
Giant Verruca Vulgaris on Scalp: A Case Report
Prilly Pricilya Theodorus
1*
, Novriyani Masuku
2
, Hanny Tanasal
2
1
RSUD Dr. M. Haulussy – Ambon, Indonesia
2
Departemen Dermatovenereologi RSUD Dr. M. Haulussy – Ambon, Indonesia
*Corresponding author
Keywords: Verruca vulgaris, histopathology, electrocauterization.
Abstract: Verruca Vulgaris (VV) or also called Common warts is a skin conditions that forms verrucose papules as a
result of skin and mucosa proliferations that caused by Human Papilloma Virus (HPV). Authors reported a
case of Giant Verruca Vulgaris on scalp in 18 years old male teenager, the lesion located in the left parietal
that continuously increasing in size within two weeks. Lesion has a cauliflower-like appearance with
nummular shape as big as 4x4x0,5cm and grayish-brown colored with verrucous surface on it.
Histopathology findings’ showed that the tissue perform a papillomatosis growth, epidermal hyperplasia,
acanthosis, hyperkeratosis and parakeratosis, hypergranulosis with rough clod of keratohyaline, it also
showed the upper epidermis has small core of coil cell, and hyperchromatic that surrounded by empty
cytoplasm. The diagnose of VV were based on the clinical and histopathology findings. The selected
treatment was electrocauterization (scar tissue presence after healing process).
1 INTRODUCTION
Warts are benign neoplasms caused by infection of
epidermal cells with papillomaviruses (Miller et al,
2013). The thickening of the dermal cells with
scaling and an upward extension of the dermal
papillae containing prominent capillaries give them
their warty of verrucous appearance (Miller et al,
2013; Androphy et al, 2012; Akram et al, 2015).
Verruca Vulgaris or usually called Common warts is
skin condition that usually comes with verrucous
papules as a consequence of skin and mucosal
proliferation that caused by Human Papilloma virus
(HPV) (Cipto, 2015; Patrick et al, 2018). The main
cause for VV is HPV type 2, followed by type 1 or 4
(Cipto, 2015). Incubations period vary from weeks
to years, and 60% of the cases has spontaneous
remission within 2 years without leaving scar tissue,
if so, it is probably because of the treatment’s
method (Stockfleth, 2009). VV can be found in all
ages, especially in children, adolescents, and young
adults (Patrick et al, 2018; Beber et al, 2018).
HPV’s transmission can occur from direct
contact (skin-to-skin) by microabrasion in the
superficial skin or through infected objects (e.g nail
clipper) and environmental surroundings (swimming
pool, because penetration is better when the skin is
in wet condition or broken) (Akram et al, 2015;
Stockfleth, 2009; Beber et al, 2018). HPV infection
mechanism can also occur through autoinoculation,
wherein virus enter the epidermis through
epithelium defect. Common predisposition factors
are trauma, finger sucking, skin rubbing, and the
presence of skin maceration (Haroen et al, 2008).
Physical examination usually presented with
solid verrucous papule, keratotic, with the size
ranging from a pin head to bigger than a centimeter,
but the average size is usually around 5mm, and the
lesion could go bigger as it goes confluent (Cipto,
2015; James et al, 2016). Variety of other shape such
as cauliflower has tendency to appear on the neck
and head, especially on scalp (warts usually bigger
in size and exophytic) and beard area (in men appear
because of shaving, as in women, they appear on
legs) (Stockfleth, 2009; Beber et al, 2018).
Predilection sites are fingers and hands (in areas that
usually exposed to trauma that produce abrasion,
e.g; elbow, knee, face, and fingers) and could be
spread elsewhere (Stockfleth, 2009; Beber et al,
2018; Sterling, 2016).
In immunocompromised
patient lesions tend to be more extensive and hard to
treat (Patrick et al, 2018; Bart, 2013).
Histopathology examination is performed to
support the diagnosis and to eliminate hesitation in
Theodorus, P., Masuku, N. and Tanasal, H.
Giant Verruca Vulgaris on Scalp: A Case Report.
DOI: 10.5220/0009988303430347
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 343-347
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
343

diagnosing a case (Miller et al, 2013; Androphy et
al, 2012; Cipto, 2015; Stockfleth, 2009).
There are
different types of treatment modalities to treat VV,
but recurrences are common with all treatment
modalities (Androphy et al, 2012).
Children with
common warts may not require treatment as
spontaneous regression is frequent (Androphy et al,
2012).
