
Verrucous Hemangioma
Nur Camelia
1*
, Syamsul Arifin
1
, Yosep Ferdinand Rahmat Sugianto
1
, Diah Adriani Malik
1
,
Yan Wisnu Prajoko
2
, Meira Dewi Kusuma Astuti
3
1
Departement of Dermatovenereology, Faculty of Medicine, Diponegoro University / Dr. Kariadi General Hospital
2
Departement of Surgery, Faculty of Medicine, Diponegoro University / Dr. Kariadi General Hospital
3
Departement of Anatomical Pathology, Faculty of Medicine, Diponegoro University / Dr. Kariadi General Hospital
Keywords: Verrucous hemangioma, vascular proliferation, excision
Abstract: Verrucous Hemangioma (VH) is a rare congenital vascular malformation consisted of capillary or cavernous
hemangioma affecting dermis and subcutaneous tissue. VH usually presents at birth or early childhood,
often unilateral and localized on the lower extremity. The clinical presentation shows hyperkeratotic plaques
and nodules, bluish-purple, and partly confluent. Early diagnosis and treatment are pivotal for a satisfactory
cosmetic result. A 28-year-old male presented with an asymptomatic rough lump on the left leg which
gradually enlarged, thickened and became rougher through time. The lesion appeared since birth and was
flat with red-bluish color, Dermatologic examination showed hyperkeratotic plaques and nodules, black-
grey colored, confluent with defined margins, measured 10 x 4 cm on lower left leg. Histopathologic
examination revealed epidermis hyperkeratosis, verrucous growth, acanthosis, elongated rete ridges, and
blood vessels proliferation in the dermis. The patient was treated with cryosurgery, and propranolol tablets 2
x 10 mg and subsequently referred for surgical excision. Diagnosis of VH is hallmarked by hyperkeratotic
nodules and confirmed by skin biopsy. Excision is one of the recommended treatment whenever possible.
The patient was treated with broad and deep excision due to the high recurrence of VH. After four months
of evaluation, the lesion showed satisfactory healing without signs of recurrences. The prognosis was quo
ad vitam ad bonam, ad sanam and ad cosmetikam dubia ad bonam. We have reported a patient with VH
treated by surgical excision, which showed satisfactory healing without signs of recurrences.
1 INTRODUCTION
Verrucous hemangioma (VH) is a rare congenital
vascular malformation, consisting of a proliferation
of dilated blood vessels of different sizes that occupy
the dermis and subcutaneous tissue. The epidermis of
the affected area shows a robust proliferative reaction
that presents as a warty appearance (fatani et al,
2016).
Verrucous hemangioma is rare, and only a few
cases have been reported (Nupur et al, 2014).
The
exact incidence is difficult to determine as it has been
referred to by many different names in the past (Laun
et al, 2019).
Verrucous hemangioma has been
reported under various names in the literature until
1967, including unilateral verrucous hemangioma,
hemangioma unilateralis neviforme, nevus vascularis
unius lateris, nevus angiokeratoticus, keratotic
hemangioma, nevus keratoangiomatosus, and papular
angiokeratoma (Fatani et al, 2016; Laun et al, 2019).
Verrucous hemangioma usually presents at
birth or in early childhood and then gradually
progresses in size with age (Laun et al, 2019; Dhanta
et al, 2018). It often unilateral and localized on the
lower extremity (Fatani et al, 2016; Dhanta et al,
2018 ; Sandhu et al, 2016).
The clinical presentations
are hyperkeratotic plaques and nodules, bluish-
purple, and partly confluent. The initial lesions
present as flat red or bluish lesions that slowly
enlarge and become verrucous (Dhanta et al, 2018 ;
Sandhu et al, 2016; Oppermann et al, 2018).
The
lesions are usually scattered but linear, serpiginous
and reticular patterns can be seen rarely. The linear
arrangement of these lesions usually reflects genetic
mosaicism or dermatomal distribution (Dhanta et al,
2018).
Verrucous hemangioma linear is a rarer
presentation, according to our literature search, only
10 cases have been reported until 2016 (Sandhu et
al, 2016).
394
Camelia, N., Arifin, S., Sugianto, Y., Malik, D., Prajoko, Y. and Astuti, M.
Verrucous Hemangioma.
DOI: 10.5220/0009989903940398
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 394-398
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
A skin biopsy is needed to confirm the clinical
diagnosis (Fatani et al, 2016).
