
Acute Cutaneous and Generalized Discoid Lupus Erythematosusin
Systemic Lupus Erythematosus with Neuropsychiatric
Complications: A Multidisciplinary Approach
Fadhli Aulia Mughni
1*
, Randy Satria Nugraha
1
, Eyleny Meisyah Fitri
1
, Tjhin Wiguna
2
,Windy
Keumala Budianti
1
1
Department of Dermatology and Venereology Faculty of Medicine Universitas Indonesia/Dr. CiptoMangunkusumo
National Central General Hospital, Indonesia
2
Department of Psychiatry Faculty of Medicine Universitas Indonesia/
Dr. CiptoMangunkusumo National Central General Hospital, Indonesia
Keywords: Acute cutaneous lupus erythematosus, discoid lupus erythematosus, multidisciplinary, neuropsychiatric
Abstract: Acute cutaneous lupus erythematosus (ACLE) is a type of cutaneous lupus erythematosus (CLE) which
presents as the characteristic malar rash and has high association with the systemic lupus erythematosus
(SLE). Discoid lupus erythematosus (DLE) is a type of chronic CLE (CCLE) typically present as discoid
atrophic scars with central hypopigmentation and is usually localized to skin lesions. SLE can present with a
wide spectrum of complications affecting multiple organs, including neuropsychiatric involvement. We
report a case of a 15-year-oldfemalepresented with the characteristic malar rash which is aggravated by sun
exposure, multiple atrophic scars on the scalp and legs, and scaring alopecia. Clinical history and complete
physical examination confirmed the diagnosis of ACLE and generalized DLE. She has been treated
routinely for SLE since two years ago with oral methylprednisolone and mycophenolate mofetil. She also
experienced psychiatric disorders, mainly depression and anxiety, and was consulted to the psychiatry clinic
for neuropsychiatric complications.We focus to describe our management plan in compiling detailed
regimen of topical sunscreen and corticosteroid usage which is tailored to the patient’s routine activity and
limitations. We also provided continuous support and established collaborative management plan with other
associated departments for evaluation of other complications. This personalized and multidisciplinary
approach proves to increaseher compliance andresulted in significant improvement of the disease and her
quality of life.
1 INTRODUCTION
Lupus erythematosus (LE) is a term used to describe
varieties of autoimmune disorders characterized by
autoimmunity towards the nucleosome and
ribonucleoprotein components. This disease ranges
from the mildest form, with only localized cutaneous
lesions, to the severe form with multiple organs
involvement and high mortality rate. Based on
clinical and histopathology,CLE-specific skin
diseaseis divided intoACLE, subacute CLE (SCLE),
and CCLE. (Costner et al., 2012)
Acute CLE is observed in 20 to 60% of LE
patients, found more often in females, and it is the
CLE most associated with SLE. (Costner et al.,
2012). Clinically ACLE is categorized into the
localized form, with erythema and edema on malar
region, and the generalized form, as large
morbilliform or exanthematous eruption focused on
the extensor aspects of arms and hands. Patients with
SCLE shows characteristic form of erythematous
macules, papules, or plaques arranged annularly or
polycyclic on sun-exposed body areas, with 50%
systemic involvement.CCLE usually manifests only
as skin lesions, most commonly DLE. (Costner et
al., 2012;Oke V et al., 2013)
It is important to evaluate the possibility of
systemic disease association in diagnosing CLE,
including neuropsychiatric manifestation. Diagnosis
can be established clinically, while laboratory and
histopathology examination may help to confirm
diagnosis and differentiate CLE types/ The
management of CLE generally include protection
320
Mughni, F., Nugraha, R., Fitri, E., Wiguna, T. and Budianti, W.
Acute Cutaneous and Generalized Discoid Lupus Erythematosusin Systemic Lupus Erythematosus with Neuropsychiatric Complications: A Multidisciplinary Approach.
DOI: 10.5220/0009987803200324
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 320-324
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

from ultraviolet (UV) radiation, avoidance of
photosensitizing agents, and topical therapy.
1
Administration of systemic immunosuppressive
agent is usually reserved for CLE in generalized
form or who have failed to benefit adequately.
(Costner et al., 2012;Hejazi et al., 2016)
Promptdiagnosis and thorough evaluation of
multiple organs involvement in ACLE and other
types of CLE greatly impact the patient’s prognosis
and quality of life. Neuropsychiatric complications
in LE patients are not commonly found and are still
poorly understood. It requires holistic management
and collaboration with other specialties according to
the systems involved. We report a case of ACLE and
generalized DLE in SLE with neuropsychiatric
complications. This case report emphasizes the need
to assess systemic complications and the importance
of multidisciplinary approach in CLE treatment.
