicine. 8
th
edition. New York : McGraw-
Hill Companies. p.897-917.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
406