Verrucous
hemangioma, histologically characterized by dilated
capillaries and large cavernous spaces, lined by
endothelium. These dilated spaces extend into the
reticular dermis and subcutaneous fat. The overlying
epidermis shows reactive hyperplasia with marked
acanthosis, hyperkeratosis, and papillomatosis
(Bindhuja et al, 2013).
Early diagnosis and treatment are pivotal for a
satisfactory cosmetic result. The treatment of choice
for VH is surgical excision. Various therapeutic
options such as cryotherapy, ultrasonography,
electrocautery, NdYAG laser, and laser pulse-dye
can be considered as additional therapy, especially
for smaller lesions and when excision is not possible
(Laun et al, 2019; Sandhu et al, 2016; Prabhakar et
al, 2015).
This case is reported to increase our
understanding of making an accurate diagnosis of
VH and choosing an appropriate treatment.
2 CASE
A 28-year-old Indonesian man presented to the
outpatient Dermatovenereology Departement Dr.
Kariadi Hospital Semarang with complaints of
asymptomatic rough lump on the left leg, which
gradually enlarged, thickened and became rougher
through time. These lesions had been present since
birth, and the initial lesion was flat with red-bluish
color. There was no history of any trauma or
bleeding from these lesions. The patient gave a
history of about 14 years ago that he had been taken
by his mother for treatment, and some of the lesions
had been excised. There was a recurrence of the
lesion after several years. The clinical notes and
histopathological reports of the previous excision
were not available.
On physical examination, the patient was
composmentis. Height 168 cm, weight 67 kg, blood
pressure: 120/70 mmHg, heart rate: 84 beats/minute,
respiratory rate: 22 breaths/minute, and axillar
temperature: 36,7
o
C. There were no enlarged lymph
nodes in the inguinal or in the area around the lesion.
On clinical examination showed hyperkeratotic
plaques and nodules in a linear pattern, black-grey
colored, confluent with defined margins, measured
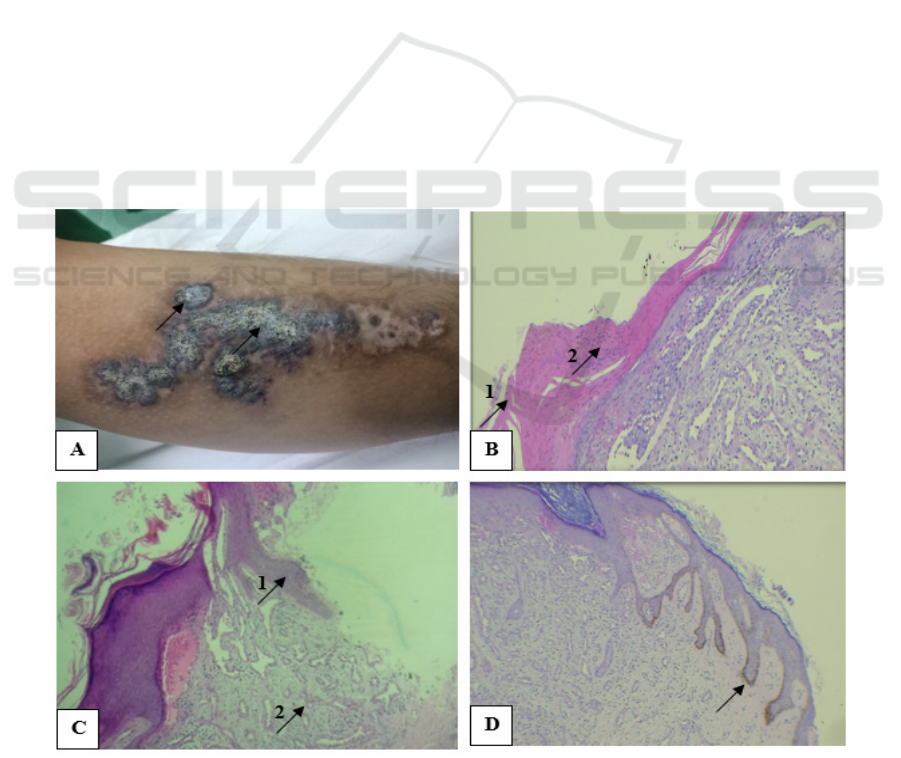
10 x 4 cm on the lower left leg (Figure 1.A).