2 CASE
A 15-year-old female was referred to the
Dermatology and Venereology clinic, Dr.
CiptoMangunkusumo National Central General
Hospital with the symptom of erythematous rash on
both cheeks. One month ago, slightly painful
erythematous patches appeared on patient’s cheeks
which are exacerbated by heat and sun exposure,
with no pruritus. Approximately in two weeks, the
lesions expanded and spread to the neck and chest
areas, with multiple small erosions observed on both
cheeks. There was no symptom of oral ulcer.
The patient has a history of SLE compatible
with SLICC (Systemic Lupus International
Collaborating Clinics) criteria since 2016. (Yu C et
al, 2014). She routinely visits the Allergy-
Immunology clinic of the Pediatric department since
diagnosed and was being treated with
methylprednisolone once daily (8 mg) and
mycophenolate mofetil twice daily (540 mg in the
morning and 360 mg in the evening) until present.
She was also given hydroxychloroquine once daily
(200 mg) but was stopped only two weeks after
retinopathy developed. Warfarin was prescribed due
to her antiphospholipid syndrome. She experienced
multiple episodes of ACLE and DLE lesions since
two years ago, and was treated with topical
corticosteroid and sunscreen. The lesions sometimes
were reduced, howeverone year later the lesions
started to spread further accompanied by progressive
hair loss on certain areas of the scalp.
Since May 2017, she started to experience
psychiatric disorders, mainly depression and anxiety,
and was consulted to the Psychiatry clinic. She was
diagnosed with neuropsychiatric systemic lupus
erythematosus (NPSLE) and was treated with
sertraline once daily (25 mg) and aripiprazole once
daily (7.5 mg), however she did not visit the clinic
routinely and did not take the medications as
instructed. She is currently on the 10
th
grade and
lives with her parents. From our interview with her
and her father, we found that since diagnosed with
SLE, she became less talkative and often seclude
herself from her peers. She often felt less confident
and has trouble concentrating while studying at
school. She described that she did not apply
sunscreen routinely because she was not convinced
that it helps.
Physical examination revealed the
characteristic malar or butterfly rash on her face, as
well as multiple discoid atrophic scars on both
supraorbital areas and multiple small erosions with
telangiectasia (Figure 1). Moon face appearance was
observed. There are also multiple erythematous
nummular patches on neck and chest, multiple
atrophic scars on the lower legs and scalp, with
alopecia and hair thinning on the surrounding areas
(Figure 2). Assessment of lesions using the Revised
Cutaneous Lupus Erythematosus Disease Area and
Severity Index (RCLASI) showed total activity
score and total damage score of 13 and 11,
respectively. Laboratory test showed increased anti
ds-DNA (268.6 IU/mL), increased ACA IgM (34
MPL), and decreased C3 and C4 levels (37.2 and
7.66 mg/dL, respectively).No histopathological or
direct immunofluorescence examination were
performed.
Figure 1.Classic ACLE and DLE lesions.Typical early
erythematous plaque demonstrating hyperkeratosis and
accentuation of follicle orifices and multiple sharply
demarcated, round-to-ovoid slightly indurated
erythematous plaque on both cheeks and eyebrows.