The management of warts depends on the
degree of physical and emotional discomfort, the
extent and duration of lesions, the patient’s
immunologic status, the patient’s desire for therapy,
and the risk of contagion to other persons (Androphy
et al, 2012).
In this case report, authors reported a case of
Giant Scalp Verruca Vulgaris in 18 years old male
teenager. The lesion grew in nummular shape at the
left side of parietal region that continuously
increasing in size within 2 weeks. The aim of this
case report to show that manifestation of VV can
occur in any part of the body (apart from the
predilection site) and may develop in variative size.
2 CASE REPORT
A 18 years old male teenager came to
Dermatovenereology policlinic at Dr.M. Haulussy
General Hospital in December 6
th
2018. He stated
that he had a lump at the left side of his head that
continuously grow bigger within 2 weeks. The lump
cause no itching sensation, pain, and no prior trauma
on the site of the lesion. During history taking,
patient stated that he had no contact with anyone
surround him that has the same complain as he does.
The lesion has never been treated before. Physical
examination showed a grayish-brown cauliflower-
like wart on the left side of the parietal with
nummular size as big as 4x4x0,5cm and verrucous
surface and a slight of blood on right side of the
lesion. Laboratory test showed normal result and
non-reactive to anti-viruses (HIV, HbsAg, anti-
HCV).
Histopathology finding showed that the tissue
perform a papillomatosis growth, epidermal
hyperplasia, acanthosis, hyperkeratosis and
parakeratosis, hypergranulosis with rough clod of
keratohyaline, it also showed the upper epidermis
has small core of coil cell, and hyperchromatic that
surrounded by empty cytoplasm. Papilla dermis
showed dilated capillaries that contains erythrocyte.
The dermis layer contains sebaceous glands, hair
follicle, eccrine gland, and perivascular lymphocyte
infiltration. The treatment comprise
electrocauterization with local anesthesia (scar tissue
presence after healing process), analgetic
(mefenamic acid 500mg t.i.d / p.o), wound compress
with gauze using normal saline 0,9% (1x10 minutes
before topical application), oral antibiotic
(cefadroxile 500mg b.i.d / p.o for 5 days), topical
antibiotic (fusidic acid 2 times a day/ TP), and
multivitamin (vitamin B complex and vitamin C q.d
/ p.o for 5 days).
Picture 1. First clinical picture.
(reference: private documentation of Prilly in 2018)
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
344
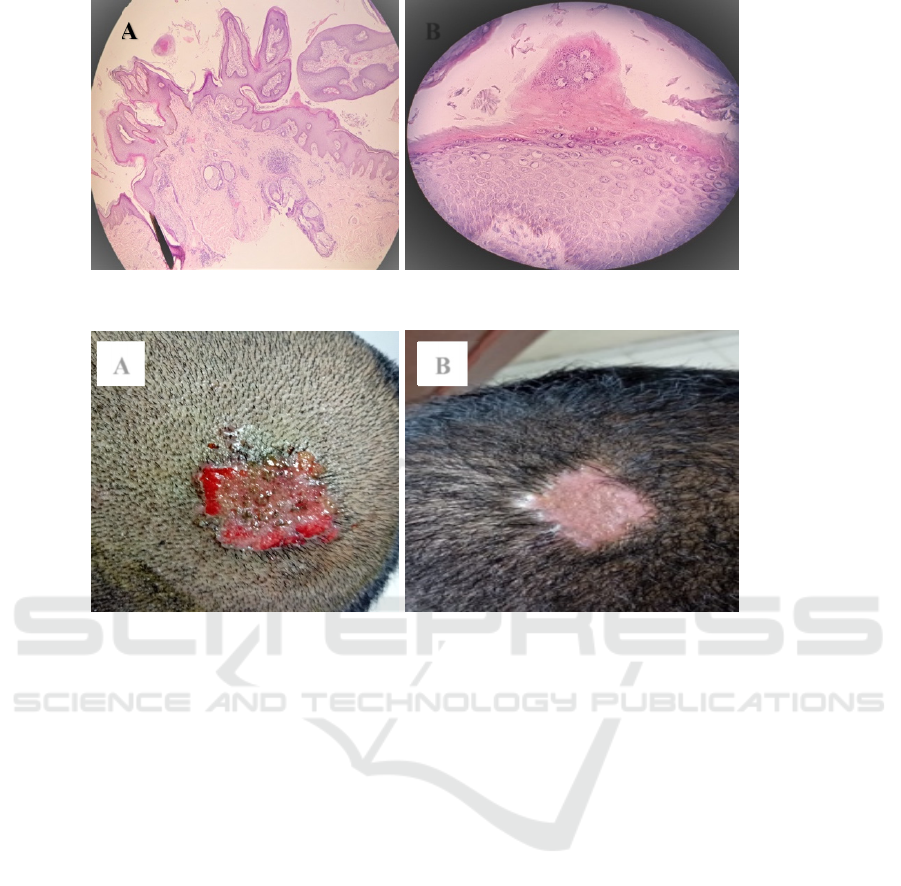
Picture 2. Biopsy result (a) zoomed 40x (b) zoomed 400x.