Figure. 1. A. Hyperkeratotic plaques and nodules in a linear pattern, black-grey colored, confluent with defined margins on
the lower left leg. B. 1. Hyperkeratosis, 2. Parakeratosis (Hematoxylin & eosin, x40). C. 1. Acanthosis, 2. The proliferation
of blood vessels in the superficial dermis (Hematoxylin & eosin, x10). D. Elongated rete ridge (Hematoxylin & eosin, x10).
Verrucous Hemangioma
395
The routine laboratory and coagulation factors
examination result were standard. The lesion was
biopsied and confirmed to be a verrucous
hemangioma. Histopathological examination
showed the epidermis in the form of a stratified
squamous cell epithelium, keratinized,
hyperkeratosis, parakeratosis, verrucous growth,
elongated rete ridge, acanthosis containing a
proliferation of partially dilated blood vessels lined
with endothelial cells, with lumen containing
erythrocytes surrounded by epidermal papillae. In
the superficial dermis, there was the varying size of
blood vessel proliferation, skin adnexa accompanied
by a mild distribution of interstitial
lymphohistiocytic. No malignancy sign found
(Figure 1. B-E).
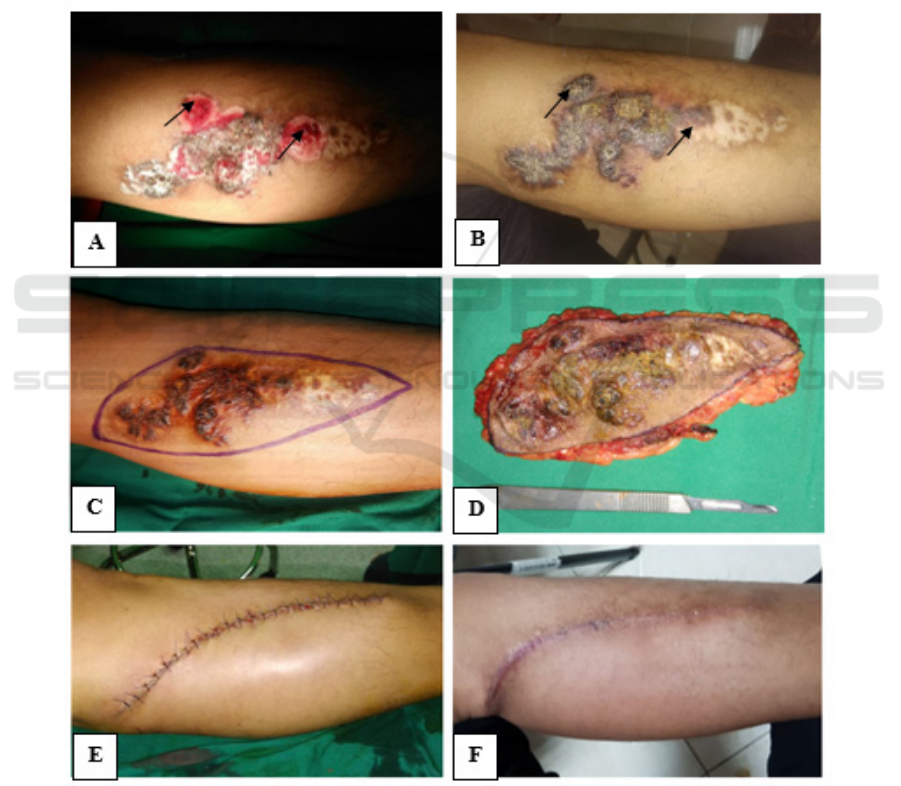
Previously this case had been treated with
cryotherapy, propranolol tablets 2x10 mg, and
retinoid acid 0,1% cream applied twice daily. After
ten days of evaluation post, cryotherapy showed that
the lesion had a mild regression. Propanolol tablets
and retinoid acid 0,1% cream were still continued.
However, after three months of evaluation, the
lesions recurred (Figure 2. A-B). Due to recurrence,
the patient was referred to the surgery department
for excision. All the lesions were excised with a 1
cm margin (Figure 2.C-F).
Figure. 2. A. The lesions immediately following the cryotherapy procedure. B. Recurrence of the lesion after three months
post cryotherapy (black arrow). C. The resected margin was 1 cm away from the lesions. D. The lesions were completely
excised. E. Postoperative photography following surgical excision. F. After four months of evaluation, the lesion showed
satisfactory healing without signs of recurrences.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
396

3 DISCUSSION
The term VH is defined by Imperial and Helwig in
1967, which means that congenital localized
vascular malformations. (fatani et al, 2016; (Dhanta
et al, 2018; Prabhakar et al, 2015).
