
Urticaria Pigmentosa in Children: A Case Report
Syafria Zidni
1*
, Elin Herlina
1
, Retno Indar Widayati
1
, Diah Adriani Malik
1
,
Meira Dewi Kusuma Astuti
2
1
Department of Dermatology and Venereology, Diponegoro University/Dr. Kariadi Hospital
2
Departement of Pathology and Anatomical, Diponegoro University/Dr. Kariadi Hospital
*Corresponding author
Keywords: Urticaria pigmentosa, mast cell, ketotifen.
Abstract: Mastocytosis is a disorder of abnormal mast cell proliferation presented as an abnormal accumulation of
mast cells in various tissues. Urticaria pigmentosa (UP) is the most common form of this disorder in
children, particularly in the first year of life. Darier’s sign is pathognomonic for UP. Management for UP
consists of patient education, triggering factors exposure prevention and symptomatic treatment to reduce
the release of mast cells mediator.A5-year-old girl presented with brown spots and itch in various area of
the body with dry skin. Physical examination found multiple hyperpigmented macules on her body, arms,
legs and face. Darier’s sign was positive. Histopathology examination demonstrated mast cell granules in
the superficial layer of dermis with Giemsa staining, consistent with the diagnosis of UP. There is no
systemic involvement. Patient was treated with ketotifen syrup, 10% urea cream, and betamethasone
valerate 0,1% cream for the erythema lesions.Ketotifen is a mast cell stabilizer that was given to relieve the
symptoms of UP. Urea was given to reduce dry skin and enhance the absorption of betamethasone.
Betamethasone was given to reduce the lesions of UP. After 12 weeks, patient showed some improvement
in her pruritus and skin dryness. The prognosis was quo ad vitam, quo ad sanam and quo ad cosmeticam
dubia ad bonam.
1 INTRODUCTION
Mastocytosis is a disorder of abnormal mast cell
proliferation presented as an abnormal accumulation
of mast cells in various tissues, include the skin
and/or bone marrow. There are two types of this
disease, cutaneous mastocytosis and systemic
mastocytosis (Wagner et al, 2017; Tharp, 2012).
Urticaria pigmentosa is the most common form of
cutaneous mastocytosis in children with onset in the
first year of life, generally below two years of age
(Tharp, 2012; Vasani et al, 2015).
Mastocytosis is rare. The incidence of 2 cases
per 300.000 people per year is estimated and may be
observed in all ethnic group. The disease is higher
predominant in children and in adults between the
third and fourth decade of life. Children are more
affected before the age of six months in 50% of the
cases. There is no gender predilection (Wagner et al,
2017; Pires et al, 2018).
In patients with urticaria pigmentosa, there is an
abnormality in stem cell factor (SCF) metabolism
that affects in cell mast proliferation and
differentiation. SCF which is bound with membrane
was released, causing an increase of dissolved SCF,
and when accumulated it will stimulates melanocyte
to produces melanin (Tharp, 2012; James et al,
2011). In the other side, mast cells contain histamine
to be released which can cause redness on the skin,
swollen, and itchy (Tharp, 2012).
Urticaria pigmentosa lesions appear as multiple,
fixed, reddish-brown, hyperpigmented macules,
papules, and nodules that have a tendency to
coalesce into plaques and often exhibit increased
skin markings (Prose et al, 2008). In children, these
lesions may be present at birth or arise during
infancy. They frequently appear on the trunk and
often spare the central face, scalp, palms, and sole.
Rubbing or trauma of the affected skin results in a
weal with flare (Darier sign) in more than 90% of
patients. The diagnosis may be confirmed by skin
biopsy and histopathology examination that shows
mast cell infiltratesindicated with metachromatic
granules in cytoplasm using special stains, such as
366
Zidni, S., Herlina, E., Widayati, R., Malik, D. and Astuti, M.
Urticaria Pigmentosa in Children: A Case Report.
DOI: 10.5220/0009989103660370
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 366-370
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

Toluidine or Giemsa (Tharp, 2012; Vasani et al,
2015; Gysel et al, 2011; Rapini, 2012).
