
Coexistence of Two Autoimmune Diseases: A Case of Colocalized
Vitiligo and Psoriasis in One Person
Ariska Silviani
1*
, Eyleny Meisyah Fitri
1
, Sammy Yahya
2
, Yari Castiliani Hapsari
2
,
Saskia Retno Ayu Hapsari
2
1
Department of Dermatology and Venereology Faculty of Medicine Universitas Indonesia/Dr. Cipto Mangunkusumo
National Central General Hospital, Indonesia
2
Department of Dermatology and Venereology Faculty of Medicine Universitas Indonesia/ Tarakan Regional General
Hospital, Indonesia
*Corresponding author
Keywords: Coexistence, psoriasis, vitiligo
Abstract: Vitiligo and psoriasis are autoimmune diseases. The occurrence of both diseases in a single patient,
especially at the same sites, has been considered unusual. Herein, we report a case of coexisting vitiligo and
psoriasis in a patient at the same site. A 40-year-old male visited our Dermatology and Venereology clinic
with a history of white patches all over the body for 20 years and red patches with thick, scaly surfaces for
three years before admission. Physical examination revealed multiple depigmented macules, lenticular-
plaque in size, irregular, circumscribed, discrete-confluent with several erythematous plaques, nummular-
plaque in size, irregular, circumscribed, thick silvery-white scaleswith positive Auspitz sign on the top of
depigmentedmacules. He was diagnosed with vitiligo Vulgaris and Psoriasis Vulgaris and received systemic
therapy, a combination of topical therapy and phototherapy narrowband UVB. The pathogenic mechanism
underlying the coexistence of vitiligo and psoriasis has not been fully elucidated. The Koebner
phenomenon, genetic, and environmental factors have been postulated to be involved in the development of
the two diseases. Comorbid vitiligo and psoriasis is a red flag signaling the need to dig deeper, looking for
potentially associated diseases, including cardiovascular, autoimmune, or psychiatric diagnoses.
1 INTRODUCTION
Vitiligo is a skin depigmentation disease caused
by interactions of genetic and non-genetic factors
causing loss of function of melanocytes, manifesting
as a well-defined depigmented macula surrounded
by healthy skin.(James WD et al., 2011; Jacoeb et
al., 2017). There is no gender difference in vitiligo
and can occur at any age. The incidence of vitiligo is
0.51% of the total population worldwide.(Ezzedine
et al., 2015).
The case of vitiligo with a family
history ranges from 6.2538%, but the genetic
pattern is still debated (Jacoeb et al.,2017).The
etiology of vitiligo is not yet known. Some
hypotheses are related to the etiology of vitiligo,
including the genetic hypothesis, the autoimmune
hypothesis, as well as the biochemical
hypothesis.(Jacoeb et al., 2017;Birlea SA 2012)
The diagnosis of vitiligo can be made based on
history and physical examination.
2,4
Various other
skin disorders that can be found in vitiligo lesions,
including psoriasis Vulgaris, scleroderma, lupus
erythematosus, alopecia areata, Morbus duhring, and
melanoma.
2
The principle of managing vitiligo is to
induce repigmentation. Spontaneous repigmentation
has been reported in 644% of patients.
Repigmentation is a sign that the lesion is responsive
to therapy. Birlea SA 2012)
Psoriasis is a chronic inflammatory skin disease
with characteristics of changes in epidermal cell
growth and differentiation as well as the presence of
vascular manifestations with a strong genetic basis,
also thought to have a nervous system effect.
5
The
worldwide incidence and prevalence of psoriasis is
poorly understood. Psoriasis is estimated to effects
about 23% of the world population.(Springate DA
et al., 2017). The etiopathogenesis of psoriasis is still
not clearly known, but the role of autoimmunity and
genetics can be used as a principle of
therapy.(Jacoeb TJA et al., 2017)
Silviani, A., Fitri, E., Yahya, S., Hapsari, Y. and Hapsari, S.
Coexistence of Two Autoimmune Diseases: A Case of Colocalized Vitiligo and Psoriasis in One Person.
DOI: 10.5220/0009987503070311
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 307-311
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
307

Clinically, a classic description of psoriasis in the
form of a white squamous encompassing
erythematous plaques with bleeding points if the
scale is released, the lesion can be the size of a
needle tip to a plaque that covers most areas of the
body, usually symmetrical lesions. In addition to the
skin, the involvement of nails, mucosa, and joints
can be found.(Ezzedine K et al., 2015). Psoriasis
diagnosis can be made based on history and physical
examination. Psoriasis treatment aims to reduce the
severity of the disease so that patients can move in
social life, work and prosperity, and also remain in a
condition of good quality of life.