In 1996, The
International Society for the Study of Vascular
Anomalies classified vascular anomalies into
vascular malformations, and vascular tumors.
(J.Bindhuja et al,2013 Diagnosis of VH is
established based on clinical features and
histopathological examination. Prabhakar et al,
2015;Nargis et al,2017).
Verrucous hemangioma presents on the lower
extremity in 95% of cases and typically is unilateral
(Laun et al, 2019;Singh et al,2017) It may also
involve unusual anatomic locations such as the
abdomen, arm, and glans penis. Although VH
almost invariably presents at birth or in early
childhood, it may appear later on, even in adult life
(Sandhu et al, 2016; Singh et al,2017) In our case,
the lesion appeared from birth and located on the
lower left leg.
In the early phase of evolution, the lesions are
non-keratotic, soft, blue/red plaques, and clearly
demarcated. Gradually the lesions become
increasingly hyperkeratotic and verrucous (Nargis et
al,2017;Moss et al,2010). The lesions may vary in
size from roughly 0,5 to 8 cm in diameter and maybe
single or grouped. (Laun et al, 2019)
Verrucous
hemangioma in its mature phase presents as
hardened, hyperkeratotic plaques or nodules with a
brownish to bluish-black appearance. This is often
accompanied by a history of tenderness and/or
bleeding following minimal trauma.(Vijayan et
al,2016) The linear form of VH is rare, and only a
few cases have been reported. It is not known
whether linear lesions actually follow Blaschko’s
lines or the linear arrangement represents genetic
mosaicism. (Nupur et al, 2014) In our case, the
lesion showed in a linear pattern, and there was no
history of any trauma or bleeding from these lesions.
Histologically, VH shows with hyperkeratosis,
variable epidermal acanthosis, and papillary
telangiectasias overlying a deep capillary or
cavernous hemangioma. The abnormal proliferating
vessels are situated in the dermis and hypodermis.
The hemangiomatous component mostly comprises
dilated capillaries and wider cavernous,
endothelium-lined, blood-filled spaces.
Inflammatory cells, fibrosis, and hemosiderin may
exist in the upper dermis. (fatani et al, 2016;
J.Bindhuja et al,2013; Moss et al,2010). Typical
histopathological features were observed in our case
also. Immunohistochemical staining with endothelial
markers like CD 31, CD 34 and GLUT1 may be
done for confirmation, but the diagnosis can be
made by light microscopic features alone.
(J.Bindhuja et al,2013;(Vijayan et al,2016)
The differential diagnosis with angiokeratoma
can be excluded. The histologic appearance closely
resembles angiokeratoma, as both lesions show
vascular spaces beneath a papillomatous and
hyperkeratotic epidermis. However, in contrast to
angiokeratoma, the vascular spaces in VH also
involve the lower dermis and subcutaneous tissues.
(Oppermann et al, 2018;.Naveen et al,2016)
Verrucous epidermal nevus (VEN) also can be
excluded because histologically, the hallmark
finding of VEN is hyperkeratosis, acanthosis, and
papillomatosis. In VEN, there are no abnormal
proliferation of blood vessels (Das et al, 2015)
Verrucous hemangioma should be identified,
diagnosed, and treated as early as possible to limit
the extent of resection. Because of the risk of
recurrence, resection should encompass the deep
portions of the lesion with usually a 1 cm margin of
excision. If the lesion is small (<2 cm), cryosurgery,
electrocautery, or laser therapy can be used, but
resection is the primary treatment. These additional
therapies can be used in combination with resection
for extensive lesions to further assist in reducing the
risk of recurrence. (Laun et al, 2019)
In our case, a
propanolol tablet was given for three months, but
after that, there was a recurrence. Propranolol is the
treatment of choice for troublesome haemangiomas.
Other studies that have employed oral propranolol
therapy would not recommend using it on other
vascular anomalies. Oral propranolol is more
effective in hemangioma infantile than in an
adult.(Dimaguila et al,2017)
Surgical excision is one of the recommended
treatment whenever possible, and Incomplete
excision leads to persistence, recurrence, and
continued enlargement of the lesion. Due to the
deeper vascular infiltration, the recurrence rate of
VH is 33%, especially when the lesions are more
significant than 2 cm in diameter (Dhanta et al,
2018) The patient was treated with broad and deep
excision. After evaluation for four months, the lesion
showed satisfactory healing without signs of
recurrences.