The management of patients with urticaria
pigmentosa consists of patient education, triggering
factors exposure prevention and symptomatic
treatment to reduce the release of mast cells
mediator (Tharp, 2012; Gysel et al, 2011; Grattan et
al, 2010).
Pediatric-onset urticaria pigmentosa has a
favorable prognosis because the lesions usually
disappear within a few years, usually before puberty,
although in a few cases the lesions may persist into
adult life (Tharp, 2012; Vasani et al, 2015; Prose et
al, 2008).
This case report was made with the aim of better
understanding about diagnosis and management of
urticaria pigmentosa in children which is relatively
rare.
2 CASE
A girl who was taken to the Dr Kariadi General
Hospital Medical Center by her parents presented
with brown patches on some parts of her body.
Based on her parent’s recollection, the spots first
manifested when the patient was 4 months old. The
lesion started as red patches on the patient’s back,
which sometimes was accompanied by itching
especially when she was sweating, causing her to
habitually scratches her body. Eventually the patches
expanded to her face, neck, arms, trunk, and legs.
The color of the patches gradually became darker
and brown, accompanied by dry skin. There was no
family history a similar disease.
Physical examination showed that the
patient was in an excellent health condition, has
normal general health status, with a weight of 17 kg.
The dermatologic examination found erythematous
and hyperpigmented macular eruption, with fine
scales on the face, neck, trunk, arms and legs.
Positive Darier’s sign.
Figure 1: A,B,C. Generalized hyperpigmented macules before treatment. 2A,B,C. After 12 weeks treatment.
Urticaria Pigmentosa in Children: A Case Report
367
Laboratory tests found no abnormalities.
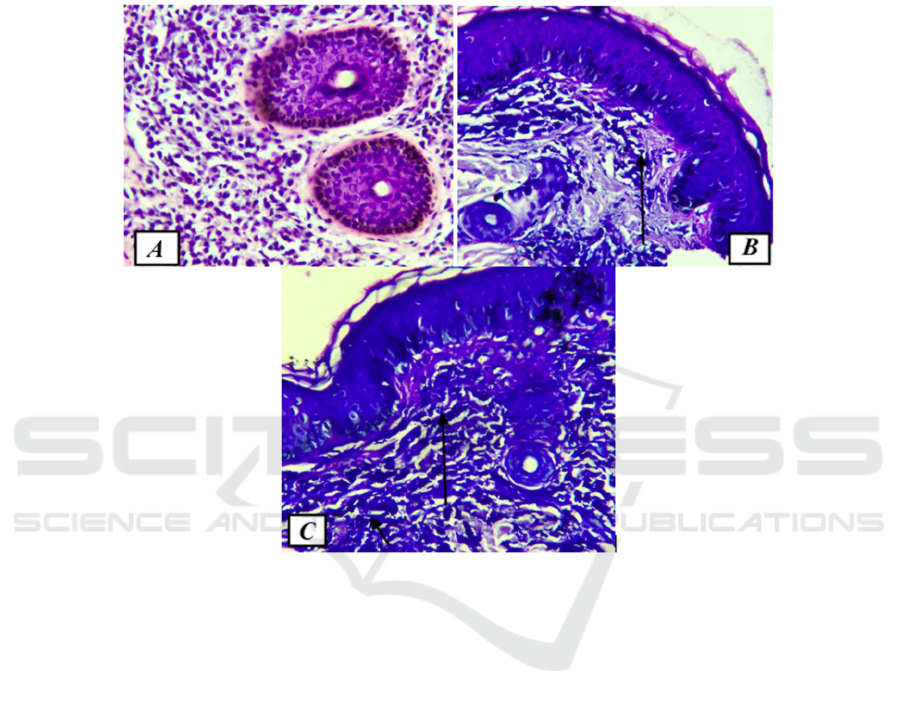
Histopathological examination by the use of special
Giemsa stain has found granulated mast cells in the
superficial dermal layer, consistent with the
diagnosis of mastocytosis. There were no systemic
abnormalities.
The patient was treated with Ketotifen syrup 1
mg bid, Urea 10% cream and Betamethasone cream.