Acute Cutaneous and Generalized Discoid Lupus Erythematosusin Systemic Lupus Erythematosus with Neuropsychiatric Complications: A
Multidisciplinary Approach
321
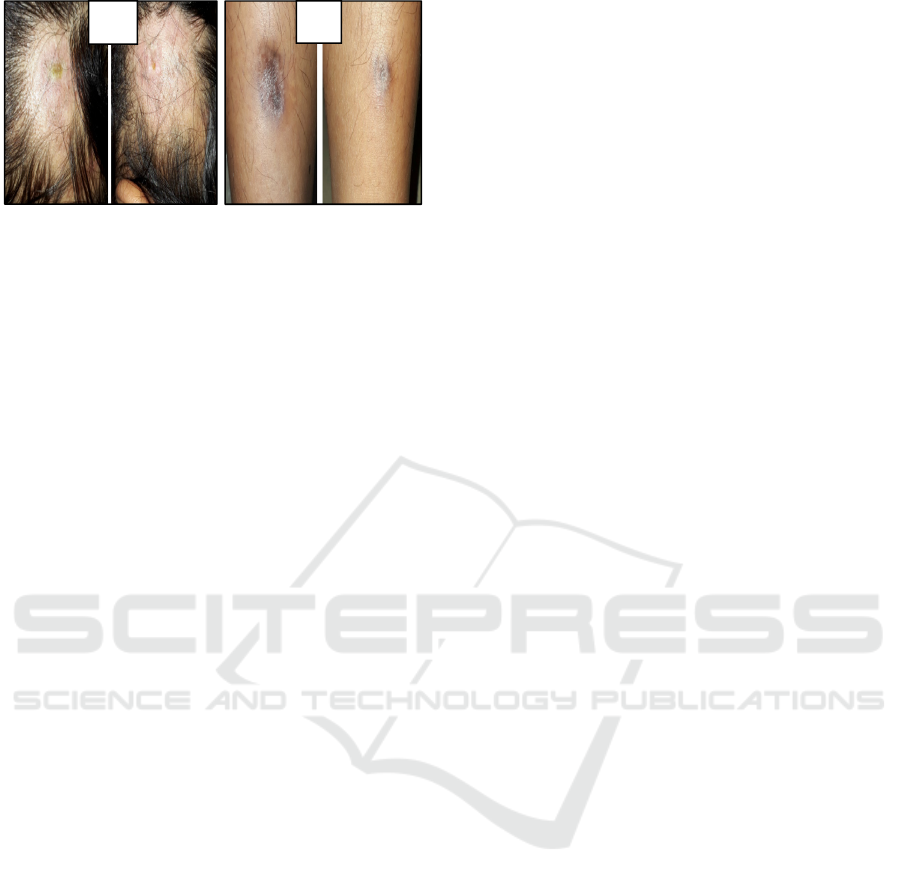
Figure 2.(A) Multiple atrophic scars and alopecia on the
occipital areas of the scalp; (B) Multiple atrophic scars on
the anterior lower legs.
She was diagnosed with ACLE and generalized
DLE in SLE with neuropsychiatric complications.
She was treated with a strict regimen of sunscreen
application (every two to three hours on sun-exposed
areas) on sun-exposed areas, which was adjusted to
her school schedule of indoor and outdoor activities
to prevent overuse and increase compliance. Topical
corticosteroid was also added while the systemic
therapy was supervised by the Pediatry clinic. We
also advised the patient and her father about the
importance and potential benefits of routine visit to
the Psychiatry clinic. After six weeks of treatment,
the erythematous plaques on cheeks subsided, while
the DLE lesions and alopecia remain the same.
Several new erosions and excoriations emerged.
Previous wounds expanded, some covered with dark
crusts and produced yellowish pus. Gram stain
examination was performed and showed bacterial
infection. After managing the infection with wet
dressing and systemic antibiotic the skin lesions
showed marked improvement, confirmed by the
decrease of RCLASI total activity score from 13 to
9. Routine visit to the Psychiatry clinic greatly
improved the patient’s compliance and quality of
life. This shows the importance of recognizing
systemic complications and multidisciplinary
management in CLE patients.
3 DISCUSSION
The patient showed characteristic clinical
appearance of localized ACLE. However, other
possible differential diagnosis that have similar
features should be excluded, such as acne rosacea,
dermatomyositis, polymorphous light eruption
(PMLE), or photoallergic contact dermatitis.
1
In
rosacea we usually find characteristic erythematous
papules or pustules, while cutaneous lesions such as
Gottron papules, pruritus and erythematous patches
distributed on the extensor aspects and muscle
weakness are commonly found in dermatomyositis,
thus both are excluded. (Costner et al., 2012; Okon
et al., 2013). She was not diagnosed as PMLE
because there were no pinkish or erythematous
papules, and other sun-exposed area besides the
face, neck, and chest were not involved.(Lehmann et
al., 2011). Photoallergic contact dermatitis could be
considered, due to the history of regular topical
sunscreen usage since 2016 which contains photo-
allergenic substances, especially butylmethoxy-
dibenzoylmethane, octylmethoxycinnamate, and
methylbenzylidene camphor. (Goncalo et al., 2013)
However, her lesions were transient and only
appeared on certain areas, which makes this
diagnosis unlikely.