Psoriasis and vitiligo are autoimmune diseases.
Yet the pathogenesis of the association between
these two dermatoses is still unknown. It is
uncommon that the occurrence of both these
diseases in the same patient, especially at the same
sites.Coexistence psoriasis lesions on the top of
vitiligo lesions made this becomes important for
discussion because it is a red flag signaling the need
to dig deeper looking for potentially associated
diseases, including cardiovascular, autoimmune, or
psychiatric diagnoses. Herein, we report on a case of
coexisting vitiligo and psoriasis in the same
individual at the same site.
2 CASE
A 40-year-old male admitted to Dermatology and
Venereology clinic at Tarakan Regional General
Hospital due to thick scaleson red spots since three
years ago that appeared on several white spots
throughout the body since 20 years ago. Initially,
white spots appear on the face, near the lips. Spots
are round, milky white, firmly defined, with a
diameter of about one centimeter. There was no
history of itch, pain, numbness, and redness before.
About five months later, the spots began wider, and
more numerous appear on both hands, legs, thighs,
calves, buttocks, lower back, stomach, and head.
Twenty years ago, the patient went to dermato-
venereologist in Cianjur Hospital. He was diagnosed
with vitiligo and was given a concoction cream that
was applied twice a day and two types of unknown
oral drug that taken one time per day. He was treated
as an outpatient clinic at a hospital in Cianjurfor
approximately three years. However, because there
was no excellent clinical response, then he went to
dermato-venereologist at one of General Hospitals in
Sukabumi. Seventeen years ago, he went to dermato-
venereologist at Sukabumi General Hospital and was
diagnosed with vitiligo. He was treated with liquid
Delsoralen® once a dayand asked to bask for 15
minutes after applying the drug. He was also given
concoction capsules that taken three times per day.
He was treated for five years, but still, there was no
excellent improvement, so that he was referred to
Hasan Sadikin Hospital, Bandung.Twelve years ago,
the patient went to Hasan Sadikin Hospital andwas
diagnosed with vitiligo. The patient is also treated
with liquid Delsoralen® once a dayand asked to
bask after applying the drug.He was treated at Hasan
Sadikin Hospital for about one year. White patches
had not expanded, and there were no new white
spotsnorimprovement.Eleven years ago, the patient
returned to dermato-venereologist in Cianjur. He
seeks treatment in about five of different dermato-
venereologist. Various drugs given by these doctors,
the patient does not remember the details of what
drugs each doctor gave and the duration of treatment
for each doctor. The patient treated for about three
years and received various drugs such as ointment
applied twice a day, pills taken 12 times a day, and
liquid Delsoralen®. Feeling tired and hopeless
because the vitiligo hasn’t healed, the patient didn’t
continue treatment for about eight years. Finally, the
patient went to dermato-venereologist of Tarakan
General Hospital on the advice of the patient's
relatives and because the spots grew wider and
added thick scales on red spots.
Three years ago, the patient complained of reddish-
scaly patches on several white spotsat almost the
entire body. Initially, small red spots appear on the
lower back, left and right elbows and left and right
thighs. Sometimes red patches feel an itch. By the
time, the red spots are more widespread and white
scales thicker than before and also appear in other
areas of the body.
The patient has a history ofuncontrolled
hypertensionsince 1.5 years ago. He denies contact
with chemicals before spots appear. A history of
reddish spots shaped like butterflies on both cheeks
when exposed to the sun, fever, migrating joint pain,
swellingor stiffness in the joints, fatigue, thirst,
hunger, weight loss, natural sweating, palpitation,
trembling in both hands is also denied by the patient.
There is no history of steroid use or long-term drugs,
drug, and food allergies. There is no history of blood
transfusion. The patient also has no history of
anemia and diabetes mellitus.There were complaints
of white spots on other family members, namely the
patient's mother and sister. The patient is married,
lives with his wife and four children in Cianjur,
West Java. He is a teacher who works indoors every
dayand rarely exposed to the sun.