(reference: Doc. of Pathology Anatomy Dept of Dr. M. Haulussy General Hospital in 2018)
Picture 3. (a)Post cauterization (b)Post healing process (scar)
(reference: private documentation of Prilly in 2019)
3 DISCUSSION
The diagnosis of VV in this case were based on
history taking, physical examination, and
histopathological finding. In history taking, authors
found a 18 years old male teenager with a lump on
the back of his head that increasing in size within 2
weeks. According to literature, VV is one of the
manifestation that occur due to the presence of HPV
infection.
1
VV can also be seen in any part of the
body, happens in both male and female, and
manifests in variety of age range, but mostly occur
in children (during school age) and adolescents.
6
HPV can be transmitted through direct contact and
autoinoculation.
2,4,6
The incubation period vary from
couple of weeks to years.
6,12
In physical examination, a wart was found in the
left parietal region with nummular shape as big as
4x4x0,5cm, with verrucous surface in it that covered
in greyish-brown color and slight of blood at the
right edge of the lesion. In case such as VV, lesion
could be distinguished from normal skin because it
interrupts the normal skin lines. This reflects the
convoluted epidermal surface (papillomatosis),
hyperkeratosis, and often punctate bleeding into the
stratum corneum.(Cipto,2015)
Generally, wart’s size
vary from 1-10mm up to larger than a
centimeter.(James et al,2016;Jr JGM et al 2013)
Lesion of VV tends to be exophytic, multiple,
and irregular with rough nodules that arise in body
part that often gets trauma or rubbed and has
abrasion. Predilections site are those who often
exposed to trauma, such as hands, fingers, elbow,
knee and could spread elsewhere in the body. Warts
can also appear in other unusual predilection site
like the beard area, vermillion, and scalp could also
(as for scalp, lesion tends to be bigger and
exophytic).(Cipto,2015)
Initial diagnosis of this case was Giant Scalp
Verruca Vulgaris with Seborrheic Keratosis (SK)
and Epidermodysplasia Verruciformis (EV) as the
differential diagnosis. Similar case report for Giant
VV has been reported before in 2008 by Haroen et
all, with different site of lesion. The lesion was
located in dorsal pedis and has been going on for so
B
A B
A
Giant Verruca Vulgaris on Scalp: A Case Report
345

many years that it had developed keratinization.
(Haroen et al, 2008).
In order to confirm the diagnosis, authors run for
skin biopsy for histopathological testing and the
result matched to Verruca Vulgaris. The result
showed acanthosis (epidermal thickening),
hyperkeratosis, papillomatosis, parakeratosis, and
dilated vessels in the upper dermis (this cause blood
to enter the stratum corneum and can be clinically
visible, therefore the stratum corneum contains
parakeratotic nucleus and blood). (Akram et al,
2015;Androphy et al, 2012; Beber at al, 2018).
;Cipto,2015;Patrick et al,2018).
The differential diagnosis with SK was removed
because lesion in SK perform as papule with smooth
or verrucous surface, covered in light brown to dark
brown or similar to the skin tone (especially in
dorsum manus), and happens in the
elderly.(Sterling,2016)
As for EV, the disease
usually inherited genetically in a way that it’s either
autosomal dominant or recessive inheritance, and
can’t be found in general population like Verruca
Vulgaris. ( Beber at al, 2018)
Therapies consist personal care hygiene and
avoidance of direct contact with infected person.
4
Medical treatment has some option to perform,
including topical medication (e.g; Cantharidin, 5-
fluorouracyl, Imiquimod, Salicylic acid 25-50%,
Tricloroacetate 25%, and phenol solution),
destructive agents method (keratolytic), destructive
surgery method (e.g; cryosurgery,
electrocauterization, and CO
2
laser), and
intralesional treatment (interferone and Bleomycin).