Physical examination also revealed multiple
discoid atrophic scars with peripheral
hyperpigmentation and central hypopigmentation on
scalp and lower legs, which are characteristic of
classic DLE lesions. DLE lesions on hairy areas
usually show follicular keratotic plug and may cause
scarring alopecia, also found in this patients.
(Cortner et al., 2012). She experienced alopecia
from one year ago and did not show any
improvement until recently, which support the
assessment that it is scarring alopecia caused by
DLE. (wang et al., 2011). This can highly impact the
patient’s quality of life, especially in female
teenager, highlighting the importance of specialized
evaluation and treatment in this case.
Evaluation of CLE lesions can be very
difficult, due to the chronic nature of the disease and
low response towards therapy. The extent and
severity of CLE lesions in this patient were not
evaluated thoroughly, which may contribute to
herlong-lasting lesions.In 2005, there was a tool
developed to evaluate the activity and damage of the
disease in CLE patients, termed CLASI (cutaneous
lupus erythematosus disease area and severity
index).
9
However in 2010 this tool is revised and
termed Revised CLASI (RCLASI).This revised tool
allow for a more complete and thorough evaluation
of all lesions as it consider different form of CLE
lesions, such as superficial or adherent scaling, and
the type of dyspigmentation. It also assesses the
presence of mucous membrane lesions and alopecia
(Kuhn et al., 2010).
Since May 2017, she was diagnosed with
neuropsychiatric SLE, which is a form of
neurological involvement in SLE. Clinical
manifestations of NPSLE could appear as
neurological symptoms, such as epileptic seizure,
headache and cerebrovascular disease, or cognitive
and psychiatric disorders. (Souirti et al., 2013).The
A
B
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
322

prevalence of depression in SLE patients was found
to be six times higher than healthy subjects, which
was correlated with serum IL-10 concentrations,
relationship assessment, and fatigue
severity.(Figueiredo-Braga et al., 2018)
Psychiatric
disorder could also be triggered by corticosteroid
usage in 10% of patients that manifest as mood
disorder in 93% of those patients.(Bertsias et al.,
2010). In this patient, NPSLE manifested more
clearly as psychiatric disorder, which are mood
disorder, depression, and anxiety, prompting her
referral to the Psychiatry clinic. She was treated with
antidepressant (sertraline) and antipsychotic
(aripiprazole), complemented by supportive
psychotherapy for depressive symptom. This is
consistent with the European League Against
Rheumatism (EULAR) recommendation for the
management of SLE with neuropsychiatric
manifestations in 2014. .(Bertsias et al., 2010).
Treatment of CLE is still a major challenge
because there is still no specific therapy approved
for CLE. The purposes of CLE management are
educating the patient about the disease and
prevention by avoiding trigger factors.(Hejazi et al.,
2016) These can be achieved by minimizing
ultraviolet (UV) exposure, physical protection, and
application of water-resistant broad-spectrum
sunscreen that contain sun protection factor (SPF) ≥
30 dan UVA-blocking agents.
1
This patient has
already used SPF≥ 30 sunscreen since 2016 and was
also given vitamin D3(cholecalciferol)
supplementation 1 tablet per day. However, she
admitted that she only applied the sunscreen two to
three times per day. This frequency could not
provide adequate photoprotective effect, considering
the sunburn dosage percentage after 30 minutes of
sun exposure, and the sunscreen actual usage
concentration of 0.5–0.8 mg/cm
2
, to achieve
adequate photoprotection the sunscreen must be
reapplied every 1.25–2 hours for SPF 30, and every
2.5–4 hours for SPF 45. The vitamin D3 dosage
given was also not enough, as one tablet of the
patient’s supplement only contain 133 IU of
cholecalciferol. It is recommended to give vitamin
D3 supplementation of at least 400 IU per day for all
CLE patients.(Hejazi et al., 2016)
For a more comprehensive treatment of this
patient, we need to pay attention to the risk of the
development of other diseases associated with SLE
and CLE. Cerebrovascular disorders affect 2–15%
SLE patients, most commonly acute ischemic stroke.
Moreover, this patient has a history of
antiphospholipid syndrome which increase the risk
of thrombosis, another risk factor of cardiovascular
disease. (Souirti et al., 2013). The risk of
cardiovascular disorder is apparently also higher in
CLE patients compared to the general
population.(Hesselvig et al., 2017). Considering
those conditions, thorough cardiologic evaluation
should be one of the priorities in the management
plan of this patient.
4 CONCLUSION
Management of CLE and SLE is quite challenging.