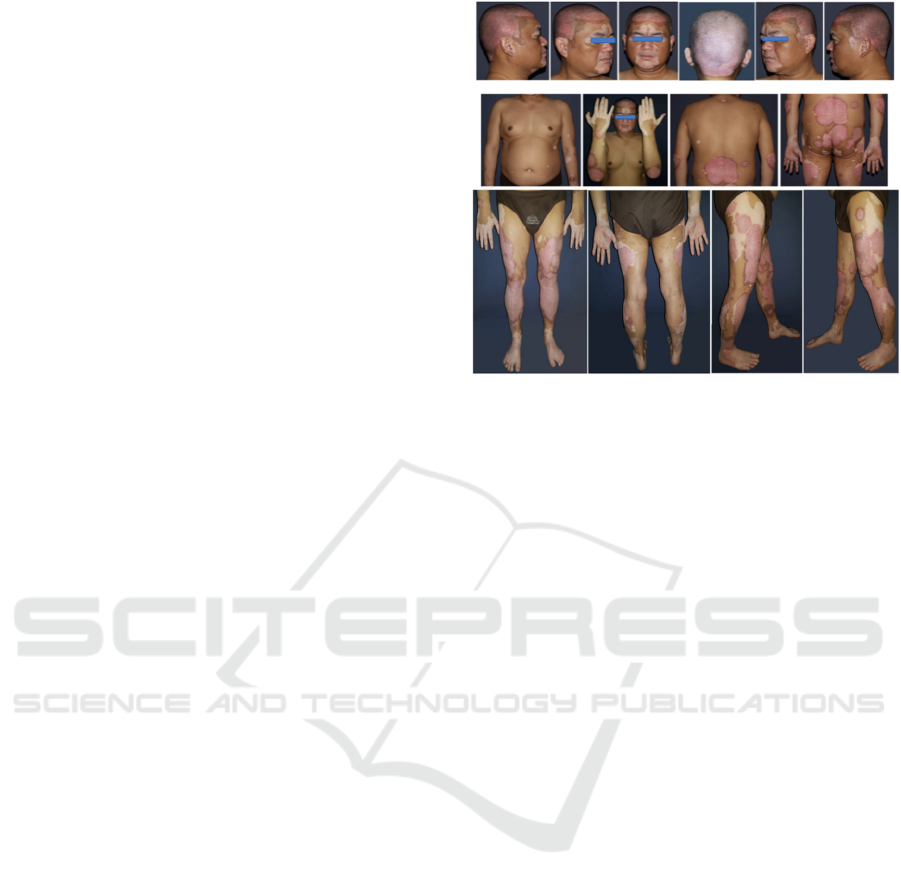
Physical examination revealed hypertension
(180/110 mmHg) and the presence of multiple
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
308
depigmented macules, lenticular-plaque in size,
irregular, circumscribed, discrete-confluent with
several erythematous plaque, nummular-plaque in
size, irregular, circumscribed, silvery-white thick
scales with positive Auspitz sign on the top of
depigmented macules on the scalp, face, bilateral
earlobe, abdomen, back and buttocks, and also
bilateral upper and lower limbs. (Figure 1) There
were also pitting nails in the entire finger of both
hands. Body Surface Area (BSA) of vitiligowas
28%while that of psoriasiswas 25% with Psoriasis
Area and Severity Index (PASI) score was
9.5.Laboratory examination including complete
blood counts, differential leukocyte counts, liver
function test, renal function test, and thyroid
function test was within normal limits,
excepthyperglycemia(324 mg/dL) and positive
antinuclear antibody with the titer of 1:320.
Based on the history and physical examination, a
clinical diagnosis of coexisting vitiligo Vulgaris and
psoriasis Vulgaris was made. He was treated with
systemic corticosteroids, a combination of topical
therapy and narrowband UVB phototherapy.
Methylprednisolone 8 mg twice a day was given as
systemic therapy for two daysper week. He applied a
combination of 3% ichthyol and 10% zinc oxide in
0.025% fluocinoloneacetonide cream twice a day on
white patches, and a combination of 3% salicylic
acid, 5% liquor carbonic detergent, and0.25%
desoximetasone ointment twice a day on
erythematous plaques. Patients also
underwentwhole-body narrowband UVB
phototherapy twice a week with an initial dose of
200 mg/cm
2
and increased by 10% per
visit.Hesubsequently consulted the internist to
control his blood pressure and to evaluate his blood
glucose.
Figure 1. Presence of multiple depigmented macules,
lenticular-plaque in size, irregular, circumscribed,
discrete-confluent with several erythematous plaques,
nummular-plaque in size, irregular, circumscribed, thick
silvery-white scales with positiveAuspitz sign on the top
of depigmented macules.
3 DISCUSSION
The coexistence of psoriasis and vitiligo is rare.