(Androphy et al,2012; Cipto,2015Jr JGM et
al,2013;Patrick et al,2018)
.
The existence of multiple treatment modalities
reflects the fact that none is uniformly effective or
directly antiviral. (Androphy et al, 2012) Literature
stated that most treatments for verrucae involve
physical destruction of the infected cells and
immunotherapy, but recurrences are common with
all treatment modalities. (Androphy et al,2012;
Bansal,2015;Cipto,2015). In this case,
electrocauterization was considered to be more
effective to eliminate the wart and to avoid patient’s
potentially non-compliance to the long course of
topical treatment.The drawback side of
electrocauterization is that it may cause scar tissue,
pain, and can isolate the virus that it will cause
recurrence. Authors did not perform HPV DNA
identification because the limitation of modality in
authors domicile. The last day of follow up showed
the post treatment lesion has been healed with scar
tissue remaining.
4 CONCLUSION
The diagnosis of Giant Scalp Verruca Vulgaris were
made based on clinical and histopathological
findings. Selected therapy was electrocauterization
which was used to destruct the lesion, authors
considered it to be more effective than topical
application that it might decrease patient’s
compliance. Patient also were given oral antibiotic
and topical antibiotic (applied on the lesion post
electrocauterization) and also multivitamin. The last
day of follow up showed the lesion has been healed
with scar tissue remaining.
REFERENCES
Akram S, Zaman H. 2015. Warts and verrucas :
assessment and treatment. Pharm J. 7867(294): [6p.].
[Accessed on March 21
st
2019]. Available from :
https://www.pharmaceutical-
journal.com/learning/learning-article/warts-and-
verrucas-assessment-and-
treatment/20068680.article?firstPass=false.
Androphy EJ, Kirnbauer R. 2012. Human papilloma virus
infections. Dalam: Goldsmith LA, Katz SI, Gilchrest
BA, Paller AS, Leffel DJ, Wolff K. Fitzpatrick’s
dermatology in general medicine. 8
th
Ed. Vol.II. New
York: McGraw-Hill; p.2421-33.
Bansal R. 2015. Essentials in dermatology, venereology &
leprosy. 1
st
Ed. Nepal: Jaypee Brothers Medical
Publishers. p. 76-82.
Bart B. 2013. Viral infections of the skin. In: Soutor C,
Hordinsky MK. Clinical dermatology. 1
st
Ed. New
York: McGraw-Hill Education. p. 88-96.
Beber AAC, Benvegnú, Dallazem LND, Lages LN. 2018.
Viral Infections. In: Bonamigo RR, Dornelles SIT.
Dermatology in public health environments. 1
st
Ed.
Switzerland : Springer Nature; p. 174-227.
Citpo H. 2015. Veruka vulgaris dan veruka plana. In:
Menaldi SLSW. Ilmu penyakit kulit dan kelamin. 7
th
Ed. Jakarta: Badan Penerbit FKUI; p.131-2.
Haroen MS, Purba HM, Kartadjukardi E, Sularsito A.
2008. Giant verruca vulgaris: a case report. Med J
Indones. 2(18): 135-8. [Accessed on March 21
st
2019].
Diunduh dari: http://mji.ui.ac.id/journal/index.php/
mji/article/view/347
James W, Berger T, Elston D. 2016. Andrew’s disease of
the skin. 12
th
Ed. Philadelphia: Elsevier; p.399-403.
Jr JGM, Miller JJ. 2013. Lookingbill & Marks’ principles
of dermatology. 5
th
Ed. Philadelphia: Elsevier; p. 55-8.
Patrick Bacaj and David Burch. 2018. Human
papillomavirus infection of the skin. Arch Pathol Lab
Med. 6( 142): 700-705. [Accessed on March 25
th
2019
]. Diunduh dari :
https://www.archivesofpathology.org/doi/full/10.5858/
arpa.2017-0572-RA.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
346

Sterling JC. 2016. Human papilloma virus infections. In:
Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer
D. Rook’s textbook of dermatology. 9
th
Ed. Vol.I.
Oxford: Wiley. ch. 25.43-61.
Stockfleth E. 2009. Human papilloma virus infections. In:
Burgdorf WHC, Plewig G, Wolf HH, Landthaler M.
Braun-Falco’s dermatology. 3
rd
Ed. German:
Springer; p.64-73.
Giant Verruca Vulgaris on Scalp: A Case Report
347