The parents were also educated to avoid some
known triggering factors. Itching and dry skin has
showed some improvements after 12 weeks of
treatment. The patient was expected to have
spontaneous resolution at puberty.
Figure 2. A. Lymphocyte infiltration, histiocyte, and mast cell around skin adnexa. B &C.Mast cell granule (Giemsa, 400x)
3 DISCUSSION
UP was diagnosed based on the medical history,
clinical examination and histopathological
examination.
Based on the medical history, a 5-year-old girl
was taken to the Dr Kariadi General Hospital
Medical Center by her parents with brown patches
on some parts of her body. The spots first
manifested when the patient was 4 months old. The
lesion started as red patches on the patient’s back,
which sometimes was accompanied by itching
especially when she was sweating, causing her to
habitually scratches her body. Eventually the patches
expanded to her face, neck, arms, trunk, and legs.
The color of the patches gradually became darker
and brown, accompanied by dry skin. There was no
family history a similar disease. The literature
specified that UP is the most common variant of
pediatric mastocytosis, with onset in the first year of
life. The lesion usually manifested before the second
year of life, and the disease is usually confined to the
skin. There were no difference in prevalence
between male and female, all race can be affected.
(Tharp, 2012; Vasani et al, 2015; Pires et al, 2018)
The physical examination found erythematous
macular lesion, hyperpigmented macular lesion, and
fine scales on the face, neck, trunk, arms and legs.
Positive Darier’s sign. The literature mentioned that
UP usually manifested as reddish-brown patches,
papules, nodules, or plaques, with positive Darier’s
sign, where rubbing or scratching may cause the
formation of urticarial lesions surrounded with areas
of erythema. The lesion is usually distributed on the
trunk, but it may manifested on other body parts, or
even widespread (generalized). The lesion is usually
accompanied by itching, but there are no signs and
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
368

symptoms of systemic mastocytosis, such as
gastrointestinal problems, lymphedema, or skeletal
abnormalities. Pediatric consult found no systemic
involvements. This result corresponded with the
literature that specified that pediatric UP is mostly
confined to the skin, and rarely shows systemic
involvements. (Tharp, 2012; James et al, 2011).
Blood laboratory examination found no
abnormalities. Histopathological examination by the
use of special Giemsa stain has found purplish
stained granulated mast cells in the superficial
dermal layer. The literature mentioned that UP can
be diagnosed based on the result of skin biopsy and
histopathological examination by the use of special
stain to clearly examine the mast cells, such as
Giemsa or Toluidine Blue stain. . (Tharp, 2012;
Vasani et al, 2015;Gysel et al,2011;Rapini,2012).
Differential diagnosis of juvenile
xanthogranuloma can be excluded because the
lesions are mostly soft, well-defined papules or
nodules. The lesions are red-orange or red-brown in
color, and then it may change into yellowish color.
The lesion are mostly found at the upper body, and
in children, the lesion will spread quickly and then
spontaneously regress in approximately a
year.(Gelmetti,2012;Burgdof et al,2010)
Differential diagnosis of Spitz nevus can be
excluded because the lesions are mostly red to dark
brown, flat, smooth, hairless, hard, well-defined
papules or nodules, with the distribution in the head
and neck region.(Grichnik at al,2012;James et
al,2011)
The current case was treated with Ketotifen
syrup 1 mg bid, Urea 10% cream and
Betamethasonevalerate 0,1% cream. The parents
were also educated to avoid some known triggering
factors, such as temperature change, physical
activity, food, and nonsteroidal anti-inflammatory
drugs, and to avoid scratching or trauma to the skin.
The literature mentioned that the treatments are
usually symptomatic. Ketotifen is a mast-cell
stabilizer that has been shown to be effective in
reducing urtica and pruritus in patients with UP.Urea
10% cream helps to moisturize the skin and prevent
dryness, and to improve the absorption of
Betamethasonevalerate 0,1% cream. Very potent
topical corticosteroid applied with occlusion for 8-
12 weeks may reduce the number lesions in UP.The
current case was treated with betamethasonevalerate
0,1% cream, a medium potency topical
corticosteroid, that was applied to the erythematous
lesions onlyto alleviate the skin lesions.After 12
weeks of treatment, there were no new lesions,
itching was reduced, and there was no skin dryness.