The prognosis for VH is excellent, with
recurrence being low when adequate surgical
margins are utilized and if in combination with
additional therapies. If inadequate wide excision is
performed, recurrence can exceed 30%.(Laun et al,
2019) The prognosis of this case was quo ad vitam
Verrucous Hemangioma
397

ad bonam, quo ad sanam, and quo ad cosmeticam
dubia ad bonam.
4 CONCLUSION
We have reported a case of verrucous hemangioma
in a 28-years old male. The diagnosis was made on
the basis of anamnesis, clinical examination, and
histopathological examination. On the anamnesis,
the patient complained of asymptomatic rough lump
on the left leg, which gradually enlarged, thickened,
and became rougher through time. The lesion
appeared since birth and was flat with red-bluish
color. The clinical examination, we found
hyperkeratotic plaques and nodules in a linear
pattern, black-grey colored, confluent with defined
margins, measured 10 x 4 cm on lower left leg.
Histopathological examination confirmed the
diagnosis of verrucous hemangioma. The patient
was treated with broad and deep surgical excision,
which showed satisfactory healing without signs of
recurrences. The prognosis of this case was quo ad
vitam ad bonam, quo ad sanam dubia ad bonam, and
quo ad cosmeticam dubia ad bonam.
REFERENCES
Das A, Podder I, Das A, Ghosh A, Shome K. 2015.
Epidermolytic blaschkoid verrucous epidermal nevus:
Report of two cases. Indian J Dermatopathol Diagn
Dermatol. 2: 46-8.
Dhanta A, Chauhan P, Meena D, Hazarika N. 2018. Linear
verrucous hemangioma - a rare case and dermoscopic
clues to diagnosis. Dermatol Pract Concept. 8(1): 43-
7.
Dimaguila GAC, Samson ES. 2017. Oral Propranolol
Therapy for Benign Capillary Hemangiomas in a
Series of Adult and Pediatric Patients. Philipp J
Otolaryngol Head Neck Surg. 32 (2): 34-7.
Fatani M, Al Otaibi H, Mohammed M, Hegazy O. 2016.
Verrucous Hemangioma Treated with Electrocautery.
Case Rep Dermatol. 8: 112–7.
J Bindhuja, S Rajendiran, N Priyathersini, Singh K B,
Josepha LD. 2013. Verrucous Hemangioma: A Rare
Vascular Tumor- A Case Report. Sri Ramachandra
Journal of Medicine. 6(2): 19-20.
Laun K, Laun J, Smith D. 2019. Verrucous
Hemangioma. Eplasty. 19: ic1
Moss C, Shahidullah H. Naevi and other Developmental
Defects. 2010. In: Burns T, Breathnach S, Cox N,
Griffiths C, editors. Rook’s Textbook of Dermatology.
Eight edition. West Sussex: Blackwell Publishing Ltd.
18.74.
Nargis T, Pinto M, Bhat S, Shenoy M. 2017. Linear
verrucous hemangioma of the upper limb: a rare case.
Dermatology Online Journal. 23(6): 1-5.
Naveen KN, Pai VV, Athanikar SB, Athanikar VS, Rai V.
2015. Bluish red verrucous lesions on the leg. Cutis.
95(3): E12-4.
Nupur P, Savant SS, Kumar P, Hassan S. 2014. Linear
verrucous hemangioma. Indian Dermatol Online J.
5(Suppl 2): S136-7.
Oppermann K, Boff AL, Bonamigo RR. 2018. Verrucous
hemangioma and histopathological differential
diagnosis with angiokeratoma circumscriptum
neviforme. An Bras Dermatol. 93(5): 712-5.
Prabhakar V, Kaliyadan F. 2015. A case of verrucous
hemangioma and its dermoscopic features. Indian
Dermatol Online J. 6(Suppl 1): S56-8.
Sandhu I, Singh H. 2016. A case report of a patient with
linear verrucous hemangioma. Saudi J Med Med Sci.
4: 118-20.
Singh J, Sharma P, Tandon S, Sinha S. 2017. Multiple
verrucous hemangiomas: A case report with new
therapeutic insight. Indian Dermatol Online J. 8: 254-
6.
Vijayan P, Ponniah A, Ilias LM. 2016. Verrucous
Hemangioma: A Clinical Mimic of Verrucous
Carcinoma. J Turk Acad Dermatol. 10 (3): 16103c7.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
398