Relatively few reports of concomitant and
colocalized psoriasis and vitiligo are available. In
this case, diagnosis vitiligo Vulgaris and psoriasis
Vulgaris were established based on history and
physical examination.The location of the patient's
depigmented lesions was almost the entire body's
area which is categorized in general vitiligo or
vitiligo Vulgaris. Vitiligo Vulgaris is characterized
by lesions in the form of multiple homogeneous
milky white macules which are clearly demarcated,
scattered, and less symmetrical.(Jacoeb et al 2017).
Vitiligo Vulgaris is associated with a number of
conditions and autoimmune diseases.Genetic factors
are thought to play a role in the onset of vitiligo
lesions, the percentage ranges from 6.25%–38% and
the genetic pattern is still debated. (Ezzedine
K et
al., 2015). In this patient, genetic predisposition was
found where the older siblings of the patient's
mother suffered from vitiligo.
The clinical variants of psoriasis include
psoriasis Vulgaris, gutata psoriasis, pustular
psoriasis, nail psoriasis, arthritis psoriasis, and
erythroderma. (Jacoeb TJA et al., 2017) Psoriasis
Vulgaris is found in about 90% of psoriasis patients.
Lesions generally begin with an erythematous
macula less than one centimeter in size or in the
form of a papule that extends, and several lesions
Coexistence of Two Autoimmune Diseases: A Case of Colocalized Vitiligo and Psoriasis in One Person
309

coalesce so that the size can reach several
centimeters.Lesions are usually found in the scalp,
elbow, knee, back, lumbar, and retro auricular.
(Jacoeb TJA et al., 2017). Theclinical manifestation
and predilection sites on this patient are categorized
in psoriasis Vulgaris. Determination of psoriasis
severity is vital to determine the treatment given to
patients. It measures the severity of psoriasis,
including BSA, PASI, dermatology life quality
index (DLQI). Mild psoriasis is categorized with
BSA of less than 3%, and severe psoriasis with BSA
more than 10%.
5
In this case, psoriasis BSA is about
25% which is categorized in severe psoriasis.
Topical corticosteroid has been used for vitiligo
as monotherapy or combination with other
modalities, such asfluocinoloneacetonide cream,
betamethasone cream, and clobetasol propionate
cream.Systemic corticosteroid was givenfor
progressive vitiligo. It helps to halt the progression
of the disease and inducingrepigmentation. There are
only several studies published the efficacy and
safety of corticosteroid in vitiligo. The available
reports are case series and lack of well-validated
randomized controlled trials. Systemic corticosteroid
in vitiligo can be administered by oral mini pulse
therapy, daily corticosteroid, and intravenous pulse
therapy.(Lahiri K et al., 2014;Lee J et al., 2016).
reported that oral mini pulse therapy of
methylprednisolone 0.5mg/kg body weight on 2
consecutive days per week with narrowband UVB
phototherapy for 3 months is useful in arresting
vitiligo progression and rapidly inducing
repigmentation with minimal side effect. In this
case, we administered 8 mg oral methylprednisolone
twice a day for two days per week, which
combination with narrowband UVB phototherapy
twice a week, as well as topical corticosteroid.
Several theories have been proposed to explain
the co-occurrence of vitiligo and psoriasis. Reports
of the concomitant disease often describe underlying
autoimmune conditions, suggesting that these
diseases may develop through similar autoimmune
mechanisms. (Puri N et al., 2013).reported that the
presence of psoriasis lesions above the vitiligo
lesions showed an association with increased
production of IL-17A produced by Th17 cells and an
increase in the number of regulatory T cells in the
two entities. Several genetic locus vulnerabilities in
psoriasis and vitiligo have been mapped. The genetic
locus for vitiligo, namely AISI found on the IP 31
chromosome, is located close to the genetic
susceptibility locus for psoriasis, PSORS7.
A recent case-control study of 463 vitiligo
patients, 27 with concomitant psoriasis (2 cases of
colocalized disease), was conducted to investigate
possible associations between vitiligo and
psoriasis.(Bassiouny DA, 2010). The strongest
predictors of concomitant psoriasis were
inflammatory-type vitiligo and a positive family
history of cardiovascular disease.(Arunachalam M et
al., 2014).The authors suggest that common
inflammatory pathways and genetic susceptibility
may explain this association of psoriasis, vitiligo,
and cardiovascular risk factors.
The coexistence of psoriasis Vulgaris limited to
the area of vitiligo lesions can be produced from the
Koebnerphenomenon.
Occurrence of lesions of both
these diseases at same sites predominantly over the
extensors of joints is probably due to chronic minor
friction/ trauma over these sites. (Chakraborty D rt
al., 2017).Coexistence of both vitiligo and psoriasis
lesions over the extensors of joints and his
extremities in the present case can be explained by
this Koebner’s phenomenon.