Diagnosis can be made by clinical basis, however
the assessment of affected areas and disease severity
must be performed thoroughly. The RCLASI is a
reliable tool for that purpose and should be used
anytime possible to allow efficient and accurate
treatment plan. Protection from sun exposure using
topical sunscreen is still the most important aspect of
CLE management. Clinicians should allocate
adequate time to educate the patient and caretaker
regarding the correct method of sunscreen
application, as well as other methods of sun
protection. Neuropsychiatric complication is a rare
manifestation of systemic involvement in SLE
patient,which may result from both the physical
effect of autoimmunity on the nervous system and
the suffering due to pain and disability. (Figueiredo-
Braga et al., 2018)
.
Therefore, it is crucial to be
aware of any early signs and symptoms of systemic
involvement and consult with the corresponding
department. Multidiscipline approach might result in
less severe complications, better quality of life and
higher therapy success rate in CLE and SLE
patients.
REFERENCES
Albrecht J, Taylor L, Berlin JA, et al. The CLASI
(cutaneous lupus erythematous disease area and
severity index): an outcome instrument for cutaneous
lupus erythematosus. J Invest Dermatol. 2005 Nov;
125: 889-94.
Bertsias GK, Ioannidis JPA, Aringer M, Bollen E,
Bombardieri S, Bruce IN, et al. EULAR
recommendations for the management of systemic
lupus erythematosus with neuropsychiatric
manifestations: report of a task force of the EULAR
standing committee for clinical affairs. Ann Rheum
Dis. 2010; 69: 2074-82.
Costner MI, Sontheimer RD. Lupus erythematosus. In:
Goldsmith LA, Kath SI, Gilchrest BA, Paller AS,
Leffel DJ, Wolff K, editors. Fitzpatrick’s dermatology
Acute Cutaneous and Generalized Discoid Lupus Erythematosusin Systemic Lupus Erythematosus with Neuropsychiatric Complications: A
Multidisciplinary Approach
323

in general medicine.Edisi ke-8. New York: McGraw-
Hill; 2012. p. 1909-26.
Figueiredo-Braga M, Cornaby C, Cortez A, Bernardes M,
Terroso G, Figueiredo M, et al. Depression and
anxiety in systemic lupus erythematosus. Med. 2018;
97: 28.
Goncalo M, Ferguson J, Bonevalle A, Bruynzeel DP,
Gimenez-Arnau A, Goossens A, et al. Photopatch
testing: recommendations for a europeanphotopatch
test baseline series. Contact Dermatitis.2013; 68: 239-
43.
Figueiredo-Braga M, Cornaby C, Cortez A, Bernardes M,
Terroso G, Figueiredo M, et al. Depression and
anxiety in systemic lupus erythematosus. Med. 2018;
97: 28.
Hesselvig JH, Ahlehoff O, Dreyer L, Gislason G, Kofoed
K. Cutaneous lupus erythematosus and systemic lupus
erythematosus are associated with clinically
significant cardiovascular risk: a danish nationwide
cohort study. Lupus.2017; 26: 48-53
Kuhn A, Amler S, Beissert S, et al. Revised cutaneous
lupus erythematous disease area and severity index
(RCLASI): a modified outcome instrument for
cutaneous lupus erythematosus. Br J Dermatol.2010;
163: 83-92.
Lehmann P, Schwarz T. Photodermatoses: diagnosis and
treatment. DeutschesArzteblatt International. 2011;
108(9): 135-41.
Oke V, Wahren-Herlenius M. Cutaneous lupus
erythematosus: clinical aspects and molecular
pathogenesis. J Intern Med. 2013; 273: 544-54.x
Okon LG, Werth VP. Cutaneous lupus erythematosus:
diagnosis and treatment. Best Pract Res
ClinRheumatol. 2013 Jun; 27(3): 391-404.
Souirti Z, Lahlou M, El Ouali O, Chtaou N, Aarab C, El
Ghazouani F, et al. Neuropsychiatric systemic lupus
erythematosus. Open J Rheumatol Autoimmune Dis.
2013 May; 3: 86-91.
Yu C, Gershwin ME, Chang C. Diagnostic criteria for
systemic lupus erythematosus: a critical review. J
Autoimmun.2014; 1-4.
Wang E, McElwee KJ. Etiopathogenesis of alopecia
areata: why do our patients get it?.DermatolTher.
2011; 24: 337-47.
.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
324