(Wagner et al, 2017; Tharp, 2012). The prognosis of
the current patient was, quo ad vitam and quo ad
sanam dubia ad bonam because there were no
systemic involvement and the patient was expected
to have spontaneous resolution before puberty, quo
ad cosmeticamdubia ad bonam because of the
remaining hyperpigmented macules. (Wagner et al,
2017; Tharp, 2012;Prose et al,2008).
4 CONCLUSION
A case of UrticariaPigmentosa treated with
ketotifen, urea, and betamethasone has been reported
that can reduce the complaint and lesions.
REFERENCES
Burgdorf WH, Zelger B. 2010. The Histiocytoses. In:
Elder DE,Elenitsas R, Johnson BL, Murphy GE, Xu
X, editor. Lever’s histopathology of the skin,10
th
ed.
Philadephia:Lippincot Williams and Wilkins. p.1520-
65.
Gelmetti C. 2012. Non-Langerhans Cell
Histiocytosis.Goldsmith LA, Katz SI, Gilchrest BA,
Paller AS, Leffel DJ, Wolff K, editors. Fitzpatrick’s
Dermatology in General Medicine, 8
th
ed. New York:
McGraw-Hill. p.1795-1808.
Grattan CE, Black AK. 2010. Urticaria and mastocytosis.
In: Burns T, Breathnach S, Cox N, Griffiths C, editors.
Rook’s Textbook of Dermatology, 8
th
ed. United
Kingdom: Wiley-Blackwell. p.22.30-22.36.
Grichnik JM, Rhodes AR, Sober AJ. 2012. Benign
neoplasias and hyperplasias of melanocytes.In:
Goldsmith LA, Katz SI, Gilchrest BA, Paller AS,
Leffel DJ, Wolff K, editors. Fitzpatrick’s Dermatology
in General Medicine, 8
th
ed. New York: McGraw-Hill.
p. 1377-410.
Gysel DV, Schaik RH, Oranje AP. 2011. Mastocytosis. In:
Irvine AD, Hoeger PH, Yan AC, editors.Harper’s
Textbook of Pediatric Dermatology, 3
rd
ed.United
Kingdom:Wiley-Blackwell. p.832-46.
James WD, Berger TG, Elston DM. 2011. Mastocytosis.
In: James WD, Berger TG, Elston DM.
Andrews’Diseases of The Skin Clinical Dermatology,
11
th
ed. China: Saunders Elsevier. p.605-9.
James WD, Berger TG, Elston DM. 2011. Melanocytic
nevi and neoplasms. In: James WD, Berger TG, Elston
DM. Andrews’ Diseases of The Skin Clinical
Dermatology, 11
th
ed. China: Saunders Elsevier.
p.675-9
Pires CG, Filho JFS, Azzouz MA. 2018. Cutaneous
mastocytoma in childhood: case report. Journal of
Dermatology and Cosmetology. 2(1):9-10.
Prose NS, Antaya RJ. 2008. Neoplastic and infiltrative
diseases. In: Eichenfield LF, Frieden IJ, Esterly NB,
Urticaria Pigmentosa in Children: A Case Report
369

editors. Neonatal Dermatology, 2
nd
ed. Philadelphia:
Saunders Elsevier. p. 467-8.
Rapini RP. 2012. Practical dermatophatology, 2
nd
ed.
China: Saunders Elsevier. .p.347-9.
Tharp MD. 2012. Mastocytosis. In: Goldsmith LA, Katz
SI, Gilchrest BA, Paller AS, Leffel DJ, Wolff K,
editors. Fitzpatrick’s Dermatology in General
Medicine, 8
th
ed. New York: McGraw-Hill. p. 1809-18.
Vasani RJ, Medhekar SV. 2015. Urticariapigmentosa.
Indian Dermatology Online Journal. 6(6):464-5.
Wagner N, Staubach P. 2017. Mastocytosis –
pathogenesis, clinical manifestation and treatment
.Journal of the German Society of Dermatology. 42-
57.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
370