Other factors that are thought to be for
coexistencevitiligo with psoriasis, namely
cytokines.Cytokines such as TNF-α may have
played a vital role in the pathogenesis of the
coexistent diseases.(Shaequie KE et al., 2017). TNF-
is the main cytokine whose levels are elevated in
psoriasis lesions, where the increase is also found to
increase in the lesion of vitiligo patients, so TNF-
is thought to be associated with the condition of both
diseases.(Park JM et al., 2009).
4 CONCLUSION
Coexistence of vitiligo and psoriasis in a single
patient furthermore at the same location is a rare
occurrence. An underlying autoimmune condition
has to be thought for when such coexistence is seen.
Pathogenesis of the coexistence between psoriasis
and vitiligo, are still not well understood. The
pathogenic factors for each disease, includes
cytokines, autoimmunity, and the Koebner
phenomenonhave been studied, but further
evaluation is needed regarding the mechanism of its
pathogenesis.Coexistence vitiligo and psoriasis is a
red flag signaling the need to dig deeper, looking for
potentially associated diseases, including
cardiovascular, autoimmune, or psychiatric
diagnoses.
REFERENCES
James WD, Berger TG, Elston DM. Andrews’s Diseases
of The Skin Clinical Dermatology.11
th
Ed. New York:
Saunders Elsevier; 2011.p.854-7.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
310

Jacoeb TJA. Vitiligo.In: Menaldi SI, Brahmono K,
Indriatmi W,editors. IlmuPenyakitKulitdanKelamin.7
th
Ed. Jakarta: BadanPenerbit FKUI; 2017.p.352-8.
Ezzedine K, Eleftheriadou V, Whitton M, van Geel N.
Vitiligo. The lancet. 2015;386:74-84.
Birlea SA, Spritz SA, Norris DA. Vitiligo. In: Wolff K,
Goldsmith LA, Katz SI, Gilchrest BA, Paller AS,
Leffell DJ, editors. Fitzpatrick’s Dermatology in
General Medicine.8
th
Ed. New York: McGraw-Hill;
2012.p.792-803.
Jacoeb TJA. Psoriasis.In: Menaldi SI, Brahmono K,
Indriatmi W, editors.
IlmuPenyakitKulitdanKelamin.7
th
Ed. Jakarta:
BadanPenerbit FKUI; 2017.p.213-21.
Springate DA, Parisi R, Kontopantelis E, Reeves D,
Griffiths CEM, Ashcroft DM. Incidence, prevalence
and mortality of patients with psoriasis: a U.K.
population-based cohort study. Br J Dermatol.
2017;176:650-8.
Lahiri K, Chatterjee CM, Sarkar R. Pigmentary disorders-
a comprehensive compendium. 1
st
Ed. India:
JaypeeBrothere Medical; 2014. p.205-21.
Lee J, Chu H, Lee H, Kim M, Kim DS, Oh SH. A
retrospective study of methylprednisolone mini-pulse
therapy combined with narrow-band UVB in non-
segmental vitiligo. Dermatology. 2016;232:224-9.
Puri N, Puri A. Strict anatomical co-existence and
colocalization of vitiligo and psoriasis–a rare
entity.Our Dermatol Online. 2013;4(2):202-4.
Bassiouny DA, Shaker O. Role of interleukin-17 in the
pathogenesis of vitiligo.ClinExpDermatol.
2010;36(3):292-7.
Arunachalam M, Dragoni F, Colucci R, Berti S, Crocetti
E, Galeone M, etal. Non-segmental vitiligo and
psoriasis comorbidity—a case-control study in Italian
patients. J EurAcadDermatolVenereol.
2014;28(4):433-7.
Chakraborty D, Haneef NS, Ravzi F, Kumar BYP, Fatima
N, Koganti NC, etal. A case report showing
coexistence of two autoimmune diseases-psoriasis and
vitiligo. J Med Allied Sci. 2017;7(2):114-7.
Sharquie KE, Salman HA, Yaseen AK. Psoriasis and
vitiligo are close relatives.
ClinCosmetInvestigDermatol. 2017;10:341-5.
Park JM, Kim HJ, Bae BG, Park YK. A case of concurrent
vitiligo and psoriasis.Ann Dermatol. 2009;21(3):330-
3.
Coexistence of Two Autoimmune Diseases: A Case of Colocalized Vitiligo and Psoriasis in One Person
311
